Abstract
Background Cementing technique is a crucial factor in prosthesis fixation. No randomized studies have been published, however, comparing the outcome of conventional fingerpacking with the outcome of pressurization of the cement prior to cup insertion.
Patients and methods We randomized 50 THAs to either fingerpacking or sequential pressurization (including individual pressurization of each anchorage hole) and followed the patients with RSA for 5 years. The penetration of cement into the anchorage holes was measured on digital radiographs. Postoperative radiolucent lines around the cup were correlated to later RSA results. For clinical evaluation, we used SF-36 and HHS.
Results The pressurized group of THAs was more stable regarding changes in inclination. We found no other difference in the migratory behavior. The cement penetration into the anchorage holes was deeper with the pressurization technique than with fingerpacking. For the whole group taken together, there was a strong relation between the presence of radiolucent lines as measured on the postoperative radiograph and later migration observed by RSA at 2 and 5 years.
Interpretation Pressurization of the cement produced better cement penetration and increased the cup stability in terms of changes in inclination. Early findings of radiolucent lines can predict later unfavorable cup migration.
Improved cementation techniques, on both the femoral and the acetabular sides, are said to be a main cause of increased implant survival because of better interlock of the cement with the bone bed and tighter closure of the interface to prevent infiow of debris (Schmalzried et al. Citation1992, Malchau et al. Citation1993, Mulroy et al. Citation1995, Ranawat et al. Citation1997).
Despite better cementing techniques, the long-term result of cemented cups is still a problem. For long follow-ups, acetabular loosening predominates over femoral loosening (Ranawat et al. Citation1995, Mulroy and Harris Citation1997, Wroblewski et al. Citation1999, Callaghan et al. Citation2000, Berry et al. Citation2002). The use of uncemented acetabular cups has not increased the longevity, and higher revision rates have been reported (Havelin et al. Citation2000, Havelin et al. Citation2002).
The quality of initial cement fixation is of importance and pressurization of the cement is regarded an important component of improved cementing techniques. However, only fingerpacking of the cement into the acetabulum before cup insertion is still being used. There have been no studies published comparing the outcome of conventional fingerpacking with pressurization of the cement. In order to optimize cement pressurization, we have previously suggested-and successfully tested-a sequential cementation technique with pressurization of individual anchorage holes before filling the entire acetabular cavity with cement (Flivik et al. Citation2004).
Early radiolucency at the bone-cement interface as well as signs of early prosthetic migration correlate with later loosening (Hodgkinson et al. Citation1988, Freeman and Plante-Bordeneuve Citation1994, Kärrholm et al. Citation1994, Ranawat et al. Citation1995, Ryd et al. Citation1995, Thanner et al. Citation1995, Krismer et al. Citation1996, Garcia-Cimbrelo et al. Citation1997, Ritter et al. Citation1999). Radiostereometry (RSA) is the most precise way of detecting early prosthetic micromotion (Kärrholm et al. Citation1997).
With the hypothesis that our improved way of pressurizing the acetabular cement was superior to fingerpacking, we compared the two methods in a randomized, controlled clinical study. The patients were evaluated by RSA for 5 years and the quality of the bone-cement interface produced was evaluated on the initial radiographs, to be correlated against later migration of the acetabular component.
Patients and methods
Patients and clinical evaluation
The study comprised 50 total hip arthroplasties performed between 1996 and 1998 in 45 patients (26 men) with primary coxarthrosis. Only patients in Charnley class A (unilateral hip disease with no other disability) and class B (bilateral hip disease with no other disability) were included. The mean age was 65 (51–82) years and the mean Body Mass Index was 27 (SD 3.8).
During the follow-up period, 3 patients died and 1 did not want to continue because of cardiac failure. 2 patients were excluded, as no relevant RSA results could be obtained due to inadequate marking of tantalum beads in the bone. 1 cup was revised after 4 years because of suspected infection, but the cultures were negative. Thus, at the 5-year follow-up, 43 hips in 38 patients remained for analysis.
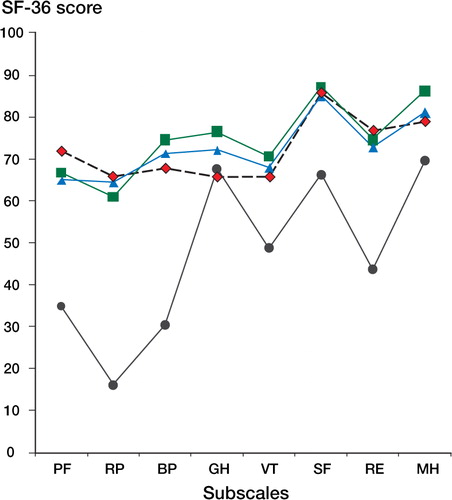
For clinical evaluation, we used Harris Hip Score and the self-administered quality of life questionnaire SF-36 preoperatively and at the 1-year follow-up. SF-36 was also registered at the 5-year follow-up examination.
