Abstract
Objective: To determine the diagnostic accuracy of three screening questions (3Q/TMD) in relation to the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD), in a specialized clinic.
Material and methods: Consecutive patients, >18 years, referred with a possible TMD complaint to the Orofacial Pain and Dysfunction clinic, Academic Centre for Dentistry Amsterdam, the Netherlands, were included in the study. All patients (n = 449; mean age 44 years; 72% females), answered the 3Q/TMD and the DC/TMD questionnaire before a DC/TMD examination. The 3Q/TMD constitutes of two questions on weekly pain from the jaw, face and temple region (Q1), and on function (Q2), and one function-related question on weekly catching and/or locking of the jaw (Q3). Q1 and Q2 were evaluated in relation to a DC/TMD pain diagnosis and Q3 in relation to a subgroup of DC/TMD intra-articular diagnosis, referred to as the reference standard.
Results: In total, 44% of patients received a pain-related DC/TMD diagnosis and 33% an intra-articular reference DC/TMD diagnosis. Sensitivity for the two pain screening questions was high (0.83–0.94), whereas specificity was low (0.41–0.55). For the function-related question, sensitivity was low (0.48), whereas specificity was high (0.96).
Conclusions: In a specialized pain clinic, the two pain questions (Q1, Q2) are positive in most patients with pain-related TMD. Therefore, in case of a positive response, further diagnostic procedures for TMD pain are warranted. For the functional screening question (Q3), a positive response is indicative for an intra-articular DC/TMD diagnosis, while in case of a negative outcome, an intra-articular TMD might still be present.
Introduction
Temporomandibular disorders (TMD) are an umbrella term for different conditions including jaw muscle and temporomandibular joint (TMJ) pain, limitations of mandibular movements, and intra-articular functional disturbances, such as TMJ sounds and locking of the jaw [Citation1]. Epidemiological studies have shown that TMD and orofacial pain conditions are common in the general population. The prevalence of TMD is highly dependent on the criteria attributed to the condition (e.g. frequency, intensity, duration and level of disability). TMD pain represents the major cause of non-dental chronic pain in the orofacial region. It has a prevalence of approximately 10% [Citation2], while the prevalence of intra-articular non-painful TMJ disorders ranges from 20% to 40% [Citation2,Citation3].
On an individual basis, TMD can pose a negative effect on the quality of life [Citation4], comparable to that of individuals with acute dental pain [Citation5]. Acute pain has the potential risk to develop into a chronic pain condition. Pain, especially chronic, can cause increased levels of stress, pain spreading and associated mood and social disturbances, which are all examples of psychosocial factors related to TMD [Citation6]. Patients referred to specialized TMD/orofacial pain clinics are likely to present more severe and complex symptoms as compared to what is expected in a general dental practice. Referred patients are typically women [Citation7] and often with co-morbid symptoms, such as wide-spread pain and psychosocial impact [Citation8]. Early diagnosis along with appropriate interventions are regarded important in order to prevent chronicity as well as to reduce the negative impact of the condition [Citation9,Citation10]. Screening tools to guide the practitioner towards more accurate diagnostic procedures within the wide array of differential diagnostic procedures are required for early diagnosis.
Despite the benefits of early identification and treatment of patients with TMD pain, there is a known discrepancy between the estimated treatment need and traceable received treatment for these patients [Citation11–13]. This may partly be explained by described difficulties among clinicians in primary care to properly recognize and address TMD conditions [Citation14,Citation15]. Recently, the TMD pain screener was introduced and showed excellent sensitivity and specificity for detecting TMD pain [Citation16]. Ahead of the publication of the TMD pain screener, three screening questions (3Q/TMD) were introduced during 2010, in large parts of the primary and secondary dental health system in Sweden for the identification of patients with a potential TMD [Citation17]. Even though the reference was first published in 2016, the publication included data from 2010 and onwards. In addition to the areas covered by the TMD pain screener, the 3Q/TMD also aims to incorporate a selection of functional aspects of TMD. Recently, the 3Q/TMD were shown to be valid and suitable for screening purposes in primary dental health care in order to detect adult patients in the general population, who would benefit from a further diagnostic TMD examination [Citation18].
