Abstract
Objectives: Using a large-scale nationwide survey database, we investigated the epidemiological characteristics for idiopathic SSNHL in Japan.
Methods: The subjects for this analysis were patients registered in a Japanese multicentre database between April 2014 and March 2016. A total of 3419 idiopathic SSNHL patients were registered in the database, and the clinical characteristics of the idiopathic SSNHL patients were obtained. Several factors associated with the severity of hearing impairment and prognosis were then investigated. Statistical analysis was performed to clarify the factors associated with the severity of hearing impairment and prognosis.
Results: There were significant correlations between the severity of hearing loss and diabetes mellitus, kidney disease, past history of brain infarction, heart disease, age (under 16 years/elderly), and symptoms of vertigo/dizziness. We also analyzed the prognostic factors for idiopathic SSNHL, and found that the severity of hearing loss (Grade 3 or 4), heart disease, aged 65 years or over, time from onset to treatment (over 7 days), and symptoms of vertigo/dizziness were all significantly related to poor prognosis.
Conclusion: The present large-scale clinical survey revealed current epidemiological trends for idiopathic sudden sensorineural hearing loss (SSNHL) and various factors associated with the severity of hearing impairment and prognosis.
Chinese abstract
结论: 这一大规模临床调查揭示出当前的特发性突发性感觉神经性听力损失 (SSNHL) 的流行病趋势以及与听力损伤的严重程度及其预后相关的各种因素。
目的: 我们利用全国大型调查数据库, 对日本特发性SSNHL的流行病学特征进行了调查。
方法: 本研究对象为2014年4月至2016年3月间在日本多中心数据库登记的患者。数据库中共登记了3419例特发性SSNHL患者, 获得了特发性SSNHL患者的临床特征。随后, 我们调查了与听力损伤的严重程度及其预后相关的几个因素, 并进行了统计分析, 以澄清与听力损伤的严重程度及其预后相关的因素。
结果: 听力损失严重程度与糖尿病、肾脏疾病、脑梗死病史、心脏病、年龄 (16岁以下/老龄) 以及眩晕/眩晕症状有显著相关性。我们还分析了特发性SSNHL的预后因素, 发现听力损失的严重程度 (3级或4级) 、心脏病、65岁以上、从发病至治疗的时间长度 (7天以上) 以及眩晕/头晕症状, 均与不良预后相关。
Introduction
Idiopathic sudden sensorineural hearing loss (SSNHL) is among those diseases specified by the Japanese government as ‘intractable diseases’ resulting from an unidentifiable cause and without a clearly established treatment, and entailing a considerably high risk of disability.
In Japan, nationwide epidemiological surveys of idiopathic SSNHL have traditionally been conducted by the Research Committee of the Ministry of Health and Welfare for Acute Profound Deafness [Citation1–2]. After 2014, the framework of the Research Committee was changed, and the epidemiological surveys of hearing disorders, including idiopathic SSNHL, have since been conducted as part of the Research on Measures for Intractable Diseases. In connection with this epidemiologic survey, a multicentre database was constructed, with data for 3419 idiopathic SSNHL patients registered to date.
In this report, we present our findings regarding the clinical features of idiopathic SSNHL based on an analysis of the epidemiologic survey database.
Material and methods
The subjects (n = 3419) for this analysis were patients registered with the abovementioned multicentre database between April 2014 and March 2016. Thirty university hospitals and medical centers participated in this epidemiologic survey. Idiopathic SSNHL was defined according to criteria established by the Sudden Deafness Research Committee of the Ministry of Health and Welfare, Japan (2012). Details of the criteria are shown in [Citation3]. We excluded patients for whom data were incomplete.
Table 1. Criteria for the diagnosis of idiopathic SSHNL.
Audiometric and recovery assessment
All data, including the hearing thresholds in the audiograms, symptoms and complications, were entered in this epidemiologic database. The initial audiogram grading () and recovery criteria (), as defined by the Ministry of Health and Welfare in Japan [Citation2], were obtained from the audiogram data.
Table 2. Criteria for the grading of hearing loss in idiopathic SSNHL.
Table 3. Hearing improvement criteria for SSHNL as defined by the Ministry of Health and Welfare in Japan.
Statistical analysis
The statistical analysis was performed using Pearson’s chi-squared test for univariate analysis, and a stepwise logistic-regression model (Wald test) for multivariate analysis. A p value <.05 was considered significant. Odds ratios were calculated with 95% confidence intervals. The PSAW Statistics version 18.0 (SPSS Inc., Chicago, IL) was used for all analysis.
