Abstract
Objective
In recent years, Molar Incisor Hypomineralization (MIH) has become a subject that concerns the Paediatric Dentistry Community. The aim of the present umbrella review was to analyse previously published systematic reviews (SRs) on MIH in children and adolescents.
Methods
Electronic database search was conducted (including PubMed, Embase, Scopus, Cochrane, Web of Science, and LILACS) until July 2020. Studies were included, if they were SR on MIH in children and adolescents. The methodological quality of SRs was judged by use of the MeaSurement Tool to Assess systematic Reviews 2. The primary outcomes included prevalence, aetiology, and clinical management of MIH. Data extraction and methodological quality assessment were performed.
Results
Eighteen systematic reviews were included for data extraction. Among these, two were focussing on prevalence, five addressed aetiology, one highlighted the mechanical and chemical characteristics of enamel in MIH, one underlined the association between MIH and dental caries, six addressed the treatment, and one focussed on hypomineralization of primary teeth as a predictor of MIH. The results showed a high worldwide prevalence of MIH and an unknown aetiology of MIH, but reporting that the aetiology is most likely multifactorial. Different treatment approaches used were desensitizing and remineralizing products, resin infiltration, fissure sealant, atraumatic restorative treatment, resin composite restoration, and stainless steel crown (SSC), but also extraction associated with orthodontic treatment of the permanent first molars (PFMs) was reported on. The AMSTAR criteria 2 was applied, where six studies were assessed as having critically low quality, two studies as having low quality, and nine studies as having moderate quality.
Conclusions
MIH is highly prevalent worldwide and has most likely a multifactorial aetiology. Different treatment approaches according to the degree of severity of lesion(s) are reported on. The quality of evidence produced by the available SRs was not favourable. More well-designed clinical trials and high standard systematic reviews are necessary to elucidate better MIH characteristics and treatment outcomes.
Introduction
Hypomineralization of tooth enamel was firstly reported on in the late 1970s, where several researchers described frequent congenital hypomineralization of the permanent first molars (PFMs) and incisors of the permanent dentition [Citation1–3]. Later in 2000 at the European Academy of Paediatric Dentistry (EAPD) Congress in Bergen, this condition was named as Molar-Incisor Hypomineralization (MIH) [Citation4].
MIH is defined as a qualitative developmental defect of enamel in children and adolescents, affecting at least one PFM with or without involvement of the incisors [Citation3,Citation5–14]. MIH is clinically characterized by more or less well-defined opacities that vary in size and can be discoloured from white to yellow-brownish [Citation5,Citation10,Citation11,Citation15].
The hypomineralized enamel is friable and has inferior mechanical properties as well as reduced modulus of elasticity when compared to sound enamel [Citation5,Citation8,Citation11,Citation13,Citation16]. Molecularly, MIH-affected enamel presents a high amount of proteins, like serum albumin, type I collagen among others, and it is suggested that the presence of these proteins inhibits the growth of hydroxyapatite crystals and enzymatic activity during enamel maturation, which results in a reduction of the mineral content of enamel in MIH cases [Citation8,Citation17]. As a consequence, hypomineralized enamel leads to post-eruptive breakdown and hypersensitivity, and it is prone to development of carious lesions and pain [Citation5,Citation7,Citation9,Citation13]. However, the full understanding of the aetiology of MIH is still not obtained [Citation9,Citation10,Citation12–14].
From an epidemiologic standpoint, MIH is the most frequent enamel defect. However, the prevalence varies significantly in studies available in the literature. A study based on Danish children showed that the prevalence of demarcated opacities, eventually complicated by loss of tooth substance in any PFM was 37.3% (95% confidence interval (95% CI) 33.6 ± 41.0%) and 6.3% (95% CI 4.7 ± 8.5%), respectively [Citation18]. On the other hand, a study on Brazilian children displayed a prevalence of 40.2%, where the number of affected incisors increased with increasing number of affected molars [Citation19]. Latest studies presented a prevalence of 3 to 22% in Europe [Citation8,Citation18], and 2 to 40% worldwide [Citation9,Citation13,Citation19].
Due to pain, fragile enamel and increased treatment need at an early point of time in life, MIH represents a clinical challenge. Due to a demand for more information and understanding of the condition, a large number of systematic reviews have been published concerning MIH in the last decade, and therefore an umbrella review encompassing all available information at present time would be of great interest.
