Abstract
Objectives: The aim of this study was to investigate the differences between idiopathic sudden sensorineural hearing loss (SSNHL), and acute low-tone sensorineural hearing loss (ALHL) using the results of a nationwide survey database in Japan and to analyze the variables associated with their clinical features and the severity of hearing impairment, treatment, and prognosis.
Methods: Participants were patients registered between April 2014 and March 2016 in a multicenter epidemiological survey database involving 30 university hospitals and medical centers across Japan. Statistical analysis was performed to clarify the factors associated with their clinical characteristics and the severity of hearing impairment, treatment, and prognosis.
Results: Idiopathic SSNHL and ALHL differed significantly in terms of male-to-female ratio, age distribution, and time from onset to start of treatment. The treatment methods and hearing prognosis also differed markedly between the two diseases. A majority (92%) of idiopathic SSNHL patients were administered some type of corticosteroid, while half of the ALHL patients received corticosteroids and a diuretic agent.
Conclusion: The results suggested that idiopathic SSNHL and ALHL belonged to different categories of inner ear disease.
Chinese abstract
目的: 本研究的目的是, 使用日本全国调查数据库的结果, 调查特发性突发感觉神经性听力损失 (SSNHL) 和急性低音感觉神经性听力损失 (ALHL) 之间的差异, 并分析与临床特征、听力损伤的程度、治疗和预后相关的条件。
方法: 参与者是在2014年4月至2016年3月期间在一个多中心流行病学调查数据库登记的患者, 该数据库涉及日本全国30所大学医院和医疗中心。进行了统计分析以澄清与他们的临床特征、听力损伤程度、治疗和预后相关的因素。
结果: 特发性SSNHL和ALHL在男女比例、年龄分布和从发病到开始治疗的时间方面有着显著差异。治疗方法和听力预后在两种疾病之间也显著不同。大多数 (92%) 特发性SSNHL患者施用某种类型的皮质类固醇, 而一半的ALHL患者接受皮质类固醇和利尿剂。
结论: 研究结果显示, 特发性SSNHL和ALHL属于不同类别的内耳疾病。
Introduction
Sudden-onset sensorineural hearing loss consists of two similar clinical entities; idiopathic sudden sensorineural hearing loss (SSNHL) and acute low-tone sensorineural hearing loss (ALHL). Idiopathic SSNHL is defined as hearing levels for SSNHL of 30 dB or more over three consecutive frequencies [Citation1,Citation2]. However, a proportion of the patients whose initial audiograms met these criteria also met the criteria for ALHL (see in [Citation3]). ALHL is characterized by acute onset low-tone hearing loss often associated with tinnitus, ear fullness, and/or autophony. A series of reports have suggested that ALHL is correlated with endolymphatic hydrops or Ménière’s disease (MD) and the clinical characteristics and hearing prognosis of ALHL differ from those of idiopathic SSNHL [Citation4–6]. In this study, to investigate the differences between these two inner ear diseases, we compared SSNHL and ALHL from both a clinical and epidemiological perspective using a multi-center large cohort database involving 21 university hospitals and four medical centers.
Table 1. Criteria for diagnosis of sudden deafness.
Materials and methods
The subjects for this analysis were patients (3419 idiopathic SSNHL and 931 ALHL) registered in the multicenter database between April 2014 and March 2016. Twenty-one university hospitals and four medical centers participated in this epidemiologic survey. The recorded data included sex, age, body height, weight, affected side, date of onset, onset age, pure-tone audiogram, past history, and treatment. Hearing thresholds were measured at octave intervals between 125 Hz and 8 kHz. Initial and final audiograms were requested for all patients. All data, including the hearing thresholds in the audiograms, were entered into a computer database. From the audiogram data, the grade of the initial audiogram and the recovery rate, as defined by the Ministry of Health and Welfare in Japan [Citation7], were obtained. In some cases, the clinical data were incomplete, but our analysis included the available data for each category in such cases.
Idiopathic SSNHL and ALHL were defined according to the criteria established by the Sudden Deafness Research Committee of the Ministry of Health and Welfare, Japan (2012, 2011) as listed in and . Criteria for the severity of hearing loss in ALHL used in this study are shown in .
Table 2. Criteria for diagnosis of acute low-tone sensorineural hearing loss without vertigo.
Table 3. Criteria for the severity of hearing loss in acute low-tone sensorineural hearing loss (ALHL) (the Research Committee of the Ministry of Health and Welfare for Acute Profound Deafness, 2005).