Results
Characteristics of the included patients
The clinical characteristics, complications and symptoms of the patients included in this study are given in . A large number of idiopathic SSNHL patients (3419 patients) were registered in the database. The average patient age was 54.2 years (SD = 17.0), with the highest proportion of patients in the 60–69 years age group. The distributions of idiopathic SSNHL patients in this survey for men and women in each age group are shown in . The average time from onset to the start of treatment was 6.0 days (SD = 23.3), with the majority of patients (94.0%) beginning treatment within two weeks of onset.
Figure 1. Age distribution of males and females in this study. In each gender group, the number of patients gradually increased from the youngest age group to the 60–69 years age group. The average patient age was 54.2 years (SD =17.0).
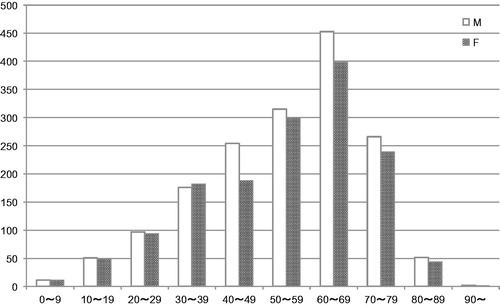
Table 4. Characteristics of the included patients.
In this study, we screened the patient medical history database to identify associations between idiopathic SSNHL and factors including diabetes mellitus, hyperlipidemia, kidney disease, brain infarction, and heart disease. Diabetes mellitus was reported in 547 (17.1%), hyperlipidemia in 342 (11.2%), kidney disease in 146 (4.8%), brain infarction in 96 (3.2%), and heart disease in 356 (11.7%) patients. Among the total patients, 1129 (35.3%) reported episodes of vertigo/dizziness, and 2451 (77.8%) reported episodes of tinnitus.
Analysis of factors associated with the severity of SSHNL
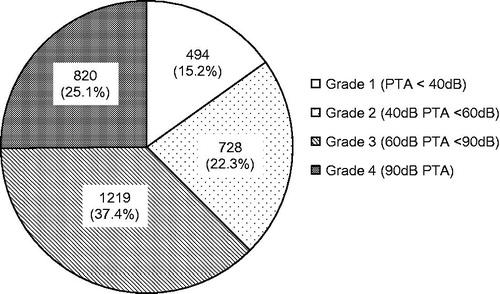
The initial pure tone average (PTA) of the affected ear was calculated for all patients, with the average found to be 69.2dB (SD =26.2). The distribution of hearing grades is given in .
Figure 2. Grade of hearing loss in this study. The grade of hearing loss was obtained from the initial audiogram, as defined by the Ministry of Health and Welfare in Japan ().
We next divided the patients into the mild hearing loss group (Grade 1 and 2) and the severe hearing loss group (Grade 3 and 4) to analyze the factors associated with the severity of SSHNL. The results of the univariate statistical analysis showed that there were significant correlations between the severity of hearing loss and diabetes mellitus, kidney disease, heart disease, past history of brain infarction and symptoms of vertigo/dizziness. Being aged under 16 years or ≧65 years was also significantly related to severe hearing loss (Grade 3 or 4). A multivariate logistic-regression analysis of hearing loss grade, adjusted for gender, age, symptoms, and the above-mentioned comorbidities, revealed a significantly higher probability of severe hearing loss in the patients with vertigo/dizziness, diabetes mellitus, heart disease, or those aged 65 years or over ().
Table 5. Analysis of risk factors and odds ratio related to Grade 3/4 hearing loss.
Type of treatment
Patient distribution by type of treatment, with a focus on corticosteroids, is shown in . The majority of patients (92%) were administered some type of corticosteroid, with systemic corticosteroid therapy being the most common (83%) and only 9% of patients in this study receiving intratympanic corticosteroids.
Figure 3. (A) The types of treatment, with a focus on corticosteroids, are summarized. The majority of patients (92%) were administered some type of corticosteroid, with systemic corticosteroid therapy being the most common (83%) and only 9% of patients in this study receiving intratympanic corticosteroids. (B) The pattern of concomitant drugs use is shown. Most patients (96.3%) in this study were treated with corticosteroids together with other concomitant drugs. Corticosteroids with ATP and Vit B12 (without PG) was the most commonly used combination (accounting for 61.6% of patients). (C) The distribution of the severity of hearing loss in each treatment group. Treatment A is corticosteroids with ATP and Vit B12 with PG, Treatment B is corticosteroids with ATP and Vit B12 without PG, and Treatment C is corticosteroids without any concomitant drugs. Treatment A tended to be selected for the patients with severe hearing loss.