This umbrella review aimed to summarize the existing systematic reviews on MIH in children and adolescents, with a particular focus on diagnosis, prevention, clinical management and quality of evidence.
Methods
The present systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [Citation20], expanded with the guide on systematic reviews of systematic reviews [Citation21]. The review protocol was approved a priori by all authors.
Eligibility criteria
The inclusion criteria were as follows: A paper (1) defined as a systematic review or a meta-analysis; (2) retrieving data from human studies; (3) investigating clinical characteristics of MIH in children and adolescents, in either dentition and/or in relation to the use of clinical procedures. No restrictions to publication year or language were applied. Grey literature was searched through appropriate databases and registers (opensigle.inist.fr, https://www.ntis.gov/, https://www.apa.org/pubs/databases/psycextra).
PECO
Population (P) – Children and Adolescents with Molar-Incisor Hypomineralization
Exposure (E) – Prevalence, prevention, clinical management and aesthetics
Comparison (C) – Prevention, treatment of hypersensitivity and/or treatment of affected teeth (through restorative, endodontic, prosthetic, surgical or orthodontic approaches)
Outcome (O) – Diagnosis and a variety of dental treatment types
Information sources search
Electronic data search was performed in seven electronic databases that cover life sciences, health sciences, and physical sciences: PubMed-Medline, Scopus, Cochrane Database of Systematic Reviews, Scielo (Scientific Electronic Library Online), EMBASE (The Excerpta Medica Database), LILACS (Latin-American scientific literature in health sciences), and TRIP (Turning Research Into Practise). We merged keywords and subject headings in accordance with the thesaurus of each database and applied exploded subject headings, so the final search was Molar-Incisor Hypomineralization, Developmental Dental Defects and Enamel Defect. The search was based on the reference of the systematic reviews and meta-analyses [Citation20,Citation21], and since the criterion for the diagnosis of MIH was not published before 2003, the search covered the period from September 2003 to August 2020.
Study selection
Two researchers (LL and JB) independently screened titles and abstracts. The agreement between the reviewers was assessed by Kappa statistics. Any paper classified as potentially eligible by either reviewer was ordered as a full text and independently screened by the reviewers. All disagreements were resolved through discussion with a third reviewer.
Data extraction process and data items
Two researchers (LL and JB) extracted independently the following data from the SRs: Authors, objective/focussed question, databases searched, number of studies included, type of studies included, main results and main conclusions. All disagreements were resolved through discussion with a third reviewer (VM).
Risk of bias assessment
Two researchers employed the MeaSurement Tool to Assess Systematic Reviews (AMSTAR 2) to determine the methodological quality of the included reviews [Citation22]. The agreement between the reviewers was assessed by Kappa statistics. AMSTAR 2 is a comprehensive 16-item tool that rates the overall confidence of the results of the review. According to the AMSTAR guidelines, the quality of the systematic reviews was considered as follows: High means ‘Zero or one non-critical weakness’; Moderate means ‘More than one non-critical weakness’; Low means ‘One critical flaw with or without non-critical weaknesses’; and Critically low means ‘More than one critical flaw with or without non-critical weaknesses’. The estimation of the AMSTAR quality rate for each study was calculated through the AMSTAR 2 online tool (https://amstar.ca/Amstar_Checklist.php).
Results
Study selection
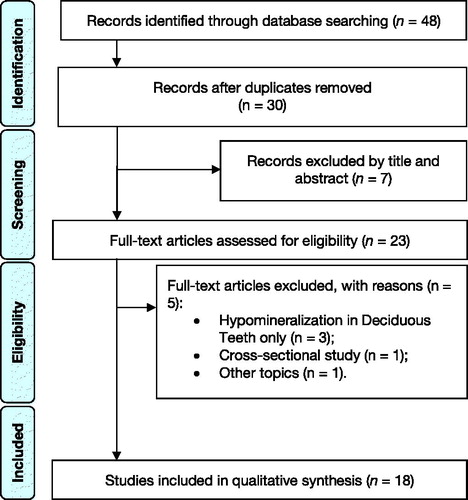
Electronic searches retrieved a total of 48 titles through the database searching. After manual assessment of title/abstract and removal of duplicates, 23 potentially eligible full-texts were screened. Full-text screening excluded five studies with reasons (), resulting in 18 systematic reviews that fulfilled the inclusion criteria. Inter-examiner reliability at the full-text screening was recorded as high (kappa score = 1.00).
