Abstract
Background To overcome the mismatch between a stiff stem and the more elastic bone, the concept of isoelasticity was introduced in the 1970s. This concept was based on the assumption that the implant and the bone should deform as one unit to avoid stress shielding. The Robert Mathys (RM) cementless total hip replacement (THR) was one of the earliest isoelastic designs.
Patients and methods From 1984 to 1987, we performed 149 total hip replacements in 135 patients (92 women, mean age 47 (21-72) years) using third-gen-eration Mathys isoelastic polyacetal stem with stain-less-steel heads and polyethylene cementless acetabular cups. 11 patients died before revision or before the examination for this study, and 14 were lost to follow-up. Average follow-up time for the remaining 110 patients was 15 (14-17) years.
Results To date, 69 hips (64 patients) have been revised, 5 due to infection. The 10-year survival rate for any reason was 70% (66-74). In the 46 remaining patients (53 hips), the average HHS was 80 (39-100) points. 13 of these were regarded as radiographic failures, with an average HHS of 75 points.
Interpretation The performance of this prosthesis was unacceptably poor. Higher debris production and poor primary fixation are believed to be the main reason for the high failure rate.
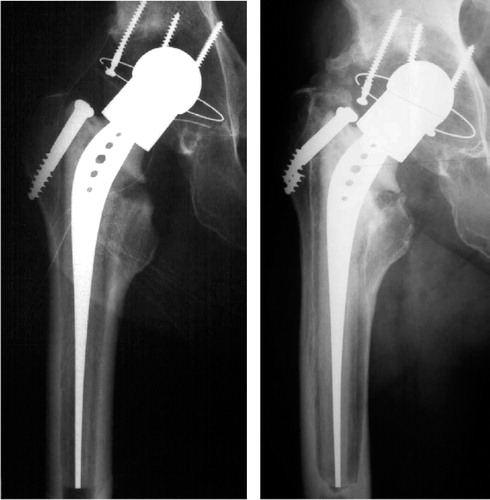
To overcome the mismatch between a stiff stem and the more elastic bone (Huiskes et al. Citation1992), the concept of isoelasticity was introduced (Morscher and Mathys Citation1974, Citation1975). This concept is based on the assumption that the implant and the bone should deform as one unit to avoid stress shielding (Bombelli and Mathys Citation1982, Andrew et al. Citation1986). The Robert Mathys (RM) isoelastic total hip replacement (THR) was one of the earliest cement-less designs (Morscher and Mathys Citation1974, Citation1975) (). Polyacetal resin seemed to be a good choice for the femoral part, since it had a modulus of elasticity similar to that of bone, good tensile strength, and durability. A stainless steel core was added to avoid over-elasticity in the neck region (Bombelli and Mathys Citation1982). Polyethylene was chosen for the acetabular part since polyacetal resin exhibited poor wear characteristics in the concave surface configuration (Morscher et al. Citation1982). The direct contact between bone and the polyethylene cup was believed to adjust to the deformation of the pelvis (Morscher et al. Citation1982).
Figure 1 The acetabular and femoral components of the third-generation iso-elastic RM total hip replacement.

The first results of the isoelastic RM prostheses were considered promising. 2 years after surgery, 92% of 400 patients had a good result (Andrew et al. 1986). Only 2 cases of aseptic loosening of the stem were observed. The study included the third-generation prostheses with a length of 180 mm and an uncoated polyethylene cup (Andrew et al. Citation1986). Bombelli reported that 96% of 614 patients had shown good or satisfactory results at a minimum of 2 years after surgery (Bombelli and Mathys Citation1982). Träger (Citation1989) reported 5 to 7-year follow-up results in 71 patients with the second-generation prostheses, which had a length of 140 mm and uncoated cup. The revision rate due to aseptic loosening was about 10%. Rosso (Citation1988) reported similar overall clinical results with 59% excellent or good, 31% fair and 11% poor results in 92 patients after 5 years. Initially, optimistic results of isoelastic THRs were somewhat overshadowed when Ninimaki et al. (Citation1994) reported a 7 to 9-year follow-up of 85 RM prostheses. 10% of the stems were revised and the radiographic failure rate was 25%. Recently, short-term results have been published on modern prostheses with reduced stiff-ness-the Epoch design (Glassman et al. Citation2001, Kärrholm et al. Citation2002).
