Abstract
Background: Low Hartmann's procedure (LHP) and intersphincteric abdominoperineal resection (iAPR) are both surgical options in the treatment of distal rectal cancer when there is no intention to restore bowel continuity. This study aimed to evaluate current practice among members of the Dutch Association of Coloproctology (WCP).
Methods: An online survey among members of the WCP who represent 66 Dutch hospitals was conducted. The survey consisted of 15 questions addressing indications for surgical procedures and complications.
Results: Surgeons from 37 hospitals (56%) responded. Thirty-six percent does not distinguish low from high Hartmann's procedures based on estimated length of the rectal remnant. Overall, iAPR was the preferred technique in 86%. If asking whether operative approach would be different in tumours at 1 cm from the pelvic floor compared to 5 cm distance, 62% stated that they would consider a different technique. The incidence of pelvic abscess after LHP was thought to be higher, equal or lower than iAPR in 36%, 36% and 21%, respectively, with the remaining respondents not answering this question.
Conclusions: The vast majority of the respondents considers iAPR as the preferred non-restorative procedure for rectal cancer not invading the sphincter complex, which contradicts with population based data from 2011.
Introduction
Colorectal cancer (CRC) is one of the top three most commonly diagnosed cancers worldwide in both males and females [Citation1]. In the Netherlands, 15,000 new cases of CRC have been diagnosed in 2016, of which 4000 new cases of rectal cancer [Citation2]. In rectal cancer, we primarily focus on resection of the tumour followed by restoration of bowel continuity, but frequently encountered problems after restorative surgery, such as anastomotic leakage and poor functional outcome have to be taken into account. Anastomotic leakage of a colorectal or coloanal anastomosis has been reported to occur in up to 21% [Citation3,Citation4], and recent studies focussing on the low anterior resection syndrome score (LARS score) show incidences of major LARS of 33 and 56% [Citation5,Citation6]. Considering these high incidences of anastomotic leakage and poor functional outcome, restoring bowel continuity might not always be the best option in specific patient populations, despite this is technically achievable and oncologically safe. Such patients are, for example, frail elderly patients or those with multiple comorbidities irrespective of age. Low Hartmann’s procedure (LHP) and intersphincteric abdominoperineal resection (iAPR), both with the creation of a definitive colostomy, have been described as surgical procedures for resection of distal rectal cancer without invasion of the sphincter complex when bowel continuity is not desired. LHP has been associated with high rates of pelvic abscesses, but literature is inconsistent [Citation7–10]. Data on the risk of pelvic abscess after iAPR are even more scarce [Citation10–12]. This lack of evidence forces colorectal surgeons to base their choice for either LHP or iAPR as non-restorative treatment for distal rectal cancer on mere experience.
The aim of this study was to gain insight into current preferences regarding indication and surgical technique, as well as opinions on infectious complications considering its incidence and preferred treatment following LHP and iAPR. This survey among Dutch colorectal surgeons was intended to be a first step towards guidelines for the treatment of rectal cancer not invading the sphincter complex, and without the intention to restore continuity.
Materials and methods
Survey
An online survey consisting of 15 questions regarding LHP and iAPR as primary treatment for rectal cancer was sent to members of the Dutch Association of Coloproctology (WCP) in October 2016, representing 66 Dutch hospitals. The WCP aspires to ensure at least one representative from every Dutch hospital. A reminder was sent by email in December 2016 to all representatives who did not respond after the first email. The survey contained questions about the definition of the LHP, choices in operative technique in ultralow tumours (<1 cm from the pelvic floor) and more proximal tumours (<5 cm), the choice for LHP or iAPR as primary treatment strategy, the use of omentoplasty in iAPR, estimated incidence of pelvic abscesses subsequent to both LHP and iAPR and the treatment of pelvic abscesses after LHP. The complete survey can be found in Supplementary file 1.
Operative techniques
In order to clearly outline the procedures being discussed in this survey, a description was included. In LHP, a rectal resection according to TME principle is performed, with transection and closure of the rectum below the tumour, and creating an end colostomy [Citation13]. In iAPR, the anoderm is incised by a perineal approach, continuing the TME dissection in the intersphincteric plane, with preservation of the external sphincter, levator muscles and puborectal muscle. No rectal remnant is left behind and an end colostomy is created [Citation11].