Patients referred to secondary specialized TMD/orofacial pain clinics usually present with more complex complaints, including neuropathic pain, atypical odontalgia and chronic dental pain. These referred patients will have chronic complaints more prevalently in comparison to a patient population in primary dental care. In addition, they more often present with comorbid symptoms, such as neck pain, headaches, widespread pain and psychosocial distress [Citation19]. In secondary care, screening tools may be used to select which differential diagnostic procedures should be applied to evaluate the full spectrum of the patients’ complaints. Since the diagnostic accuracy of a test may be influenced by the type of population under study [Citation20–22], the accuracy of the 3Q/TMD when applied in secondary care might differ from that shown in the general population. Therefore, the aim of this study was to evaluate the diagnostic accuracy of the 3Q/TMD among adult patients referred to a specialized TMD/orofacial pain clinic.
Materials and methods
Participants
The study design was a retrospective medical file study from patients referred to the Orofacial Pain and Dysfunction (OPD) clinic of the Academic Centre for Dentistry Amsterdam, the Netherlands. Consecutive patients referred between 17 September 2014, until 2 May 2016, who fulfilled the inclusion criteria were included in the sample. Inclusion criteria were: at least 18 years of age, referred for a TMD complaint, complete intake examination and written informed consent by the patient to grant the researchers the anonymous use of their clinical data. The study sample consisted of 449 adults (72% female), with a mean age of 44 years (SD = 14.2 years; range = 18–76 years). This study was considered by the Ethical Committee of ACTA not to fall under the provisions of the Medical Research Involving Human Subjects Act and medical ethical approval was granted (ref no 2017006).
Questionnaire
Preceding the intake visit, as part of the usual care, all patients received a questionnaire regarding their general and oral health, physical complaints and psychosocial factors. This questionnaire also included the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) Symptom Questionnaire [Citation23] and the 3Q/TMD screening tool [Citation17]:
Q1. Do you have pain in your temple, face, jaw, or jaw joint once a week or more? Q2. Do you have pain once a week or more when you open your mouth or chew? Q3. Does your jaw lock or become stuck once a week or more?
Individuals with an affirmative answer to at least one of the 3Q/TMD were classified as 3Q-positives, whereas individuals with negative answers to all three questions were classified as 3Q-negatives.
Physical examination
At the intake visit, all patients underwent a standardized clinical examination according to the DC/TMD protocol [Citation23]. The intake examination was performed as part of the usual care by one of 10 well-trained dentists from the OPD clinic. The dentists were calibrated annually to perform the standardized DC/TMD clinical examination. The calibration was supervised by a dentist previously trained and calibrated in the DC/TMD clinical examination by an official DC/TMD Training and Calibration Centre according to the DC/TMD Training and Calibration Guidelines [Citation24].
Reference standard
The DC/TMD was used as reference standard to compare the outcomes of the 3Q/TMD with. The DC/TMD classification has shown high sensitivity and specificity for the most common pain-related TMD diagnoses and some intra-articular disorders [Citation23]. The DC/TMD consists of two axes – axis I for assessment of a diagnosis based on signs and symptoms, and axis II for assessment of psychosocial factors of importance for prognosis and treatment planning.
As a reference standard to compare the outcomes of the 3Q/TMD with, the various DC/TMD diagnoses were grouped into two reference categories: (1) Pain-related TMD, including patients with myalgia and/or arthralgia, and (2) Intra-articular TMD, including patients with disc displacement with reduction with intermittent locking, disc displacement without reduction with limited opening, disc displacement without reduction without limited opening, and/or subluxation.
The 3Q/TMD was constructed to capture symptoms with an expected major influence on individuals’ physical functioning, which may be associated with treatment need. TMJ sounds without pain or limitation/locking of jaw movement were regarded symptoms of minor significance for the individual [Citation22] and therefore not incorporated as part of the reference standard.