Here we report the 14-17-year outcome in follow-up of a consecutive series of patients treated with the RM total hip replacement. To our knowledge, this study describes the longest follow-up results of this particular prosthesis.
Patients and methods
Between the years 1984 and 1987, 149 consecutive RM total hip replacements (Robert Mathys Co, Bettlach, Switzerland) were implanted in 135 patients (92 women) at our institution. The average age at the time of the index surgery was 47 (21-72) years. There were 68 right hips and 81 left hips. A patient was more apt to have a cementless RM hip replacement if he or she was under 50, had good bone stock and was expected to have increased demands on the artificial joint. The preoperative diagnosis was primary osteoarthrosis in 73 hips, rheumatoid arthritis in 10, osteonecrosis in 14, and osteoarthrosis secondary to congenital dislocation in 17, to trauma in 18, and to other conditions in 17. All operative procedures were performed through a direct lateral (Hardinge Citation1982) or an anterolateral surgical approach (McFarland and OsborneCitation1954). Templating was used preoperatively to determine the sizes of the components intended to be implanted. The operations were carried out by 5 skilled and experienced surgeons who performed a large number of THRs each year. All operations were performed in strict aseptic conditions with vertical laminar-flow OR.
The femoral stem was produced from a polyoxymethylene (polyacetal) resin with a central stain-less-steel reinforcement and a modular femoral head of stainless steel. The acetabular component was made of high-density polyethylene HDPE (). The femoral stem had circumferential crosshatchings on its proximal third and was quadrilaterally grooved distally.
The acetabular component was non-modu-lar. On the surface there were circular grooves and two pegs for firm anchorage and to resist rotational forces. The holes for the pegs were drilled using a special guide, so that they had an angle of difference of 5 degrees, compared with the pegs themselves. This allowed the cup to be press-fitted into the reamed acetabular bone, thus achieving primary stability. There were four screw holes in the cup. To enhance primary stability further, special screws were used in 135 hips. The acetabular components were available as standard and deep-pro-file designs.
For placement of the femoral component, a large pilot hole was made in the piriformis fossa to ensure correct alignment of the straight intramedullary drills used to prepare the femoral canal. In the next step, the canal was prepared with cylindrical and conical reamers in the diaphyseal and metaphyseal region, to fit the desired shape and size. Our goal was to use a femoral prosthesis that was large enough to contact both the medial and the lateral endosteal cortex of the femoral canal at the femoral isthmus, as determined by the templates (Pisot Citation1993). The prosthesis was fixed with press-fit in the prepared bone bed. Further fixation was obtained by two lag screws inserted through its proximal part to distribute the tension forces from the prosthesis to the trochanteric bone. Femoral heads of 32 mm in diameter were available with neck lengths that varied from 28 to 44 mm. The head fitted onto the conical neck by means of a Morse taper and was further secured with a silicone ring.
All acetabular components were inserted without cement. The cups were transfixed with 4 screws in 8 hips, 3 screws in 25, 2 screws in 94 and 1 screw in 8 hips. In 14 hips, no screws were used. In 2 cases with osteoarthrosis secondary to trauma, 1 peg was removed from the socket to allow insertion without removing osteosynthetic material from the acetabulum. Acetabular roof augmentation with an autologous graft fixed with screws was performed in 8 hips. The median size of the acetabular component was 52 (50-62) mm. The corresponding stem length and stem diameter were 180 (140-180) mm and 14 (8-18) mm, respectively. A 32-mm stainless steel (AISI 316L) femoral head with a median neck length of 34 (28-44) mm was used. Tenotomy of the adductors was done in 1 case. Postoperatively, the patients were partially weight bearing for the first 3 months. Heparin was not given routinely for prophylaxis against deep-vein thrombosis. To prevent infection, first-generation cephalosporin was administrated perioperatively in the last 75 cases, after the praxis was instituted in our hospital in 1986.