The study protocol was approved by the Ethics Review Committee of Nagoya University as well as those of all the other universities. The data were analyzed using SPSS 24.0 for Windows (SPSS, Chicago, IL, USA). Statistical analysis was performed using the available data in each category, using a χ2 test and Student’s t-test. The level of significance was set at p < .05.
Results
Prior to detailed analysis, we performed data cleaning of both the idiopathic SSNHL and ALHL registered data. As a result of data cleaning, 67 cases registered as idiopathic SSNHL were found to fulfill the defined ALHL criteria and 36 cases registered as idiopathic SSNHL fulfilled the probable ALHL criteria. To aid in making a more precise comparison, we removed these 103 cases from the idiopathic SSNHL group in the further analysis.
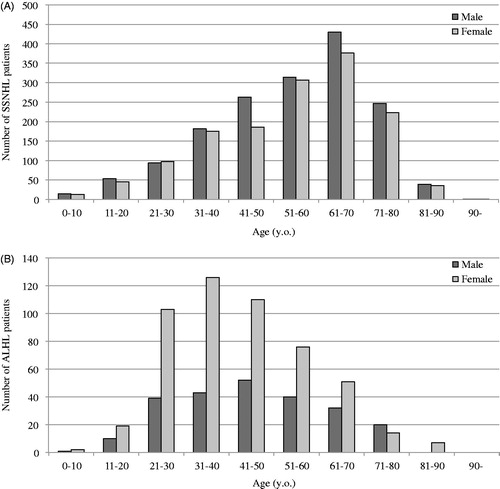
A comparison of the clinical characteristics in 3316 idiopathic SSNHL (male: 1719, female: 1556) and 931 ALHL (male: 241, female: 523) patients is presented in . The age of disease onset in patients with ALHL was significantly younger than that for idiopathic SSNHL. The mean onset age of idiopathic SSNHL was 54.5 years (SD =17.0) whereas the mean onset age of ALHL was 38.0 years (SD =18.8).
Table 4. Characteristics of the included patients.
The proportion of women with ALHL was significantly higher than that with idiopathic SSNHL. For all participants, the female:male ratio was 0.91:1 for SSNHL and 2.17:1 for ALHL. In patients <60 years old, the female:male ratio was 0.89:1 for SSNHL and 2.36:1 for ALHL (). These data indicated that there is a female predominance in ALHL (p < .01). The number of bilateral affected cases was significantly higher among the ALHL cases (p < .05) and the time from onset to start of treatment was significantly longer for ALHL (mean: 13.5 days) than for idiopathic SSNHL (mean: 6.5 days) (p < .01).
Figure 1. (A) Distribution of the incidence of SSNHL in males and females in each group. (B) Distribution of the incidence of ALHL in males and females in each group.
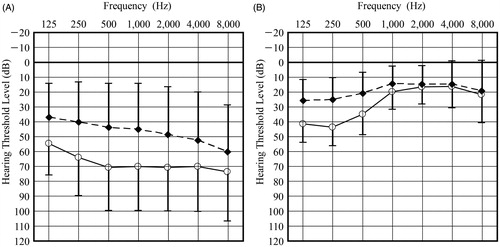
The initial and final average hearing thresholds at each frequency for SSNHL and ALHL are shown in . Both the initial and final average PTA for all frequencies were worse for idiopathic SSNHL than for ALHL. In idiopathic SSNHL, the final average hearing thresholds for high tones were relatively poorer than those for low tones.
Figure 2. (A) Average of initial and final pure tone audiograms for SSNHL patients. Initial average pure tone audiogram: solid line; final average pure tone audiogram: dotted line. (B) Average of initial and final pure tone audiograms for ALHL patients. Initial average pure tone audiogram: solid line; final average pure tone audiogram: dotted line.
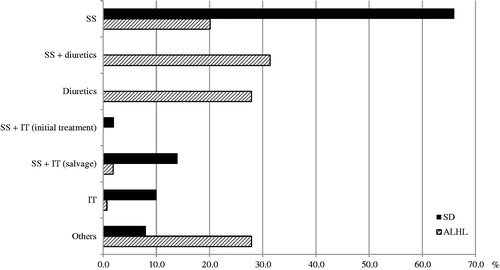
Systemic corticosteroids are commonly used to treat patients with acute sensorineural hearing loss (Kitoh et al. [Citation8], in this special issue). In idiopathic SSNHL patients, systemic steroids were the primary treatment, with intratympanic steroids chosen for salvage and substitute treatment (Kitoh et al. [Citation8], in this special issue). However, in ALHL patients, systemic or intratympanic steroids were used in only 54.1% and diuretic agents were used in 63.8% of patients. Combined treatment with steroids and diuretic agents was given in 31.4% of patients and diuretic therapy alone in 27.9% of patients (). The rates of complete recovery for ALHL patients were 72.0% in the systemic steroid group and 83.1% in the diuretic-only group. However, 41.3% of patients in the systemic steroid group had Grade 3 or 4 ALHL, while only 22.8% of patients in the diuretic-only group had Grade 3 or 4 ALHL. Most patients were simultaneously treated with vitamin B12 and adenosine triphosphate. The detailed treatments outcome of SSNHL and ALHL are described in other papers in this supplement [Citation8–10].
