Abstract
Objective
To investigate adoption and integration of technological aids during endodontic treatment and where dental practitioners (DPs) learnt to use this technology.
Materials and methods
An electronic questionnaire was distributed to all 459 dentists who graduated from University of Bergen between 2008 and 2018. The respondents were divided into two cohorts, older graduates (2008–2013) and newer graduates(2014–2018).
Results
A total of 314(68.4%) DPs answered the questionnaire. Magnification in the form of dental operating microscopes (DOM) and dental loupes was used by 180 (59.6%), electronic apex locators (EAL) by 271(89.7%) and motor-driven files by 281 (93.4%) DPs. The most frequent response, as to where they learnt to use them was: during undergraduate dental (UG) education. Significantly more newer graduates (90.7%) performed instrumentation based on what they learnt during UG education (p < .001). Older graduates based their instrumentation method equally on what they learnt during UG education (51.9%) and continuing dental education(42.6%). Rubber dam was used during all treatment procedures by 93% of the DPs.
Conclusions
UG education is a communication channel with long-lasting importance for adoption and integration of technology by DPs. Exposure to innovations (awareness) during UG education is adequate for integration of technology. Continuing dental education is as valuable as UG education for adoption of technology for older graduates.
Introduction
Dental practitioners (DPs) are confronted with challenges when selecting tools, techniques and products to perform root canal treatment (RCT). There is limited information on factors that influence the dentists’ everyday choices in a dental practice. Price, advertising campaigns, recommendations from colleagues or experience during undergraduate dental (UG) education are several factors that may influence the DPs’ final choice of technique and tools to perform RCT.
Endodontic treatment is performed to retain teeth that would otherwise have to be extracted. In the field of clinical endodontics, the late 1990s was an important era for innovations and expansion of new technology. Innovation refers to any idea, practice, or object that is perceived as new by an individual, whereas technology is the application of scientific knowledge through machinery and equipment. Advances in technology are intended to improve endodontic treatment outcome. Some of the most pertinent introductions were the use of dental operating microscopes (DOM) for better visualization [Citation1,Citation2] electronic apex locators (EAL) to aid working length determination [Citation3] and motor-driven file systems for instrumentation [Citation4]. One technology that has evolved considerably due to innovations in metallurgy and material sciences is the motor-driven file systems. This has resulted in frequent introduction of new file systems. Newer file systems often claim to be more efficient, reliable and user-friendly than the current system. Thus, DPs have to make important decisions on whether the new system is indeed what it claims to be and integrate it into their clinical practice.
Diffusion of innovations is a theory that seeks to explain how, why and at what rate new ideas and technology spread. According to Rogers, adoption of technology depends on four recognized elements of diffusion: the innovation itself, communication channels, time and social system [Citation5]. DPs are expected to adopt new technology in line with developments. However, studies have shown that DPs are slow to integrate innovations into daily clinical practice [Citation6]. Bjørndal and Reit (2005) describes a phenomenon where adoption of new technology among general DPs does not occur in isolation, but as a “technology cluster”. This means that adoption of new technology is correlated with other innovations. Interestingly, Danish general DPs’ frequent use of rotary instrumentation is associated with frequent use of rubber dam [Citation6].
Dental students at the Department of Clinical Dentistry, University of Bergen (UoB), Bergen, Norway, are educated with current endodontic concepts and technology. However, current concepts change over the years [Citation7]. The dental education curriculum at UoB is based on the European Society of Endodontology (ESE) guidelines [Citation8]. All RCT procedures at the student clinic are performed with rubber dam isolation.
The primary aim of this study is to investigate integration and adoption of technology by DPs who graduated between 2008 and 2018 at the UoB and compare it with implementation of technology at the educational institution. The secondary aim is to identify the mode of communication channel for this diffusion of innovation. We utilized the impact of relocating to a new building in 2012 with better equipped dental clinic to help identify how the use of technological aids during UG education influenced adoption of innovations in subsequent careers.