Clinical outcome
Patients were assessed 3, 6 and 12 months after the index operation and according to their own judgment thereafter. 14-17 years after the index operation, attempts were made to contact the patients who had not been revised or clinically examined recently. Observers other than the operating surgeon performed all clinical evaluations. Patients were asked to return for a clinical examination, and those who could not come answered a telephone questionnaire. The national death statistics bureau was contacted to confirm the number of deaths. Any complication related to the hip arthroplasty or revision of the femoral or acetabular component was recorded, and survival statistics were calculated. Postoperative evaluation included pain assessment in 43 of 46 patients (48/53 hips) and Harris (Citation1969) hip score, which could be evaluated in 41 of 46 unrevised patients (46/53 hips) at an average of 15 (14-17) years.
Radiographic assessment
The preoperative, immediate postoperative and most recent follow-up radiographs were assessed for those patients who had not had a revision. One observer who had not been involved in any of the index operations performed the radiographic examinations.
The locations of radiographic findings on the anteroposterior radiograph were recorded using 3 regions for the acetabulum (DeLee and Charnley Citation1976) and 7 regions for the femur (Gruen et al. Citation1979). The extent of osteolysis was graded as significant when larger than 2 cm in any dimension on the acetabular side, and when the lesions were progressive and eroded more than half of the adjacent cortical bone on the femoral side.
Radiographic acetabular loosening was defined as the presence of a complete radiolucent line in all three zones of greater than 1 mm, cup migration for more than 3 mm, or more than 5 degrees change in cup inclination. The femoral component was considered to be loose if serial radiographs demonstrated a change in the position of the femoral component (that is, subsidence of 3 mm or more, or varus or valgus tilting) (Engh et al. Citation1987). We were not trying to judge the type of ingrowth in radiographically stable stems.
Statistics
All statistical calculations were performed using SPSS version 10.0 software (SPSS, Chicago, IL). Kaplan-Meier survivorship analysis was performed with the use of 3 endpoints (any revision, femoral revision, or acetabular revision) and using two covariates (patient age and gender). Predicted survival rates after 10 and 15 years were determined. In addition, average survival time for the total prosthesis and separately for the stem and acetabulum were calculated. The interdependence between the revision of the acetabulum and the revision of the femoral stem was examined using the contingency table and Kappa test.
Results
11 patients (12 hips) died before revision, or before the time of the latest review for the present study. The average age of the deceased patients at the time of the index surgery had been 49 (38-56) years. 14 patients (15 hips) were lost before at least 14 years of follow-up. The average duration of follow-up for those patients was 1.7 (0.5-6) years. None had been revised before being lost to follow-up. 110 patients (122 hips) were followed until revision or, in patients without a revision, for at least 14 years.
Figure 2 Isoelastic prosthesis, showing (a) close contact between the implant and bone, and (b) massive osteolysis along the whole length of the prosthesis after 9.7 years in situ.
Complications
There were 3 corticalis perforations during preparation of the femoral canal. 2 acute dislocations of the hip occurred. 6 patients sustained a limited longitudinal fracture of the femoral neck during insertion of the femoral component and were left untreated. 2 patients had a trochanteric fracture. Sciatic nerve palsy developed in 1 patient who had a residual neurological deficit. Femoral nerve palsy developed in 1 patient and resolved spontaneously. After the index operation, no patient developed a verified deep-vein thrombosis. Non-fatal pulmonary embolism developed in 3 patients. Deep infection occurred in 5 patients; 1 early intraoperative, 3 delayed intraoperative and 1 hematogeneous. 4 occurred in the group who had not received routine perioperative antibiotic prophylaxis.
Clinical outcome
Harris hip score reached an average of 80 (39-100) points. Pain was rated as none or slight in 38 hips, moderate in 7 and severe in 3. At the latest follow-up evaluation, 15 hips were graded as excellent, 10 as good, 11 as fair, and 5 as poor.
