Abstract
Objective: Tonsillotomy has emerged as an alternative for tonsillectomy in treating patients with tonsil-related afflictions. Tonsillotomy provides favourable outcomes in children, but treatment of choice in adults remains unclear. This systematic review sought to evaluate the current literature on the efficacy and adverse events of tonsillotomy compared to tonsillectomy in adults.
Methods: A Medline and Cochrane search was conducted for randomized clinical trials (RCTs) and cohort studies comparing tonsillotomy to tonsillectomy in adults. Risk of bias was assessed. Outcome measures were efficacy of the procedure in resolving the initial tonsil-related symptoms (tonsillitis, obstructive sleep apnoea, tonsil stones, halitosis, dysphagia), procedure-related complications, recovery time, post-operative use of analgesics, patient satisfaction, and operating time.
Results: In total nine papers were included. These trials had a high risk of bias and the inter-comparability of results was poor. The reported studies found generally a similar efficacy for both interventions. With regard to pain, the use of analgesics, patient satisfaction and operation time, the results were generally in favour of tonsillotomy. Post-operative haemorrhages were more frequent after tonsillectomy.
Conclusion: Current evidence suggests an equal efficacy of tonsillotomy and tonsillectomy in adults and a preference for tonsillotomy in terms of pain, analgesics use, patient-satisfaction, operation time and post-operative complications.
Chinese abstract
目的:扁桃体切开术已成为治疗扁桃体相关并发症时替代扁桃体切除术的一种方法。扁桃体切开术对儿童产生了有效结果, 但成年人的治疗选择尚不清楚。该系统综述旨在评估目前关于成人的扁桃体切开术与扁桃体切除术相比, 其疗效和副作用的文献。
方法:采用Medline和Cochrane搜索系统进行随机临床试验(RCTs)和队列研究, 来比较成人的扁桃体切开术和扁桃体切除术。检测了偏差风险。结果测量指标包括缓解初始扁桃体相关症状(扁桃体炎、阻塞性睡眠呼吸暂停、扁桃体结石、口臭、吞咽困难)的功效、手术相关并发症、恢复时间、术后止痛药的使用、患者满意度和手术用时。
结果:共有9篇论文被收录。这些试验有较高的偏差风险, 其结果的相互比较性较差。所报告的研究发现两种干预措施的效果相似。关于疼痛、使用镇痛药、病人满意度和手术时间, 结果一般都偏向于扁桃体切开术。扁桃体切除术的术后出血更为频繁。
结论:目前的证据表明, 扁桃体切开术和扁桃体切除术对成人具有相同的效果, 而在疼痛、镇痛药使用、患者满意度、手术时间和手术后并发症方面, 扁桃体切开术更有优势。
Introduction
Classic tonsillectomy, the surgical removal of the palatine tonsils, is one of the most performed surgical interventions in the head-and-neck area. Within the United States alone, over half a million tonsillectomies are performed every year. Tonsillectomies have been performed for over 3 millennia and even though different tonsillectomy methods have been developed over time, the traditional cold dissection tonsillectomy is still regarded as the gold standard.
The function of the palatine tonsils is related to the immune system, but their exact role in the immune response is under debate, especially since studies have shown that the function of the immune system was not compromised in early nor in late childhood in children that had undergone tonsillectomy compared to their age-matched healthy controls [Citation1].
Indications for tonsillectomy vary between the paediatric and adult population. In the adult population, tonsillectomy is mainly performed for chronic or recurrent tonsillar infections rather than for tonsillar hypertrophy with obstructive symptoms. Other indications for tonsillectomy in both adults and children include established or suspected tonsil-related malignancies and dysphagia related to the tonsils. Tonsil-related symptoms, such as halitosis, dysphagia and detritus (tonsil stones) are rarely an indication for tonsillectomy. The median recovery-duration after tonsillectomy is around 10 d for adults and 7 d for children. Post-operative haemorrhage rates after adult tonsillectomy are reported to be around 5% and post-operative infection rates around 1–7% [Citation2]. Adult patients suffering from tonsillitis are reported to both miss around 9 d of work and use antibiotics for 6 weeks on a yearly basis. Altogether, these data underline the fact that the burden of tonsillectomy for patients is not to be underestimated.