Our hypothesis is that tools and techniques used during UG education are important determinants for integration of technological aids in a general dental practice.
Materials and methods
The participants
The survey was sent to all 459 dentists who graduated from UoB during an 11-year period, 2008–2018. During this period, new innovations were integrated into the UG education. Before 2012, only two DOMs and several EALs were available for undergraduate clinical training. In 2012, the dental school was relocated to a new building with a better equipped endodontic clinic. The new clinic had ceiling mounted DOM in individual cubicles, more EAL and motor-driven files for dental education. In 2008, the motor-driven instrumentation system ProTaper® (Dentsply) was introduced. In 2014, a new motor-driven instrumentation system WaveOne® (Dentsply) was introduced in the undergraduate clinic. Our study compares respondents graduating at UoB from 2008 to 2013 (older graduates) with those graduating from 2014 to 2018 (newer graduates).
Questionnaire
The questionnaire consisted of closed-end questions, Likert scale (1-5) and open-ended questions. The closed-end questions were a combination of one-answer options and several options when appropriate. To obtain accurate information, an open-ended answer option was always provided when questions had closed-end alternatives. This allowed the respondents to answer if they felt that the closed-end options did not match their opinion. A response had to be registered to a question to proceed to the next question.
The first part of the questionnaire dealt with demographic and background information such as gender, year of graduation and practice location. The respondents were asked in a second part if they performed RCT and whether they had completed any specialist training. Participants who responded to “do not perform root canal treatment” or reported being specialist in endodontics were rejected from further participation as they were not part of our target group. Part three was about the practice characteristics and use of technology during RCT. Questions included the opportunity to refer to an Endodontist, the number of RCTs performed by the respondent per month, tools used for magnification, determination of working length and instrumentation. Only respondents who gave a positive response to the use of DOM, EAL and motor-driven instrumentation were directed to a question as to where they learnt to use these tools. Respondents could select more than one option as to where they had learnt to use the technological aids. The final question was on the use of rubber dam. Participants were given the following options on the use of rubber dam for isolation during root canal procedures; always, never, or selected groups of teeth such as anteriors, posteriors, maxillary and/or mandibular.
Collection of data
An electronic questionnaire was designed via SurveyXact (SurveyXact; Rambøll, Oslo, Norway). A recruitment letter with link to the questionnaire was sent to all 459 graduates from the 11-year period 2008–2018.
Ethics
Participation in the survey was voluntary. The survey was anonymous, and the processing of personal data was approved in July 2018 by the Norwegian Centre for Research Data (NSD, reference number 61475). The aim of the survey, how contact information was obtained, and what the data were intended for was stated on the first page. All participants consented before they proceeded to respond to the questions. On the last page, the researcher’s (SRH) contact information was provided. This was in accordance with the NSD approval and their requirements for informed consent. The data were anonymized to not breech privacy. There was no direct contact between participants and researchers.
Statistics
Data were exported from SurveyXact’s database into IBM Statistical Package for Social Sciences (SPSS, IBM Corp. Released 2017. IBM SPSS Statistics for Windows, version 25.0, Armonk, NY: IBM CORP). Before analysing, the data were coded, controlled and checked against the responses to ensure accuracy. Open-ended answers were reviewed and placed into already existing categories if possible or redefined as a new category. A Pearson’s Chi-square test was performed to test the correlation among usage of magnification aids, EAL, motor-driven instrumentation and rubber dam. The level of significance was set at 5%.
Results
Response rate
Of the 459 dentists invited to participate, 314 (68.4%) answered the questionnaire. Of these, 15 respondents could not proceed with the survey as they did not perform RCT (n = 10, 3.2%) or were specialists in Endodontics (n = 5, 1.6%). Five participants gave only partial answers and did not complete the survey. This resulted in 299 to 304 respondents, a response rate of at least 65%. We did not receive any response from 145 dentists. One reason for this could be that we used registered contact information during UG education. Dentists who have changed their email address and telephone number would not have received the invitation to participate. Another reason could be that the electronic survey invitation via email address may have ended up in the ‘junk email’ folder and participants may not have checked this folder during the data collection period.
