Abstract
Recent developments in the treatment of HIV-1 have improved the disease prognosis from a terminal disease to a chronic disease. The number of HIV-1-infected patients who require surgery has become more common. The main threat to HIV-1-infected patients following surgery is the development of sepsis. In this study, we collected a large number of clinical recordings of HIV-1-infected patients from two hospitals in China, specializing in HIV-1 treatment in order to summarize the risk indicators of sepsis in HIV-1-infected patients. We compared the significant risk indicators between the sepsis and non-sepsis groups. Using logistic regression based on the indicators of four separate surgery-based diseases, we generally found that low CD4 and hypoalbuminemia counts prior to surgery were the significant risk factors for developing sepsis. The morbidity of sepsis in trauma patients was approximately 10 times higher than the dysfunction group, whereas the tumor and the infection groups were approximately 1.5 and 2 times higher, respectively. Based on the comparison between the sepsis and non-sepsis groups for each surgery-based disease, we found that the severity of trauma is a critical risk factor for trauma patients; therefore, limiting the size of the wound during surgery is crucial. HIV-1-infected patients often develop postoperative sepsis due to immunodeficiency and complications due to the surgery. We hope that this study can help to reduce the risk of developing sepsis due to surgery and improve the survival rate of HIV-1-infected patients.
Introduction
Gottlieb et al. published the first report of HIV-1-infected patients in 1981.Citation1 Barre-Sinoussi et al. identified the HIV-1 virus in 1983.Citation2 Because there were no effective treatments, HIV-1-infected patients had a short survival time. The widespread clinical use of antiretroviral drugs has improved the survival time of HIV-1-infected patients significantly.Citation3,Citation4 HIV-1/AIDS is becoming a chronic disease that can be gradually controlled.Citation5 In China, approximately 50 000 patients are newly diagnosed with HIV-1 yearly. Therefore, the number of HIV-1-infected people is rapidly increasing.Citation6 HIV-1-infected people are prone to developing diseases that require surgical treatment,Citation7 such as appendicitis, liver cancer, and thighbone fracture. It is anticipated that there will be a corresponding increase in surgical workload for HIV-1-infected patients.
In Europe, Africa, and America, HIV-1-infected patients generally receive surgery in general hospitals. Because the immune system of HIV-1-infected patients is weak, standard treatment for HIV-1-infected patient is typically not sufficient to ensure the expected outcome. Therefore, HIV-1-infected patients who received surgery in general hospitals had a greater chance to develop complications due to infections, thus leading to the high rate of mortality.
In China, HIV-1-infected patients are referred to a special hospital for infectious diseases to receive treatment. The medical staff in these hospitals has significant experience in treating HIV-1-infected patients. Shanghai Public Health Clinical Center (SPHCC), a research-oriented hospital located in Shanghai, is the designated hospital for the treatment of HIV-1-infected patients in Shanghai and surrounding regions. Nearly all of the confirmed HIV-1-infected patients in Shanghai, and several in other nearby provinces, are referred to the SPHCC.Citation8 Henan province in China is one of the regions where the incidence of HIV-1 is high. Most of the HIV-1-infected patients there are treated at Zhengzhou Sixth People Hospital, which is a special hospital for infectious diseases. The main threat to HIV-1-infected patients following surgery is the development of sepsis. An effective perioperative management is capable of controlling the occurrence of sepsis, but the design of an efficient management strategy is still unexplored. In this study, the clinical recordings of 541 HIV-1-infected patients who underwent surgery at SPHCC and 262 HIV-1-infected patients who underwent surgery at Zhengzhou Sixth People Hospital from January 2010 to February 2014 were collected. The surgery breakdown in these patients can be classified into four separate surgery-based diseases (trauma, dysfunction, infection, and tumor). The trauma patients mainly had fractures and required surgery for open wound reduction and internal fixation. The dysfunction patients included hernia of the abdominal wall, varicose of the great saphenous veins, cirrhosis of the liver, excessive spleen functions, intestinal adhesion obstruction, gall bladder, and urinary tract calculi obstruction, etc. The infected patients were largely associated with tuberculosis (mainly abdominal tuberculosis or bone tuberculosis lesion) and genital warts caused by the papillomavirus. The tumor patients mainly had lymphoma, stomach, and liver cancer. Based on our large sample of clinical data, the purpose of this study was to generate a comprehensive surgery risk evaluation of HIV-1-infected patients. We approached this problem in three directions as follows: (i) we reported a detailed surgical state of HIV-1-infected patients who underwent surgery at the two Chinese hospitals specializing in infectious diseases and the different physiological measures between non-sepsis and sepsis patients, (ii) we analyzed the postoperative risk of sepsis under different conditions using multi-factor analysis methods, (iii) we discussed the relationship between physiological measures and sepsis in different surgery-based diseases. We hope that this work can provide a critical reference for controlling and reducing the mortality of patients with postoperative sepsis.