An alternative surgical intervention for tonsillectomy is tonsillotomy. Although first described more than a century ago, tonsillotomy has only become a regular intervention in several areas around the world since its re-introduction in the 1990s. Tonsillotomy is defined as the partial, intra-capsular removal of tonsil tissue, as opposed to the total, extra-capsular removal performed during tonsillectomy. Different synonyms are used in literature for the partial removal of tonsils, including tonsillotomy, partial tonsillectomy, tonsil ablation, intra-capsular tonsillectomy, radiofrequency-induced thermotherapy (RFITT) of the tonsils and subtotal tonsillectomy [Citation3]. Moreover, a wide variety of different surgical instruments have been used for tonsillotomy, including CO2-Laser, diathermy, radiofrequency, microdebrider, coblation, bipolar and cold-steel tonsillotomy. Tonsillotomy is mostly performed under general anaesthesia, but it can also be executed under local anaesthesia [Citation4].
Tonsillotomy is currently mostly used in children with paediatric obstructive sleep apnoea syndrome (pOSAS) and performed under general anaesthesia. A recent systematic review by Wood et al. showed a comparable effect of tonsillotomy versus tonsillectomy on improving sleep disordered breathing, whereas tonsillotomy was associated with fewer post-operative complications [Citation5]. However, there is insufficient data to show that a single technique for surgical tonsillotomy is superior to others, or to indisputably determine whether tonsillotomy can replace tonsillectomy [Citation6]. Moreover, currently available study reports do not allow for a reliable estimation of the chance of infection of tonsil remnants after tonsillotomy, which might lead to recurrent tonsillitis, but studies on children have reported a median recurrent tonsillitis rate following tonsillotomy of 3.9% [Citation6].
In adult patients, tonsillotomy is also increasingly performed, but not yet as frequently as in children. A well-designed overview of current literature comparing the efficacy and safety of tonsillotomy and tonsillectomy in adults is currently lacking. Therefore, the aim of this literature review was to evaluate the current literature on the efficacy and adverse events of tonsillotomy compared to tonsillectomy in adults suffering from tonsil-related diseases and afflictions and identify the knowledge gaps.
Materials and methods
We performed a systematic review following the Cochrane guidelines to assess the efficacy and safety in tonsillotomy versus tonsillectomy in adults suffering from a tonsil-related disease. This study was an exempt from institutional board approval as it is a review of previously published data.
Study groups (tonsillotomy)
Our predefined study group of interest consisted of adults or adolescent patients aged over 15 who had been treated with any technique of tonsillotomy for tonsil-related diseases. We used the system of Windfuhr and Werner to classify tonsillotomy interventions into two classes: tonsillotomy procedures in which only the protruding part of the tonsil, the part medial to the faucal pillars, is removed (class I), and tonsillotomy procedures in which only the inner surface of the tonsil-capsule is preserved and approximately 90% of the tonsil is removed [Citation3].
Control group
Our predefined control group consisted of adult patients with tonsil-related diseases who had undergone conventional tonsillectomy. Tonsillectomy was defined as the complete removal of the tonsil, including its complete capsule.
Tonsil-related diseases and afflictions
We included studies comparing the outcomes of tonsillotomy and tonsillectomy for the following tonsil-related diseases and afflictions: (recurrent) tonsillitis, peritonsillar abscess, obstructive symptoms including OSAS, dysphagia, halitosis and tonsil stones.
Outcome measures
Our predefined outcome measures of interest were efficacy of the procedure in terms of resolution of the initial tonsil-related symptoms that lead to surgery ([recurrent] tonsillitis, peritonsillar abscess, obstructive symptoms including OSAS, dysphagia, halitosis and tonsil stones), complications related to surgery, operating time, recovery time, post-operative pain and use of analgesics, and patient satisfaction.