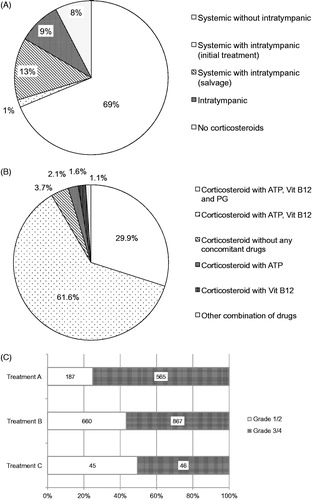
We also examined the use of other drugs concomitantly with corticosteroids. Specifically, adenosine triphospate (ATP), vitamin B12 (Vit B12) , and prostaglandin (PG) were recorded in the database. The pattern of concomitant drug use is shown in . Corticosteroids with all drugs mentioned above (ATP, Vit B12, and PG) (Treatment A) accounted for 29.9% and corticosteroids with ATP and Vit B12 (without PG) (Treatment B) accounted for 61.6% of patients in this study. Only 3.7% of patients received corticosteroids alone (without any concomitant drugs) (Treatment C). Among these three types of concomitant drug use, patients with severe hearing loss (Grade 3 or 4) more frequently received Treatment A, accounting for 75.1% in that treatment group, 56.8% in the Treatment B group and 50.5% in the Treatment C group. Statistically significant differences were observed in the severity of hearing loss between Treatment A and Treatment B or C (). Based on these findings, it appears that PG has commonly been used for patients with severe hearing impairment.
Analysis of factors associated with the prognosis of idiopathic SSNHL
In this study, the treatment efficacy for all patients, represented by the recovery criteria in , was as follows; complete recovery was observed in 1317 patients (41.2%), marked improvement in 521 patients (16.3%), slight improvement in 549 patients (17.2%), and no change in 807 patients (25.3%) (). We next divided the patients into the good prognosis group (complete recovery or marked improvement) and the poor prognosis group (slight improvement or no change) to analyze the factors associated with prognosis, and found that the severity of hearing loss (Grade 3 or 4), hyperlipidemia, heart disease, aged 65 years or over, time from onset to treatment (over 7 days) and symptoms of vertigo/dizziness were significantly related to poor prognosis based on univariate analysis. We also performed a multivariate analysis, adjusted for gender, age, symptoms, above-mentioned comorbidities, time from onset to the start of treatment, and severity (grade) of initial hearing loss. The multivariate analysis showed that hyperlipidemia, heart disease, age (65 years or over), time from onset to treatment (over 7 days), and symptoms of vertigo/dizziness could be considered as independent prognostic factors in relation to recovery. Diabetes mellitus was correlated with better prognosis based on the multivariate analysis (no significant correlation was observed in the univariate analysis). Severity of hearing loss was excluded by the multivariate model ().
Figure 4. Treatment outcome, classified according to the recovery criteria defined by the Ministry of Health and Welfare in Japan (), for all patients in this study is shown.
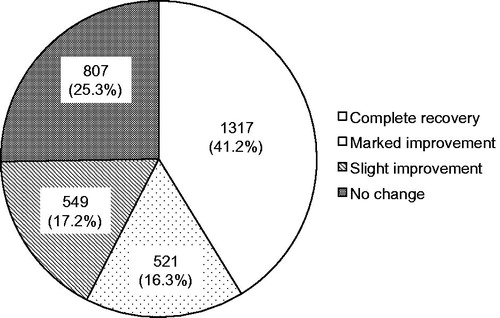
Table 6. Analysis of risk factors and odds ratio related to a poor outcome.
Discussion
This epidemiologic survey was able to accumulate a large amount of detailed data from thirty university hospitals and medical centers, and there have been almost no previous reports of such large-scale clinical analyses. Furthermore, we could analyze the route of corticosteroid administration including intratympanic administration. On the other hand, we could not clarify the incidence of idiopathic SSNHL as this study was not designed as a complete survey of all patients in each hospital.