Statistical analysis
Frequencies for the different DC/TMD diagnoses and affirmative answers to the 3Q/TMD are presented descriptively. The sensitivities and specificities of the 3Q/TMD pain questions (Q1, Q2) were calculated with the pain-related TMD as reference standard. Sensitivity and specificity of the screening question for function-related TMD (Q3) was calculated in relation to the category of intra-articular TMD as the reference standard. Combinations of 3Q/TMD questions (at least one positive, two or more positives, and all three positive) were evaluated in relation to the reference standard (i.e. either pain-related TMD or intra-articular TMD). The estimated prevalence of a TMD-pain diagnosis for a specialized clinic was set at 50% [Citation25]; this was also the case for the intra-articular TMD [Citation7], the positive and negative predictive values (PPV and NPV) were calculated based on these estimates. Confidence intervals for sensitivity, specificity, and predictive values were calculated according to the Wilson score method [Citation26].
Positive and negative likelihood ratios (LR + and LR-), including 95% confidence intervals, were calculated as suggested by Simel and co-workers [Citation27]. The related post-test probabilities were also provided (post-test probability = prevalence*LR/(1-prevalence + prevalence*LR)). The statistical calculations were conducted with SPSS version 24, and a p value <.05 was considered statistically significant.
Results
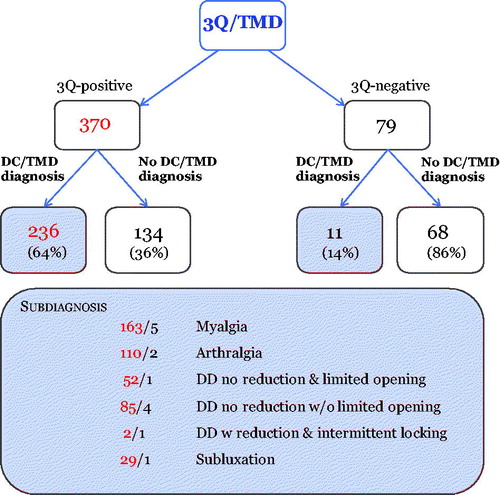
The prevalence of TMD diagnoses (either pain-related or intra-articular) was 55% (n = 247) (). In total, 44% (n = 196) qualified for any TMD-pain diagnosis, with myalgia being the most prevalent DC/TMD diagnosis (). The prevalence of DC/TMD diagnoses not included in the reference standard, viz., disc displacement with reduction and degenerative joint disorder, was 71% and 37% among 3Q-positives compared to 27% and 5% among 3Q-negatives, respectively.
Table 1. DC/TMD diagnoses in the study sample (n = 449 patients).
In total, 64% of the 3Q-positives and 14% of the 3Q-negatives qualified for at least one of the DC/TMD diagnoses used as reference standard ().
Figure 1. The distribution of diagnoses used in the analysis among 3Q-positives and 3Q-negatives based on answers to the 3Q/TMD (disc displacement (DD), DD with reduction, and degenerative joint disorder excluded).
The frequencies of affirmative answers are provided in . In total, 82% of the patients answered affirmatively to at least one of the 3Q/TMD. There was a large overlap between affirmative answers to the separate screening questions of the 3Q/TMD ().
Figure 2. Covariance of affirmative answers to the separate 3Q/TMD questions; weekly pain from the jaw, face, and temple region in rest (Q1) and on function (Q2), and weekly catching and/or locking of the jaw (Q3).
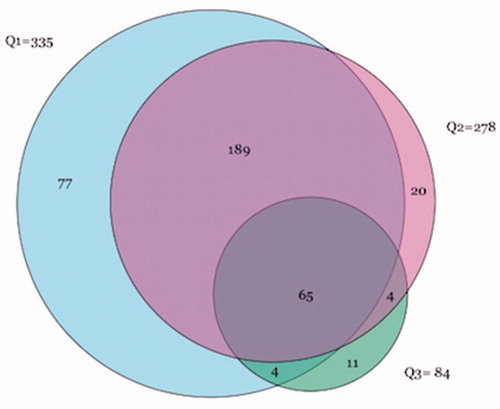
Table 2. Frequencies (n = 449) and sensitivities, specificities, likelihood ratios, positive and negative predictive values, and post-test probabilities (PTP) for Q1 and Q2 in relation to DC/TMD pain, for Q3 in relation to a subgroup of intra-articular DC/TMD diagnosis; and for one or more affirmatives in relation to any DC/TMD diagnosis used in the analysis.
