Abstract
Objective
To examine how hospital-affiliated dentists assess risk and evaluate oral foci of infection in patients facing certain medical treatments, and whether the nature of upcoming medical treatment affects the choice of dental intervention.
Materials and methods
A survey comprising six clinical cases (50 teeth) was sent to hospital-affiliated dentists in Sweden. A treatment option for the affected tooth/teeth in each case was selected whether the patient was facing heart valve surgery, chemotherapy, radiation therapy, intravenous bisphosphonate treatment, solid organ transplantation or was diagnosed with endocarditis.
Results
Consensus in choice of dental treatment was high in 62%, moderate in 32% and low in 6% of the assessments. High variability of choice of treatment was seen for eight teeth whereas the remaining 42 teeth often received the same therapy regardless of medical issue. Chemotherapy and radiotherapy were thought to entail the highest risk for oral infectious sequelae with a risk ranging from 1% to 100%.
Conclusion
Pre-medical dental evaluations and recommended treatments are often uniform with the exception of the management of asymptomatic root canal treated teeth with persisting apical radiolucency and heavily decayed molars. In many instances, dental diagnosis has a greater impact on choice of treatment than the underlying medical issue and associated implications thereof.
Introduction
Medical treatment may cause adverse side effects in the oral cavity and oral infection may give rise to complications affecting the medical procedure and treatment outcome [Citation1–6]. In Sweden, patients diagnosed with endocarditis, patients facing radiotherapy of the head/jaw/neck, chemotherapy, intravenous bisphosphonate (IVBP) treatment, solid organ transplantation (SOT) or heart valve surgery (HVS) are commonly sent upon referral to hospital-affiliated dental clinics for evaluation prior to the onset of medical treatment. These investigations, which are subsidised by the Swedish government, include a full clinical examination of the oral cavity and intraoral/panoramic radiographic images [Citation7,Citation8]. The objectives are to detect and eliminate oral infections that might affect the medical procedure as well as to reduce the risk of oral infectious sequelae arising due to the medical intervention [Citation1,Citation7,Citation9,Citation10].
Various guidelines exist on regional and national levels in Sweden as well as in other countries, yet no detailed or unanimous protocols for treating medically compromised patients are available [Citation4,Citation11–15], and studies on the importance of dental disease management prior to some of the above-mentioned medical treatments give unclear or contradictory results [Citation16–20]. The ethical difficulties of performing prospective trials on these patients may to some degree explain the meagre scientific evidence [Citation17].
Ideally, dental care should be consistent and equivalent, and the nature of dental treatment should not be reliant on where or by whom the patient is treated. Yet, due to the lack of unequivocal guidelines for pre-therapeutic dental treatment, as well as the difficulty of distinguishing those oral findings that require treatment from those that can be left untreated without jeopardizing the patient’s health, there is a risk that assessment and subsequent dental treatment will depend on clinic routines and the individual clinician’s experience.
The purpose of the present study was to discern areas within pre-medical dental care where more pronounced treatment guidelines for best practice would be beneficial for both patients and dentists. The aim was to examine how dentists working in hospital-affiliated dental clinics in Sweden evaluate oral findings identified during dental examinations prior to medical therapies and whether the nature of the medical treatment and its estimated risk affect the choice of dental intervention.
Material and methods
Participation
All dentists working in hospital-affiliated dental clinics in Sweden were invited to participate. As no national registry of these clinicians exists, a list comprised of 146 dentists was created after researching all centres conducting pre-medical dental investigations in Sweden.
No specialist degree is required in order to work as a hospital-affiliated dentist in Sweden and hospital-affiliated dentists are with few exceptions general dentists that have undergone further field-specific education and courses. However, on 1 June 2018, the National Board of Health and Welfare approved Orofacial Medicine as a new specialist branch in Swedish dentistry, but at the time of this survey, only a handful of dentists were qualified specialists.
Survey
The survey included six authentic clinical cases. Each case comprised a number of affected teeth, ranging from one tooth to 16 teeth. The oral findings were apical periodontitis, marginal periodontitis, caries and impacted molars. The cases were presented on a website with brief anamnestic information, clinical findings and radiographs (panoramic and/or intraoral X-ray images). summarises each of the cases.