Study characteristics
In total, 18 systematic reviews were included in the present umbrella review ().
Table 1. Characteristics of the included systematic reviews.
Most systematic reviews covered a defined timeframe, however, four did not mention such information [Citation4,Citation11,Citation14,Citation23].
Regarding language restriction, two systematics reviews failed to report this characteristic [Citation6,Citation23], seven had language restrictions [Citation4,Citation5,Citation7,Citation12,Citation14,Citation15,Citation24], and the remaining had no language restrictions [Citation3,Citation10,Citation11,Citation13,Citation17,Citation25,Citation26].
There were even two systematic reviews that mentioned no language restriction were set, and studies in other languages than English or German were translated by native speakers [Citation8,Citation9].
Because MIH is a qualitative developmental defect of enamel, multiple sub-topics in the systematic reviews were addressed. For example, the included systematic reviews addressed: aetiology [Citation3,Citation6,Citation10,Citation14,Citation17,Citation23], prevalence [Citation4,Citation13,Citation24], diagnosis [Citation4], mechanical and chemical characteristic of enamel in MIH [Citation9], the association between MIH and dental caries [Citation5], and treatment [Citation7,Citation8,Citation12,Citation25,Citation26]. A particular study aimed to review, if hypomineralization was a predictor of MIH [Citation15].
Risk of bias
Good inter-examiner reliability at the risk of bias screening was recorded (kappa score = 0.91; 95% confidence interval: 0.89–0.92). None of the included systematic reviews satisfied entirely the AMSTAR 2 Criteria (). Overall, nine presented moderate quality [Citation6–8,Citation10,Citation11,Citation13–15,Citation25] and seven were assessed as having critically low quality [Citation4,Citation5,Citation9,Citation12,Citation23,Citation24,Citation26].
Table 2. Risk of bias of systematic reviews (AMSTAR 2 tool).
Synthesis of results
Prevalence of MIH
Due to the fact that MIH was named at the EAPD meeting in 2003, multiple examination criteria were found among papers reporting the prevalence of MIH [Citation4]. Consequently, studies applying the EAPD definition were found to report higher prevalence of MIH (14.5%) than those using other case definitions (10.2%) [Citation13].
Overall, MIH is currently estimated to have a prevalence of 14.2% [Citation24] and to affect 17.5 million children and adolescents worldwide (ranging from 15.8 to 19.4 million) [Citation13], and this prevalence does not differ between females and males (OR: 0.92; 95% confidence interval: 0.81–1.04) [Citation13]. In terms of cases with need for care (i.e. with symptoms or post-eruptive breakdown), the prevalence was estimated to 27.4% [Citation13].
In Europe, two nation-wide studies carried out in Germany and Bulgaria [Citation4] reported a prevalence close to 2.4%, while in the city of Leeds (in the United Kingdom) a prevalence of 40% was reported [Citation4]. In South America, a study carried out in Rio de Janeiro, Brazil reported 40.2% [Citation19]. In Africa, a Kenyan study reported 13.7% of MIH cases, while in Sydney, Australia the MIH prevalence was reported to be 44% [Citation4]. The prevalence of MIH was found to be elevated in high-income countries from Southeast Asia, East Asia, and Oceania. At country/geographic region level, India, China and the United States had the highest prevalence rates [Citation13].
Aetiology of MIH
Six systematic reviews addressed the aetiology of MIH [Citation3,Citation6,Citation10,Citation14,Citation17,Citation23], among which three computed meta-analyses where several parameters were evaluated. Overall, multiple aetiological factors associated with MIH were reported on and can be divided according to pre-, peri- and postnatal periods.
Regarding the prenatal period, the most striking factor was the existence of systemic conditions. For example, medical problems were more prevalent in mothers of children with MIH in comparison to those mothers whose children did not have MIH [Citation23]. Urinary infection during the last trimester of pregnancy was associated with higher risk of MIH in one study [Citation23], however, in two other studies no association was found in relation to specific diseases [Citation10,Citation23]. Furthermore, the role of maternal systemic conditions during pregnancy is inconclusive, as a review reported no association [Citation14], and in another paper maternal illness was associated with 40% higher odds of having MIH [Citation10]. Furthermore, maternal smoking and alcohol intake during pregnancy had no significant association with MIH, but maternal stress was positively associated with MIH [Citation10,Citation14].