The response rate out of total survey population categorized according to year of graduation and gender is presented on . There were no significant differences in year of education and response rate. The distribution of the respondents’ general information is presented in . Of the respondents, 183 (58.3%) graduated between 2008 and 2013 (older graduates) and 131 (41.7%) graduated between 2014 and 2018 (newer graduates). The survey invitation was sent to a larger proportion of female (n = 224) than male (n = 128) dentists (). Sorted by gender there were 87 male respondents out of 128 potential male participants, which gave a response rate of 68.0% for male DPs. There were 224 female respondents out of 331 potential female participants, which gave a response rate of 67.7% for female DPs. The response rate between gender was similar. Three respondents (0.9%) did not disclose their gender.
Table 1. Distribution of total survey population and respondents in numbers (n) and percentage (%).
Table 2. Distribution of the respondents’ general information and practitioner characteristics (n = 303–314).
Majority of respondents were female dentists (71%) who were equally distributed between public sector (49.5%) and private practice (50.5%). Among male dentists, only 25.3% worked in the public sector. A significantly larger number of male DPs worked in private practice compared with female (p < .001). Eighty-five (28.0%) DPs did not have the possibility to refer to an endodontist, while three (1.0%) DPs reported that they prefer not to refer to an Endodontist [].
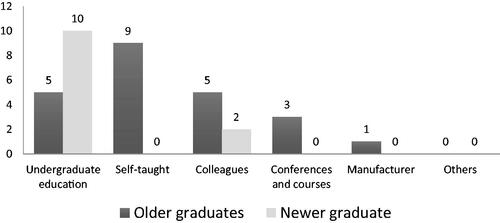
Magnification
More than half the respondents (n = 180, 59.6%) used some form of magnification when performing RCT. Of these, 145 (80.6%) used dental loupes and 35 (19.4%) used DOM. There was a tendency for newer graduates (65.9%) to use some form of magnification compared with older graduates (54.9%) (p = 0.059). A significantly higher number of DPs in private practice (80%) used some form of magnification (DOM and dental loupes) (p < .01). Magnification aids were used by 69.9% of the male DPs and 52.3% of the female DPs. However, there were significantly more female DPs who did not use any form of magnification (p < .01). Of the dentists who used DOM, the most frequent response as to where they learnt to use it was during UG education (42.5%) followed by self-taught (25.7%) and colleagues (20.0%) (). There were no significant differences between older and newer graduates (p = .054) on the use of the DOM as a form of magnification.
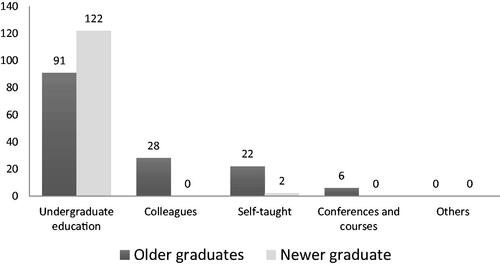
Electronic apex locators
When determining working length, 242 (80.1%) DPs used both EAL and radiographs, 29 (9.6%) used only EAL and 31 (10.3%) used only radiographs. Significantly more newer graduates (94.7%) used EAL compared with older graduates (80.3%) (p < .001). Significantly more newer graduates (90.8%) reported they learnt to use EAL during UG education compared with older graduates (69.4%) (p = .002) (). Of all the DPs who used the EAL, the most frequent response as to where they learnt to use it was during UG education. There were no significant differences between male and female DPs or DPs in private versus public sector on the use of EAL.