Table 1. Summary of the six patient cases included in the survey.
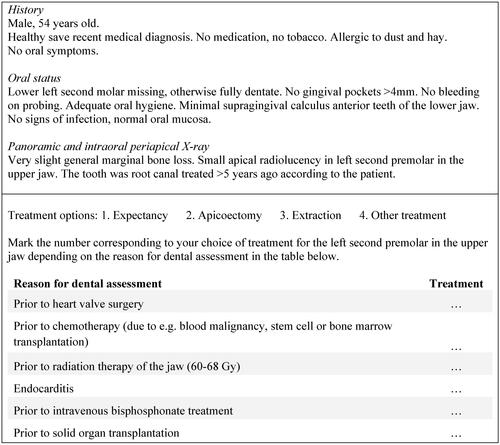
A paper reply form was distributed by postal service. The reply form also contained questions regarding the views on the importance of focal investigations and the awareness of available scientific evidence in the field. The participants were instructed to choose a treatment option for the affected tooth/teeth in each case depending on whether the patient was to undergo HVS, chemotherapy, radiation therapy, IVBP treatment, SOT or had been diagnosed with endocarditis. Each tooth was therefore assessed six times – once for each medical situation. A complete case illustrating the nature of the information provided to the participants as well as the layout of the reply form is presented in .
The participants were also asked to estimate the risk for serious complications if the patient was left without dental treatment, and which medical situation was believed to pose the highest risk for complications in each of the six cases.
Procedure
A letter explaining the purpose, aim and execution of the study, a consent form, a reply form with the link to the digital information and a return envelope was sent by postal service to all participants. Two additional mailings were sent out as reminders under the course of three months. The study was approved by the Regional Ethics Review Board in Lund, Sweden (Dnr. FO 4.3-2018/220).
Compilation of data
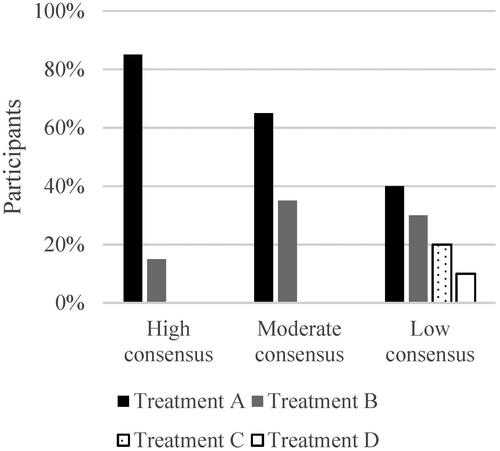
The study included six cases with a total of 50 teeth. For each tooth, a treatment was selected six times, once for every medical situation, which resulted in 300 assessments. Assessments were compiled according to the answers from each individual dentist regarding choice of treatment for each tooth and categorised as either: high consensus, where ≥75% of participants chose the same dental treatment; moderate consensus, where 50–74% of participants chose the same dental treatment or low consensus, where <50% of participants chose the same dental treatment ().
Figure 2. Model for grouping of consensus on the choice of dental treatment. High consensus: ≥75% of participants agreed on choice of dental treatment. Moderate consensus: 50–74% of participants agreed on choice of dental treatment. Low consensus: <50% of participants agreed on choice of dental treatment. Treatments A–D different for each patient case.
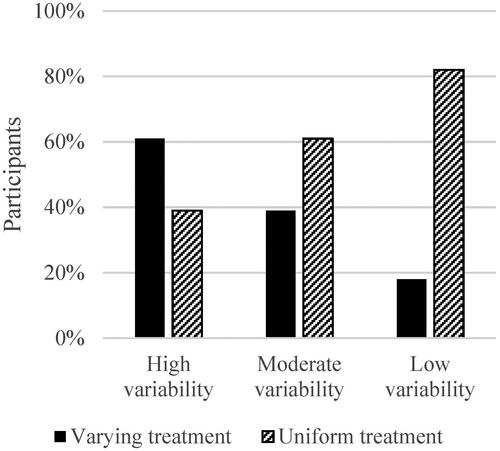
Additionally, survey responses were compiled according to the level of variability in treatment selection, i.e. whether the same treatment was selected for a tooth in all medical situations or whether dental treatment varied depending on underlying medical issue. Teeth were categorised as either: high variability, where ≥50% of participants altered their selection of dental treatment in relation to medical situation; moderate variability, where 25–49% of participants altered their treatment selection in relation to underlying medical issue or low variability, where <25% of the participants altered their treatment selection in relation to underlying medical issue ().