In the perinatal period (covering caesarean delivery, prolonged delivery, premature birth and twinning), studies were also contradictory with reports of as well positive [Citation23] as negative associations [Citation10,Citation23]. Hypoxia is common during birth (such as prematurity respiratory stress or traumatic and prolonged birth) and was related to MIH due to the effect of oxygen insufficiency on the activity of ameloblasts [Citation23]. Another condition reported on was hypocalcaemia, given that MIH is suggested to occur in cases of low calcium levels that suggest possible impairment of the ameloblasts’ calcium metabolism [Citation23]. Hypocalcaemia can occur in any of the periods (pre-, peri- or postnatal) and is also associated with multiple conditions, like maternal diabetes, vitamin D deficiency during the prenatal and/or perinatal period and prematurity [Citation23]. Concerning the association between MIH and preterm birth (PB) and low birth weight (LBW), respectively, the results were once again inconsistent. MIH was significantly associated with PB in both the primary and permanent dentitions [Citation3,Citation6]. Considering LBW, two meta-analyses were contradictory, with one showing no association (OR = 1.52; 95% CI 0.83‐2.79) [Citation10], and another reporting that LBW neonates were about three times more likely to have MIH (OR = 3.25, 95%CI: 2.28–4.62) [Citation3]. Lastly, the association of MIH with preterm (PT), LBW, caesarean delivery and birth complications was reported to be low [Citation14].
In the postnatal period, long duration of breastfeeding, childhood illnesses and early childhood medication were in one or another way linked to MIH. Long duration of breastfeeding had no association with MIH [Citation10,Citation14], as well as one review found contradictory information about the levels of pollutants in human milk [Citation23 ].
Concerning reports on early childhood illness, several disorders were taken into consideration and found to have a positive association with MIH, for example fever, respiratory diseases (asthma, pneumonia), otitis, adenoiditis, urinary tract infection, chickenpox [Citation10,Citation14,Citation23]. MIH was significantly more common among children for whom amoxicillin was the only antibiotic medicament they had received, but not among children who were exposed to mixed use of antibiotics, including amoxicillin [Citation10,Citation14,Citation23]. Nevertheless, it was also mentioned in the study by Silva et al. [Citation14] that no association between amoxicillin and MIH was found, and even antibiotics exposure was not associated with MIH (OR = 1.28; 95% CI 0.99‐1.65) [Citation10]. On the other hand, other types of antibiotics, like erythromycin and macrolides, were found to be more commonly used in children with MIH [Citation23]. Concerning anti-neoplastic treatment and anti-epileptic drugs, these were also reported as being associated with an increased risk of developing numerous teeth with diffuse opacities and even enamel hypoplasia [Citation17]. In relation to asthma medication as corticosteroids and bronchodilators, an association with enamel defects has been reported [Citation17]. Yet, other authors found no association with anti-asthma medication, although there could be an association with a subset of cases involving post-eruptive breakdown [Citation14].
Clinical management of MIH
Overall, MIH causes concern to children and their parents, for example related to aesthetics, enamel loss, increased risk of development of caries lesions, hypersensitivity and possibility of tooth loss, especially in severe cases [Citation5,Citation12]. Clinical management of MIH is dependent on the disease stage (mild, moderate and/or severe) [Citation12], and the treatment need can be comprehensive.
Concerning remineralization of the affected enamel and reduction of the sensitivity, fluoride varnishes may be relevant to use. However, often such an approach is followed also by a need for the use of sealing or restoration [Citation7,Citation12]. In MIH cases, the effect of casein phospho-peptides and amorphous calcium phosphate (CPP-ACP) pastes has shown no significant differences with or without added fluoride when used in MIH cases [Citation7,Citation12,Citation26].
Fissure sealants may be beneficial in the handling of mild defects where sensitivity and enamel breakdown are not prominent [Citation12]. Although some types of fissure sealants often require the need for re-treatment [Citation12], they present higher retention with fifth generation adhesives (i.e. a two-step etch-and-rinse adhesive) [Citation11]. Some papers also reported on the use of glass ionomer cements were also referred to as fissure sealants as well as temporary restorations in provisional situations, in order to decrease sensitivity and minimize further breakdown of enamel [Citation8,Citation12]. Furthermore, amalgam restorations were also explored and had relatively low success rates [Citation8,Citation12]. Restorative approaches with, e.g. use of resin composite fillings were assessed in several clinical trials, where the effects of deproteinization and various types of adhesives also were evaluated [Citation7,Citation11,Citation12].