The study was approved by the Ethics Committee of Lund University, and all patients gave their informed written consent.
Surgical procedure and randomization
All patients were operated on with a postero-lateral approach. Most operations were performed with normotensive spinal anesthesia. 5 surgeons performed the 50 operations, with 2 surgeons doing the majority of them (22 and 11, respectively). The acetabulum was prepared by reaming down to the subchondral bone, which should be slightly bleeding but if possible not perforated, according to practice in our department during that time period. 5 anchorage holes (9 mm diameter) were drilled, 3 in os ilium, 1 in os pubis and 1 in os ischi. 9 tantalum markers (0.8 mm diameter) were inserted into the periacetabular bone through the anchorage holes, and with as much spread as possible. The bone bed was thoroughly cleaned with pulsative lavage, and before cementing a cloth soaked in hydrogen peroxide was pressed into the acetabulum. We used pre-chilled Palacos, with Gentamicin bone cement (Schering-Plough, Belgium) in all cases. The cement was mixed using the Optivac, vacuum-mixing system (Biomet Cementing Technologies, Sweden).
The patients were randomized using closed envelopes which were opened in each case once the preparation of the acetabulum had been completed. The randomization determined whether the acetabular cement would be applied with fingerpacking (F) or by a sequential pressurization cementation procedure (SP). Of the 47 hips that could be analyzed, 24 were fingerpacked and 23 were sequentially pressurized.
In the fingerpacked group, the cement was applied into the acetabulum with the cement gun after 3–3.5 min, when the cement was no longer sticky. The cement was lightly moulded into the acetabulum using the finger. The cup was then inserted after 4–5 min, followed by light pressure until the cement had cured.
The sequential procedure included initial cementation of each individual anchorage hole via a silicone nozzle (outer diameter 15 mm; called the injector) attached to the tip of the cement gun. Subsequently, the rest of the acetabulum was filled with cement through a full-size pressurizer (called the compressor) replacing the nozzle at the tip of the gun (). Both the injector and the compressor were custom-made in silicone for this study. In the sequential pressurization group, cementation with the injector started at approximately 2 min after the start of cement mixing. Each hole was pressurized for 3–5 seconds. Subsequent cement filling of the rest of the acetabulum started (at the latest) at 3 minutes through the compressor, while it was covering the entire acetabulum. The pressure was maintained with the compressor until insertion of the cup at 4–5 minutes. Thereafter, light load was maintained on the cup until the cement had cured.
Prosthesis
We used the ScanHip system with the Opticup, in all patients (Biomet, UK). The cup was marked with 7–9 tantalum markers by the manufacturer, and was available in sizes of 46 to 56 mm.
Radiostereometry
RSA examinations were done by a uniplanar technique (Selvik Citation1989, Kärrholm et al. Citation1997), with the patient in supine position. The two X-ray sources were fixed (mounted to the ceiling). We used a type-41 calibration cage (Tilly Medical, Sweden) and the computer software UmRSA version 5.0 (RSA Biomedical, Sweden). The reference examination was done within 1 week of the operation and the follow-up examinations were done after 3 and 6 months and at 1, 2 and 5 years, with a time tolerance of 5–10%.
We set the cut-off level for exclusion of patients or of specific examinations at a condition number of 150 (an expression for how well the tantalum markers are inserted). For mean error of rigid body fitting (an expression for marker stability within the bone or prosthesis), the cut-off level was set at 0.35. In 3 cases the condition number regarding the cup segment was >150, and therefore the results for rotational migration in these cases were excluded, although their translation results were included.
We expressed the RSA analyses as rotation and translation about/along the three axes in an orthogonal coordinate system (6 degrees of freedom of motion). Of these, we selected proximal translation (Y-axis) and sagittal rotation (Z-axis) as primary effect variables. The precision of the RSA measurements was assessed by 40 double examinations of the patients in the study ().