Figure 3. Model for grouping of variability of the choice of dental treatment. High variability: ≥50% of participants altered their treatment selection in relation to underlying medical issue. Moderate variability: 25–49% of participants altered their treatment selection in relation to underlying medical issue. Low variability: <25% of participants altered their treatment selection in relation to underlying medical issue.
Statistical analysis
Spearman’s r was used to assess correlation between risk-estimation in each case and proportion of assessments where extraction was selected. Each case was compiled according to the proportion of assessments where extraction was selected, i.e. the proportion of extractions would be 50% in a case comprised of one tooth if extraction was selected in three out of six medical scenarios.
Mann–Whitney’s U was used to assess relation between risk-estimation and years of experience.
Results
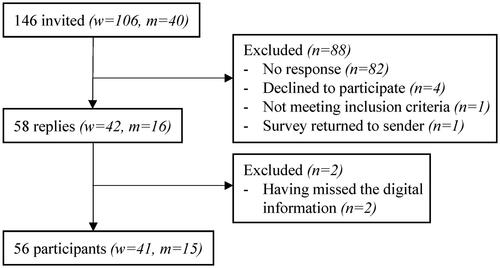
One hundred forty-six dentists, 106 (73%) women and 40 (27%) men, were invited to participate. 58 out of 146 dentists responded to the survey and replies from 56 (38%) dentists, 41 (73%) women and 15 (27%) men were included in the study (2 missed the digital information). A flow-chart of study participation is shown in . The mean age of the participants was 49 years (SD 11 years). Experience of working with hospital-affiliated dentistry ranged from one year to 40 years with an average of 12 years.
Opinions on the importance of, and level of scientific research on, pre-medical dental evaluations
Participants were asked to grade the importance of conducting dental assessments in relation to the medical situations provided in this study. Nearly all participants regarded patients facing radiation therapy very important to examine, closely followed by patients facing chemotherapy or IVBP treatment. Patients subjected to HVS were viewed least important to assess ().
Figure 5. Estimation of the importance of dental evaluations in relation to the various medical situations. HVS: Heart valve surgery; CT: chemotherapy; RT: radiation therapy; EC: endocarditis; IVBP: intravenous bisphosphonate treatment; SOT: solid organ transplantation.
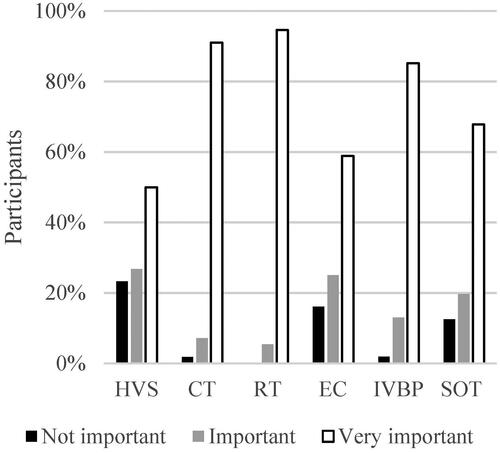
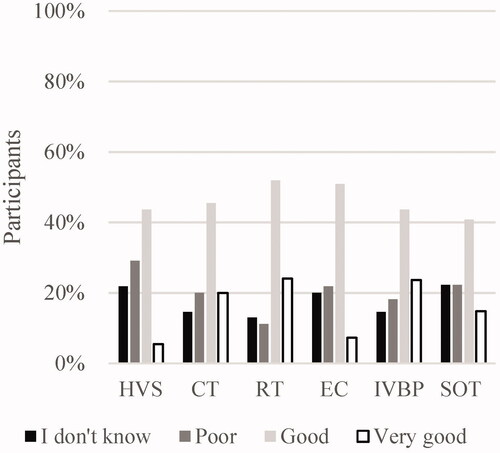
The participants’ opinions on how solid the scientific research is in relation to the medical situations are shown in . HVS, endocarditis and SOT were the medical situations thought to have the poorest evidence and yielded the highest number of “I don’t know” responses. The evidence for dental evaluations prior to radiation therapy was judged to be the best.