Discussion
The present results showed a clear difference between idiopathic SSNHL and ALHL in both clinical and epidemiological terms. Possible etiologies of SSHNL include viral infection, vascular impairment, autoimmune disease, inner ear pathology, and central nervous system anomalies, although the cause in most patients is never identified [Citation11]. On the other hand, ALHL has been hypothesized to be associated with endolymphatic hydrops on the basis of electrophysiological and audiological characteristics [Citation4–6]. Yamasoba et al. [Citation4] reported that ALHL patients frequently present with abnormal results for functional tests, such as the glycerol test or electrocochleography, and that over the long term, some patients develop cochlear or classic MD. Some reports have suggested similar clinical features or abnormal functional test results in ALHL patients and that ALHL may be caused by endolymphatic hydrops confined to the cochlea [Citation6]. Recent studies using magnetic resonance imaging have demonstrated that some patients with ALHL have evidence of endolymphatic hydrops [Citation3].
The incidence of idiopathic SSNHL was highest in older men, and that of ALHL was highest in younger women. These observations supported the view that some idiopathic SSNHL may be related to vascular disease, particularly as the rate of cardiovascular events increases with age [Citation12].
Our study showed a significant female predominance in ALHL patients, which is in agreement with the results of a previous study [Citation7]. The question of gender difference has been discussed for MD patients [Citation13], and a hormonal influence on MD has been suggested. In epidemiological studies, the gender difference in ALHL appears similar to that for MD. Nakashima et al. [Citation2] reported that among patients under 60 years of age, idiopathic SSNHL was more frequent in women than in men. This tendency was associated with the incidence of confirmed ALHL in young women. This must be viewed with some caution, however, as their study included only idiopathic SSNHL patients who visited private clinics. Therefore, there may be a certain sampling bias; i.e., this population might comprise mild cases and/or those associated with endolymphatic hydrops or MD.
We analyzed hearing recovery after treatment for idiopathic SSNHL [Citation7]. The average hearing level of idiopathic SSNHL patients was Grade 3 to Grade 2, according to these criteria, and it was found to improve by about 23 dB (slight improvement). In our study, idiopathic SSNHL had a poor hearing prognosis compared to that for ALHL, as shown in .
Diverse treatments have been considered for SSNHL and ALHL. Corticosteroids are a commonly used treatment for SSNHL in Japan [Citation2,Citation14]. Recently, intratympanic steroid administration has been used for some cases [Citation15–17]. In our study, most idiopathic SSNHL patients received systemic steroids as a primary treatment, whereas a combination of systemic steroids and diuretic agents was mainly used for ALHL patients. For cases of severe ALHL, systemic steroids alone or a combination of steroids and diuretic agents were frequently administered. Despite the fact that corticosteroids have been used as the general treatment modality for idiopathic SSNHL in Japan [Citation2,Citation14], the evidence for steroid treatment is controversial with no significant difference in hearing prognosis found in comparison with other treatments [Citation18–20]. To improve the treatment of SSNHL, it is important to clarify its pathophysiology. With regard to ALHL treatment, diuretic agents have been used in addition to corticosteroids [Citation21] as endolymphatic hydrops is speculated to be an etiology for ALHL as it is for MD [Citation3,Citation5].
Our large clinical database revealed differences in the characteristics of patients with idiopathic SSNHL and ALHL; however, idiopathic SSNHL and ALHL may include various pathophysiological states. Future physiological and imaging studies are needed to clarify the pathophysiological conditions responsible for these inner ear diseases.
Conclusions
The etiologies of idiopathic SSNHL and ALHL remain unclear. However, the present epidemiological survey suggested that there are clear differences between these two inner ear diseases, and that some ALHL patients should be treated as early stage MD.
Acknowledgements
This study was supported by a Health and Labour Sciences Research Grant for Comprehensive Research on Disability Health and Welfare from the Ministry of Health, Labour and Welfare, Japan (http://www.mhlw.go.jp/english/) (Shin-ichi Usami).