Adhesion procedures are challenging in MIH lesions. In the included reviews, there were no consensus regarding the best adhesive materials to be used and/or protocols on how to apply it in MIH teeth [Citation11], although the use of several adhesives were studied, such as ClearfilTM SE Bond, OptiBondTM FL, 3 MTM Single Bond, AdperTM, ScotchbondTM Multi-Purpose and ScotchbondTM Universal) [Citation11]. Regarding deproteinization, the results were contradictory, with some studies showing that application of NaOCl after etching significantly increased bond strength to MIH-affected enamel, and other studies reporting that NaOCl pre-treatment on the affected enamel did not enhance enamel bonding, but caused less pre-test failures (NaOCl 23.6 MPa vs. MIH-affected enamel 21.3 MPa, and sound enamel 31.2 MPa) [Citation11].
Stainless steel crowns (SSCs) were considered reliable to prevent further enamel loss, to control the hypersensitivity, to establish correctly interproximal and proper occlusal contacts with a low cost and little working time required [Citation8,Citation12]. In severe MIH cases, extraction can be a clinical option; however, in such cases we should consider the child’s age, pulp involvement, and take orthodontic considerations into account [Citation8,Citation12].
As anterior teeth may be affected by MIH, manifesting as white or yellow-brown defects, there may be aesthetic challenges to bear in mind. Different approaches have been mentioned [Citation12], namely etch-bleach-seal technique, bleaching with 10% to 38% carbamide peroxide in permanent teeth only, enamel reduction followed by the use of opaque resins and direct composite veneering, micro-abrasion using an abrasive paste and 18% hydrochloric, or polishing with pumice and etching with 37.5% phosphoric acid [Citation7,Citation12]. Very recently, resin infiltration has been discussed as a possibility for restoration of decalcified enamel, since it masks the enamel whitish discolorations. However, there is no agreement because of an erratic or poor penetration [Citation7,Citation11,Citation25].
Discussion
This umbrella review poignantly synthesizes the evidence accrued so far from studies on MIH. The methodological quality of the included SRs ranged from moderate to critically low, and therefore current evidence is far from being of high confidence. The main conclusion to retain relies on the importance of prevention, since the available evidence on prevalence, aetiology, and clinical management is still very heterogeneous.
The present umbrella review is highly relevant given the relatively high number of systematic reviews published in the last few years, indicating the importance and relevance of this topic. Also, this is the first umbrella review on MIH compiling evidence from multiple reviews about MIH, a recent clinical entity, as the term ‘Molar Incisor Hypomineralization’ was defined in 2000 established to the European Academy Paediatric Dentistry (EAPD) definition [Citation3–5,Citation10,Citation13,Citation15,Citation17,Citation27].
Strengths and limitations
Our umbrella review has several strengths. It provides a comprehensive overview of the available systematic reviews published regarding MIH using a transparent methodology.
It should be considered, when interpreting the results that the individual studies included in each of the present systematic review were not explored. Thus, the conclusions lean on the interpretation of the systematic review’s authors. Another point worth mentioning is the existence of two PROSPERO registers that are in an ongoing status, but not published [Citation28,Citation29].
It should be noted that at the meeting in Athens, Greece in 2003, 8 years of age was mentioned as the best age for the performance of an examination of MIH. In this sense, not all studies are based on the same clinical parameters and criteria using the terminology of MIH defined by EAPD [Citation3–5,Citation10,Citation13,Citation15,Citation17].
MIH prevalence
Referring to the prevalence and aetiology of MIH, there were two systematic reviews, from which it was possible to verify the importance of using appropriate case definitions of MIH. The case definition of MIH was significantly associated with the prevalence, thus studies using the EAPD case definition presented higher prevalence values compared to other studies, where other types of definitions were used [Citation4,Citation13,Citation17].