Material and methods
Patients
The 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definition was used as a reference.Citation9 A total of 803 clinical documents corresponding to the HIV-1-infected patients admitted between January 2010 and February 2014 were gathered for the retrospective analysis. Of those, 541 records were collected from SPHCC and 262 from Zhengzhou Sixth People Hospital. The patients selected in this study underwent surgeries with complete perioperative records, which contained routine examinations and an immune system function test. The HIV-1-infected patients who developed systemic inflammatory response syndrome with infection were confirmed to develop postoperative sepsis. The basic demographic characteristics included gender, age, and year of diagnosis. The clinical condition included the physiological parameters before and after operation, the type of surgery performed, the presence of sepsis and the outcome. To control the sepsis variance that may be caused by contamination in the two hospitals, we reviewed the clinical recordings of the patients with normal immune systems who had surgeries in the same hospital to obtain their incidence of postoperative sepsis.
Perioperative management and treatment
All the patients had been required to undergo routine laboratory examinations and preoperative preparations before surgery and two weeks following surgery. Antiretroviral therapy, antifungal medication, and sulfamethoxazole were administered preoperatively as the prophylaxis against Pneumocystis jirovecii, fungal, and other infections when the patient’s CD4 count was <200 cells/µL. Nutritional support and symptomatic treatment were ensured. The surgical procedures were carried out by veteran surgeons, including general surgery (six surgeons), thoracic surgery (four surgeons), orthopedic surgery (two surgeons), and urologic surgery (one surgeon).
Statistical analysis
The data were analyzed using SPSS 17.0 (SPSS, Chicago, IL, USA). The descriptive statistics were represented as the mean ± SD when the data sets were of normal distribution. Otherwise, the descriptions were represented as the median (95% confidence interval (CI) low, 95% CI high). The demographic and the available laboratory data were compared in a singer-factor analysis according to the sepsis status, the type of the surgery-based diseases or the cross-effect of the sepsis status and the type of the surgery-based diseases. The enumeration data were compared by the chi-square test or the Fisher’s test. The measurement data were compared with an independent t-test sample, analysis of variance, or the rank-sum test when the data sets did not comply with the normal distribution. An unconditional binary logistic regression analysis checked for the interactions and was represented as an odds ratio with the 95% CI used to determine the sepsis morbidity factors using the multi-factor analysis method. The positive condition was marked by 1, and the negative condition was marked by 0. In addition, the operation type was set as the category, and the dysfunction group was chosen as the control group. Statistical significance was set at P < 0.05.
Ethical considerations
The community surveys were conducted and approved by the ethical committees of the SPHCC affiliated with Fudan University. The clinical documents were provided by two of the co-authors of this study. All of the received records were anonymized and could not be linked to individuals. The methods carried out in this study were in accordance with the approved guidelines.