Literature search
The predefined selection criteria were randomized controlled trials (RCT) and cohort studies comparing tonsillotomy to tonsillectomy in adult or adolescent (>15 y) patients, written in English, Dutch, French or German and published after 1960. We included studies with internal controls (one tonsil removed with tonsillotomy and the other with tonsillectomy in the same patient) and studies with external controls, which are patients undergoing classic tonsillectomies.
A three-step search strategy was executed. First, an initial limited search of MEDLINE and Cochrane collaboration databases was conducted, followed by an analysis of the wording used in the titles and abstracts, and of the index terms used to categorize the articles. Second, a search was performed using all the identified keywords and index terms across the MEDLINE and Cochrane databases. The following keywords and index terms were used: ‘tonsillotomy’, ‘partial tonsillectomy’, ‘subtotal tonsillectomy’, ‘intra-capsular tonsillectomy’, ‘hot tonsillectomy’, ‘radiofrequency-induced thermotherapy tonsil’, ‘RFITT’ and ‘tonsil ablation’. Third, the reference lists of all the identified reports and articles were searched for additional studies.
Risk of bias
Prior to inclusion, all papers selected for retrieval were assessed by two independent reviewers (J. W. C. and H. B.) for methodological validity using the Cochrane Risk of Bias Tool. This tool addresses possible bias, more specifically selection bias, performance bias, detection bias, attrition bias and reporting bias. Any disagreements that arose between the reviewers were resolved through discussion between the two reviewers or in consultation with a third reviewer (P. P. v. B.).
Results
Literature search
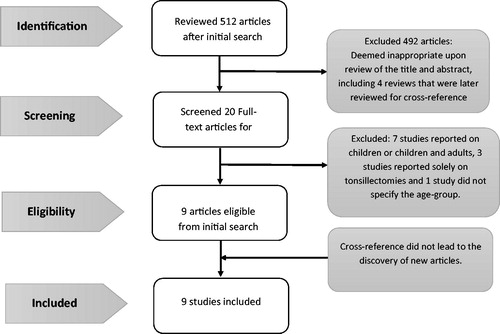
Our search and selection process are shown in . The initial search performed on 1 April 2017 identified 512 articles. Of these, the majority focused on paediatric patients and had study designs other than RCT. Based on title and abstract, we further excluded papers that did not match the objective of this study (e.g. studies that only examined extra-capsular tonsillectomies). Of a total of 20 articles eligible for full-text review, 3 studies were excluded because they only focused on extra-capsular removal of the tonsils (tonsillectomy), and 7 studies were excluded for reporting on paediatric or paediatric and adult patients and 1 study did not specify the age group. No additional articles were included after cross-reference checking of the included studies and reviews on tonsillotomies. This resulted in a total of nine RCT and cohort studies eligible for inclusion ().
Table 1. Characteristics of included studies.
The nine included RCTs and cohort studies reported on a total of 770 (284 in RCTs and 486 in cohort studies) adult patients. The term used most frequently for describing tonsillotomy was partial tonsillectomy. shows the distribution of the terms used for tonsillotomy in the literature.
Table 2. Terminology use in current literature for discribing tonsillotomy.
The papers by Ericsson and Hultcrantz [Citation7], Ericsson and Ledin [Citation8] and Wireklint and Ericsson [Citation9] reported on the same cohort of patients in Linköping, Sweden, using a consecutively longer follow-up period. From here on, we will refer to this cohort as ‘the Swedish cohort’.
Of all 770 patients, 485 (63%) underwent a tonsillotomy intervention and 327 (42%) underwent tonsillectomy. In the 42 patients included in the studies by Arya et al. [Citation10] and Hall et al. [Citation11], tonsillotomy was performed on one tonsil and tonsillectomy on the contralateral tonsil. We included these patients in both arms of our review, and outcome measures were included for the respective treatment.