Table 1. 99% confidence limits for significant movements. Values represent mean ±2.7 SD of the error obtained from 40 double investigations of patients in the study
Conventional radiographic evalution
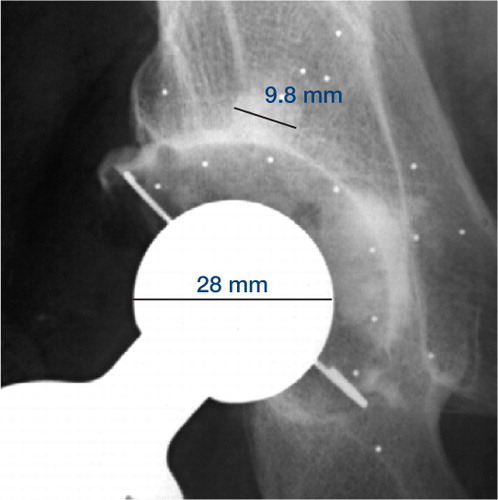
All patients had conventional radiographs taken postoperatively and at 1, 2 and 5 years, including anterior-posterior (AP) and lateral projections and a pelvic view centered over the symphysis. In order to measure cement penetration into the anchorage holes, special postoperative AP digital radiographs were also taken at a standardized angle to the cup. By fiuoroscopy, the X-ray tube was angled in the cranio-caudal direction to obtain an image tangential to the steel wire in the base of the acetabular component. Using a multimodality workstation (Fuji HIC654), the three individual anchorage holes in the os ilium, with their cement protrusions, could be separated (Flivik et al. Citation2004). The cement width of the medial/uppermost acetabular anchorage tap was then measured twice. We used the mean value of these two measurements. The widest part of the top of the tap was used for measurement (). The measured scale was calibrated for magnification using the known diameter of the patient′s prosthetic femoral component. The observer was free to optimize the digital image on the monitor before measurement with respect to magnification, contrast and density levels. With this possibility, in combination with the standardized positioning of the 3 anchorage holes of os ilium, the difficulty of distinguishing the cement protrusions from two adjacent anchorage holes was overcome. To assess the penetration of cement on each side of the anchorage hole, we used the mean value of the two measurements of the cement tap minus the width of the drill hole (9 mm) and divided by two. A radiologist, blinded as to the operative procedure, evaluated all the radiographs.
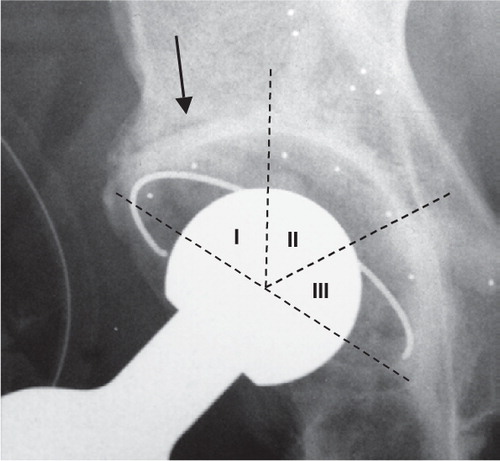
To evaluate the quality of the cement-bone junction around the acetabular component radiographically, the postoperative pelvic and AP-view radiographs were analyzed regarding the extent and width of any radiolucent line at the cement-bone interface (). Again, we used the diameter of the prosthetic femoral head to calibrate for magnification.
The examination was done with the use of a digital slide calliper with a 1/100 mm scale. The region around the acetabular components was divided into 3 equal zones of 60° (zone 1: outer lateral, zone 2: central, and zone 3: outer medial). The visual definition of radiolucency involves a gray zone. Therefore, in order not to overestimate the phenomenon, we considered a radiolucent line at the cement-bone interface to be present if there was a radiolucency width of > 0.3 mm (excluding the sclerotic demarcation) and a length of > 50% of the interface in that zone (Hultmark et al. Citation2003). We classified the demarcation of the bone-cement interface around the cup according to Hodgkinson et al. (Citation1988) with grade 0 meaning no demarcation, grade 1 meaning demarcation of the outer one-third, grade 2 meaning demarcation of the outer and middle one-third, and grade 3 signifying complete demarcation. Also, the inclination of the cup was determined with the teardrop line as reference.
In order to correlate the quality of the postoperative cement-bone interface with later loosening as measured by RSA, we analyzed all cases separately regarding their RSA results. They were classified into migrating or not, based on RSA values of the proximal migration (y-translation) and changes in inclination (z-rotation) between 1–2 years and 2–5 years. Previous studies have shown that migration before 1 year represents a healing phase with little prognostic value (Ryd et al. Citation1995). The cups that were migrating above the significant level of our RSA values in the above-mentioned intervals were classified as migrating, and the rest were classified as stable. We then assessed the 2 groups by type of demarcation measured on the postoperative radiographs.
