Abstract
Background Postoperative widening of the bone tunnels have been found after anterior cruciate ligament reconstruction using autologus bone-patellar tendon-bone or hamstring tendon grafts. These changes seem to be of no clinical significance in a short to midterm follow-up. We investigated if a synthetic graft evokes the same bone tunnel widening and if it is of clinical significance in a longterm follow-up.
Methods We examined 17 patients, 13–15 years after their anterior cruciate ligament reconstruction using a Gore-Tex ligament prosthesis. The follow-up consisted of clinical examination, K-1000 arthrometric measurement, Tegner, Lysholm and IKDC scores, and CT examination of their tibia bone tunnels. 6 patients had been reoperated before follow-up, 3 because of graft rupture and 3 because of effusion and/or pain.
Results 5 patients were graded as normal (n = 2) or nearly normal according to the IKDC score, and 4 of these patients still had their Gore-Tex prosthesis intact. 15 of the patients had a tibia bone tunnel wider than the drilled 7.9 mm diameter, ranging from 9.6 to 26 mm. These changes in the bone tunnels were in some cases without symptoms and could not be detected with arthroscopy, clinical examination, arthrometry or evaluation scores. We do not know whether they are progressive.
Interpretation Based on our findings, we recommend that patients who have had a Gore-Tex anterior cruciate ligament reconstruction should be examined not only clinically or by questionnaire, but also with CT.
In a prospective, randomized study running from 1985 to 1987, we used the Gore-Tex prosthetic anterior cruciate ligament (W.L. Gore and Associates Inc., Flagstaff, Arizona) which has shown good short-term results (James et al. Citation1979, Bolton and Bruchman Citation1985, Glousman et al. Citation1988, Indelicato et al. Citation1989). However, a progressive increase in problems was reported in the early nineties (Dahlstedt et al. Citation1990, Citation1993, Woods et al. Citation1991, Paulos et al. Citation1992, Roolker et al. Citation2000). These problems were mainly synovitis, recurrent sterile effusions, and graft breakage and loosening, in some cases to the extent that the graft had to be explanted. The prosthesis was withdrawn from the market by the manufacturer in 1993.
Seemann and Steadman (Citation1993) reported 2 cases who had osteolytic widening of their tibia tunnel, which needed bone grafting at revision surgery. We decided to examine all patients who had had anterior cruciate ligament reconstruction performed at our department using the Gore-Tex ligament, with CT-scan and by clinical and arthrometric examination. The aim was to see whether there was osteolytic widening of the bone tunnels and whether it could be detected by clinical and/or arthrometric examination.
Patients and methods
Between 1985 and 1987, 22 patients were operated on with the Gore-Tex ligament prosthesis because of old anterior cruciate ligament injuries. Of these, 3 could not be reached and 2 declined to participate. According to our charts, 1 of the latter was active at a high physical level with no problems at the 5-year follow-up, while the other one was having problems with instability and had had 3 arthroscopic meniscus resections performed within 3 years of the Gore-Tex reconstruction. 2 of the 3 patients who could not be reached were rereconstructed, one because of atraumatic instability, one because of recurrent, painful effusions and the third one was unstable but satisfied at the last follow-up. Of the remaining 17 patients (8 women), 6 patients had been reoperated between index surgery and follow-up. 3 patients were reoperated because of traumatic rupture (2 less than 1 year after surgery and 1 patient 3 years postoperatively), and the other 3 because of increasing laxity, recurrent effusions and/or pain (all 3 had symptoms less than 1 year after reconstruction). They all had had the Gore-Tex ligament explanted and 5 of them had an anterior cruciate ligament rereconstruction performed with another graft ().
Patient characteristics and follow-up results after 13–15 years in patients reconstructed with Gore-Tex prosthetic anterior cruciate ligament
Operative technique
The Gore-Tex reconstructions were done with a modified over-the-top technique as described by Bolton and Bruchman (Citation1985), using an 7.9–mm drill to prepare the bone tunnels in both femur and tibia.
Follow-up
The patients where examined by OM or LD. The follow-up protocol consisted of: examination with the KT-1000 arthrometer with maximum manual displacement, CT-scans of the bone tunnel in the proximal tibia, IKDC score (Hefti et al. Citation1993), Lysholm and Tegner scores (Tegner and Lysholm Citation1985, Hefti et al. Citation1993), pivot shift, Lachman test and visual analog scale (VAS) score for pain.