The included papers studied different age ranges. The study by Bender et al. considered patients between 18 and 65 years as adults. Nemati et al. included all patients between 15 and 65 years, and Arya et al. reported on adults aged between 17 and 57. The Swedish cohort focused on ‘young adults’ aged 16 to 25 [Citation7–9], Hall et al. did not specify age other than ‘adults’ [Citation11]. Lourijsen et al. included all patients aged 18(4) and above and Johnston made a subdivision between teens (12–19 years old) and adults (>18 years old) [Citation12]. We included results from the adult patient group of Johnston et al.
Indication for surgery
Primary indications for surgery were tonsillitis in five studies [Citation4,Citation10,Citation12–14], obstructive symptoms with or without tonsillitis in five studies [Citation4,Citation7–9,Citation12], obstructive symptoms or recurrent tonsillitis in two studies [Citation4,Citation11], and halithosis, tonsilloliths and dysphagia in one study [Citation4].
Surgical technique
The surgical methods used for tonsillotomy were RFITT [Citation7–9,Citation11,Citation14], coblation tonsillotomy [Citation10,Citation11], CO2-laser tonsillotomy [Citation4], power-assisted tonsillotomy [Citation12] and scissor-assisted dissection of the tonsil part medial to the palatine arches followed by the removal of remnants with a microdebrider [Citation13] (). The surgical method for tonsillectomy was standard cold knife dissection in all studies except for the study by Arya et al. [Citation10], in which coblation was used for both tonsillotomy and tonsillectomy, and for the studies by Johnston et al. and Hall et al., which used electrosurgery [Citation11,Citation12].
The number of surgeons performing the surgical interventions was specified in five of nine studied populations. In the studies by Nemati et al. and Arya et al., operations were performed by a single surgeon [Citation11,Citation14]. The Swedish cohort was operated on by three surgeons, and in the study by Hall et al., the interventions were performed by six surgeons, four of whom had no prior experience with coblation tonsillotomy.
RFITT was performed differently in the study by Nemati et al. and in the Swedish cohort. In the study by Nemati et al., the bipolar linear RFITT probe was introduced into the crypts of the tonsils at five up to nine locations, depending on the size of the tonsils, and the tonsil tissue was vaporized with the power set at 7 watt to perform complete cryptolysis. Afterwards, probable bleeding sites were coagulated [Citation14]. In the Swedish cohort, the RF-probe was used to cut the tonsil parallel to the anterior pillar, followed by coagulation of bleeding vessels if necessary [Citation8].
Five studies performed a Class I tonsillotomy, and four studies performed a class II tonsillotomy (). Arya et al. and Hall et al. removed all tonsil tissue, except the tonsillar capsule, during coblation tonsillotomy [Citation10,Citation11].
Follow-up
Follow-up varied between all the included studies. Follow-up was 1 day in the study by Arya et al. [Citation10], 14 d in the study by Hall et al. [Citation11], 6 months in the study by Bender et al. [Citation13], 1 year in the study by Lourijssen et al. [Citation4] and 12 to 24 months in the study by Nemati et al. [Citation14] and 32 months in the study by Johnston et al. [Citation12]. In the consecutive papers on the Swedish cohort, follow-up was 3 weeks, 1 and 6 years [Citation7–9].
Risk of bias
Apart from the studies by Lourijssen et al. [Citation4] (prospective follow-up non-randomized cohort study) and Johnston et al. [Citation12] (retrospective study), all included studies were RCTs. Risk of bias is summarized in . Studies by Bender et al. [Citation13] and Arya et al. [Citation10] had low risks of bias [Citation10,Citation13]. The study by Nemati et al. had a medium risk of bias for blinding, the studies on the Swedish cohort [Citation7–9], the study by Lourijssen et al. [Citation4], Johnston et al. [Citation12] and the study by Hall et al. [Citation11] had medium and high risk of bias. Possible bias will be further debated in the discussion section of this review.
Table 3. Risk of bias of included studies (Cochrane risk of bias tool).
Table 4. Summary of outcomes.