Revisions
64 patients (69 hips, 46%) had a revision or had their implants removed. 58 revisions were for aseptic loosening, 5 for infection, 1 for instability, 4 for a periprosthetic fracture and 1 for a suspected loosening that was not confirmed intraoperatively. The average time to the revision for any reason was 9 (0.5-17) years. 4 patients (4 hips) had revision of the acetabular component only, 13 patients (15 hips) had revision of the femoral component only, and 47 patients (50 hips) had revision of both components. 8 of these patients (8 hips) had a staged revision, because at the first revision the acetabular component was considered stable. The analysis of interdependence of acetabular and femoral revisions showed a high degree of coincidence between these two events (K = 0.67).
Survival analysis
The Kaplan-Meier survival rate, with any revision as the endpoint, was 70% (95% CI = 66-74) at 10 years, and 48% (44-52) at 15 years (). With acetabular revision as the endpoint, the survival rate was 80% (76-84) at 10 years, and 56% (50-62) at 15 years (). With femoral revision as the endpoint, the survival rate was 74% (70-78) at 10 years, and 54% (49-59) at 15 years ().
Figure 3 Estimated Kaplan-Meier survivorship curve for the isoelastic RM total hip prosthesis with revision for any reason (A), acetabular loosening (B), and stem loosening (C) as the end point. The 95% confidence limits are shown by the blue area.
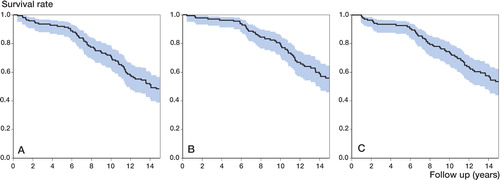
With both femoral and acetabular revisions done together or with only one of them as the endpoint, the survival rates did not differ between men and women (p = 0.7, 1.0 and 0.6, respectively). Similarly, there was no statistically significant difference in survival rate between different age groups (p = 0.7). Predicted survival rate in the group of patients under 50 years of age at the time of operation was 70% after 10 years and 45% after 15 years. In the group of patients over 50 years of age at the time of operation, the survival rates were 65% and 52% after 10 and 15 years, respectively.
Radiographic results
Radiographic failure was defined as loosening or significant osteolysis as described earlier. Radiographic assessment was completed for 38 hips (33 patients) of the 53 (46 patients) unrevised hips, giving a median radiographic follow-up of 12 (10- 18) years. Among these, there were 13 acetabular and/or femoral failures. On the acetabular side, significant osteolysis was frequently noted in zones 2 and 3 (5 hips). There were one stage 1, two 2.A, one 2.C, two 3.A and one stage 3.C (Paprosky et al. Citation1994) cases of acetabular loosening. Femoral osteolysis was observed mostly in regions 1 and 7 (9 hips). Distal osteolysis around the stem tip was noted in 5 hips. All distal lesions were non-signifi-cant. Of the cases of femoral loosening, there were; 5 stage 1, 1 stage 2.A, 3 stage 2.C, 1 stage 3.A and 1 stage 3.C stage (Paprosky et al. Citation1990). Interestingly, the Harris hip score for the radiographically loose hips reached on average 76 points, compared to an average score of 80 points in the unrevised group.
Discussion
The isoelastic RM prosthesis was claimed to preserve the proximal bone mass, to provide good bone coverage, and to facilitate rapid fracture healing and easy revision (Bombelli and Mathys Citation1982, Andrew et al. Citation1986, Niinimaki and Jalovaara Citation1995). Based on these advantages, the isoelastic prostheses have usually been recommended for younger, more active patients. Earlier studies showed almost no loss of bone stock from the proximal femur or the acetabulum, even in cases that were clearly loose (Horne et al. Citation1987, Niinimaki and Jalovaara Citation1995). The reduction in BMD in the calcar region seemed to be of the same magnitude with cemented and isoelastic stems, but bone density in the diaphyseal area was better preserved with the isoelastic stems (Niinimaki and Jalovaara Citation1995). The RM prosthesis has a collar, which should have loaded the calcar and the most proximal femur, thereby preserving bone quality. However, an unexpected atrophy of the calcar found by Niinimaki indicated possible stress bypass (Niinimaki and Jalovaara Citation1995).