Results
Geographical coverage of this study
The patients in our study were from 28 provinces or autonomous regions in China with the exceptions of Tibet, Tianjing, Hebei, Hong Kong, and Taiwan. The majority were patients from Henan and Shanghai, which accounted for 24.31% and 24.39% of all patients, respectively. The other places of residence for the patients included the nearby provinces Jiangsu (10.76%), Anhui (6.77%), Zhejiang (9.03%), Fujian (5.03%), and Jiangxi (3.30%), which accounted for 34.90% of all the patients.
Patient characteristics and comparisons
Most of the HIV-1-infected patients were between 30 and 55 years old, but the ages ranged from 10 to 84 years. Among the 803 HIV-1-infected patients, 313 (38.9%) developed sepsis. Within the same period, the population of patients with a normal immune system and having the same general surgeries in same hospital had a much lower incidence rate of postoperative sepsis at approximately 3%. Therefore, the sepsis in HIV-1-infected patients was not caused by hospital contamination. In our study, a total of 17 HIV-1-infected patients died (2.11%) within 30 days following surgery with the majority being males. There were no significant differences in the incidence of sepsis between the genders.
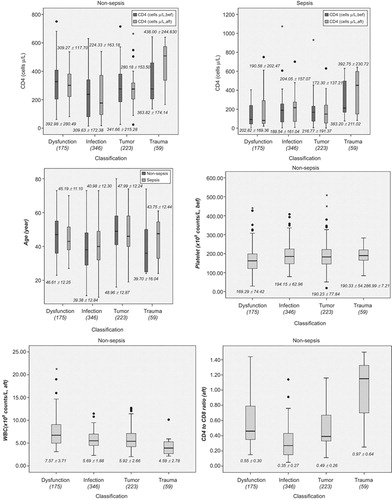
The patients were divided into two groups: sepsis and non-sepsis. A detailed report is described in . The white blood cell (WBC) measurement in the sepsis and the non-sepsis groups before and after the surgery were in the normal range (4.0–10.0 × 109/L). Prior to surgery, the WBC measurement of the sepsis group was significantly higher than the non-sepsis group. Likewise, the hemoglobin measurement in both groups before and after the surgery was in the normal range (120–170 g/L); the hemoglobin count of the sepsis group was significantly lower than the non-sepsis group before and after surgery. The platelet and protein measurements in both groups before and after the surgery were also in normal range (100–300 × 109/L, 40–55 g/L, respectively). The preoperative and postoperative protein levels of the sepsis group were significantly lower than the non-sepsis group. The preoperative and postoperative CD4 counts and the CD4 to CD8 ratio of the two groups were lower than normal (726.99 ± 255.21 and 1.66 ± 0.33, respectively), while the preoperative and postoperative CD8 counts were higher than normal (539.58 ± 134.00). Among the different surgery-based diseases, including dysfunction (21.7%), infection (43.1%), tumor (27.8%), and trauma (7.4%), the incidence of sepsis varied significantly. The morbidity of the trauma group was the highest, and the dysfunction group morbidity was the lowest. The difference in the sepsis incidence between the infection and the tumor group was not significant.
Table 1 Statistical results after the classification in term of sepsis
Unconditional binary logistic regression analysis
The results of the unconditional binary logistic regression analysis are represented in . It was found that low CD4 and hypoalbuminemia counts prior to surgery were the significant risk factors for postoperative sepsis (P < 0.05). The sepsis morbidity of the four surgery-based diseases varies greatly. The sepsis morbidity in the trauma patients was approximately 10 times higher than the dysfunction group, whereas the tumor group and the infection group were approximately 1.5 and 2 times higher, respectively (). Using this regression model, the accuracy in predicting sepsis based on the measurements prior to surgery was 72.6%; the sensitivity and the specificity were 84.6% and 52.6%, respectively.