Outcome measures ()
Efficacy (primary outcome)
Efficacy of the surgical intervention in resolving the initial tonsil-related symptoms was reported in six of nine papers and was evaluated differently between studies. Eight of nine studies showed no difference in efficacy between tonsillotomy and tonsillectomy, the study by Lourijssen et al. showed a significant better efficacy in favour of tonsillectomy. Bender et al. [Citation13] scored efficacy with the Tonsil and Adenoid Health Status Instrument (TAHSI). The TAHSI is a questionnaire for tonsil disease with a score ranging from 0 to 64, a higher score indicating more severe tonsil-related morbidity. The TAHSI score in the study by Bender et al. did change significantly after surgery, and there were no differences between the two treatment groups.
Nemati et al. [Citation14] did not find a difference between the two treatment groups in controlling recurrent tonsillitis in 12 to 24 months follow-up. In the Swedish cohort, efficacy was studied using the Short Form 36 Health Survey to evaluate Health-Related Quality of Life (HRQoL) and the EuroQol five dimensions questionnaire (EQ-5D VAS) scales to evaluate the self-rated overall health. The HRQoL and EQ-5D VAS scales did improve significantly after both interventions. No significant difference was found between the treatment groups at 1-year and 6-year follow-up. A significant decrease in ENT-infections was seen following both interventions at 1-year and 6-year follow-up, without any difference between treatment groups. Furthermore, the snoring intensity decreased in both treatment groups without a difference between treatments.
In the study by Lourijsen et al., 72.5% of patient were complaint free 1 year after tonsillotomy compared to 97.2% of patients after tonsillectomy (p < .001) [Citation4].
The study by Johnston et al. showed a difference in persistence of tonsillitis after both interventions in favour of tonsillectomy, but no statistical analyses had been performed between both groups [Citation12].
Complications
Complications were reported in all papers. Bender et al. [Citation13] reported post-tonsillectomy haemorrhage (PTH) in 16 of 54 patients (29.6%) after tonsillectomy and in 6 of 50 patients (12%) after tonsillotomy (p = .03). Furthermore, PTH was more severe and recurrent PTH was more frequent after tonsillectomy. In the Swedish cohort, six patients in the tonsillectomy group had a PTH (two primary, four secondary) [Citation7–9]. Hall et al. found two minor PTH on the coblation tonsillotomy side and one on the electrosurgery tonsillectomy side. None of the patients required transfusion or a return to the operating theatre [Citation11]. There were no primary or secondary haemorrhages in the tonsillotomy group, but in one patient there were difficulties in maintaining intra-capsular haemostasis during the tonsillotomy intervention and therefore surgery was converted to tonsillectomy. In the cohort studied by Arya et al., in which patients underwent tonsillotomy as well as tonsillectomy, PTH occurred in one patient, but the type of intervention causing the complication was not mentioned [Citation10]. No PTH occurred in the study by Nemati et al. [Citation14]. Lourijssen et al. reported a significant difference in PTH in favour of tonsillotomy: three (3%) PTH’s were seen after tonsillectomy, two requiring intervention and two (1%) PTH’s were seen after tonsillotomy, none requiring intervention [Citation4]. Johnston reported a PTH rate of 1.7% after tonsillotomy and 2.7% after tonsillectomy, no statistical analysis was performed [Citation12].
In addition, Lourijssen et al. reported four post-operative infections after tonsillectomy, none after tonsillotomy [Citation4]. Bender et al. reported more vomiting after tonsillectomy [Citation13], and Nemati et al. reported dysphagia in one patient after tonsillotomy caused by loose tonsil tissue in the throat post-operatively [Citation14]. No deaths occurred in any of the studies.