The MIH prevalence varies significantly. Nevertheless, it was considered that the proportion of cases in need of care was estimated to 27.4% (95% CI: 23.5–31.7%), or nearly 5 million new MIH cases every year that need dental treatment, and 240 million existing cases, among which some cases were not treated, particularly in poorer countries [Citation13]. Another review estimated a global prevalence of 14.2% (95% CI: 12.6–15.8%) [Citation24]. Overall, South America was the continent with the highest prevalence (18.0%) and Africa the lowest (10.9%).
After all, comparing results between different studies is difficult, mainly because of the study material selected and different methodologies used. This differed at several points in the studies, such as sample size, age of observation, calibration of examiners, the way of observing and collecting data, among others parameters [Citation4].
MIH aetiology
MIH is a qualitative defect of enamel with affection of the mineralization and maturation of the enamel of the PFMs and incisors. Most of the published papers reported on are case–control studies, retrospective cohort studies, and observational studies are of low quality [Citation3,Citation10,Citation14,Citation17]. Moreover, the methodology of the studies differed in several ways, like the type of medication focussed on, the age at which the medication was administered, and the history of drugs used among other events [Citation17]. Another important problem of MIH aetiology is to determine, for example, if the enamel defect is caused by the illness itself, the fever caused by the illness, or the medication [Citation10,Citation14,Citation17,Citation23]. Regardless of the association between systemic exposures, including other relevant factors (e.g. preterm birth, low birth weight, and others) and the occurrence of MIH, the aetiology is not yet fully understood. In addition, it is likely that MIH is caused by many factors acting simultaneously. For example, in a very recent study, however not a systematic review, the results were adjusted for potential confounding (use of antibiotics and various birth outcomes), and no association was found between the use of asthma drugs and MIH [Citation30].
Conclusively, more high-quality studies are needed within this important area of research. For example, one recent clinical investigation of enamel defects in off-springs of mothers randomized to a high-dose of Vitamin D supplementation in pregnant mothers was found to reduce the risk of having enamel defects [Citation31]. This study was, however, most likely due to a recent publication date or not using the terminology of MIH, but enamel defects, not included in any of the systematic reviews on which this umbrella review relies.
MIH clinical management
MIH is a hard tissue pathology that requires constant control and requires a high number of dental treatments, especially in severe cases, given the fact that there is a positive association with the development of dental caries, possible post-eruptive breakdown, which may lead to pulpal inflammation, hypersensitivity or even pain. In addition, it was described that hypersensitivity decreases the effect of anaesthetic agents, which makes it harder to obtain pain control [Citation7].
Regarding fissure sealants which may be an effective preventive treatment, the use of an adhesive system to permit a higher retention is still controversial, and more studies are needed to confirm the best way of applying these adhesive systems [Citation7,Citation8]. Taking into account atraumatic restorative treatment in permanent teeth, there is still lack of information [Citation7,Citation8]. Concerning resin composite restoration, several factors as the type of adhesive and deproteinization must be taken into consideration, and despite the development of new techniques and materials, further long-term clinical trials and further laboratory research projects are needed [Citation7,Citation8].
In young patients with severe MIH, the use of SSCs is a suitable option to avoid more enamel loss, in order to prevent hypersensitivity, and for the establishment of interproximal and occlusal contacts [Citation7,Citation8]. In cases with severe MIH, the extraction of the PFMs, eventually including also orthodontic treatment, is well considered as part of the treatment regimen [Citation7,Citation8].
Concerning the improvement of the aesthetic appearance of the discolouration of MIH-affected teeth, resin infiltration has been reported as useful. However, there is no strong evidence to support this technique [Citation25].
Implications for research
Countless recommendations can be considered in the scientific literature. Perhaps, if there was a well-defined methodology that could be applied in the assessment of clinical outcomes, the results would be more comparable and meaningful. Forthcoming studies should include a significant number of patients with long periods of follow up. Confounding factors, like the patient’s age, porous enamel, MIH severity, lesion appearance/colour, number of teeth affected in subjects with MIH, the surfaces affected, and the presence of post-eruptive breakdown should also be recorded and considered.
Therefore, designs as controlled clinical trials should be recommended in order to have reliable, significant and comparable outcomes.