Table 2 Logistical regression of risk factors before operation (different operation type)
Differences among the four types of surgery-based diseases
The measurements that were significantly different among the four groups were the CD4 counts before and after surgery in the sepsis group and the WBC counts, CD4 to CD8 ratio after surgery and platelet level prior to surgery in the non-sepsis group. The patient age in the four separate surgery-based diseases varied significantly in the non-sepsis and sepsis groups. In the non-sepsis group, the CD4 counts and the CD4 to CD8 ratio after surgery in the trauma group were significantly different. Similar preoperative and postoperative CD4 counts were found in the trauma sepsis group. In contrast, the postoperative WBC level in the non-sepsis group was the highest.
outlines the significant results among the four groups. The CD4 level following surgery in the non-sepsis trauma HIV-1-infected patients was higher than other groups, while the CD4 level following surgery in the non-sepsis infection HIV-1-infected patients was the lowest. In the sepsis patients, the CD4 level of the dysfunction group was the lowest. For age, the non-sepsis tumor group was the oldest, and the non-sepsis trauma group was the youngest. The non-sepsis dysfunction group had the lowest platelet count. The non-sepsis trauma group had the lowest WBC but the highest CD4 to CD8 ratio.
Sepsis differences of the four types of surgery-based diseases
Based on the classification of the surgery-based diseases, the data sets were further divided into eight groups according to the sepsis condition. The statistical results are displayed in . Prior to surgery, there was no significant difference in the CD4 level of trauma patients between the non-sepsis and the sepsis group. A study by Guth et al. reported similar results.Citation10 The CD8 level of the trauma group is different than the CD8 level in the other three surgery-based diseases. In trauma patients, the CD8 level of the sepsis group was higher than the level of the non-sepsis group. After surgery, the CD4 level of the trauma group showed little change, and the CD4 level in other groups also showed little or no change. The CD8 level of the trauma sepsis group was still higher than the non-sepsis group. The CD8 level of all the groups following surgery returned to the normal level. The changes of the other parameters were also in the normal range.
Table 3 Statistical results of operation type and sepsis condition
Discussion
We divided the data into the sepsis group and the non-sepsis group following surgery. Before surgery, the CD4, CD8, CD4 to CD8 ratio, hemoglobin and protein levels of the sepsis group were significantly lower than the non-sepsis group. Following surgery, the hemoglobin, protein, CD4 and CD4 to CD8 ratio were significantly different. Using unconditional multi-factors logistic regression, we calculated that low preoperative CD4 and hemoglobin levels were the significant risk factors for postoperative sepsis. CD4 has a direct relationship with the immune system. When a patient is infected with the HIV-1 virus, their immune system is severely compromised. These patients with a weak immune system are more prone to developing infections and other complications. Therefore, a low CD4 level is an important indicator for HIV-1-infected patients prior to surgery. Hemoglobin is an important transporter in the body. A lack of hemoglobin greatly influences the transport of oxygen, which further weakens the production of CD4 cells in the body. Therefore, a low hemoglobin level is also a critical indicator for HIV-1-infected patients prior to surgery. It has been suggested that patients with low hemoglobin should be supported with enhanced nutrition. Surgery can be performed when the condition of the patient has improved. Ideally, patients with a CD4 level is less than 200 cells/µL should be treated in special hospitals for infectious diseases where they can receive high-quality perioperative management. HIV-1-infected patients with a normal CD4 level can be treated in a general hospital. If the surgical procedure is demanding and the patient condition is complicated, the surgery should be performed in a high-level hospital that specializes in infectious diseases. Non-sepsis patients possessing lower WBC counts but a higher proportion of CD4 and CD8 counts, compared to the sepsis population and HIV-1-infected patients with lower CD4 and CD8 counts, are more vulnerable to the HIV-1 virus and therefore have a higher chance of developing sepsis. As the viral load in the body increases, more WBCs are generated in the sepsis patients to combat the virus.