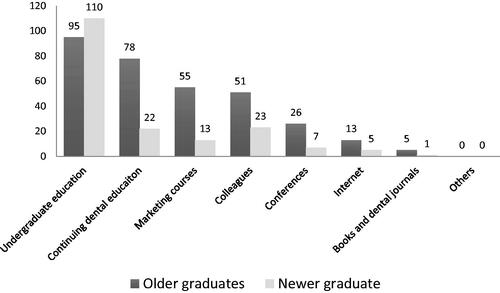
Instrumentation
Motor-driven file systems were used by 93.4% of the DPs. Twenty (6.6%) respondents used only hand files for instrumentation. Of the 20 DPs who used only hand files, 13 (65%) were older graduates and 7 (35%) were newer graduates; 16 (80%) were female and 4 (20%) were male DPs; 17 (85%) used the rubber dam; 6 (30%) used some form of magnification; 18 (90%) used EAL and 12 (60%) worked in private practice. There were no significant differences between older and newer graduates with regards to the use of motor-driven file system. Information on where the participants learnt to use motor-driven files is presented in . Significantly more newer graduates stated that they learnt to use motor-driven files during UG education (p < .001).
Figure 3. Number of the DPs reporting where they learnt to use motor-driven instrumentation (n = 281). Respondents could select more than one option for this question.
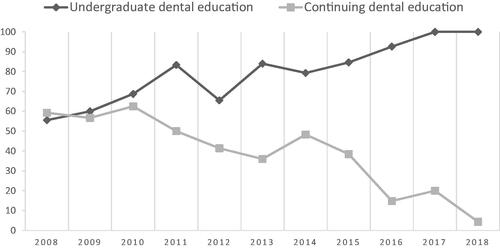
Results as to where DPs acquired the knowledge for their choice of instrumentation method (). Significantly more newer graduates (90.1%) based their instrumentation method on what they had learnt during UG education (p < .001). The next most frequent communication channel for newer graduates was colleagues (30.5%) (). For older graduates, the most frequent response was also UG education (65.6%) followed by continuing dental education (48.6%). When these two main forms of communication channel were selected, all of graduates from 2018 performed instrumentation based on what they had learnt during UG education, while around half of the graduates from 2008 performed instrumentation based on what they had learnt during UG education and half from continuing dental education ().
Figure 4. Number of the DPs reporting where they acquired knowledge for their current instrumentation method (n = 304). Respondents could select more than one option for this question.
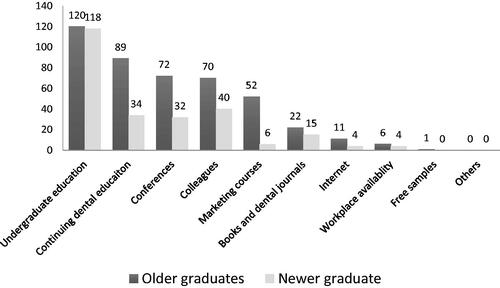
Figure 5. Plot showing percentage of DPs who selected undergraduate dental education and continuing dental education against year of graduation. All of graduates from 2018 performed instrumentation based on what they learnt during undergraduate dental education while around half of graduates from 2008 performed instrumentation based on what they had learnt during undergraduate dental education and the other half from continuing dental education.
Rubber dam
Rubber dam use for all RCT procedures was reported by 280 (93%) DPs, while 16 DPs (5.3%) reported using rubber dam sometimes and 5 DPs (1.7%) reported never using rubber dam. Significantly more female DPs always used rubber dam (p < .05) when compared with male DPs. Dentists who applied rubber dam sometimes during treatment procedures placed them on maxillary and mandibular posterior teeth. The least frequent tooth isolated with rubber dam was the maxillary anterior teeth. Significantly higher number of DPs in private practice did not use rubber dam (p < .01). Of the five dentists who never placed rubber dam, four were male and one female, and all of them worked in private practice. Three of these “non-rubber dam users” performed RCT more than 10 times a month. There were no significant differences in use of rubber dam between newer and older graduates.