Statistics
We used repeated measures ANOVA (MANOVA), including RSA values at 3 and 6 months and 1, 2 and 5 years. The results were adjusted for age, sex, BMI, Charnley group, cup inclination and surgeon by covariance analysis. To compare differences between groups at a given time, Student′s t-test was used. Comparison of results in the Cross tabulation was done by Fisher′s exact test. RSA results are given for signed values of migration. For analysis of the clinical outcome (SF-36 and HHS), we used the Wilcoxon test over time and the Mann-Whitney U-test for comparison between the groups.
The primary effect variable, used for power analysis, was proximal migration of the cup (y-transla-tion). With an assumption of a difference in means of 0.3 mm and an SD of 0.45 mm for both groups, and with the aim of reaching a power of 0.80 and a risk of 0.05 for type-1 error, 21 patients were needed in each group. To compensate for potential dropouts of patients and the fact that there are secondary effect variables, we decided to include 25 hips in each group.
We used SPSS software (version 11.0; SPSS Inc., Chicago, IL), and p > 0.05 was considered significant.
Results
Cement penetration
The penetration of cement into the anchorage holes was deeper with the sequential technique than with fingerpacking (p = 0.02). Given the anchorage hole diameter of 9 mm, the mean penetration on each side of the anchorage hole was 0.7 mm for the sequential technique and 0.2 mm for fingerpacking ().
Table 2. Cement penetration (mm) on each side of the uppermost medial anchorage hole
Radiostereometry
We found statistically significant differences between the two techniques in rotation around the sagittal axis (z-axis), i.e. differences in inclination of the cup (; ). The fingerpacked cups tilted towards a more horizontal position with a mean of 0.8° at 5 years and with a slight, but continuous, progression of the rotation. The sequentially pressurized cups rotated slightly towards a more vertical position, with a mean of −0.2° at 5 years, but they were more stable and reached this rotation after 6 months. The difference was significant as early as 6 months, and throughout the follow-up period. There was no significant difference between the two techniques in any other respect of measured migrations (6 variables for movement), either by using repeated measures ANOVA or by using the values at a given time measured by t-test. Non-parametric testing gave the same results. Adjustment for covariates in the MANOVA test (sex, age, BMI, Charnley group, cup inclination and surgeon (as a stochastic variable)) did not affect the outcome of the statistical analysis. The mean proximal migrations for all cups taken together were 0.6 mm at 5 years ().
Figure 4. Rotation around the sagittal axis (Z), i.e. changes in inclination, up to 5 years. Values are mean with 95% confidence intervals.
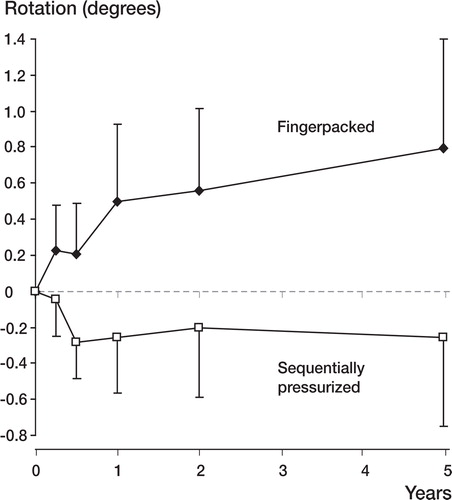
Figure 5. Proximal cup migration (Y-axis) up to 5 years. Values are mean with 95% confidence intervals.
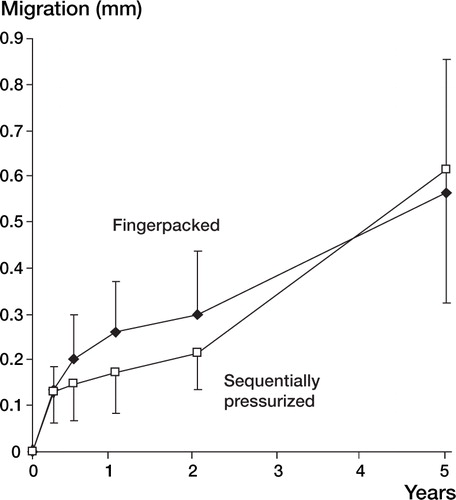
Table 3. Translations and rotations measured by RSA at the 5-year follow-up. Signed values
Radiographic evalution
There was no significant difference between the two groups regarding distribution of demarcation around the cup in the postoperative radiograph (p = 0.8, Mann-Whitney U-test) (). For the whole group taken together, however, there was a strong relationship between the presence and extension of demarcation (as measured on the postoperative radiograph) and the later findings of migration according to our classification at 2 and 5 years, respectively (p > 0.001 and p > 0.001, Fish-er′s exact test) (). At 2 years, none of the cups without demarcation were migrating, whereas 10 out of 29 of the cups with demarcation postoperatively (grade 1–3) were migrating. At 5 years, 2 out of 17 in the no-demarcation group showed signs of migration and in the group with demarcation postoperatively, 21 out of 27 were migrating (including the cup that was revised).