Data extraction and statistical analysis
Data were collected using an online survey tool. All data were collected anonymously and processed using IBM SPSS Statistics for Windows (Version 24.0. Armonk, NY: IBM Corp). According to distribution, numerical data were reported as median with range or interquartile range (IQR) or mean with standard deviation (SD). Categorical variables were presented as number and proportion in percentages.
Results
Response rate at hospital level was 37 out of 66 (56%). Of four hospitals with multiple locations, multiple surgeons representing each location responded, resulting in a total number of responding surgeons of 42. Representatives of six out of eight Dutch academic hospitals responded, 23 teaching hospitals and eight non-teaching hospitals. An overview of the respondents’ characteristics is shown in .
Table 1. Respondents’ characteristics.
LHP and iAPR
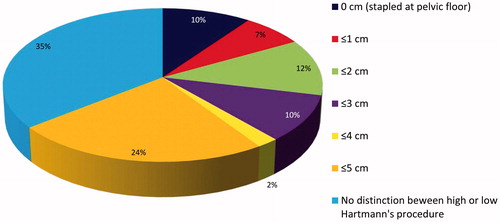
In total, 36% of the respondents (n = 15/42) stated not to distinguish between a high or low Hartmann’s procedure. shows the distribution of the definition of a low Hartmann’s procedure as reported by all responding surgeons. When there is no oncological indication to perform a conventional or extralevator APR, 86% (n = 36/42) of the responding surgeons consider an iAPR as the preferred procedure in low rectal cancer when there is no intention to restore bowel continuity. Twenty-six respondents (62%) indicated that they would consider a different operative technique in a tumour located at one centimetre (cm) from the pelvic floor than in a tumour located at 5 cm. Not all choices were clarified, but the most frequently stated reason was that in ultralow tumours (one cm from the pelvic floor) an iAPR is more frequently considered than in more proximal tumours. Regarding the definitions of a low Hartmann’s procedure and the choice for operative technique in tumours at 1 and 5 cm from the pelvic floor, 21% (n = 9/42) reported that there is no consensus within their hospital.
Figure 1. At what expected length of the rectal remnant do you consider a Hartmann’s procedure as a low Hartmann’s procedure?
Omentoplasty in iAPR is always performed by 45% (n = 19/42) of the surgeons, 36% (n = 15/42) performs an omentoplasty selectively and 19% (n = 8/42) never performs an omentoplasty in iAPR. Thirty-two surgeons (76%) reported consensus in their hospital regarding the creation of an omentoplasty.
Pelvic abscess
Of all responding surgeons, 36% (n = 15/42) believes that a pelvic abscess occurs more frequently after LHP than after iAPR, 36% (n = 15/42) believes that pelvic abscesses occur in a similar rate after both LHP and iAPR and 21% (n = 9/42) thinks that iAPR results in more pelvic abscesses than LHP. Three correspondents did not answer this question. The majority of the respondents (27/42, 64%) use transanal drainage as preferred treatment for pelvic abscesses after LHP with percutaneous drainage on indication, while 14% (n = 6/42) always use transanal drainage and 14% (n = 6/42) prefer percutaneous drainage and transanal drainage on indication. Three respondents did not answer this question. In total, 29/42 surgeons (69%) indicated that there was a consensus in their unit regarding the treatment of pelvic abscesses subsequent to LHP, 11/42 (26%) reported no consensus regarding this topic and two respondents (5%) did not answer this question.
Discussion
This study shows that there is no consensus regarding operative technique for non-restorative surgery in the primary treatment of rectal cancer within the community of Dutch colorectal surgeons. It shows that 86% of the surgeons consider iAPR as the preferred procedure, but 21% indicates that there is no consensus within their hospital regarding the specific use of LHP or iAPR if considering tumours at 1 or 5 cm distance from the pelvic floor. Omentoplasty following iAPR is used in 81% of the respondents, either as a routine or on indication. Abscesses after LHP are preferably drained through the rectal stump, with 14% preference for percutaneous drainage, but 26% of respondents indicate absence of consensus on this topic within their units.
