Abstract
Background There are no clear indications for conversion of knee fusion to total arthroplasty. In this paper we report outcome and complications in 8 patients.
Patients and methods We reviewed 8 total knee arthroplasties after takedown of previous fusion 24–55 months after the conversion. The original diagnoses were complications following injury in 3 patients, rheumatoid arthritis in 3, complication after chondromalacia in 1 patient and tuberculous arthritis in 1 patient. The age at operation ranged from 31 to 67 years. The time since arthrodesis ranged from 1 to 49 years.
Results 5 patients had to undergo reoperation for postoperative complications. 2 patients experienced recurrence of previous deep infection, which led to thigh amputation in one and chronic fistulation in the other. Only 1 patient had an uneventful course after the conversion procedure, but he died later on due to a heart attack. As another patient also died of cardiovascular disease, 5 of the 8 patients were available for evaluation of knee function. In these patients the knee flexion ranged from 90 to 120 degrees, extension lag ranged from 10 to 40 degrees, and all knees were aligned at 6 to 8 degrees of valgus. The Knee Society clinical scores ranged from 47 to 74, the Womac scores ranged from 9 to 47, and EuroQol ranged from 0.1 to 0.8.
Interpretation Our findings indicate that conversion of knee arthrodesis to total arthroplasty should only be performed in selected cases, and after giving the patient extensive information about the high risk of rather serious complications.
In most cases, a knee fusion is associated with considerable restrictions, the patients may be dissatisfied and conversion to a total knee arthroplasty may be considered (Holden and Jackson Citation1988). There have, however, been few reports on the results of total knee arthroplasty after solid fusion. The indications are uncertain and few, and questions about adequate muscle function and stability will arise. In general, a semiconstrained prosthesis is recommended to substitute for ligament deficiency. Holden and Jackson (Citation1988) reported results in 2 patients, 3 and 5 years following conversion, and concluded that the outcome was gratifying with good stability and adequate motion. The patients claimed that function had been substantially improved. Henkel et al. Citation(2001) reviewed 7 patients with a mean follow-up of 5 years, and found that the procedure is technically demanding and has a considerable complication rate. During the past 7 years, we have converted 8 fused knees with the use of a semi-constrained prosthesis. We report subjective and objective outcome.
Patients and methods
Patients
During the years 1998–2002, we converted 8 fused knees in 8 patients (6 women) to a total knee arthroplasty. Median age at conversion was 53 (31–76) years. The reasons for the initial fusion were complications after injury in 3 patients, rheumatoid arthritis in 3, complications after chondromalacia in 1 patient and tuberculous arthritis in another. The median time from fusion to conversion was 3 (1–49) years.
Figure 1. Radiographs before and after conversion of knee arthrodesis to arthroplasty (patient no. 2).
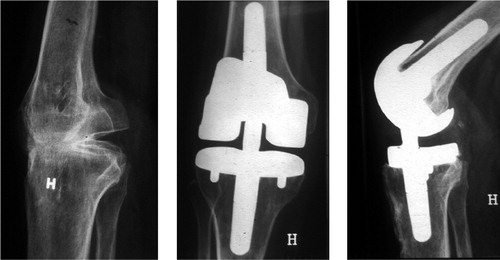
Figure 2. Patient no. 2. She has full extension against gravity and flexion to 110 degrees. Measurements of muscle strength indicated 60% of the hamstrings and 69% of the quadriceps as compared to the healthy side. The scar tissue around the knee was due to multiple operations, skin transpositions and transplantations.

Surgical technique
We used templates to estimate the suitable size of the components. To estimate the level of the joint line, radiographs of both lower extremities were taken, and further planning was carried out at the drawing board. The approach was dependent on old scars, but was made preferably through a medial parapatellar incision with a gentle soft tissue dissection. Where necessary, we osteotomized the tuberositas of the tibia to ensure proper exposure. The fusion was osteotomized at the estimated junction of the femur and the tibia, with care taken to preserve bone stock. In 6 knees, the patella had to be osteotomized from the distal femur. In all cases we used a semi-constrained prosthesis (Dual Articular, Biomet,GB). The prosthesis was cemented, and partial weight bearing was allowed as soon as the patient felt comfortable.