For the two questions related to pain, the sensitivities were high (0.81–0.96). When calculated for this patient sample referred to a specialist clinic, the negative predictive values were 0.76-0.89 for the questions on pain, separately or in combinations. The corresponding positive predictive value was highest for a TMD-pain diagnosis when both Q1 and Q2 were positive (0.69). The highest positive likelihood ratio was associated with both Q1 and Q2 positive (2.16; 1.82–2.57). In contrast, the sensitivity for Q3 was low (0.48), whereas the positive predictive value and post-test probability was high (0.92, 0.92, respectively). The option of ‘at least one affirmative answer’ of the three screening questions was related to the highest sensitivity and negative predictive value for any TMD (either pain-related or intra-articular) (0.96;0.90).
Discussion
The main findings from this specialist clinic patient sample are that the vast majority of patients responded affirmatively to one or more of the three screening questions. Furthermore, the two screening questions on pain (Q1 and Q2) are strongly associated with a pain-related TMD diagnosis, as illustrated by the high sensitivity. However, the lower specificity illustrates that also individuals without a TMD complaint answer affirmatively to the two questions on pain. For the functional screening question (Q3), the sensitivity was low, although the specificity was high (0.96). In other words, the question is usually answered negatively in absence of an intra-articular DC/TMD diagnosis. Yet, in case of a positive answer, still not many patients receive an intra-articular TMD diagnosis with expected major influence on the individuals’ physical functioning.
While sensitivity and specificity are independent of the prevalence of a condition, positive and negative predictive values are related to the prevalence of the condition in the population of interest. For all diagnostic tests, including screening tests, the diagnostic accuracy should be expressed in a way that can guide clinicians in their clinical decision-making for the individual patient. For such a purpose, the positive and negative predictive values are useful measures that describe the individual risk of having a condition, given a positive or negative test result, respectively [Citation28]. The individual risk of having a diagnosis could also be reported by post-test probabilities that will express the chance that the patient will have the condition, after the test has been performed [Citation29]. For the recognition of TMD, acceptable levels of sensitivity and specificity have been proposed to be at least 70% and 95%, respectively [Citation30]. For specialized clinics, the a priori estimated prevalence for TMD was 50% [Citation25], which was well in line with the observed prevalence in the study sample of 44%. With the above recommendations, and a 50% estimate of the prevalence of TMD in specialized clinics, a positive predictive value of 93% and a negative predictive value of 76% is generated. For screening purposes within a specialized clinic, a high positive predictive value is most important, since this will rule in individuals with a possible disorder. Further diagnostics can then be applied to confirm the initial screening diagnosis. In this sample, Q3 and ‘all three questions answered affirmatively’ (as indicative for either pain-related or intra-articular TMD) met the suggested cut-off.
Nowadays, the 3Q/TMD is widely implemented in the Swedish system, so information on its validity is important for clinicians using the screener. Yet, in the meantime, a partly comparable screening questionnaire, the TMD pain screener (Citation16), has been introduced. The TMD pain screener has shown higher sensitivity and specificity (0.99 and 0.97, respectively) (Citation16) for TMD pain as compared to the 3Q/TMD. However, the 3Q/TMD uniquely incorporates an item to screen for a selection of functional disorders. These conditions represent a group of TMD disorders, like disc displacements without reduction with limited mouth opening, that also need to be better recognized in primary dental care. Future research could explore the possibilities of combining the outcomes of both screening tools to reach the most valid and comprehensive questionnaire covering all relevant domains of TMD that should be recognized in primary care.