The high rate of 86% of surgeons who consider iAPR as the preferred technique in this specific group of rectal cancer patients is noteworthy. A recent publication by the Dutch Snapshot Research Group, reporting on cross-sectional data on the treatment of rectal cancer in the Netherlands in 2011, shows that non-restorative surgery consisted of 25% iAPR and 75% LHP [Citation12]. Possible explanations for this discrepancy might be related to the relatively low response rate with limited representativity, the restricted intra-hospital consensus, and historical changes in decision making (between 2011 and 2016). The iAPR technique has gained popularity over the last years as an alternative to LHP, probably related to some literature reports on relatively high abscess rates after LHP [Citation7–9].
The lack of consensus on preferred operative technique might be explained by the differences in expected complications. This survey shows that there is a difference in expectations among surgeons regarding the pelvic abscess rate after both iAPR and LHP. Probably, surgeons who expect a higher rate of pelvic abscesses after LHP will prefer an iAPR and vice versa. The variety in opinions regarding the risk of pelvic abscess subsequent to both techniques is not surprising, since literature on this topic is also inconclusive. There are only few small and retrospective studies which report on pelvic abscess rate after Hartmann’s procedure, with varying rates between 3 and 33% [Citation7–10,Citation14]. T⊘ttrupand Frost [Citation9] reported an incidence of pelvic abscesses of 33%, when in the Hartmann’s procedure the rectum was transected within 2 cm of the pelvic floor. In contrast, Sverrisson et al. reported an incidence of only 3% in patients who had a Hartmann’s procedure of which 90% was stapled just above or at the pelvic floor. Therefore, it is still unclear if the length of the rectal remnant influences the risk of pelvic abscess formation [Citation9,Citation14]. Pelvic sepsis has been reported between 6 and 17% following iAPR with end colostomy [Citation10–12]. Also, a 30% rate of perineal wound problems after iAPR has been described [Citation15]. This finding might also influence surgeons in choosing between LHP and iAPR, but this aspect was not included in the survey.
The HAPIrect trial is an ongoing randomized multicentre trial comparing Hartmann’s procedure and iAPR as primary treatment for rectal cancer, also including patients with rectal cancer with tumours up to 5 cm from the anal verge [Citation16]. The lowest of these tumours are of specific interest, since it can be hypothesized that a shorter rectal remnant is more likely to break down and cause pelvic sepsis, possibly favouring the iAPR in this group. Since the (ultra)low Hartmann’s procedure might be more prone to complications than the more proximal procedure, it is of importance to distinguish between the two. Of all surgeons, 36% does not distinguish between high or low Hartmann’s procedure, and within the remaining 64% there is no consensus on the definition of a low procedure. Similar to the respondents of this survey, literature is not consistent on the definition of a low Hartmann’s procedure.
Performing an omentoplasty can potentially reduce the incidence of pelvic abscess by filling the pelvic cavity and because of its physiological properties such as the promotion of angiogenesis and immunological effects. This was confirmed in a recent review showing a reduction of perineal wound morbidity after APR when an omentoplasty is created [Citation17]. A large cross-sectional study in the Netherlands, however, revealed no reduction of pelvic abscesses after APR with primary closure of the perineal wound and omentoplasty compared to primary closure without omentoplasty [Citation18]. The present survey found that only 19% of respondents never perform an omentoplasty in iAPR, despite conclusive evidence on the additional value and the need for additional dissection and increase in operating time.
Limitation of this study is the low response rate of 56%, which could lead to nonresponse errors. However, it has been demonstrated that a low response rate does not necessarily influence the outcome and the representativeness of the respondents is more important than the actual response rate [Citation19,Citation20]. We do believe to have reached a representative sample of Dutch colorectal surgeons by contacting members of the WCP from each hospital throughout all the Netherlands, with respondents from academic, teaching as well as non-teaching hospitals.
Clearly, there is a need for more high-quality studies and guidelines regarding the primary treatment of rectal cancer without restoration of bowel continuity, especially since the frail elderly patients with multiple comorbidities are a growing population; a population wherein the surgeon and patient might choose to avoid the risks of a leaking anastomosis or poor functional outcome after restoration of bowel continuity by creating a definitive colostomy.