To our knowledge the present study with an average follow-up of 15 years represents the longest follow-up time ever reported for RM isoelastic THR, and one of the longest for any cementless THR (Table). With survival rates of 69% (10-year) and 48% (15-year) for any reason, it presents one of the worst performances reported for a cement-less THR. Even if we take into account that, in young patients, the results of THRs are generally worse than those in older patients (Herberts and Malchau Citation2000), this performance is still not acceptable; even more so, if we compare these results to the results of some studies of cemented THRs in the young age group (Torchia et al. Citation1996, Hartofilakidis et al. Citation1997, Sochart and Porter Citation1998, Herberts and Malchau Citation2000). Cementless PC Anatomic and uncoated PM also yielded similar unsatisfactory results, and their use was restricted or discontinued (Dickob and Martin Citation1996, Kim et al. Citation1999). The results from the Swedish National Hip Arthroplasty Register reported that cementless prostheses implanted in the eighties had a 10-year survival rate of about 80% due to aseptic loosening, which was still much better than that of the present study, partly because all ages were included (Herberts and Malchau Citation2000). At the same time, a 21-year survival rate of 80% has been reported due to aseptic loosening of the cemented devices implanted in the same time period (Herberts and Malchau Citation2000).
Some recent clinical experiences with cementless total hip replacements
The main disadvantage of the isoelastic stem seems to be its flexibility, which allows a greater range of micromotion. The original idea of isoelasticity was to reduce stem stiffness in order to reduce stress shielding and prevent severe bone resorption. However, computer-simulated models have proven that flexible stems create high proximal stem/bone interface stresses, which may cause interface debonding and relative motions, possibly affecting implant loosening (Burke et al. Citation1991, Huiskes et al. Citation1992). Therefore, the concept of isoelasticity should achieve a compromise between the optimal stem flexibility, which reduces interface stresses and, at the same time, only moderate stress shielding. Furthermore, during simulated stair climbing, the micromotion between the flexible stem and bone is up to four times greater for cementless components than for cemented ones (Burke et al. Citation1991). The extent of the micromotion, which is detrimental to the long-term stability of the cementless stem, is hard to evaluate. However, the large micromotion definitely interferes with bone ingrowth. Recently, polyacetal wear debris particles have been isolated from periprosthetic tissue of loosened isoelastic stems (Minovic et al. Citation2001). An increased formation of polyacetal debris, combined with the normally occurring formation of polyethylene particles, leads to the accumulation of wear products at the interface, and induces the formation of a pathological membrane, including mononuclear and multinucleated histiocytes. Such a process affects the implant stability and weakens the integrity of the anchorage by allowing the wear particles to be spread more readily around the flexible isoelastic stem.
Considering the RM stem and the socket separately, we did not find differences in survival rates, but based on our experiences we have strong reasons to believe that the socket, when used with another type of stem, performed much better than in this study. The possible explanation is that the osteolytic process due to stem failure also involved the socket.
We had a high intraoperative fracture rate, which is common for cementless arthroplasty due to the efforts to achieve good primary stability. However, all the fractures were harmless and did not affect the stability of the stem, as already reported by other authors (Fitzgerald et al. Citation1988, Niinimaki et al. Citation1994). These authors observed a high dislocation rate and concluded that it was related to the design of the prosthesis, especially due to the thick neck of the femoral component. We could not confirm this hypothesis and believe that the most probable reason was the posterior approach used in these studies.
Previous studies (Träger Citation1989, Niinimaki et al. Citation1994) and ours found a discrepancy between the radiographic results and patient satisfaction. In some cases, we have observed significant bone destruction without accompanying pain or bad function. We speculate that the soft polyacetal resin of the femoral component did not cause a great degree of medullary reaction and thigh pain. Such revisions were very demanding and we recommend that even symptomless patients should be regularly monitored radiographically to facilitate early intervention.