Surgery-based diseases can be divided into five categories: trauma, infection, tumor, dysfunction, and deformity. These disease states require surgery for treatment. Therefore, we used this category to group our data. No surgeries related to innate or acquired deformity were performed. Surgeries for infection were the most common. The second and the third most common surgeries were tumor and dysfunction, respectively. There were only a few cases of surgeries due to trauma.
Among the four groups in our study, the trauma patients group had a higher CD4 level than the other groups (). The HIV-1-infected trauma patients in our study were initially diagnosed in general hospitals. The HIV-1 virus was detected prior to surgery, and the patients were subsequently referred to a hospital specializing in infectious diseases. Most of the trauma patients had fractures and required surgery for open wound reduction and internal fixation. They did present obvious symptoms of HIV-1. Several patients did not even know they were infected with the HIV-1 virus. Some patients deliberately withheld their HIV-1 history. The CD4 level in the trauma patients between the sepsis group and the non-sepsis group differed slightly. If the CD4 level of the trauma patients was close to normal, the complications due to infections are similar to patients without HIV-1. Therefore, we think that the morbidity of sepsis in the trauma patients may have something to do with the severity of the trauma. When surgeons perform surgery on HIV-1-infected trauma patients, it is necessary to control and limit the size of the wound.
Patients in the tumor or infection groups with a low CD4 level had a high probability of developing postoperative sepsis. Some HIV-1-infected patients presented with complications resulting from abscesses, which could be caused by purulent bacteria. However, in most cases, the infections were complicated by tuberculosis (mainly abdominal tuberculosis or bone tuberculosis lesions) and genital warts caused by papillomavirus. Although the infectious lesions can be eliminated by surgery, the wounds do not heal well, and the lesions could easily relapse. These factors increase the rate of developing postoperative sepsis. The majority of HIV-1-infected patients in the tumor group had lymphoma (23%) with the second and third most common cause being stomach cancer and liver cancer, respectively. The incidences of postoperative sepsis in the HIV-1-infected tumor and infection patients are related to the immunodeficiency and the complexity of the surgery. After removal of the lesions, it is crucial to provide patients anti-viral, anti-tuberculosis, and anti-fungal treatments during the perioperative period for patients undergoing surgery for tumors and infections.
The dysfunction patients presented with a variety of conditions, including hernia of abdominal wall, varicose of the great saphenous veins, cirrhosis of the liver, excessive spleen functions, intestinal adhesion obstruction, gall bladder and urinary tract calculi obstruction, etc. The incidences of postoperative sepsis in the dysfunction patients also are related with the immunodeficiency and the complexity of the surgery.
In Europe, Africa, and America, the majority of HIV-1-infected patients undergo surgery in general hospitals. Medical personnel in general hospitals may have insufficient experience in the treatment of HIV-1-infected patients, so the patients may experience many postoperative complications. It has been reported that between January 1997 and December 2007, 55% of HIV-1-infected patients had complications due to infections, and 30% of the patients died following abdominal surgery.Citation11,Citation12 Abdominal surgery is often not a difficult operation. HIV-1-infected patients who have abdominal surgery rarely die during the process of surgery. In fact, nearly all of the patients died of postoperative complications caused by an infection. In the past few years, HIV-1-infected patients in China have had difficulty receiving surgeries, due mainly to these complications. To address this situation, special hospitals for infectious diseases have started to build their own surgical departments in recent years. Therefore, nearly all HIV-1-infected patients in China are referred to and have surgeries performed in these specialized hospitals. Gradually, the surgeons in these hospitals have obtained vast experience in treating HIV-1-infected patients. Therefore, HIV-1-infected patients can receive high-quality perioperative management and as a result, a much higher survival rate.
Surgery on HIV-1-infected patients is vastly different than surgery on patients without HIV-1. During the treatment process for HIV-1-infected patients, other than the preoperative preparation and postoperative care,Citation13,Citation14 it is also crucial to possess the knowledge and skills required for the prevention of infection. Our work, based on a large number of clinical records, analyzes the risks of different surgical-based diseases for HIV-1-infected patients, which can be referenced during perioperative management. Surgeons in special hospitals for infectious diseases can accumulate clinical experience in the treatment of HIV-1-infected patients. HIV-1-infected patients, especially those in critical condition who choose to have surgery in these specialized hospitals, have a much lower chance of developing complications and have a higher chance of survival.