Figure 6. Distribution of migrating or stable cups determined by RSA at 2 and 5 years, respectively. Depending on the distribution of direct postoperative radiographical demarcation, all patients were grouped as grade 0 (no demarcation), grade 1 (outer 1/3), grade 2 (outer and middle 1/3) or grade 3 (complete demarcation).
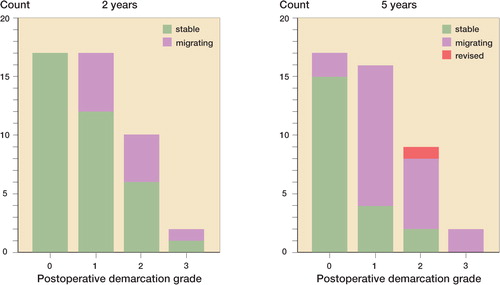
Table 4. Demarcation grades on immediate postoperative radiographs in the two groups (number).
Patients and clinical evaluation
There was no significant difference between the two groups preoperatively or postoperatively, either regarding SF-36 or Harris Hip Score. The patients improved between the pre- and postoperative assessments of quality of life, especially regarding physical functioning, role-physical and bodily pain (all three p < 0.001). This result persisted up to 5 years (). Harris Hip Score increased from a preoperative value of 43 (SD 11) to a 1-year score of 91 (SD 9) for the whole group (p < 0.001).
Figure 7. Mean values of SF-36 subscales preoperatively (—•—) and after 1 year (—▴—) and 5 years (—▪—) postoperatively, for all patients. Dotted line (--♦--) represents reference population for SF-36 collected from norms of the general Swedish population, comprising 2 184 subjects of corresponding age and sex (Sullivan et al. Citation1995). PF: physical functioning; RP: role-physical; BP: bodily pain; GH: general health; VT: vitality; SF: social functioning; RE: role-emotional, MH: mental health.
Discussion
This study confirms our previous finding that increased pressurization during acetabular cementation, with the use of a sequential pressurization technique, results in better penetration of cement into the anchorage holes (Flivik et al. Citation2004). Measured by RSA, this was refiected by a significant difference in inclination (i.e. rotation around the sagittal axis) between groups, observed early in the follow-up period (at 6 months) and persisting up to 5 years. We detected no other difference by RSA.
We could not find any statistical difference between the two groups, either pre- or postoperatively, regarding quality of life as measured by SF-36 (up to 5 years) or hip status as measured by Harris Hip Score (up to 1 year). This is not surprising, as early loosening of the cup often gives very few symptoms, and, furthermore, the differences in migration between the two groups were small.
Comparison with previous RSA reports is difficult because of alternative ways of presenting data, other methods of fixation and shorter follow-up. The only comparable RSA report on cemented cups with a 5-year follow-up in patients with osteoarthrosis, however, shows migrations of similar magnitudes as in our study (Önsten et al. Citation1998).