Characteristics of the included patients
The present study demonstrated that the incidence of idiopathic SSNHL was highest in both males and females aged in their 60s, and the average patient age was 54.2 years (SD = 17.0). There was a tendency for the peak incidence to shift toward the older generation in comparison with the results of previous surveys in Japan [Citation1].
In this study, the patient medical history was included as part of the clinical data, and diabetes mellitus was reported in 17.1%, hyperlipidemia in 11.2%, kidney disease in 4.8%, brain infarction in 3.2%, and heart disease in 11.7% of patients included in this study. In the Japanese survey undertaken in 2001, 13.5% of patients had diabetes mellitus, 7.9% had hyperlipidemia, 2.0% cerebral infarction, and 8.0% had heart disease. Kidney disease was not reported in the 2001 survey [Citation1]. Higher incidences of all comorbidities reported in the patient medical history were noted in this study compared to those in the 2001 survey, and this may reflect an increase in the prevalence of those diseases in the elderly population itself.
Analysis of factors associated with the severity of SSHNL
In the present study, the average initial PTA for the affected ear was 69.2dB (SD =26.2), and the distribution of hearing grades was 15.2%, 22.3%, 37.4%, and 25.1%, for Grade 1, 2, 3, and 4, respectively.
Hearing grade distributions in the 2001 survey were 29.7%, 25.3%, 32%, and 13%, and those in the 2012 survey were 40.6%, 26.1%, 25.5%, and 7.7%, respectively. Based on these figures, we can see that the proportion of Grade 4 patients was higher in this study than in the past epidemiologic surveys in Japan. We speculate that this difference reflects the higher percentage (100%) of patients treated in tertiary care centers in this survey compared to the past surveys. In the 2001 survey, the total number of reported patients was 12,468, and the percentage of patients reported from university hospitals was 30.7% (3827 patients) [Citation1], while in the 2012 survey, the actual total number of reported patients was 4753, with the percentage of patients from university hospitals only 7.7% (365 patients) [Citation2].
We next examined the factors associated with the severity of SSHNL. The results of the statistical analysis showed that there were significant correlations between the severity of the hearing loss and diabetes mellitus, heart disease, age (under 16 years or elderly), and symptoms of vertigo/dizziness. Although kidney disease, past history of brain infarction, and gender were shown as significant prognostic factors by univariate analysis, they were excluded by the multivariate model.
Fukui et al. [Citation4] reported that idiopathic SSNHL patients with diabetes mellitus had more severe hearing loss than patients without diabetes mellitus. In that report, patient age and symptoms of vertigo were also found to be factors determining the severity of hearing loss, but the effect of diabetes mellitus on the severity of SSHNL was independent from those factors. In a temporal bone study of diabetes mellitus, histological findings revealed thickening of the wall of the inner ear microvasculature [Citation5], suggesting that diabetic patients might be at increased risk of ischemic injury to the inner ear.
Chronic kidney disease was reported as a risk factor for the onset of idiopathic SSNHL in a population-based cohort study from Taiwan (adjusted hazard ratio = 1.46) [Citation6], and several articles showed the presence of cochlear damage in patients with chronic renal failure on the basis of human temporal bone studies [Citation7]. In the present study, kidney disease was shown to be a significant prognostic factor by the univariate analysis, but was excluded by the multivariate model. One of the reasons for this discrepancy was that about half of the patients with kidney disease in this study had diabetes mellitus, which was more significantly related to the severity of hearing loss.
Brain infarction (only found to be significant by univariate analysis) and heart disease, which were related to the severity of idiopathic SSNHL in this study, have also been thought to be related to micro- or macrovascular insufficiency. The findings in this study supported the hypothesis that the disturbance of blood circulation in the inner ear is one of the possible causes of idiopathic SSNHL.
Type of treatment
Various treatments have been considered for idiopathic SSNHL. We examined the type of treatment recorded in this survey, and found that the majority of patients (92%) were administered some type of corticosteroid.