We have compiled a comprehensive surgery risk evaluation based on a large number of surgical records from HIV-1-infected patients. This work could provide a critical reference for controlling and reducing the mortality of patients with postoperative sepsis. Our study analyzed the sepsis risk of HIV-1-infected patients in regards to general surgery-based diseases. Based on our findings, further research can focus on the risk of developing postoperative sepsis in other specific disease states associated with HIV-1-infected patients and the complications that could arise as a result of surgery.
We thank the staff of the Shanghai Public Health Clinical Center and Zhengzhou Sixth People Hospital for collecting the clinical data. We also thank the anonymous reviewers for their comments and clarifications concerning this manuscript. We are grateful to Dr Da Wo, who is a native English speaker and works at the Tongji University Medicine School, for revising and editing the manuscript.
- Gottlieb MS, Schroff R, Schanker HM et al.Pneumocystis carinii pneumonia and mucosal candidiasis in previously healthy homosexual men: evidence of a new acquired cellular immunodeficiency. New Engl J Med 1981;305: 1425–1431.
- Barré-Sinoussi F, Chermann JC, Rey F et al.Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS). Science 1983;220: 868–871.
- Gutierrez F, Garcia L, Padilla S et al.Risk of clinically significant depression in HIV-infected patients: effect of antiretroviral drugs. HIV Med 2014;15: 213–223.
- Hattab S, Guihot A, Guiguet M et al.Comparative impact of antiretroviral drugs on markers of inflammation and immune activation during the first two years of effective therapy for HIV-1 infection: an observational study. BMC Infect Dis 2014;14: 122.
- Ma Y, Zhang FJ, Zhao Y et al. Cohort profile: The Chinese national free antiretroviral treatment cohort. Int J Epidemiol 2010;39: 973–979.
- Qin QQ, Wang L, Ding ZW et al.[Situation on HIV/AIDS epidemics among migrant population in China, 2008–2011.] Zhonghua Liu Xing Bing Xue Za Zhi 2013;34: 41–43.Chinese.
- Kerr E, Middleton A, Churchill D et al.A case−control study of elective hip surgery among HIV‐infected patients: exposure to systemic glucocorticoids significantly increases the risk. HIV Med 2014;15:182–188.
- Feng TN, Sun XW, Wu HJ, Jiang CH.The essential of hierarchy of E-continuing medical education in China. In: Li SZ, Jin Q, Jiang XH, James J, Park JK, editors, Frontier and Future Development of Information Technology in Medicine and Education. 2nd edn. Qinghai: Springe, 2014: 2267–2272.Chinese.
- Levy MM, Fink MP, Marshall JC et al.2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intens Care Med 2003;29: 530–538.
- Guth AA, Hofstetter SR, Pachter HL.Human immunodeficiency virus and the trauma patient: factors influencing postoperative infectious complications. J Trauma 1996;41: 251–255.
- Moody F, Deneve JL, Grant W.CD4 count is predictive of outcome in HIV-positive patients undergoing abdominal operations Discussion. Am J Surg 2010;200: 699–700.
- Deneve JL, Shantha JG, Page AJ, Wyrzykowski AD, Rozycki GS, Feliciano DV.CD4 count is predictive of outcome in HIV-positive patients undergoing abdominal operations. Am J Surg 2010;200: 694–699.
- Owens C, Stoessel K.Surgical site infections: epidemiology, microbiology and prevention. J Hosp Infect 2008;70: 3–10.
- Dua R, Wajed S, Winslet M.Impact of HIV and AIDS on surgical practice. Ann Roy Coll Surg 2007;89: 354.