The use of some kind of pressurizer for cementing the acetabulum has been suggested as being superior to fingerpacking, and the efficiency of various acetabular pressurization devices has been evaluated (Lee and Ling Citation1974, Oh et al. Citation1983, Bernoski et al. Citation1998, New et al. Citation1999, Flivik et al. Citation2004). The reason for pressurizing the cement before insertion of the cup is that the penetration of cement is better when the cement has a lower viscosity. The effect of better pressurization in this study might not only be due to the pressure in itself, but also to the fact that we applied the cement in an earlier phase using the sequential technique. However, the study is one of cementation technique as a whole, and fingerpacking cannot be performed with the cement in the earlier (more sticky) stage. The cup cannot be introduced at the early stage either, as the cement will take the path of least resistance and leak out of the acetabulum around the advancing cup, where there is no counter-pressure. Thus, a pressurizer can be used to maintain the pressure once the cement has been applied into the acetabulum. However, the anatomy of the acetabulum presents particular difficulties for cement pressurization. It has a large surface area, a wide opening, and moreover, has a discontinuity of the wall under the transverse ligament, all of which make it difficult to achieve the high cement extrusion pressures needed for adequate cement penetration. A cement penetration of at least 2 mm but with an optimal depth of 3–5 mm is considered to give the strongest cement-bone interface (Krause et al. Citation1982, Askew et al. Citation1984, MacDonald et al. Citation1993). We have shown previously in experimental studies that pressures of 0.2–0.3 MPa (1500–2250 mmHg) are required to achieve penetrations of 3–4 mm on each side of the anchorage hole in arthrotic cancellous bone (Juliusson et al. Citation1995). It is not possible to achieve such high pressures—either with a conventional pressurizer or, as in this study, with a compressor through which the cement is delivered. We have reported peak cementation pressures in vivo (from inside one of the anchorage holes) of 480 mmHg for the compressor and 650 mmHg with a conventional pressurizer (Flivik et al. Citation2004). New et al. (Citation1999) reported similar in vivo results (570–700 mmHg) for the pressure produced using an instrumented pressurizer. Using an in vitro model, Parsch et al. (Citation2004) recently reported similar mean peak values at the cement-bone interface of 600 mmHg (80kPa) with an Exeter pressurizer and 548 mmHg (73kPa) with a Bernoski pressurizer. However, Oh et al. (Citation1983) recorded higher local pressures in vitro inside the anchorage hole when pressurizing the cement with a finger occluding the mouth of the hole, and therefore suggested a sequential cementation procedure. We have previously (Flivik et al. Citation2004) evaluated the in vivo sequential cementation procedure with an injector similar to the one used in the present study, and with the same type of compressor. In that study, we registered in vivo mean peak values during the injector phase of about 860 mmHg and achieved a mean of 2.8 mm of penetration with the sequential procedure, compared to 0.65 mm with a conventional pressurizer. Thus, the penetration results in the present study were lower than previously reported. It is possible that this is due to differences in the patient cohort and to less consistently applied technique because of the increased number of surgeons.
This study clearly supports previous reports that any demarcation at the bone-cement interface around the cup, observed on the immediate postoperative radiograph, is an important indicator of later loosening (Garcia-Cimbrelo et al. Citation1997, Hodgkinson et al. Citation1993, Ranawat et al. Citation1995, Ritter et al. Citation1999). Even a minor radiographical demarcation present postoperatively or emerging during the first year has been shown to lead to radiographical loosening in 35–40% within 10 years (Mulroy and Harris Citation1990, Hodgkinson et al. Citation1993, Garcia-Cim-brelo et al. Citation1997). Ritter et al (Citation1999) were able to show that radiolucency in zone 1 on the first postoperative radiograph had a 40% higher probability of later loosening than when no radiolucency was present. Our study has confirmed these results using RSA. Several authors have come to the conclusion that it is not the thickness of the gap but the length of the demarcation that is the most important factor (Hodgkinson et al. Citation1988, Schmalzried et al. Citation1992, Garcia-Cimbrelo et al. Citation1997, Hultmark et al. Citation2003) and some papers report demarcation irrespective of thickness. Hodgkinson et al. (Citation1988) reported that 94% of all cups with a complete demarcation, through all 3 zones and regardless of thickness, were loose by direct testing, whereas all cups showing no demarcation were solidly fixed. In our study, no demarcation was wider than 1 mm since the analysis was made on the direct postoperative radiograph.
Ritter (Citation2003) recently described the problems of preventing radiolucency occurring in zone 1. He concluded that despite their attempts over the years, early postoperative zone 1 radiolucency still occurred in 20–30% of cases. We had a high rate of type 1 and type 2 demarcations on the postoperative radiographs. We believe the reason for this to be the bone preparation technique we used, with retention of the subchondral bone plate. This has been recommended previously as an important measure for prevention of excessive stress concentrations in the periacetabular bone (Carter et al. Citation1983, Mulroy and Harris Citation1990, Kobayashi et al. Citation1994, Ziegler and Lachiewicz Citation1996). However, the biomechanical basis of this conclusion has been questioned (Sutherland et al. Citation2000) and further studies are in progress.
In conclusion, we have achieved improved penetration of cement in the anchorage holes with the sequential pressurization technique as compared to fingerpacking. This penetration had a stabilizing effect on changes in inclination, but it did not substantially improve the cup stability in other respects. We also found that early radiographical demarcation predicts later unfavorable cup migration as measured by RSA.