There was significant correlation in the usage of magnification aids (DOM and dental loupes), EAL, motor-driven files and rubber dam. DPs who used magnification aids also used rubber dam (p < .001), EAL (p < .01) and motor-driven files (p < .01). However, a similar correlation was not observed between the use of EAL and motor-driven files, EAL and rubber dam, and motor-driven files and rubber dam.
Discussion
The main findings from this survey are that DPs who use DOM, EAL and motor-driven files when performing RCT have learnt to use these tools during UG education. Majority of DPs have based their instrumentation method on what they had learnt during UG education. The most frequent communication channel after graduation was continuing dental education for older graduates and colleagues for newer graduates.
One advantage of this study was that the survey participants were former students and therefore, we had knowledge of the education they had received. UG education at the University of Bergen (UoB), Norway is based on the European Society of Endodontology (ESE) guidelines [Citation8]. After a five-year long dental education, newly graduated dentists are expected to possess the skills and knowledge to perform a wide range of clinical dental procedures independently in accordance to the ESE guidelines [Citation8]. This survey revealed that around one in three (29%) DPs did or could not refer their patients to an Endodontist. It is therefore important that DPs possess a level of skill where they can perform a wide range of dental procedures independently. Failing to provide appropriate endodontic treatment can result in patients living with pain, chronic periapical disease, or tooth loss with or without expensive replacement therapy.
Technology plays a crucial role in current endodontic practice. However, technology evolves over time. The DOM, EAL and motor driven instrumentation were technological aids that were integrated into UG education when relocating to a new building. To compare how integration of technology during UG education influenced the adoption of technology by DPs, participants were divided into two cohorts; older and newer graduates. Newer graduates received endodontic education in a new building with integrated technological aids during UG education. Older graduates had only limited exposure and use of technological aids.
Magnification
Magnification tools are essential to endodontic practice. The position of the American Association of Endodontists on DOM is that it is an integral and important part of the performance of modern endodontic techniques [Citation1]. Magnification along with illumination is pertinent to localize calcified root canals, remove root canal obstructions and repair iatrogenic perforations. It is not necessary to use DOMs for the entire RCT procedure nor on teeth in minimal case difficulty category [Citation9]. Although the implementation of DOM in postgraduate training is compulsory, this is not the case for UG education. A recent survey revealed that not all educational institutions teach UG students the use of DOM during endodontic procedures [Citation10]. Results from this survey revealed that only about one-tenth of DPs (11.6%) have integrated the use of DOM. However, a larger number of newer graduates used some form of magnification, for example, dental loupes when performing RCT. One of the limitations of this survey is that only those who selected the use of DOM could proceed to the next question as to where they learned it. In this case, both older and newer graduates who use DOM frequently state that they have learnt to use it during UG education. Older graduates were made aware of DOM through demonstrations, seminar and in a few selected cases, during patient treatment. Therefore, it is interesting to observe that awareness to technology during UG education was adequate for older DPs to select that they had learned it during UG education. Furthermore, it is easier to be “self-taught” when one is made aware of technology.
Electronic apex locators
EAL, like DOM, has undergone minimum change since its introduction and needs to be learned only once. The use of EAL before taking working length radiograph reduces the number of radiographs and radiation exposure on patients. A significantly higher number of newer graduates used EAL in clinical practice and stated that they learned it during UG education. This shows that integration of technology during UG education has resulted in DPs using these tools. Although only a few EALs were available for older graduates, those who have integrated this technology to their clinical practice have stated that they learnt to use it during UG education.