CT-scans, using the same technique as that we have described earlier (Muren et al. Citation2001), were taken perpendicular to the tunnel with axial technique (5-mm thick slices and 5 mm image interval). Anterior/posterior (A/P) and medial/lateral (M/L) diameters were calculated. All the measurements on the CT were made by the same radiologist (EB).
Statistics
For arthrometric and radiological values, we used Student t-test and regression analysis. For the nonparametric scores, Spearman′s correlation coefficient was used. The calculations were made using JMP 3 (SAS Institute inc.) software.
Results ()
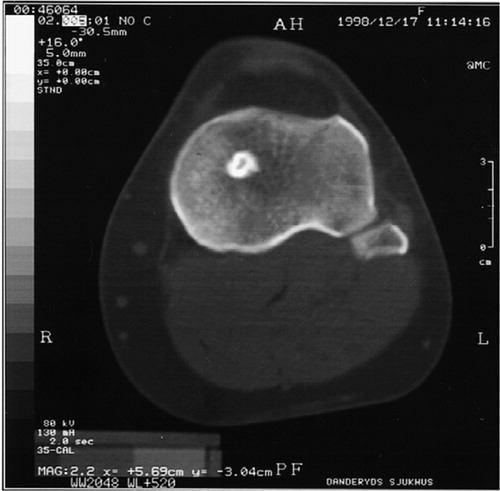
5 patients were graded normal (A = 2) or nearly normal (B = 3) according to the IKDC evaluation form. One of these patients (no. 11), who had normal results in all the scores as well as in clinical and arthrometric exams, had the second greatest widening of the bone tunnel. 2 of the patients (nos. 6 and 13) had a bone tunnel that was close in diameter to that of the 7.9 mm drill diameter used at surgery. The rest of the patients had a widening of the tunnel with diameters ranging from 8.7 mm to 26 mm. In 8 of the patients the margins of the bone tunnel were lytic (), and in 9 they were sclerotic (). 4 patients had an arthrometric test with a maximal manual displacement difference of more than 3 mm.
Figure 1 CT-scan of patient no. 11, showing almost 3 times wider bone tunnel than the original 7.9 mm; lytic tunnel walls.
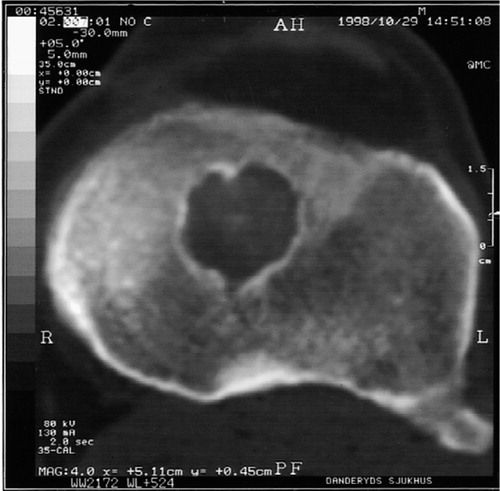
Figure 2 CT-scan of patient no. 12. Only slight widening of the bone tunnel was apparent; sclerotic tunnel walls.
No correlation could be found between anterior/ posterior (A/P) diameters and the clinical evaluation scores, i.e. a lytic widening of the bone tunnel could not be detected by clinical examination. Spearman correlation coefficient and t-test showed good correlation (r = 0.64, p < 0.002) between large A/P diameter and lytic bone tunnel walls as well as small A/P diameter and sclerotic walls.
3 of the patients (no.s 7, 14 and 16) with widening of their tibia tunnel on the CT scans, and with symptomatic instability and recurrent, painful effusions, had their Gore-Tex ligament explanted after the follow-up. Before the open surgery, arthroscopy showed general synovitis but it could not reveal the widening of the tibia tunnel. All the ligaments were partially ruptured, and tissue macroscopically much the same as in rheumatoid bone cysts was found in the tibia bone tunnel; microscopic examination showed chronic inflammatory cells. The bone tunnels were bone grafted. Follow- up CT-scans showed good consolidation of the bone graft, and the patients are now scheduled for further surgery (high tibia osteotomy/anterior cruciate ligament rereconstruction).