Risk assessment
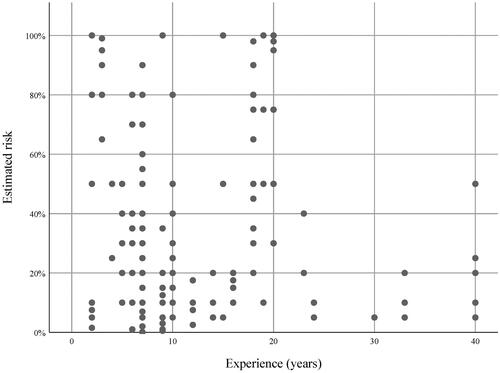
When asked to estimate the risk for serious complications if the patient was left without dental treatment, not all participants responded and some only answered what medical situation they thought brought forth the highest risk without defining the percentage. Estimated risk in percentage for all cases is shown in .
Figure 7. Estimation of risk for complications if patients in cases 1–6 were to be left without dental treatment in relation to the various medical situations. HVS: Heart valve surgery; CT: chemotherapy; RT: radiation therapy; EC: endocarditis; IVBP: intravenous bisphosphonate treatment; SOT: solid organ transplantation.
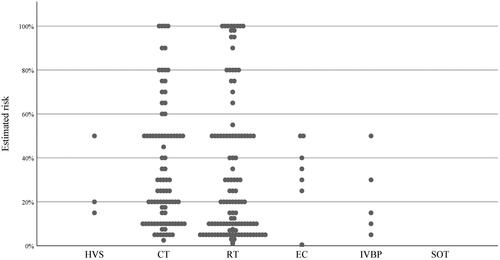
Case 1 – For a patient with untreated active marginal periodontitis, 25 dentists believed chemotherapy would entail the highest risk and 23 dentists thought radiation therapy would cause the highest risk for infectious complications. A vast range in assessed risk was seen for both categories, ranging from 5% to 100% and 2% to 95% respectively.
Case 2 – A patient with an asymptomatic root canal treated upper premolar with persisting apical radiolucency was believed to face the highest risk by 23 participants when undergoing chemotherapy, whereas 22 participants considered radiation therapy to cause the highest risk. The range in risk regarding chemotherapy was 1–100% and 1–70% regarding radiation therapy.
Case 3 – If a patient with numerous caries lesions, periodontal problems and a number of periapical infections was to be left without dental treatment, 27 participants believed chemotherapy entailed the highest risk, ranging from 7% to 80%. 18 dentists believed radiation therapy most risk-associated with a risk ranging from 5% to 100%.
Case 4 – If leaving a patient with impacted molars and an asymptomatic root canal treated lower left first molar with persisting apical radiolucency without treatment, the highest risk would according to 25 participants arise during radiation therapy and according to 24 participants during chemotherapy, ranging from 5% to 100% in both events.
Case 5 – For a patient with untreated furcation involved lower molars and impacted third molars, 25 dentists believed radiation therapy would cause the highest risk for infectious complications and 22 dentists expected chemotherapy would entail the highest risk. The range in risk was 3–100% regarding radiation therapy and 5–80% regarding chemotherapy.
Case 6 – Radiation therapy of a patient with numerous untreated caries lesions would entail the highest risk of infectious sequelae according to 32 participants with a risk ranging from 2% to 100%. 15 participants judged chemotherapy to be most risk-associated, ranging from 5% to 80% ().
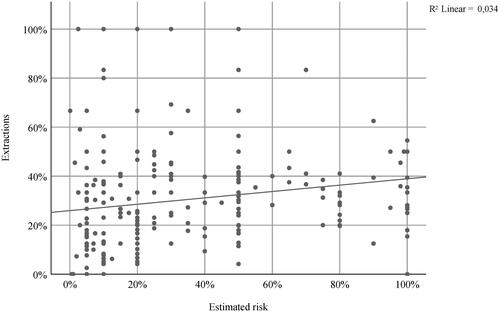
Participant risk-estimation in each case was compared to the proportion of assessments in each case where extraction was selected. Distributed across the six cases, the total number of risk-estimations where a percentage was offered was 219. There was a significant but very low correlation between risk-estimation and number of extractions (p < .001; r2 = 0.034) ().