Pain-related TMD
On an individual basis, when translated into positive and negative predictive values, the results show that according to the negative predictive value, the two pain-related questions (Q1 or Q2) are useful to screen for the absence of TMD pain in a specialist clinic setting. This is also reflected in the negative likelihood ratio post-test probability after a negative test outcome; when applied in a specialized clinical sample, the probability of an individual to qualify for a DC/TMD pain diagnosis decreases from 50% (i.e. the pre-test probability based on the estimated prevalence) to below 11% after a negative test outcome. In case of a positive answer, the likelihood of the individual to suffer from TMD pain has increased, especially when both Q1 and Q2 are positive (i.e. from 50% to 69%), and further procedures for a definite diagnosis of a pain-related TMD are warranted. Yet, not all patients who had an affirmative answer to the pain questions received a DC/TMD diagnosis. An obvious reason is that within a population that is referred to a secondary care setting for orofacial pain complaints, also patients with other causes of pain are included (such as neuropathic pain or atypical odontalgia). Since TMD pain is the most frequent cause for chronic orofacial pain, in the case of a positive screening outcome in a specialist clinic, the following examination should first carefully examine the masticatory system. In case that examination does not verify the patient’s complaint, the diagnostic examination should be expanded towards other orofacial pain disorders, such as neuropathic pain.
The sensitivity of the 3Q/TMD of the two pain questions (Q1 and Q2) was comparable to that of the TMD pain screener. However, the specificity of the 3Q/TMD in a specialist clinic sample was lower. Probably, this relates to the different choice of study population. In the present study, all participants were patients referred with complaints in the orofacial area, while in the paper on the TMD pain screener, the sample used to calculate specificity consisted of healthy controls. As illustrated before [Citation21], the estimation of specificity of a diagnostic tool usually drops when outcomes from healthy controls are compared to those of patient controls (i.e. participants with complaints in the same region, other than the disease of interest).
Function-related TMD
For the outcomes of the screening question for function-related TMD (Q3), the specificity was high, and sensitivity was low. Individuals without an intra-articular diagnosis seldom reported signs of locking (Q3, high specificity). However, individuals with a disc displacement with intermittent locking or limited opening, or with a subluxation of the TMJ, were often not identified by the screening question (Q3, low sensitivity). One reason for the lower sensitivity of Q3 might be related to the reference standard itself. The sensitivity of some intra-articular DC/TMD diagnoses has been reported to be low [Citation23,Citation31] and instead, imaging, such as magnetic resonance imaging, is suggested to be the appropriate reference standard [Citation23]. As a consequence, in the present study, an individual with signs and symptoms of a function-related TMD, such as disc displacement with reduction and intermittent locking, might screen positive on Q3 but might not receive a DC/TMD intra-articular diagnosis. In addition, this may reflect the possibility that for individuals with a true intra-articular TMD, the Q3 is not interpreted by patients as dentists intended when the question was constructed. Still, the high specificity combined with the estimated prevalence of 50% for these disturbances in a specialized clinic, show that Q3 is useful to screen for an intra-articular TMD. The post-test probabilities show that after a positive test outcome, the probability of an individual to qualify from an intra-articular TMD increases from 50% to 92%.
The effects of samples on outcome
The outcome of diagnostic accuracy will differ, depending on the prevalence of the condition in the examined population and will therefore differ for patients with TMD in the general population compared to a specialized clinic with a higher prevalence of the disorder of interest (Citation20).
The 3Q/TMD has recently been validated in relation to the DC/TMD in adults from a general population [Citation18]. In the general population, the separate questions as well as combinations of questions showed high negative predictive values. The highest positive predictive value was related to a positive outcome on both Q1 and Q2. In the previous paper, based on the sensitivity and specificity found in the general population, data were extrapolated to estimate the diagnostic accuracy of the 3Q/TMD in a secondary care setting (with higher prevalence of TMD) [Citation16]. The predictive values calculated in the current study are however quite different from these previously estimated values. This confirms the idea that differences in study populations significantly impact the outcomes of diagnostic accuracy [Citation20,Citation21,Citation32]. The results also reinforce the importance of taking the relevant prevalence into account when determining diagnostic accuracy.
Taken together, screening questionnaires for TMD seem to be highly needed in primary care, since many patients with TMD-pain complaints are not adequately recognized. The 3Q/TMD is shown efficient to rule out a TMD within the general population, and individuals with positive 3Q/TMD results should be referred for further diagnostic examination [Citation18]. In more specialized pain clinics, the 3Q/TMD seems useful as a tool to direct clinicians in the differential diagnostic phase towards tailored further examinations.