Discussion
Our findings indicate that the Gore-Tex ligament, in a synovial surrounding, is not a biologically inert implant. Numerous studies (Dahlstedt et al. Citation1990, Citation1993, Woods et al. Citation1991, Paulos et al. Citation1992, Sledge et al. Citation1992) have shown it to evoke aseptic effusions, and in 2 other studies (Seemann and Stead-man Citation1993, Fukubayashi and Ikeda Citation2000) osteolytic bone tunnel widening has been described. We found that all cases of osteolysis are not symptomatic and cannot be detected with evaluation scores, or clinical or arthrometric examinations. We consider this to be important information, since such osteolytic bone changes may influence future knee surgery (i.e. revision of anterior cruciate ligament reconstruction, high tibia osteotomy, uni- or total knee artroplasties). It may also increase the risk of periarticular fractures although we have found no proofs of that, nor among our patients or in the literature. The good correlation found between sclerotic/lytic bone tunnel walls and diameter of the bone tunnel might be interpreted as the lytic tunnel walls indicating an ongoing process as opposed to sclerotic walls. To investigate this further, new CT examinations should be performed after 1–2 years.
The two most commonly used techniques in anterior cruciate ligament reconstruction today use autologous bone-patellar tendon-bone or hamstring grafts. Both techniques, especially hamstring grafts, have shown tibia tunnel widening radiologically which did not affect the clinical outcome after a short to medium-term follow-up (Clatworthy et al. Citation1999, Fink et al. Citation2001, Webster et al. Citation2001, Jo et al. Citation2004). They have not been associated with the other problems we have encountered with the Gore-Tex ligament. Two problems associated with these techniques are donor site morbidity and weakness of the graft during the revascularization and collagenization. In order to avoid these problems, different ligament prostheses have been tried. In our study as well as others (Dahlstedt et al. Citation1990, Citation1993, Engstrom et al. Citation1993, Wredmark and Engstrom Citation1993, Maletius and Gillquist Citation1997), different prosthetic ligaments (Gore-Tex, Leeds- Keio, ABC carbon polyester and Stryker Dacron) have not maintained joint stability and have also led to painful synovitis and recurrent effusions (Jenkins Citation1978, Klein and Jensen Citation1992, Paulos et al. Citation1992, Mody et al. Citation1993, Wredmark and Engstrom Citation1993).
On the basis of this study and after reviewing the literature, we recommend reexamination of all patients who have had an intraarticular anterior cruciate ligament reconstruction using a Gore-Tex prosthetic ligament. Although 12 of our 17 patients were rated abnormal or gravely abnormal on the IKDC score, none of them had contacted an orthopedic surgeon. That they did not try to contact their treating physician does not mean that they were free of problems. These re-examinations should include CT, clinical and arthrometic examination. All patients should be followed until one has made sure that the osteolysis is not progressing. Patients with strong symptoms (instability, pain, swelling) and/or progressive osteolysis should have the ligament explanted, the bone tunnel thoroughly curettaged, and-if necessary-bone transplanted. A second-stage rereconstruction should be considered on an individual basis.
No competing interests declared.