This work was supported by the Swedish Medical Research Council (project 09509), Stiftelsen för bistånd åt rörelsehindrade i Skåne, Region Skåne and the Medical Faculty of Lund University. We wish to thank Håkan Leijon of the RSA Laboratory, University Hospital, Lund, for help in computerizing the RSA pictures. Thanks also to Per-Erik Isberg, Department of Statistics, Lund University, for advice regarding statistics.
No competing interests declared
- Askew M J, Steege J W, Lewis J L, Ranieri J R, Wixson R L. Effect of cement pressure and bone strength on polymethylmethacrylate fixation. J Orthop Res 1984; 1: 412–420
- Bernoski F P, New A M, Scott R A, Northmore-Ball M D. An in vitro study of a new design of acetabular cement pressurizer. J Arthroplasty 1998; 13: 200–206
- Berry D J, Harmsen W S, Cabanela M E, Morrey B F. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am 2002; 84-A: 171–177
- Callaghan J J, Albright J C, Goetz D D, Olejniczak J P, Johnston R C. Charnley total hip arthroplasty with cement. Minimum twenty-five-year follow-up. J Bone Joint Surg Am 2000; 82-A: 487–497
- Carter D R, Vasu R, Harris W H. Periacetabular stress distributions after joint replacement with subchondral bone retention. Acta Orthop Scand 1983; 54: 29–35
- Flivik G, Wulff K, Sanfridsson J, Ryd L. Improved acetabular pressurization gives better cement penetration: In vivo measurements during total hip arthroplasty. J Arthroplasty 2004; 19: 911–918
- Freeman M A, Plante-Bordeneuve P. Early migration and late aseptic failure of proximal femoral prostheses. J Bone Joint Surg Br 1994; 76-B: 432–438
- Garcia-Cimbrelo E, Diez-Vazquez V, Madero R, Munuera L. Progression of radiolucent lines adjacent to the acetabular component and factors infiuencing migration after Charnley low-friction total hip arthroplasty. J Bone Joint Surg Am 1997; 79-A: 1373–1380
- Havelin L I, Engesaeter L B, Espehaug B, Furnes O, Lie S A, Vollset S E. The Norwegian Arthroplasty Register: 11 years and 73,000 arthroplasties. Acta Orthop Scand 2000; 71: 337–353
- Havelin L I, Espehaug B, Engesaeter L B. The performance of two hydroxyapatite-coated acetabular cups compared with Charnley cups. From the Norwegian Arthroplasty Register. J Bone Joint Surg Br 2002; 84-B: 839–845
- Hodgkinson J P, Maskell A P, Paul A, Wroblewski B M. Flanged acetabular components in cemented Charnley hip arthroplasty. Ten-year follow-up of 350 patients. J Bone Joint Surg Br 1993; 75-B: 464–467
- Hodgkinson J P, Shelley P, Wroblewski B M. The correlation between the roentgenographic appearance and operative findings at the bone-cement junction of the socket in Charnley low friction arthroplasties. Clin Orthop 1988; 228: 105–109
- Hultmark P, Hostner J, Herberts P, Kärrholm J. Radiographic evaluation of Charnley cups used in first-time revision: repeated observations for 7–15 years. J Arthroplasty 2003; 18: 1005–1015
- Juliusson R, Flivik G, Nilsson J, Ryd L, Önnerfält R. Circulating blood diminishes cement penetration into cancellous bone. In vivo studies of 21 arthrotic femoral heads. Acta Orthop Scand 1995; 66: 234–238
- Kärrholm J, Borssen B, Löwenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4–7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg Br 1994; 76-B: 912–917
- Kärrholm J, Herberts P, Hultmark P, Malchau H, Nivbrant B, Thanner J. Radiostereometry of hip prostheses. Review of methodology and clinical results. Clin Orthop 1997; 344: 94–110
- Kobayashi S, Eftekhar N S, Terayama K, Iorio R. Risk factors affecting radiological failure of the socket in primary Charnley low friction arthroplasty. A 10- to 20-year followup study. Clin Orthop 1994; 306: 84–96
- Krause W R, Krug W, Miller J. Strength of the cement-bone interface. Clin Orthop 1982; 163: 290–299
- Krismer M, Stockl B, Fischer M, Bauer R, Mayrhofer P, Ogon M. Early migration predicts late aseptic failure of hip sockets. J Bone Joint Surg Br 1996; 78-B: 422–426