Even if a new prosthetic design seems logical and potentially successful at first glance, it should not be used on a large scale until its performance has been proven in the long term, and preferably in randomized clinical trials.
The authors would like to thank Mr. Silvester Fonda, M.D., and Mr. Anton Bergoc, M.D., of the Valdoltra Orthopaedic Hospital for contributing data on the patients included in the study and Mr. Gaj Vidmar B.A. and Ms. Maja Pohar for the statistical analysis.
No competing interests declared.
- Andrew T A, Flanagan J P, Gerundini M, Bombelli R. The isoelastic, noncemented total hip arthroplasty. Preliminary experience with 400 cases. Clin Orthop 1986; (206): 127–38
- Archibeck M J, Berger R A, Jacobs J J, Quigley L R, Gitelis S, Rosenberg A G, Galante J O. Second-generation cementless total hip arthroplasty. Eight to eleven-year results. J Bone Joint Surg (Am) 2001; 83: 1666–73
- Bombelli R, Mathys R. Cementless isoelastic RM total hip prosthesis. J R Soc Med 1982; 75: 588–97
- Burke D W, O′Connor D, Zalenski E B, Jasty M, Harris W H. Micromotion of cemented and uncemented femoral components. J Bone Joint Surg (Br) 1991; 73: 33–7
- DeLee J G, Charnley J. Radiographical demarcation of cemented sockets in total hip replacement. Clin Orthop 1976; (121): 20–32
- Dickob M, Martini T. The cementless PM hip arthroplasty. J Bone Joint Surgery (Br) 1996; 78: 195–9
- Duffy G P, Berry D J, Rowland C, Cabanela M E. Primary uncemented total hip arthroplasty in patients <40 years old. 10 to 14-year result using first-generation proximally porous-coated implants. J Arthroplasty (Suppl 1) 2001; 16: 140–4
- Engh C A, Bobyn J D, Glassman A H. Porous coated hip replacement: the factors governing bone ingrowth, stress shielding and clinical results. J Bone Joint Surg (Br) 1987; 69: 45–55
- Engh A, Culpepper W J, Engh C A. Long-term results of use of th e anatomic medullary locking prosthesis in total hip artroplasty. J Bone Joint Surg (Am) 1997; 79: 177–84
- Fitzgerald R H Jr, Brindley G W, Kavanagh B F. The uncemented total hip arthroplasty. Intraoperative femoral fractures. Clin Orthop 1988; (235): 61–6
- Glassman A H, Crowninshield R D, Schenck R, Herberts P. A low stiffness composite biologically fixed prosthesis. Clin Orthop 2001; (393): 128–36
- Grübl A, Chiari C, Gruber M, Kaider A, Gottsauner-Wolf F. Cementless total hip arthroplasty with a tapered, rectangular titanium stem and a threaded cup: a minimum ten-year follow-up. J Bone Joint Surg (Am) 2002; 84: 425–31
- Gruen T A, McNeice G M, Amstutz H C. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop 1979; (141): 17–27
- Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg (Br) 1982; 64: 17–19
- Harris W H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of results evaluation. J Bone Joint Surg (Am) 1969; 51: 737–55
- Hartofilakidis G, Karachalios T, Zacharakis N. Charnley low friction arthroplasty in young patients with osteoarthritis. A 12- to 24-year clinical and radiographic follow-up study of 84 cases. Clin Orthop 1997; (341): 51–4
- Herberts P, Malchau H. Long-term registration has improved the quality of hip replacement: a review of the Swedish THR Register comparing 160,000 cases. Acta Orthop Scand 2000; 71: 111–21
- Horne G, Berry N, Collis D. Isoelastic uncemented hip arthroplasty - early experience Aust N Z J Surg. 1987; 57: 461–6