Evaluation
2 patients died in the follow-up period because of unrelated cardiovascular disease, and 1 was amputated because of infection (Table). Thus, 5 patients were available for evaluation. Median follow-up time was 41 (25–63) months.
Patient data
At follow-up, the range of motion was recorded using a goniometer. The clinical results were evaluated by the Knee Society Clinical Score (Insall et al. Citation1989) with 100 as the best outcome and 0 as the worst possible outcome. We used the WOMAC score for osteoarthrosis to assess the functional results (Bellamy et al. Citation1998), with a total score from 0 (worst) to 96 (best). Quality of life was measured by the EuroQol instrument (The Euro-Qual Group Citation1990) with +1 as best and –0.594 as worst possible outcome.
We tested quadriceps and hamstring muscle strength using a Cybex 6000 (Cybex-Lumex Inc., Ronkonkoma, NY). The test protocol consisted of 5 repetitions at an angular velocity of 60 degrees per sec (strength) followed by a 1-minute rest period and 25 repetitions at 180 degrees per sec (endurance) (Holm et al. Citation1994). The parameter used for analysis was total work.
We examined all radiographs for signs of loosening of either component according to the Knee Society Radiographic Score (Ewald Citation1989). The assessment of the quality of fixation depended on analysis of any radiolucencies and osteolysis. Any radiolucency above 5 mm was assumed to indicate non-osseointegration, and osteolysis was defined as newly developed expansile scalloping radiolucency extending away from the prosthesis, which had not been seen on the immediate postoperative radiographs.
Results
Complications
7 patients had complications (Table). In 3 cases, severe skin necrosis occurred during the early postoperative course. 2 of these were operated on with a gastrocnemius flap, and the third patient was operated on with wound revisions followed by skin transplants. 4 patients had late complications. 2 patients developed recurrence of previous deep infection that led to thigh amputation in 1 and persistent fistulations in the other. 1 patient suffered from patellofemoral pain and was operated on with a patellarprosthesis. 1 patient developed a stiff knee and was operated on with open mobilization.
Follow-up
At follow-up, the median Knee Society Score for the 5 patients was 58 (47–74). The Womac score was 37 (9–47) and Euroqol was 0.7 (0.1–0.8). Median knee flexion was 100° (90°–120°), and extension lag was 20° (10°–40°). All knees were clinically and radiographically aligned at 6°–8° of valgus, and anteroposterior and mediolateral instability was less than 10° due to the constraint within the prosthesis itself. We found no signs of loosening by radiographic analysis. Muscle strength could be tested in only 3 patients; due to a generally poor condition, the 2 others could not be tested. All 3 patients showed extensive reduction in muscle strength compared to the contralateral side. The deficits were 75% for hamstrings and 78% for quadriceps, respectively. One of the patients who died had no extensor mechanism at all, but the knee could take full weight bearing by means of an orthosis.
Discussion
Our results are in agreement with those of others that there is a high complication rate after conversion of a fused knee. Kreder et al. (Citation1999) converted 18 knee fusions to total knee replacements; infection occurred in 2 patients, and 1 knee was revised after 4 years. Furthermore, 3 of the patients required removal of the components within 4 years. These authors concluded that such issues must be carefully considered and discussed with the patients before any conversion procedure. Kim et al. (Citation2003) reviewed 36 consecutive patients with a knee fusion undergoing conversion to total knee prosthesis, and reported a high frequency of necrosis of the skin edges. Soft-tissue necrosis was a common complication in our series also. This was solved in an acceptable way in all cases, considering the difficult circumstances. However, our experience indicates that when the skin is in poor condition, one should be prepared for an intraoperative gastrocnemius transfer and skin transplant.
3 of our patients were in poor condition due to serious rheumatoid arthritis, and developed major complications. In 2 of them, a gastrocnemius flap with skin transplant was carried out in the postoperative phase. 1 of these patients developed a chronic infection, and the other did not gain adequate extensor mechanism. The third patient with rheumatoid arthritis was infected and had to undergo a thigh amputation. Both patients with infection had had the knee fusion because of a previously failed prosthesis due to infection.
The oldest patient had a stiff knee after a complicated fracture, and a gastrocnemius flap with skin transplant had to be carried out in the early post-operative course. She had no real extensor mechanism, but managed very well in daily activities. Thus, in our series only 1 patient had an uneventful course after conversion.