Figure 8. Correlation between estimated risk for complications and rate of extractions. Y-axis: proportion of estimations in each case where extraction was selected. X-axis: estimated risk for complications. Each dot represents a case assessed by a participant having defined the risk in percentage.
The risk assessment related to years of experience is depicted in . There was a significant difference in anticipated risk between dentists with less than 20 years of experience and those with more (p < .001), especially for cases 4 and 5 (data not shown).
Consensus on choice of dental treatment
High level of consensus was seen in 62% of the assessments. Dentists were in high consensus on course of treatment for impacted third molars, premolars with moderate caries lesions, molars with severe caries lesions and periodontally damaged premolars and incisors as well as molars with vertical bone defects and furcation involvement II–III.
Moderate level of consensus was seen in 32% of the assessments. Periodontally damaged second and third molars, decayed teeth with apical periodontitis as well as incisors with large cavities were found in this group.
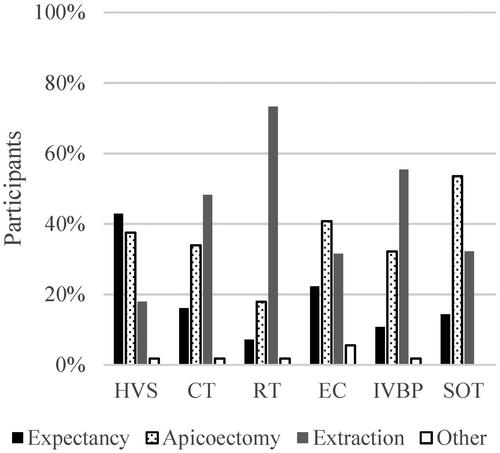
Low level of consensus was seen in 6% of the assessments. Out of the 19 assessments where low consensus was seen, six were regarding HVS and endocarditis respectively. Asymptomatic root canal treated teeth with apical radiolucency (n = 10), molars with deep caries lesions (n = 5) and a premolar with deep filling and uncertain vitality (n = 4) were found in this group. Selected treatment options for an asymptomatic root canal treated second premolar in the upper jaw with apical radiolucency in the various medical scenarios are shown in . Low consensus on course of treatment is seen for HVS, chemotherapy and endocarditis.
Figure 10. Case 2: Proposed treatment for an asymptomatic root canal treated upper left second premolar with apical radiolucency in various medical situations. HVS: Heart valve surgery; CT: chemotherapy; RT: radiation therapy; EC: endocarditis; IVBP: intravenous bisphosphonate treatment; SOT: solid organ transplantation. Other treatment unspecified by participants.
Variability of choice of dental treatment
Low variability of choice of dental treatment was seen for 17 teeth. Impacted third molars, periodontally damaged incisors and premolars as well as molars with furcation involvement II–III and/or vertical bone defects were found in this group where most dentists chose one and the same dental treatment regardless of medical situation.
Moderate variability was seen for 25 teeth. Teeth with caries lesions, periodontally damaged molars as well as decayed teeth with apical periodontitis were found in this group.
High variability of choice of dental treatment was seen for eight teeth. Asymptomatic root canal treated teeth with apical radiolucency (n = 3), molars with deep caries lesions (n = 3), a premolar with deep filling and uncertain vitality (n = 1) and a lower second molar with furcation involvement I (n = 1) were found in this category.
Discussion
Rate of participation
Two dentists declined participation due to time constraints and the same reason could presumably account for a large number of response dropouts since the survey was quite extensive. Access to the internet was a prerequisite for responding. As one dentist not able to access the link declined participation, others may have refrained from responding due to similar firewall snags.
Risk assessment
The extreme range in the estimated risk of complications in each case shows how challenging the task of risk-estimation is. For one thing, the threshold for considering a complication serious may have varied. However, it is also likely that ‘risk’ was interpreted differently by the participants. For some, ‘risk’ appeared to be the probability for complications to occur whereas others regarded ‘risk’ as the combination of risk probability and risk impact, i.e. the severity of the complications. Accordingly, the finding that participants with long experience tended to estimate risk lower must be regarded cautiously. In addition, the experience of a specific medical scenario varied between the participants, not only with regard to years of experience but also to the number of patients the participants normally were confronted with.