Implications for practice
An early diagnosis is fundamental in MIH, in order to prevent further complications like hypersensitivity, dental caries, pulp inflammation, and pain. In this way, preventive interventions with glass ionomer cements as temporary restoration or an early restorative treatment is advisable and indicated. When MIH is detected, parents and off-spring with MIH must be informed about the consequences, like the risk of hypersensitivity, post-eruptive breakdown, higher incidence of caries, difficulties to obtain pain control, and the possibility of numerous appointments for dental care. Recall consultations should be defined according to the severity of MIH, colour of the opacities, and even based on the presence of symptoms. Thus, the treatment modalities available are prevention and symptom control, sealant, restoration, SSCs, and extraction. The hypersensitivity requires to be addressed, because it does not allow effective oral hygiene, thereby an increased risk of caries arises. Remineralization, using CPP-ACP, seems to a possibility for minimization of mild or moderate hypersensitivity in teeth affected by MIH.
In case of severe defects of MIH, composite restorations, indirect restorations (inlay, onlay or overlay) or SSCs are possibilities for intervention/treatment. To make a composite restoration is a reasonable treatment approach for several reasons, like isolation, and sealing dentine and desensitization, although low adhesion to enamel and risk of marginal breakdown of restorations may still be challenges. However, despite it is advisable to end the margins in unaffected enamel and to perform de-proteinization, clinical limitations are observed, in particularly in multi-surface defects. Indirect restoration is also a good treatment approach, given that it provides cuspid coverage, and no mechanical retention is necessary due to the adhesion.
In cases of markedly severe lesions of MIH, extraction may be considered, however, the need for orthodontic treatment may arise. Thus, when orthodontic treatment is necessary, the extraction of teeth severely damaged by MIH is important to include in the treatment plan. In cases of no dental crowding and incisor protrusion, the upper molars should be extracted at the age of 9 to 10 years, and the lower molars at the age of 11 to 12 years. When dental crowding is present or there is incisor protrusion, tooth extraction(s) may occur later, and a suitable time for the extraction of upper molars is about 12 years of age and for the lower molars it is about 9 to 10 years of age. The risks due to early extraction are several, such as distal migration and rotation of the premolar’s germs, or risk of bite deepening given the lack of vertical support.
Regarding incisors, aesthetics is of great importance both for parents and for MIH-affected patients. In this case, remineralization therapy, micro-abrasion, resin infiltration, composites restoration, even veneers or crowns can be weighted.
Conclusion
In conclusion, MIH is highly prevalent seen in a global perspective, the aetiology is likely to be multifactorial, and there are suggested different treatment approaches according to the degree of severity of the MIH lesions. The results should be interpreted cautiously due to the quality of papers included in the systematic reviews available. Furthermore, long-term clinical trials with well-designed methodologies are warranted.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Goodman AH, Allen LH, Hernandez GP, et al. Prevalence and age at development of enamel hypoplasias in Mexican children. Am J Phys Anthropol. 1987;72:7–19.
- Koch G, Hallonsten AL, Ludvigsson N, et al. Epidemiologic study of idiopathic enamel hypomineralization in permanent teeth of Swedish children. Community Dent Oral Epidemiol. 1987;15:279–285.
- Wu X, Wang J, Y. Heng L, et al. Association of molar incisor hypomineralization with premature birth or low birth weight: systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2020;33:1700–1708.
- Jälevik B. Prevalence and diagnosis of molar-incisor-hypomineralisation (MIH): A systematic review. Eur Arch Paediatr Dent. 2010;11:59–64.
- Americano GCA, Jacobsen PE, Soviero VM, et al. A systematic review on the association between molar incisor hypomineralization and dental caries. Int J Paediatr Dent. 2017;27:11–21.
- Bensi C, Costacurta M, Belli S, et al. Relationship between preterm birth and developmental defects of enamel: a systematic review and meta-analysis. Int J Paediatr Dent. 2020;30:676–686.
- da Cunha Coelho ASE, Mata PCM, Lino CA, et al. Dental hypomineralization treatment: a systematic review. J Esthet Restor Dent. 2019;31:26–39.
- Elhennawy K, Schwendicke F. Managing molar-incisor hypomineralization: a systematic review. J Dent. 2016;55:16–24.
- Elhennawy K, Manton DJ, Crombie F, et al. Structural, mechanical and chemical evaluation of molar-incisor hypomineralization-affected enamel: a systematic review. Arch Oral Biol. 2017; 83:272–281.