Strengths and limitations
The diagnostic accuracy of the 3Q/TMD in this specialist setting was established in relation to the DC/TMD. The DC/TMD is at present recommended for both research and clinical purposes, and thus constitutes a valid reference standard in relation to the aim of this study. However, the psychometric properties of the 3Q/TMD are not evaluated, which may be regarded a limitation of the screening tool. On the other hand, the 3Q/TMD is not intended to be a psychometric tool for an optimal description of the construct TMD. It is merely intended as a screening tool for the clinician not to oversee TMD, and an incentive to carry out further examination to diagnose a possible TMD.
As recommended, the 3Q/TMD was always filled out by the patient before the structured clinical examination. The 3Q/TMD was part of the intake questionnaire, starting with the Symptom Questionnaire, while the 3Q/TMD are answered at the end. Since the screening questions were answered after completing the Symptom Questionnaire, it is possible that the validity of the 3Q/TMD was inflated by the previously asked questions. On the other hand, the length of the questionnaire itself may instead deflate the validity.
The present study population has shown an expected high proportion of TMD diagnoses (44% had a pain-related TMD and 33% showed an intra-articular TMD) as well as a high variety of other chronic pain conditions. The data for this study were extracted from routine patient files and based on this, we evaluated the diagnostic accuracy. The test-retest reliability of the screening tool in adults has not been established yet. Further research is needed to evaluate the reproducibility of the 3Q/TMD. Due to the selection of patients from a specialized clinic sample, where most patients will have symptoms, the number of 3Q-negative individuals was rather small. In order to increase the control group, patients from other specialized clinics from ACTA could have been included. This, however, would have interfered with the usual care as provided in the other specialized clinics, as a standardized DC/TMD examination is not part of their routine. Furthermore, the composition of patient groups within different specialist clinics can vary widely, depending on the focus in the clinic, which will affect the external validity of the results. Taken together, the results may be generalized to comparable specialist clinic settings, where mainly patients with orofacial pain and dysfunction are referred to.
Conclusions
Within the limitations of this study, in a specialized pain clinic, the two pain screening questions are positive in most patients with a pain-related TMD. Therefore, in case of a positive response, further diagnostic procedures for TMD pain are warranted. The high negative predictive values of the two questions on pain (Q1 and Q2) indicate that in patients with negative responses, the presence of pain-related TMD is unlikely, and differential diagnostic procedures should include a wider array of possibilities at an early stage. For the functional screening question (Q3), a positive response is indicative for an intra-articular DC/TMD diagnoses, while in case of a negative outcome, an intra-articular TMD might still be present.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
References
- Okeson JP. Management of Temporomandibular Disorders and Occlusion. 7th ed: Mosby; 2013.
- LeResche L. Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors. Crit Rev Oral Biol Med. 1997;8:291–305.
- Huddleston Slater JJ, Lobbezoo F, Onland-Moret NC, et al. Anterior disc displacement with reduction and symptomatic hypermobility in the human temporomandibular joint: prevalence rates and risk factors in children and teenagers. J Orofac Pain. 2007;21:55–62.
- Dahlström L, Carlsson GE. Temporomandibular disorders and oral health-related quality of life. A systematic review. Acta Odontol Scand. 2010;68:80–85.
- Shueb SS, Nixdorf DR, John MT, et al. What is the impact of acute and chronic orofacial pain on quality of life? J Dent. 2015;43:1203–1210.
- Suvinen TI, Reade PC, Kemppainen P, et al. Review of aetiological concepts of temporomandibular pain disorders: towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain. 2005;9:613–633.
- Anastassaki A, Magnusson T. Patients referred to a specialist clinic because of suspected temporomandibular disorders: a survey of 3194 patients in respect of diagnoses, treatments, and treatment outcome. Acta Odontol Scand. 2004;62:183–192.