Instrumentation
In this study, both older and newer graduates used motor-driven file systems with no significant differences between the groups. Metallurgical advances and new design concepts on file systems have made instrumentation reliable, efficient and user-friendly. Motor-driven nickel-titanium rotary file instrumentation was introduced in the preclinical training in 2008. However, rotary files were not commonly used during patient treatment as students found it cumbersome to change program each time a new file was used and fear for file separation [Citation9]. The rotary files were replaced in 2014 with a reciprocating file system which was considered as ‘new’ technology and easy-to-use [Citation9].
Adoption of innovation
According to Rogers’ theory, adoption of innovation occurs in five stages: awareness, interest, evaluation, trial and adoption [Citation5]. In this study, awareness of technology such as DOM and EAL during dental education through clinical demonstrations for older graduates has resulted in adoption of this technology later in career.
Adoption of new technology is a complex interplay of perceived benefits and advantages, and psychosocial and behavioural factors in decision making for a DP [Citation11]. In this study, a fraction of older graduates had not adopted new technology such as magnification tools or EALs. The reason for this could be because they were not aware of these technologies, nor the advantages and benefits associated with the use of these technology. A survey in UK showed that lack of training was the most frequent reason for not adopting nickel-titanium rotary instrumentation by general dental practitioners [Citation12]. Dental education program that provides minimal clinical training without exposure to new technology places newly graduated DPs at a disadvantage. Training can be provided during UG education or by providing continuing dental educational programs. Awareness of technology is the first stage for adoption of innovation. Next the DP must be interested with an understanding of the advantages and the importance of technology. To evaluate the benefits and advantages of a particular technology, some form of training is required. Final adoption of innovation occurs after a period of trial. Training courses can be time-consuming, costly, and perhaps not available. According to this study, after graduation, continuing dental education, conferences and marketing courses have been an essential form of communication channel for adoption of technology while books, journals and internet have had little influence. Lifelong learning to improve knowledge, skills and competence is important so that patients receive optimal dental care. Koch et al. confirmed that continuing dental education with hands-on training resulted in successful adoption and integration of technology for DPs [Citation13]. In our recent study, the majority of DPs indicated that UG education provided inadequate clinical training and that hand-on courses were the most preferred mode of learning after graduation [Citation14]. Therefore, to provide an opportunity for lifelong learning through continued dental education program is imperative and may be a task for educational institutions.
Colleagues
An interesting finding with this study is the role played by colleagues on adoption of technology by newer graduates. Newer graduates in this study have adopted the use of technology such as DOM, EAL, motor-driven files and based for their instrumentation methods from colleagues as well as UG education. However, it is questionable as to what colleagues can teach a new DP. Colleagues play an important role in acclimatizing a newly graduated dentist into a workplace environment. However, in some situations, learning from colleagues may not be ideal if the colleague does not have an academic background nor follow standard of care during patient treatment. It is an established fact that many dentists do not practice what they were taught as students once they have graduated [Citation15–17]. It is apparent that learning habits from colleagues may have led to dentists not practicing what they were taught as students. Unfortunately, use of rubber dam for isolation is one such practice that is often neglected during RCT [Citation6,Citation16,Citation18].
Rubber dam
Rubber dam is not a new technology. Nevertheless, it was included in this study to serve as a control on the impact of dental education on daily dental practice after graduation. Rubber dam isolation during RCT is the standard of care and mandatory when performing RCT procedures during UG education [Citation19]. Unfortunately, studies have shown the use of rubber dam by general practitioners can be as low as 3.4% indicating a mismatch between daily practice and academic teaching [Citation16]. In this study, 93% of the dentists used rubber dam when performing RCT. This high response is comparable to other surveys performed in Norway and Sweden [Citation13,Citation20,Citation21]. It is however disappointing that 7% of our graduates do not adhere to the standard of care when treating patients. According to this study, 7% of DPs did not practice what they were taught during UG education.
The phenomenon of “technology cluster” was observed in this study as well [Citation6]. DPs who used magnification aids also used rubber dam, EAL and motor-driven files. This study confirms that adoption of technological aids among general DPs did not occur in isolation. However, this finding was only applicable to DPs who used magnification aids.