Amarillo et al. [Citation8] reported on a national survey in Spain, and found that corticosteroids were used to treat almost all of the survey subjects (99.7%). Although corticosteroids have been the mainstay of idiopathic SSNHL treatment since the report by Wilson et al. [Citation9], Alexander and Harris [Citation10] reported that the use of some type of corticosteroid was under 50% in United States in 2006 and 2007, based on the data from a medical and pharmaceutical claims database. In fact, initial corticosteroid treatment is regarded as an option in the American Clinical Practice Guidelines for SSNHL [Citation11]. Although certain regional differences therefore exist with regard to treatment, corticosteroids were regarded as the primary treatment modality in past surveys in Japan [Citation1,Citation2], and our findings confirm that the use of corticosteroids remains the standard treatment in Japan. In this study, several types of corticosteroids were used, such as prednisolone, hydrocortisone, betamethasone, dexamethasone, and methylprednisolone. Furthermore, the type of administration (oral or intravenous) and dosage depended on each institution. Prednisolone was used most frequently (∼60%), and hydrocortisone was used in 23% of cases. Further studies are needed to investigate the effect of corticosteroid type, administration route, and dosage on the prognosis of patients with idiopathic SSNHL.
Intratympanic corticosteroids were used in about 23% of cases in this study, although intratympanic treatment was never previously reported in epidemiologic surveys in Japan. As intratympanic administration was reported in 1.4% and 5.5% of cases, respectively, in Spain and the United States, this suggests that intratympanic treatment is more actively used in Japan, at least in university hospitals.
With regard to drugs administered concomitantly with corticosteroids, ATP, vitamin B12, and prostaglandin (PG) were recorded in the database. ATP and vitamin B12 were used in about 90% of cases. On the other hand, only 3.6% of the patients in this survey were treated by corticosteroids without any concomitant drugs. We also analyzed the relationship between the type of concomitant drug and the severity of hearing loss. The results indicated that PG has been commonly used for patients with severe hearing impairment. Ogawa et al. reported that no significant differences were observed in hearing improvement or subjective symptoms between the group treated with corticosteroids plus PGE1 and the group treated with corticosteroids plus placebo (without PGE1); however, the improvement in hearing in the higher frequencies was significantly greater in the PGE1 group than in the placebo group [Citation12]. In this survey, it seemed that there were various biases in terms of patient selection, so a larger prospective, randomized clinical study is needed to confirm the actual efficacy of the various treatments.
Analysis of factors associated with the prognosis of idiopathic SSNHL
In this study, the treatment efficacy for all patients, based on recovery criteria, was as follows; complete recovery was observed in 1317 patients (41.2%), marked improvement in 521 patients (16.3%), slight improvement in 549 patients (17.2%), and no change in 807 patients (25.3%). The 2012 Japanese epidemiologic survey using the same recovery criteria showed that 45.5% of patients achieved a complete recovery, 11.9% marked improvement, 15.5% slight improvement, and 27.4% no change [Citation2]. In addition, in a review of the Japanese literature regarding the treatment efficacy of idiopathic SSNHL from 1989 to 1998, Asakuma and Shida [Citation13] reported that a complete recovery was observed in 30.8%, marked improvement in 24.7%, slight improvement in 23.3%, and no change in 21.8% of patients. It is difficult to compare our findings with those of the previous reports simply because of differences in the subjects and treatments; however, good response rate, including a complete recovery and marked improvement, was roughly the same in this study as in the past reports.
We also examined the association between the prognosis of idiopathic SSNHL and several factors, such as hyperlipidemia, heart disease, aged 65 years or over, time from onset to treatment (over 7 days), and symptoms of vertigo/dizziness. Univariate and multivariate analysis were used to elucidate the existence of any relationships to poor prognosis. There was a statistically significant correlation between the severity of hearing loss (Grade 3 or 4) alone and poor prognosis in the univariate analysis, and diabetes mellitus alone was significantly related to prognosis in the multivariate analysis.
The presence of vertigo/dizziness was shown to be one of the negative prognostic factors in this study, and there have been many reports of the presence of vertigo being related to poor prognosis in idiopathic SSNHL patients [Citation14,Citation15].
As for comorbidities, our results demonstrated that hyperlipidemia and heart disease were related to the prognosis for idiopathic SSNHL. Although diabetes mellitus was one of the factors associated with the severity of idiopathic SSNHL, as described above, it was found that diabetes mellitus tended to be associated with a better response to the treatment. The reason for the tendency toward a better recovery in diabetic patients in our study is speculated to be due to differences in pathophysiology between diabetic patients and non-diabetic patients, although the cause remains unclear. For example, Yandani et al. reported that the genotype of macrophage migration inhibitory factor (MIF) was associated with the response to glucocorticoid treatment in patients with idiopathic SSNHL [Citation16], and that gene polymorphism of c.−173G>C was also related to the risk of diabetes [Citation17]. Further study is needed to clarify the association between diabetes mellitus and sudden hearing loss.