Even though most of our patients experienced a complicated postoperative course and many of them have had to rely on a stick, they all preferred to have a movable knee rather than their previously fused one. In 3 patients, quadriceps and hamstring muscle strength was successfully tested. Although the patients functioned well from a clinical point of view, all had extensive reduction in muscle strength compared to the contralateral side. It may be that the semiconstrained prosthesis secured stability. Holden and Jackson (Citation1988) recommended that a constrained total knee prosthesis should be used in the conversion of a fused knee to total knee arthroplasty, to substitute for the lack of soft tissue stabilizers. It has been shown recently that when soft-tissue sleeves can be preserved, a posterior stabilized prosthesis may be used effectively (Kim et al. Citation2003).
The clinical, functional and quality of life scores indicated acceptable results. For comparisons, Lingard et al. (Citation2001) reported a Knee Society Clinical Score of 87 after primary knee replacement. Our patients had a median score of 58, which we consider to be acceptable in relation to the rather complicated preoperative situation. The median WOMAC score in our study was 37, which can be compared to the results of Hartley et al. (Citation2002) who reported a score of 48 one year after revision knee arthroplasty. EuroQol-5D is a standardized instrument for use as a measure of health outcome. Except for one, our patients had EuroQual score between 0.6 and 0.8. As a comparison, in the UK population, sample means range from 0.9 to 0.7 in ages ranging from 30 to 79 years (Kind et al. Citation1999). 1 of our patients had a low EuroQol score of 0.1. The main reason for this was severe pain. The initial fusion was also carried out due to severe knee pain after injury. This patient probably reflects the fact that knee fusion due to extensive pain should not be considered for arthroplasty.
We must emphasize that at every knee fusion, a later conversion to a total prosthesis should be taken into consideration. The extensor mechanism should be preserved if possible, and the patella should not be used as a graft. However, before conversion from knee fusion to arthroplasty, the patients should be given extensive information about the high risk of serious complications.
No competing interests declared.
- Bellamy N, Buchanan W W, Goldsmith T H, Campell J. Validation study or WOMAC: a health status instrument for measuring clinically-important patient-relevant outcomes following total hip or knee arthroplasty in osteoarthritis. J Orthop Rheumatol 1998; 1: 95–108
- Ewald F C. The knee society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop 1989, 248: 9–12
- Hartley R C, Barton-Hanson N G, Finley R, Parkinson R W. Early patient outcomes after primary and revision total knee arthroplasty. J Bone Joint Surg (Br) 2002; 84: 994–9
- Henkel T R, Boldt J G, Drobny T K, Munzinger U K. Total knee arthroplasty after formal knee fusion using unconstrained and semi-constrained components: a report of 7 cases. J Arthroplasty 2001; 16(6)768–76
- Holden D L, Jackson D W. Considerations in total knee arthroplasty following previous knee fusion. Clin Orthop 1988, 227: 223–8
- Holm I, Ludvigsen P, Steen H. Isokinetic hamstrings/quadriceps ratios: normal values and reproducibility in sport students. Isokinetic and Exercise Science 1994; 4: 141–5
- Insall J N, Dorr L D, Scott R D, Scott W N. Rationale of the knee society clinical rating system. Clin Orthop 1989, 248: 13–4
- Kim Y-H, Oh S-H, Kim J-S. Conversion of a fused knee with use of a posterior stabilized total knee prosthesis. J Bone Joint Surg (Am) 2003; 85: 1047–50
- Kind P, Hardman G, Macran S. UK Population norms for EQ-5D. York Centre for Health Economics Discussion Paper. 1999; 172
- Kreder H J, Williams J I, Jaglal S, Axcell T, Stephen D. A population study in the Province of Ontario of the complications after conversion of hip or knee arthrodesis to total joint replacement. Can J Surg 1999; 42(6)433–9
- Lingard E A, Katz J N, Wright R J, Wright E A, Sledge C B. Kinemax outcomes group. Validity and responsiveness of the Knee Society Clinical Rating System in comparison with the SF 36 and WOMAC. J Bone Joint Surg (Am) 2001; 83: 1856–64
- The EuroQol Group. EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 1990; 16: 199–208