Conclusions
There is no consensus among colorectal surgeons in the Netherlands regarding the choice for LHP or iAPR as primary treatment for patients with distal rectal cancer without the intention to restore bowel continuity. The majority prefers iAPR, which is in contradiction to published Dutch daily practice 5 years earlier. The lack of consensus on the definition of LHP and the varying thoughts on pelvic abscess formation following the two procedures reflects the ambiguity on this topic in current literature.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108.
- Dutch Cancer Registry. Cijfers over Kanker. 2017. Available from: http://www.cijfersoverkanker.nl/
- Trencheva K, Morrissey KP, Wells M, et al. Identifying important predictors for anastomotic leak after colon and rectal resection: prospective study on 616 patients. Ann Surg. 2013;257:108.
- Borstlap WAA, Westerduin E, Aukema TS, et al. Anastomotic leakage and chronic presacral sinus formation after low anterior resection: results from a large cross-sectional study. Ann Surg. 2017;266:870–877.
- Hughes DL, Cornish J, Morris C. Functional outcome following rectal surgery-predisposing factors for low anterior resection syndrome. Int J Colorectal Dis. 2017;32:691–697.
- Koedam TW, van Ramshorst GH, Deijen CL, et al. Transanal total mesorectal excision (TaTME) for rectal cancer: effects on patient-reported quality of life and functional outcome. Tech Coloproctol. 2017;21:25–33.
- Frye JN, Carne PW, Robertson GM, et al. Abdominoperineal resection or low Hartmann’s procedure. ANZ J Surg. 2004;74:537–540.
- Molina Rodriguez JL, Flor-Lorente B, Frasson M, et al. Low rectal cancer: abdominoperineal resection or low Hartmann resection? A postoperative outcome analysis. Dis Colon Rectum. 2011;54:958–962.
- Tøttrup A, Frost L. Pelvic sepsis after extended Hartmann’s procedure. Dis Colon Rectum. 2005;48:251–255.
- Westerduin E, Musters GD, van Geloven AAW, et al. Low Hartmann’s procedure or intersphincteric proctectomy for distal rectal cancer: a retrospective comparative cohort study. Int J Colorectal Dis. 2017;32:1583–1589.
- Eriksen MH, Maina P, Jensen KH. Low risk of pelvic sepsis after intersphincteric proctectomy in patients with low rectal cancer. Dan Med J. 2014;61:A4972.
- Westerduin E, Aukema TS, van Geloven AAW, et al. What to do with the rectal stump during sphincter preserving rectal cancer resection with end colostomy: a collaborative snapshot study. Colorectal Dis. 2018;20:696.
- Enker WE. Total mesorectal excision-the new golden standard of surgery for rectal cancer. Ann Med. 1997;29:127–133.
- Sverrisson I, Nikberg M, Chabok A, et al. Hartmann’s procedure in rectal cancer: a population-based study of postoperative complications. Int J Colorectal Dis. 2015;30:181–186.
- Musters GD, Sloothaak DA, Roodbeen S, et al. Perineal wound healing after abdominoperineal resection for rectal cancer: a two-centre experience in the era of intensified oncological treatment. Int J Colorectal Dis. 2014;29:1151–1157.
- Smedh K, Sverrisson I, Chabok A, et al. Hartmann’s procedure vs abdominoperineal resection with intersphincteric dissection in patients with rectal cancer: a randomized multicentre trial (HAPIrect). BMC Surg. 2016;16:11–43.
- Killeen S, Devaney A, Mannion M, et al. Omental pedicle flaps following proctectomy: a systematic review. Colorectal Dis. 2013;15:e634–e645.
- Blok RD, Musters GD, Borstlap WAA, et al. Snapshot study on the value of omentoplasty in abdominoperineal resection with primary perineal closure for rectal cancer. Ann Surg Oncol. 2018;25:729–736.
- Cook C, Heath F, Thompson RL. A meta-analysis of response rates in web- or internet-based surveys. Educ Psychol Meas. 2000;60:821–836.
- Krosnick JA. Survey research. Annu Rev Psychol. 1999;50:537–567.