- Huiskes R, Weinans H, van Rietbergen B. The relationship between stress shielding and bone resorption around total hip stems and the effects of flexible materials. Clin Orthop 1992; (274): 124–34
- Kärrholm J, Anderber C, Snorrason F, Thanner J, Langeland N, Malchau H, Herberts P. Evaluation of a Femoral Stem with Reduced Stiffness. A Randomized Study with Use of Radiostereometry and Bone Densitometry. J Bone Joint Surg (Am) 2002; 84: 1651–8
- Kawamura H, Dunbar M J, Murray P, Bourne R B, Rorabeck C H. The porous coated anatomic total hip replacement. A ten to fourteen year follow-up study of a cementless total hip arthroplasty. J Bone Joint Surg (Am) 2001; 83: 1333–8
- Kim Y H, Kim J S, Cho S H. Primary total hip arthroplasty with a cementless porous-coated anatomic total hip prosthesis: 10- to 12-year results of prospective and consecutive series. J. Arthroplasty 1999; 14: 538–48
- Kubo T, Inoue S, Maeda T, Arai Y, Hirakawa K, Wu Y, Suehara M, Ogura T, Hirasawa Y. Cementless Lord total hip arthroplasty: cup loosening common after minimum 10years follow-up of 103 hips. Acta Orthop Scand 2001; 72: 585–90
- McFarland B, Osborne G. Approach to the hip: a suggested improvement on Koher′s method. J Bone Joint Surg (Br) 1954; 36: 364–7
- Minovic A, Milošev I, Pisot V, Cör A, Antolic V. Isolation of polyacetal wear particles from periprosthetic tissue of isoelastic femoral stems. J Bone Joint Surg (Br) 2001; 83: 1182–90
- Morscher E, Mathys R. Total isoelastic hip prosthesis implanted without cement. Initial results. Acta Orthop Belg 1974; 40: 639–47
- Morscher E, Mathys R. First experiences with a cementless isoelastic total hip prosthesis. Z Orthop Ihre Grenzgeb 1975; 113: 745–9
- Morscher E W, Dick W, Kernen V. Cementless fixation of polyethylene acetabular components in total hip arthroplasty. Arch Orthop Traumat Surg 1982; 99: 223–30
- Niinimaki T, Jalovaara P. Bone loss from the proximal femur after arthroplasty with an isoelastic femoral stem. BMD measurements in 25 patients after 9 years. 1995; 66: 347–51
- Niinimaki T, Puranen J, Jalovaara P. Total hip arthroplasty using isoelastic femoral stems. A seven- to nine-year follow-up in 108 patients. J Bone Joint Surg (Br) 1994; 76: 413–8
- Paprosky W G, Lawrence J, Cameron H. Femoral defect classification; clinical application. Orthop Rev (Suppl 9) 1990; 19: 9–15
- Paprosky W G, Perona P G, Laurence J M. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6 year follow-up evaluation. J Arthroplasty 1994; 9: 33–44
- Pisot V. The evaluation of isoelastic and RCM cementless endoprostheses. Thesis, University of Zagreb, Croatia 1993
- Rosso R. Five-year review of the isoelastic RM total hip endoprosthesis. Arch Orthop Trauma Surg 1988; 107: 86–8
- Siebold R, Scheller G, Schrener U, Jani L. Long-term results with the cement-free Spotorno CLS shaft. Orthopade 2001; 30: 317–22
- Sochart D H, Porter M L. Long-term results of cemented Charnley low-friction arthroplasty in patients aged less than 30 years. J Arthroplasty 1998; 13: 123–31
- Torchia M E, Klassen R A, Bianco A J. Total hip arthroplasty with cement in patients less than twenty years old. Long-term results. J Bone Joint Surg (Am) 1996; 78: 995–1003
- Träger D. Results of 5–7 year follow-up of implantation of RM isoelastic hip endoprosthesis. Unfallchirurg 1989; 92: 301–4
- Trauslen F C, Hassenpfiug J, Hahne H J. Long-term results with cement-free total hip prostheses. Z Orthop Ihre Grenzgeb 2001; 139: 206–11