Disclosure Statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Additional information
Funding
References
- O’Malley MR, Haynes DS. Sudden hearing loss. Otolaryngology Clin North Am 2008;41:633–49.
- Nakashima T, Sato H, Gyo K, Hato N, Yoshida T, Shimono M, et al. Idiopathic sudden sensorineural hearing loss in Japan. Acta Otolaryngol 2014;134:1158–63.
- Shimono M, Teranishi M, Yoshida T, Kato M, Sano R, Otake H, et al. Endolymphatic hydrops revealed by magnetic resonance imaging in patients with acute low-tone sensorineural hearing loss. Otol Neurotol 2013;34:1241–6.
- Yamasoba T, Sugasawa M, Kikuchi S, Yagi M, Harada T. An electrocochleographic study of acute low-tone sensorineural hearing loss. Eur Arch Otorhinolaryngol 1993;250:418–22.
- Yamasoba T, Kikuchi S, Sugasawa M, Yagi M, Harada T. Acute low-tone sensorineural hearing loss without vertigo. Arch Otolaryngol Head Neck Surg 1994;120:532–5.
- Imamura S, Nozawa I, Imamura M, Murakami Y. Clinical observations on acute low-tone sensorineural hearing loss. Survey and analysis of 137 patients. Ann Otol Rhinol Laryngol 1997;106:746–50.
- Furuhashi A, Matsuda K, Asahi K, Nakashima T. Sudden deafness: long-term follow-up and recurrence. Clin Otolaryngol Allied Sci 2002;27:458–63.
- Kitoh R, Nishio SY, Ogawa K, Kanzaki S, Hato N, Sone M, et al. Nationwide epidemiological survey of idiopathic sudden sensorineural hearing loss in Japan. Acta Otolaryngol 2017; (in this special issue). DOI:10.1080/00016489.2017.1297537
- Okada M, Hato N, Nishio SY, Kitoh R, Ogawa K, Kanzaki S, et al. The effect of initial treatment on hearing prognosis in idiopathic sudden sensorineural hearing loss: a nationwide survey in Japan. Acta Otolaryngol 2017; (in this special issue). DOI:10.1080/00016489.2017.1296970
- Sato H, Kuwashima S, Nishio SY, Kitoh R, Fukuda S, Hara A, et al. Epidemiological survey of acute low-tone sensorineural hearing loss. Acta Otolaryngol 2017; (in this special issue). doi:10.1080/00016489.2017.1297538
- Chau JK, Lin JR, Atashband S, Irvine RA, Westerberg BD. Systematic review of the evidence for the etiology of adult sudden sensorineural hearing loss. Laryngoscope 2010;120:1011–21.
- Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation 1983;67:968–77.
- Alexander TH, Harris JP. Current epidemiology of Meniere’s syndrome. Otolaryngol Clin North Am 2010;43:965–70.
- Teranishi M, Katayama N, Uchida Y, Tominaga M, Nakashima T. Thirty-year trends in sudden deafness from four nationwide epidemiological surveys in Japan. Acta Otolaryngol 2007;127:1259–65.
- Morita S, Nakamaru Y, Fujiwara K, Iizuka K, Masuya M, Homma A, et al. The short- and long-term outcome of intratympanic steroid therapy as a salvage treatment for acute low-tone sensorineural hearing loss without episodes of vertigo. Audiol Neurootol 2016;21:132–40.
- Lavigne P, Lavigne F, Saliba I. Intratympanic corticosteroids injections: a systematic review of literature. Eur Arch Otorhinolaryngol 2016;273:2271–8.
- Jung dJ, Park JH, Jang JH, Lee KY. The efficacy of combination therapy for idiopathic sudden sensorineural hearing loss. Laryngoscope 2016;126:1871–6.
- Labus J, Breil J, Stutzer H, Michel O. Meta-analysis for the effect of medical therapy vs. placebo on recovery of idiopathic sudden hearing loss. Laryngoscope 2010;120:1863–71.
- Nosrati-Zarenoe R, Hultcrantz E. Corticosteroid treatment of idiopathic sudden sensorineural hearing loss: randomized triple-blind placebo-controlled trial. Otol Neurotol 2012;33:523–31.
- Wilson WR, Byl FM, Laird N. The efficacy of steroids in the treatment of idiopathic sudden hearing loss. A double-blind clinical study. Arch Otolaryngol 1980;106:772–6.
- Suzuki M, Otake R, Kashio A. Effect of corticosteroids or diuretics in low-tone sensorineural hearing loss. ORL J Otorhinolaryngol Relat Spec 2006;68:170–6.