- Lee A J, Ling R S. A device to improve the extrusion of bone cement into the bone of the acetabulum in the replacement of the hip joint. Biomed Eng 1974; 9: 522–524
- MacDonald W, Swarts E, Beaver R. Penetration and shear strength of cement-bone interfaces in vivo. Clin Orthop 1993; 286: 283–288
- Malchau H, Herberts P, Ahnfelt L. Prognosis of total hip replacement in Sweden. Follow-up of 92,675 operations performed 1978–1990. Acta Orthop Scand 1993; 64: 497–506
- Mulroy R D, Jr., Harris W H. The effect of improved cementing techniques on component loosening in total hip replacement. An 11-year radiographic review. J Bone Joint Surg Br 1990; 72-B: 757–760
- Mulroy W F, Estok D M, Harris W H. Total hip arthroplasty with use of so-called second-generation cementing techniques. A fifteen-year-average follow-up study. J Bone Joint Surg Am 1995; 77-A: 1845–1852
- Mulroy W F, Harris W H. Acetabular and femoral fixation 15 years after cemented total hip surgery. Clin Orthop 1997; 337: 118–128
- New A M, Northmore-Ball M D, Tanner K E, Cheah S K. In vivo measurement of acetabular cement pressurization using a simple new design of cement pressurizer. J Arthroplasty 1999; 14: 854–859
- Oh I, Merckx D B, Harris W H. Acetabular cement compactor. An experimental study of pressurization of cement in the acetabulum in total hip arthroplasty. Clin Orthop 1983; 177: 289–293
- Önsten I, Carlsson A S, Besjakov J. Wear in uncemented porous and cemented polyethylene sockets: a randomised, radiostereometric study. J Bone Joint Surg Br 1998; 80-B: 345–350
- Parsch D, Diehm C, New A M, Schneider S, Breusch S J. A new bleeding model of the human acetabulum and a pilot comparison of 2 different cement pressurizers. J Arthroplasty 2004; 19: 381–386
- Ranawat C S, Deshmukh R G, Peters L E, Umlas M E. Prediction of the long-term durability of all-polyethylene cemented sockets. Clin Orthop 1995; 317: 89–105
- Ranawat C S, Peters L E, Umlas M E. Fixation of the acetabular component. The case for cement. Clin Orthop 1997; 344: 207–215
- Ritter M A. Acetabular options. J Arthroplasty 2003; 18: 80–81
- Ritter M A, Zhou H, Keating C M, Keating E M, Faris P M, Meding J B, Berend M E. Radiological factors infiuencing femoral and acetabular failure in cemented Charnley total hip arthroplasties. J Bone Joint Surg Br 1999; 81-B: 982–986
- Ryd L, Albrektsson B E, Carlsson L, Dansgard F, Herberts P, Lindstrand A, Regner L, Toksvig-Larsen S. Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg Br 1995; 77-B: 377–383
- Schmalzried T P, Kwong L M, Jasty M, Sedlacek R C, Haire T C, O′Connor D O, Bragdon C R, Kabo J M, Malcolm A J, Harris W H. The mechanism of loosening of cemented acetabular components in total hip arthroplasty. Analysis of specimens retrieved at autopsy. Clin Orthop 1992; 274: 60–78
- Selvik G. Roentgen stereophotogrammetry. A method for the study of the kinematics of the skeletal system. Acta Orthop Scand (Suppl 232) 1989; 60: 1–51
- Sullivan M, Karlsson J, Ware J E, Jr. The Swedish SF-36 Health Survey--I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Soc Sci Med 1995; 41: 1349–1358
- Sutherland A G, D′Arcy S, Smart D, Ashcroft G P. Removal of the subchondral plate in acetabular preparation. Int Orthop 2000; 24: 19–22
- Thanner J, Freij-Larsson C, Kärrholm J, Malchau H, Wesslen B. Evaluation of Boneloc. Chemical and mechanical properties, and a randomized clinical study of 30 total hip arthroplasties. Acta Orthop Scand 1995; 66: 207–214
- Wroblewski B M, Fleming P A, Siney P D. Charnley low-frictional torque arthroplasty of the hip. 20-to-30 year results. J Bone Joint Surg Br 1999; 81-B: 427–430
- Ziegler B S, Lachiewicz P F. Survivorship analysis of cemented total hip arthroplasty acetabular components implanted with second-generation techniques. J Arthroplasty 1996; 11: 750–756