- Fatturi AL, Wambier LM, Chibinski AC, et al. A systematic review and meta-analysis of systemic exposure associated with molar incisor hypomineralization. Community Dent Oral Epidemiol. 2019;47:407–415.
- Lagarde M, Vennat E, Attal JP, et al. Strategies to optimize bonding of adhesive materials to molar-incisor hypomineralization-affected enamel: a systematic review. Int J Paediatr Dent. 2020;30:405–420.
- Lygidakis NA. Treatment modalities in children with teeth affected by molar-incisor enamel hypomineralisation (MIH): a systematic review. Eur Arch Paediatr Dent. 2010;11:65–74.
- Schwendicke F, Elhennawy K, Reda S, et al. Global burden of molar incisor hypomineralization. J Dent. 2018;68:10–18.
- Silva MJ, Scurrah KJ, Craig JM, et al. Etiology of molar incisor hypomineralization – a systematic review. Community Dent Oral Epidemiol. 2016;44:342–353.
- Garot E, Denis A, Delbos Y, et al. Are hypomineralised lesions on second primary molars (HSPM) a predictive sign of molar incisor hypomineralisation (MIH)? A systematic review and a meta-analysis. J Dent. 2018;72:8–13.
- Crombie FA, Manton DJ, Palamara JEA, et al. Characterisation of developmentally hypomineralised human enamel. J. Dent. 2013;41:611–618.
- Serna C, Vicente A, Finke C, et al. Drugs related to the etiology of molar incisor hypomineralization: a systematic review. J Am Dent Assoc. 2016;147:120–130.
- Wogelius P, Haubek D, Poulsen S. Prevalence and distribution of demarcated opacities in permanent 1st molars and incisors in 6 to 8-year-old Danish children. Acta Odontol Scand. 2008;66:58–64.
- Soviero V, Haubek D, Trindade C, et al. Prevalence and distribution of demarcated opacities and their sequelae in permanent 1st molars and incisors in 7 to 13-year-old Brazilian children. Acta Odontol Scand. 2009;67:170–175.
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6:e1000100.
- Smith V, Devane D, M Begley C, et al. Methodology in conducting a systematic review of biomedical research. Med. Reasearch Methodol. 2011;1:61–73.
- Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. Bmj. 2017; 358:1–9.
- Alaluusua S. Aetiology of molar-incisor hypomineralisation: a systematic review. Eur Arch Paediatr Dent. 2010;11:53–58.
- Zhao D, Dong B, Yu D, et al. The prevalence of molar incisor hypomineralization: evidence from 70 studies. Int J Paediatr Dent. 2018;28:170–179.
- Borges AB, Caneppele TMF, Masterson D, et al. Is resin infiltration an effective esthetic treatment for enamel development defects and white spot lesions? A systematic review. J Dent. 2017; 56:11–18.
- Elhennawy K, Krois J, Jost-Brinkmann PG, et al. Outcome and comparator choice in molar incisor hypomineralisation (MIH) intervention studies: a systematic review and social network analysis. BMJ Open. 2019;9:e028352.
- Weerheijm KL, Duggal M, Mejàre I, et al. Judgement criteria for Molar Incisor Hypomineralisation (MIH) in epidemiologic studies: a summary of the European meeting on MIH held in Athens, 2003. Eur J Paediatr Dent. 2003;4:110–113.
- Dantas E, Cavalcanti Y, Vieira B, et al. Association between dental enamel development defects and low birth weight: a systematic review and metanalysis. Citation Review question Participants/population Intervention(s), exposure(s). International prospective register of systematic reviews. PROSPERO 2020 CRD42020171765. 2017. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42017078004
- Ureles S, Howe M, Ureles S, et al. The association of molar incisor hypomineralization (MIH) and hypomineralization of the second primary molar (HSPM) with dental caries in the mixed dentition: a systematic review and meta-analysis. International prospective register of systematic reviews. PROSPERO 2017 CRD42017078004. 2020. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020171765
- Wogelius P, Viuff JH, Haubek D. Use of asthma drugs and prevalence of molar incisor hypomineralization. Int J Paediatr Dent. 2020;30:734–740.
- Nørrisgaard PE, Haubek D, Kühnisch J, et al. Association of high-dose vitamin D supplementation during pregnancy with the risk of enamel defects in offspring: a 6-year follow-up of a randomized clinical trial. JAMA Pediatr. 2019;173:924–930.