Radiation therapy of the neck/jaw/head can lead to an array of short- and long-term complications in the oral cavity [Citation21] and one aim of dental treatment prior to radiation is to prevent future development of osteoradionecrosis [Citation22]. This severe complication may explain why radiation therapy was believed to be one of the highest risk factors for sequelae, and why patients facing radiation therapy of the head/jaw/neck were judged to be the most important to examine prior to the onset of medical therapy.
It is probable that untreated dental disease will eventually necessitate tooth extraction, which is an important cause for developing osteoradionecrosis (ORN) in the area exposed to radiation [Citation23]. An increased risk for ORN has also been suggested in patients undergoing radiation therapy with severe untreated marginal periodontitis [Citation24]. A previous study found the 5-year rate of ORN to be 6% in patients where poor teeth were left in the irradiated area and 2% where good teeth were left [Citation25]. In comparison, many of the risk-assessments in the present study were considerably higher.
Participants associated chemotherapy with a high risk for infectious complications. A systematic review of the literature found that the prevalence of infections and abscesses linked to oral foci during chemotherapy was 5.4% and did not substantially differ when excluding studies where oral infection had not been eliminated [Citation17]. A study on apical periodontitis as an infection source during chemotherapy found that exacerbation of asymptomatic apical periodontitis may occur, but that exacerbation did not severely affect the patient’s general health [Citation26]. Schuurhuis et al. [Citation27] found that chronic oral infections did not increase the risk for complications in patients receiving chemotherapy and Hong et al. [Citation17] concluded that symptom free teeth with probing depth less than 8 mm, small periapical lesions and slightly mobile teeth could be left without treatment prior to chemotherapy in light of the relative low risk of complications. Compared to these studies, the results of the present study show that the risk of complications is considered higher by practicing dentists.
Screening patients facing IVBP treatment was regarded as very important by many participants, yet few participants considered IVBP treatment as the highest risk for infectious complications. This is interesting as IVBP treatment results, much like radiation therapy, in a long-term locus minoris resistentiae with a susceptibility of developing bisphosphonate-related osteonecrosis of the jaw (BRONJ) [Citation28,Citation29].
A hypothesis when conducting this study was that a high risk-estimation would result in more extractions. However, there was no substantial correlation between risk-estimation and number of extractions. Interestingly, some participants that assessed risk as low chose extraction more often than participants that believed the risk for complications to be high, and vice versa. It is possible that time constraints associated with the various medical situations, clinical routines, compliance or other patient-related aspects affected the treatment selection and led to extraction rather than to conservative treatment. For example, extraction prior to radiation therapy is a risk factor for ORN [Citation25], and extractions prior to chemotherapy can give rise to complications delaying the onset of medical treatment [Citation17]. In addition, various interpretations of the concept of risk may have contributed to the disparate choices of treatment.
To what extent patient-related factors influenced treatment selection was beyond the scope of this survey and since the six patient cases often included multiple dental diagnoses, it was not possible to discern what dental source of infection that was referred to in relation to risk for complications.
Consensus on choice of dental treatment
Although the participants varied greatly in their risk assessment, they were still often in high agreement on the course of dental treatment. The results indicate that treatment of impacted third molars, moderate carious lesions as well as periodontally damaged teeth is quite consistent regardless of where or by whom the treatment is performed.
There was low agreement on the management of asymptomatic root canal treated teeth with persisting apical radiolucency as well as molars with deep cavities, allowing for large treatment variations. Differing views on whether the apical lesions represented ongoing inflammation or merely scar tissue may have contributed to less uniform treatment selections. However, consensus on treatment was high prior to radiation therapy and often lead to extraction of the tooth. This is consistent with the difficulty of predicting the longevity of endodontically unsound teeth and the increased risk of ORN from endodontic treatment prior to radiation therapy [Citation30].