- Bolton C W, Bruchman W C. The GORE-TEX expanded polytetrafluoroethylene prosthetic ligament. An in vitro and in vivo evaluation. Clin Orthop 1985, 196: 202–13
- Clatworthy M G, Annear P, Bulow J U, Bartlett R J. Tunnel widening in anterior cruciate ligament reconstruction: a prospective evaluation of hamstring and patella tendon grafts. Knee Surg Sports Traumatol Arthrosc 1999; 7: 138–45
- Dahlstedt L, Dalen N, Jonsson U. Goretex prosthetic ligament vs. Kennedy ligament augmentation device in anterior cruciate ligament reconstruction. A prospective randomized 3-year follow-up of 41 cases. Acta Orthop Scand 1990; 61: 217–24
- Dahlstedt L, Dalen N, Jonsson U, Adolphson P. Cruciate ligament prosthesis vs. augmentation. A randomized, prospective 5-year follow-up of 41 cases. Acta Orthop Scand 1993; 64: 431–3
- Engstrom B, Wredmark T, Westblad P. Patellar tendon or Leeds-Keio graft in the surgical treatment of anterior cruciate ligament ruptures. Intermediate results. Clin Orthop 1993, 295: 190–7
- Fink C, Zapp M, Benedetto K P, Hackl W, Hoser C, Rieger M. Tibial tunnel enlargement following anterior cruciate ligament reconstruction with patellar tendon autograft. Arthroscopy 2001; 17: 138–43
- Fukubayashi T, Ikeda K. Follow-up study of Gore-Tex artificial ligament--special emphasis on tunnel osteolysis. J Long Term Eff Med Implants 2000; 10: 267–77
- Glousman R, Shields C, Jr., Kerlan R, Jobe F, Lombardo S, Yocum L. Gore-Tex prosthetic ligament in anterior cruciate deficient knees. Am J Sports Med 1988; 16: 321–6, (alla namnen, ej et al)
- Hefti F, Muller W, Jakob R P, Staubli H U. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1993; 1: 226–34
- Indelicato P A, Pascale M S, Huegel M O. Early experience with the GORE-TEX polytetrafluoroethylene anterior cruciate ligament prosthesis. Am J Sports Med 1989; 17: 55–62
- James S L, Woods G W, Homsy C A, Prewitt J M, 3rd., Slocum D B. Cruciate ligament stents in reconstruction of the unstable knee. A preliminary report. Clin Orthop 1979, 143: 90–6
- Jenkins D H. The repair of cruciate ligaments with flexible carbon fibre. A longer term study of the induction of new ligaments and of the fate of the implanted carbon. J Bone Joint Surg (Br) 1978; 60: 520–2
- Jo H, Jun D S, Lee D Y, Lee S H, Seong S C, Lee M C. Tibial tunnel area changes following arthroscopic anterior cruciate ligament reconstructions with autogenous patellar tendon graft. Knee Surg Sports Traumatol Arthrosc 2004; 12(4)311–6
- Klein W, Jensen K U. Synovitis and artificial ligaments. Arthroscopy 1992; 8: 116–24
- Maletius W, Gillquist J. Long-term results of anterior cruciate ligament reconstruction with a Dacron prosthesis. The frequency of osteoarthritis after seven to eleven years. Am J Sports Med 1997; 25: 288–93
- Mody B S, Howard L, Harding ML, Parmar H V, Learmonth D J. The ABC carbon and polyester prosthetic ligam ent for ACL-deficient knees. Early results in 31 cases. J Bone Joint Surg (Br) 1993; 75: 818–21
- Muren O, Brosjo E, Dahlstedt L, Dahlborn M, Dalen N. No bone ingrowth into the tibia tunnel in anterior cruciate ligament-reconstructed patients: a 1-year prospective quantified CT study of 10 patients reconstructed with an autologous bone-patellar tendon-bone graft. Acta Orthop Scand 2001; 72: 481–6
- Paulos L E, Rosenberg T D, Grewe S R, Tearse D S, Beck C L. The GORE-TEX anterior cruciate ligament prosthesis. A long-term followup. Am J Sports Med 1992; 20: 246–52
- Roolker W, Patt T W, van Dijk C N, Vegter M, Marti R K. The Gore-Tex prosthetic ligament as a salvage procedure in deficient knees. Knee Surg Sports Traumatol Arthrosc 2000; 8: 20–5
- Seemann M D, Steadman J R. Tibial osteolysis associated with Gore-Tex grafts. Am J Knee Surg 1993; 6: 31–8
- Sledge S L, Steadman J R, Silliman J F, Peloza J, Fulstone H A. Five-year results with the Gore-Tex anterior cruciate ligament prosthesis. Am J Knee Surg 1992; 5: 65–70
- Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop 1985, 198: 43–9
- Webster K E, Feller J A, Hameister K A. Bone tunnel enlargement following anterior cruciate ligament reconstruction: a randomised comparison of hamstring and patellar tendon grafts with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc 2001; 9: 86–91
- Woods G A, Indelicato P A, Prevot T J. The Gore-Tex anterior cruciate ligament prosthesis. Two versus three year results. Am J Sports Med 1991; 19: 48–55
- Wredmark T, Engstrom B. Five-year results of anterior cruciate ligament reconstruction with the Stryker Dacron high-strength ligament. Knee Surg Sports Traumatol Arthrosc 1993; 1: 71–5