As cardiovascular risk factors are likely to be involved in the etiopathogenesis of some cases of idiopathic SSNHL, we recorded heart disease in this survey. In fact, Lin et al. [Citation18] suggested that idiopathic SSNHL was associated with the development of myocardial infarction. However, the concept of heart disease consists of several diseases with different pathogeneses, such as myocardial infarction, angina pectoris, and arrhythmia, and we believe that the details of patients reporting heart disease require further analysis.
Hyperlipidemia was found to be significantly correlated to poor prognosis in the present study, but the association between comorbid hypercholesterolemia or hyperlipidemia and hearing improvement in idiopathic SSNHL has been controversial in previously published articles. Lin et al. reported that hypercholesterolemia had a significant negative effect on hearing improvement in a large number of idiopathic SSNHL patients (781 patients) [Citation19]. The manner in which high cholesterol interferes with hearing recovery has not yet been investigated; however, high levels of total cholesterol were associated with an increased pro-thrombotic state.
Many articles in the past have suggested that hearing recovery is associated with the severity of the initial hearing impairment [Citation14,Citation15,Citation20]. In the present study, we used the hearing grade criteria determined by the Research Committee of the Ministry of Health and Welfare in Japan () for assessing the severity of hearing impairment, and demonstrated that the Grade 3 or Grade 4 patients showed worse hearing recovery than Grade 1 or Grade 2 patients. In fact, the rate of patients showing a complete recovery or marked improvement in each hearing grade was as follows: Grade 1 was 74.2% (316/442), Grade 2 was 55.4% (340/635), Grade 3 was 59.0% (589/1022), and Grade 4 was 48.0% (314/686). Patients with Grade 4 hearing impairment had significantly worse hearing outcomes than the other grades. Furthermore, the number of patients with Grade 4 hearing impairment showing a complete recovery was quite small at 10.3%. It appears that a more effective treatment method should be considered for idiopathic SSNHL patients with Grade 4 hearing loss.
In this study, the time from the onset of idiopathic SSNHL to the start of treatment was also identified as a prognostic factor for hearing recovery, with this result being consistent with most of the literature [Citation14,Citation15,Citation20]. The length of time from onset to treatment, however, differed from those in previous articles. Taken together, our study and past articles indicate that the initiation of treatment within at least seven days after onset is recommended for idiopathic SSNHL patients [Citation20].
Our results also indicated that age was strongly correlated with hearing recovery, with elderly patients (≧65 years) carrying a significantly higher risk of poor prognosis (OR 1.58). Although there are some reports that support this relationship between age at onset and hearing recovery in idiopathic SSNHL patients [Citation14,Citation15], the cutoff for patient age varies. On the other hand, some reports found no significant correlation between age and hearing recovery [Citation20]. Suzuki et al. reported on the prediction of hearing outcomes in idiopathic SSNHL using a multiple regression model, and found that the regression coefficient for patient age was 0.166dB per year [Citation15].
Although many articles have reported on the prognostic factors for idiopathic SSNHL, there is little consensus regarding the factors predicting hearing recovery in the literature. In most of the articles, the study population was at most 300 [Citation14,Citation15,Citation20], whereas in the present study we analyzed 3419 patients, and such a large-scale clinical survey is considered to be better suited to the analysis of the various complicated factors. Development of a more effective treatment for idiopathic SSNHL patients with negative prognostic factors is highly anticipated in the future.
Conclusion
In the present study, we examined the clinical features of idiopathic SSNHL in a database constructed on the basis of an epidemiologic survey, and analyzed the factors associated with the severity of hearing impairment and prognosis.
A large number of idiopathic SSNHL patients (n = 3419) were registered in the database, and the clinical characteristics of the idiopathic SSNHL patients were obtained.
We examined the factors associated with the severity of SSHNL, with the results of the statistical analysis showing significant correlations between the severity of the hearing loss and diabetes mellitus, past history of brain infarction, heart disease, age (under 16 years or elderly), and symptoms of vertigo/dizziness. We also examined the treatment type recorded in this survey, and found that the majority of patients (92%) were administered some type of corticosteroid. Intratympanic corticosteroids were also used actively in Japan, at least in university hospitals.
Furthermore, we examined the prognostic factors for idiopathic SSNHL, and found that the severity of hearing loss (Grade 3 or 4), heart disease, aged 65 years or over, time from onset to treatment (over 7 days), and symptoms of vertigo/dizziness were significantly related to a poor prognosis.