Out of the assessments where low consensus on treatment was seen, one third were regarding patients facing HVS and one third regarding patients having been diagnosed with endocarditis. HVS and endocarditis were also the scenarios viewed to have the poorest scientific evidence and where pre-medical dental assessments were considered least important. Accordingly, Bratel et al. [Citation31] could not establish that elimination of oral infection prior to HVS improved long term survival and a systematic review of the literature evaluating the effects of dental treatment before HVS concludes that it is uncertain as to whether rates of mortality, infective endocarditis, post-surgical infections and length of hospital stay are affected by pre-medical dental treatment [Citation32]. Apparently, there is a need for clear, evidence-based treatment guidelines.
Variability of choice of dental treatment
The nature of the upcoming medical treatment plays a central role in assessments and pre-medical dental treatment. Dental treatment prior to chemotherapy depends on the probability that an existing oral focus of infection will exacerbate during the impairment of the immune system. Prior to radiation and IVBP treatment the plausibility of a tooth needing extraction within the years to come needs to be considered [Citation1]. Nevertheless, for a substantial number of teeth in the present survey, one dental treatment was proposed regardless of medical situation. One participant commented that extraction of one tooth would be proposed even in a healthy individual due to severe caries and poor prognosis. This indicates that the tooth diagnosis may have a greater impact on choice of treatment than the nature of medical treatment. In contrast, the management of asymptomatic root canal treated teeth with apical radiolucency as well as molars with deep caries lesions varied depending on the reason for dental assessment, indicating that the implications of the medical situation have a greater impact on the choice of treatment for these oral findings.
Conclusion
The result of the present study shows that dental investigations and pre-medical dental treatments often are consistent and uniform regardless of where or by whom they are performed. It also appears that the dental diagnosis often has a greater impact on choice of dental treatment than the underlying medical issue and associated implications thereof. The present study implies that hospital-affiliated dentists are most concerned about oral infectious sequelae in patients facing chemotherapy and radiation therapy. However, patients with asymptomatic root canal treated teeth with persisting apical radiolucency as well as molars with deep caries lesions may receive less uniform treatment as consensus for management of these conditions was low. Further studies on the pre-medical dental management could hopefully lead to guidelines, not only describing the need for treatment in various situations but also suggesting evidence-based, yet individually adapted, therapies related to risk. This would certainly be beneficial to both patients and the dental community.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Brennan MT, Woo SB, Lockhart PB. Dental treatment planning and management in the patient who has cancer. Dent Clin North Am. 2008;52:19–37.
- Guggenheimer J, Mayher D, Eghtesad B. A survey of dental care protocols among US organ transplant centers. Clin Transplant. 2005;19:15–18.
- Souza AF, Rocha AL, Castro WH, et al. Dental management for patients undergoing heart valve surgery. J Card Surg. 2017;32:627–632.
- PDQ® Supportive and Palliative Care Editorial Board. PDQ oral complications of chemotherapy and head/neck radiation. Bethesda (MD): National Cancer Institute. [cited 2016 Dec 16]. Available from: https://www.cancer.gov/about-cancer/treatment/side-effects/mouth-throat/oral-complications-hp-pdq.
- Graber CJ, de Almeida KN, Atkinson JC, et al. Dental health and viridans streptococcal bacteremia in allogeneic hematopoietic stem cell transplant recipients. Bone Marrow Transplant. 2001;27:537–542.
- Gruter MO, Brand HS. Oral health complications after a heart transplant: a review. Br Dent J. 2020;228:177–182.
- Internetodontologi.se [Internet]. Internetmedicin AB. [cited 2020 May 18]. Available from: https://www.internetodontologi.se/orofacial-medicin/fokalutredning/.Swedish.
- Tandvårdsförordning (SFS 1998:1338). Socialdepartementet. 1998. Swedish.
- Levi LE, Lalla RV. Dental treatment planning for the patient with oral cancer. Dent Clin North Am. 2018;62:121–130.
- Melkos AB, Massenkeil G, Arnold R, et al. Dental treatment prior to stem cell transplantation and its influence on the posttransplantation outcome. Clin Oral Investig. 2003;7:113–115.
- Guggenheimer J, Eghtesad B, Stock DJ. Dental management of the (solid) organ transplant patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:383–389.
- Cotti E, Arrica M, Di Lenarda A, et al. The perioperative dental screening and management of patients undergoing cardiothoracic, vascular surgery and other cardiovascular invasive procedures: a systematic review. Eur J Prev Cardiol. 2017;24:409–425.