- Suvinen TI, Kemppainen P, Le Bell Y, et al. Assessment of Pain Drawings and Self-Reported Comorbid Pains as Part of the Biopsychosocial Profiling of Temporomandibular Disorder Pain Patients. J Oral Facial Pain Headache. 2016;30:287–295.
- Durham J, Steele J, Moufti MA, et al. Temporomandibular disorder patients' journey through care. Community Dent Oral Epidemiol. 2011;39:532–541.
- Macfarlane GJ. The epidemiology of chronic pain. Pain. 2016;157:2158–2159.
- Al-Jundi MA, John MT, Setz JM, et al. Meta-analysis of treatment need for temporomandibular disorders in adult nonpatients. J Orofac Pain. 2008;22:97–107.
- Wänman A, Wigren L. Need and demand for dental treatment. A comparison between an evaluation based on an epidemiologic study of 35-, 50-, and 65-year-olds and performed dental treatment of matched age groups. Acta Odontol Scand. 1995;53:318–324.
- Rollman A, Gorter RC, Visscher CM, et al. Why seek treatment for temporomandibular disorder pain complaints? A study based on semi-structured interviews. J Orofac Pain. 2013;27:227–234.
- Durham J, Exley C, Wassell R, et al. Management is a black art’– professional ideologies with respect to temporomandibular disorders. Br Dent J. 2007;202:E29.
- Lindfors E, Tegelberg A, Magnusson T, et al. Treatment of temporomandibular disorders - knowledge, attitudes and clinical experience among general practising dentists in Sweden. Acta Odontol Scand. 2016;74:460–465.
- Gonzalez YM, Schiffman E, Gordon SM, et al. Development of a brief and effective temporomandibular disorder pain screening questionnaire: reliability and validity. J Am Dent Assoc. 2011;142:1183–1191.
- Lövgren A, Haggman-Henrikson B, Visscher CM, et al. Temporomandibular pain and jaw dysfunction at different ages covering the lifespan-A population based study. Eur J Pain. 2016;20:532–540.
- Lövgren A, Visscher CM, Haggman-Henrikson B, et al. Validity of three screening questions (3Q/TMD) in relation to the DC/TMD. J Oral Rehabil. 2016;43:729–736.
- Velly A, List T, Lobbezoo F. Comorbid pain and psychological conditions in patients with orofacial pain. Orofacial pain: recent advances in assessment, management, and understanding of mechanisms: IASP Press; 2014.
- Levitt SR, McKinney MW. Appropriate use of predictive values in clinical decision making and evaluating diagnostic tests for TMD. J Orofac Pain. 1994;8:298–308.
- Visscher CM, Naeije M, De Laat A, et al. Diagnostic accuracy of temporomandibular disorder pain tests: a multicenter study. J Orofac Pain. 2009;23:108–114.
- Cohen JF, Korevaar DA, Altman DG, et al. STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ Open. 2016;6:e012799.
- Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Groupdagger. J Oral Facial Pain Headache. 2014;28:6–27.
- Vilanova LS, Garcia RC, List T, et al. Diagnostic criteria for temporomandibular disorders: self-instruction or formal training and calibration?. J Headache Pain. 2015;16:505.
- Manfredini D, Guarda-Nardini L, Winocur E, et al. Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:453–462.
- Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998;17:857–872.
- Simel DL, Samsa GP, Matchar DB. Likelihood ratios with confidence: sample size estimation for diagnostic test studies. J Clin Epidemiol. 1991;44:763–770.
- Mallett S, Halligan S, Thompson M, et al. Interpreting diagnostic accuracy studies for patient care. BMJ. 2012;345:e3999.
- Oakley C, Brunette DM. The use of diagnostic data in clinical dental practice. Dent Clin North Am. 2002;46:87–115.
- Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–355.
- Schiffman E, Ohrbach R. Executive summary of the Diagnostic Criteria for Temporomandibular Disorders for clinical and research applications. J Am Dent Assoc. 2016;147:438–445.
- Aleem IS, Jalal H, Aleem IS, et al. Clinical decision analysis: Incorporating the evidence with patient preferences. Patient Prefer Adherence. 2009;3:21–24.