Acknowledgements
This study was supported by a Health and Labour Sciences Research Grant for Comprehensive Research on Disability Health and Welfare from the Ministry of Health, Labour and Welfare, Japan (http://www.mhlw.go.jp/english/) (S.U).
Disclosure statement
The authors alone are responsible for the content and writing of the paper. The Shinshu University Conflict of Interest Committee also approved the study.
Additional information
Funding
References
- Teranishi M, Katayama N, Uchida Y, et al. Thirty-year trends in sudden deafness from four nationwide epidemiological surveys in Japan. Acta Otolaryngol. 2007;127:1259–1265.
- Nakashima T, Sato H, Gyo K, et al. Idiopathic sudden sensorineural hearing loss in Japan. Acta Otolaryngol. 2014;134:1158–1163.
- Nomura Y. Morphological aspects of inner ear disease. Tokyo: Springer; 2014.
- Fukui M, Kitagawa Y, Nakamura N, et al. Idiopathic sudden hearing loss in patients with type 2 diabetes. Diabetes Res Clin Pract. 2004;63:205–211.
- Costa OA. Inner ear pathology in experimental diabetes. Laryngoscope. 1967;80:68–75.
- Lin C, Hsu HT, Lin YS, et al. Increased risk of getting sudden sensorineural hearing loss in patients with chronic kidney disease: a population-based cohort study. Laryngoscope. 2013;123:767–773.
- Oda M, Preciado MC, Quick CA, et al. Labyrinthine pathology of chronic renal failure patients treated with hemodialysis and kidney transplantation. Laryngoscope. 1974;84:1489–1506.
- Amarillo E, Hernández-García E, Herrera M, et al. Sudden hearing loss: National survey in Spain. Acta Otorrinolaringol Esp. 2016;67:59–65.
- Wilson WR, Byl FM, Laird N. The efficacy of steroids in the treatment of idiopathic sudden hearing loss. A double-blind clinical study. Arch Otolaryngol. 1980;106:772–776.
- Alexander TH, Harris JP. Incidence of sudden sensorineural hearing loss. Otol Neurotol. 2013;34:1586–1589.
- Stachler RJ, Chandrasekhar SS, Archer SM, et al. American Academy of Otolaryngology-Head and Neck Surgery. Clinical practice guideline: sudden hearing loss. Otolaryngol Head Neck Surg. 2012;146:S1–S35.
- Ogawa K, Takei S, Inoue Y, et al. Effect of prostaglandin E1 on idiopathic sudden sensorineural hearing loss: a double-blinded clinical study. Otol Neurotol. 2002;23:665–668.
- Asakuma S, Shida S. Review of papers ion the efficacy of the treatment in sudden deafness reported between 1989 and 1998 in Japan. J Otolaryngol Jpn. 2001;104:489–494.
- Harada H, Kato T. Prognosis for sudden sensorineural hearing loss: a retrospective study using logistical regression analysis. Int Tinnitus J. 2005;11:115–118.
- Suzuki H, Tabata T, Koizumi H, et al. Prediction of hearing outcomes by multiple regression analysis in patients with idiopathic sudden sensorineural hearing loss. Ann Otol Rhinol Laryngol. 2014;123:821–825.
- Yazdani N, Kakavand Hamidi A, Ghazavi H, et al. Association between macrophage migration inhibitory factor gene variation and response to glucocorticoid treatment in sudden sensorineural hearing loss. Audiol Neurootol. 2015;20:376–382.
- Coban N, Onat A, Yildirim O, et al. Oxidative stress-mediated (sex-specific) loss of protection against type-2 diabetes by macrophage migration inhibitory factor (MIF)-173G/C polymorphism. Clin Chim Acta. 2015;438:1–86.
- Lin C, Lin SW, Lin YS, et al. Sudden sensorineural hearing loss is correlated with an increased risk of acute myocardial infarction: a population-based cohort study. Laryngoscope. 2013;123:2254–2258.
- Lin CF, Lee KJ, Yu SS, et al. Effect of comorbid diabetes and hypercholesterolemia on the prognosis of idiopathic sudden sensorineural hearing loss. Laryngoscope. 2016;126:142–149.
- Ceylan A, Celenk F, Kemaloğlu YK, et al. Impact of prognostic factors on recovery from sudden hearing loss. J Laryngol Otol. 2007;121:1035–1040.