Conclusion
UG education is a communication channel with long-lasting importance for adoption and integration of technological aids by DPs. Exposure to innovations (awareness) during UG education is adequate for adoption and integration of technology. Continuing dental education is as valuable as UG education for adoption of technology for older graduates.
Disclosure statement
The authors report there are no competing interests to declare.
Additional information
Funding
References
- Amercian Association of Endodontists AAE position statement. Use of microscopes and other magnification techniques. J Endod. 2012;38(8):1153–1155.
- Selden HS. The role of a dental operating microscope in improved nonsurgical treatment of "calcified" canals. Oral Surg Oral Med Oral Pathol. 1989;68(1):93–98.
- Hoer D, Attin T. The accuracy of electronic working length determination. Int Endod J. 2004;37(2):125–131.
- Parashos P, Messer HH. Questionnaire survey on the use of rotary nickel-titanium endodontic instruments by australian dentists. Int Endod J. 2004;37(4):249–259.
- Rogers EM, editor. Diffusion of innovations. New York (NY): The Free Press; 1983.
- Bjørndal L, Reit C. The adoption of new endodontic technology amongst danish general dental practitioners. Int Endod J. 2005;38(1):52–58.
- Abbott PV. Endodontics – current and future. J Conserv Dent. 2012;15(3):202–205. Jul
- European Society of Endodontology. Undergraduate curriculum guidelines for endodontology. Int Endod J. 2013;46(12):1105–1114.
- Haug SR, Solfjeld AF, Ranheim LE, et al. Impact of case difficulty on endodontic mishaps in an undergraduate student clinic. J Endod. 2018;44(7):1088–1095.
- Brown MG, Qualtrough AJE, McLean W. Magnification in undergraduate endodontic teaching in the UK and Ireland: a survey of teaching leads in endodontology. Int Endod J. 2020;53(4):553–561.
- Parashos P, Messer HH. The diffusion of innovation in dentistry: a review using rotary nickel-titanium technology as an example. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(3):395–401.
- Locke M, Thomas MB, Dummer PM. A survey of adoption of endodontic nickel-titanium rotary instrumentation part 1: general dental practitioners in Wales. Br Dent J. 2013;214(3):E6.
- Koch M, Eriksson HG, Axelsson S, et al. Effect of educational intervention on adoption of new endodontic technology by general dental practitioners: a questionnaire survey. Int Endod J. 2009;42(4):313–321.
- Haug SR, Linde BR, Christensen HQ, et al. An investigation into security, self-confidence and gender differences related to undergraduate education in endodontics. Int Endod J. 2021;54(5):802–811.
- Silversin JB, Shafer SM, Sheiham A, et al. The teaching and practice of some clinical aspects of endodontics in Great Britain. J Dent. 1975;3(2):77–80.
- Slaus G, Bottenberg P. A survey of endodontic practice amongst Flemish dentists. Int Endod J. 2002;35(9):759–767.
- Whitworth JM, Seccombe GV, Shoker K, et al. Use of rubber dam and irrigant selection in UK general dental practice. Int Endod J. 2000;33(5):435–441.
- Hommez GM, Braem M, De Moor RJ. Root canal treatment performed by Flemish dentists. Part 1. Cleaning and shaping. Int Endod J. 2003;36(3):166–173.
- Amercian Association of Endodontists. Dental Dams, https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/dentaldamstatement.pdf. J Endod. 2017. [Accessed 2022 Apr 9].
- Bletsa A, Iden O, Sulo G, et al. Work experience influences treatment approaches in endodontics: a questionnaire survey among dentists in Western Norway. Acta Odontol Scand. 2019;77(8):617–623.
- Malmberg L, Hagg E, Bjorkner AE. Endodontic infection control routines among general dental practitioners in Sweden and Norway: a questionnaire survey. Acta Odontol Scand. 2019;77(6):434–438.