- Svensk förening för orofacial medicin. Odontologiskt omhändertagande av patienter med hematologisk sjukdom och patienter med huvud/halscancer (H/N cancer). [cited 2017 May 10] Available from: odontologiskt-omhandertagande-av-hematologiska-sjukdomar.pdf (regionkronoberg.se). Swedish.
- Napenas JJ, Kujan O, Arduino PG, et al. World Workshop on Oral Medicine VI: controversies regarding dental management of medically complex patients: assessment of current recommendations. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120:207–226.
- British Society for Disability and Oral Health. The oral management of oncology patients requiring radiotherapy, chemotherapy and/or bone marrow transplantation – clinical guidelines. [cited 2018]. Available from: RCS Oncology Guideline Update V36.pdf
- de Souza AF, Rocha AL, Castro WH, et al. Dental care before cardiac valve surgery: is it important to prevent infective endocarditis? Int J Cardiol Heart Vasc. 2016;12:57–62.
- Hong CHL, Hu S, Haverman T, et al. A systematic review of dental disease management in cancer patients. Support Care Cancer. 2018;26(1):155–174.
- Schuurhuis JM, Stokman MA, Witjes MJ, et al. Evidence supporting pre-radiation elimination of oral foci of infection in head and neck cancer patients to prevent oral sequelae. A systematic review. Oral Oncol. 2015;51:212–220.
- Meyer U, Weingart D, Deng MC, et al. Heart transplants-assessment of dental procedures. Clin Oral Investig. 1999;3:79–83.
- Rustemeyer J, Bremerich A. Necessity of surgical dental foci treatment prior to organ transplantation and heart valve replacement. Clin Oral Investig. 2007;11:171–174.
- Kufta K, Forman M, Swisher-McClure S, et al. Pre-radiation dental considerations and management for head and neck cancer patients. Oral Oncol. 2018;76:42–51.
- Chrcanovic BR, Reher P, Sousa AA, et al. Osteoradionecrosis of the jaws-a current overview-part 2: dental management and therapeutic options for treatment. Oral Maxillofac Surg. 2010;14:81–95.
- Strojan P, Hutcheson KA, Eisbruch A, et al. Treatment of late sequelae after radiotherapy for head and neck cancer. Cancer Treat Rev. 2017;59:79–92.
- Schuurhuis JM, Stokman MA, Roodenburg JLN, et al. Efficacy of routine pre-radiation dental screening and dental follow-up in head and neck oncology patients on intermediate and late radiation effects. A retrospective evaluation. Radiother Oncol. 2011;101:403–409.
- Chang DT, Sandow PR, Morris CG, et al. Do pre-irradiation dental extractions reduce the risk of osteoradionecrosis of the mandible? Head Neck. 2007;29(6):528–536.
- Skallsjo K, Johansson JE, Jonasson P, et al. Apical periodontitis as potential source of infection in patients with lymphoma treated with chemotherapy. Clin Oral Invest. 2020;24(1):133–140.
- Schuurhuis JM, Span LFR, Stokman MA, et al. Effect of leaving chronic oral foci untreated on infectious complications during intensive chemotherapy. Br J Cancer. 2016;114:972–978.
- Otto S, Schreyer C, Hafner S, et al. Bisphosphonate-related osteonecrosis of the jaws – characteristics, risk factors, clinical features, localization and impact on oncological treatment. J Craniomaxillofac Surg. 2012;40:303–309.
- Ruggiero SL, Dodson TB, Fantasia J, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw-2014 update. J Oral Maxillofac Surg. 2014;72(10):1938–1956.
- Huang YF, Liu SP, Muo CH, et al. The association between dental therapy timelines and osteoradionecrosis: a nationwide population-based cohort study. Clin Oral Invest. 2020;24(1):455–463.
- Bratel J, Kennergren C, Dernevik L, et al. Treatment of oral infections prior to heart valve surgery does not improve long-term survival. Swed Dent J. 2011;35:49–55.
- Lockhart PB, DeLong HR, Lipman RD, et al. Effect of dental treatment before cardiac valve surgery: systematic review and meta-analysis. J Am Dent Assoc. 2019;150:739–747.