Pain
Post-operative pain or the use of pain medication was registered in all studies except in the study by Johnston et al. [Citation12]. Arya et al. did not find a difference in 24-h post-operative pain scores between the sides operated with tonsillotomy and the tonsillectomy sides [Citation10]. This finding does not come unexpected since significant relief of post-operative pain is not expected within 24 h. All other studies reported a difference in pain scores or analgesic medication use in favour of tonsillotomy. Bender et al. found that the tonsillotomy group used less and milder pain medication (only paracetamol and NSAID, instead of hydromorphone) than the tonsillectomy group [Citation13]. Hall et al. found less pain after tonsil ablation than after electrosurgical tonsillectomy [Citation11]. Nemati et al. found a lower pain score on day 1, 3, 5 and 10 after tonsillotomy [Citation14]. The differences in pain scores were significant after day 1 and day 3. In the Swedish cohort, patients who had undergone tonsillotomy recorded less pain from the first day onwards, required less analgesics and were pain free 4 d earlier than the tonsillectomy group [Citation7–9]. In the study by Lourijssen et al. both overall pain scores (5.4 after tonsillotomy and 7.7 after tonsillectomy) and analgesics use (median of 5.4 d after tonsillotomy and 9.6 d after tonsillectomy) were significantly different in favour of tonsillotomy. The days until resumption of daily activities were significantly different (4.8 d after tonsillotomy and 9.6 d after tonsillectomy) [Citation4].
Duration of surgery
Four studies reported on the duration of surgery. Bender et al. concluded that tonsillectomy prolonged the duration of surgery as compared to microdebrider-assisted tonsillotomy [Citation13]. Arya et al. concluded that the duration of coblation-assisted tonsillectomy was longer than the duration of coblation-assisted tonsillotomy [Citation10]. Hall et al. concluded that electrosurgical tonsillectomy took longer than coblation tonsillotomy [Citation11] and Lourijssen et al. found a shorter operation time after CO2-lasertonsillotomy compared to cold dissection tonsillectomy [Citation4].
Discussion
We conducted a systematic review to assess the value of tonsillotomy versus conventional tonsillectomy for tonsil-related diseases in adults. We identified nine studies comparing the efficacy of tonsillotomy and tonsillectomy. In eight of the nine studies, tonsillotomy was found to be as effective as tonsillectomy and nine of the nine studies was associated with less pain, a shorter period of recovery and a shorter duration of surgery.
This systematic review confirms that tonsillotomy versus tonsillectomy in adults has been scarcely studied. Our search only revealed nine papers describing randomized controlled trials or cohort studies comparing intra-capsular tonsillotomy with extra-capsular tonsillectomy, with a combined population of 770 patients. These studies made use of a variety of tonsillotomy methods, inclusion criteria and outcome measures, which led to poor inter-comparability and therefore no meta-analysis could be performed. Furthermore, some of the studies were of questionable quality. The study by Bender et al. was the only study of a relatively high quality, with a clearly stated randomization and sufficient patients to meet predefined power. Unfortunately, this study had a relatively high percentage of lost-to-follow-up of 16%, and blinding of outcome assessment was not mentioned. A per-protocol analysis was performed, but an intention-to-treat analysis would have been preferred in this study [Citation13]. The study by Nemati et al. had a high dispersion in follow-up time (range 12–24 months) and reported sparse data on group differences. Therefore, possible bias cannot be evaluated thoroughly [Citation14]. Arya et al. chose a very different study design, in which patients were used as their own controls. The number of studied patients was small with only 14 included patients, and follow-up for pain evaluation was as short as 24 h. Therefore, no meaningful statements can be made on pain, symptom improvement and post-operative bleeding. The study reported one complication, a PTH, but it did not state which type of intervention led to this complication. Moreover, patients being their own controls has its limitations in the context of the current interventions, since for example it may be hard to distinguish pain or discomfort from the one side or the other [Citation10].
The study on the Swedish cohort reported on a more substantial number of patients (n = 76) with a total follow-up period of 6 years. Unfortunately, patients were not blinded to treatment, and randomization and allocation were not stated. Therefore, subsequent bias cannot be ruled out. Patients lost to follow-up were excluded from the analyses, which may potentially have led to classification bias. The study by Hall et al. [Citation11] was, of all RCTs, most prone to bias. Randomization was based on order of presentation and was done before invitation to participate. Also, blinding was not performed correctly since two patients were operated by the primary investigator. Besides, there was no statistical correction for missing data during follow-up [Citation7–9].
The study by Lourijssen et al. is limited by a non-randomized non-blinded study-design with a high loss-to-follow-up in both treatment groups [Citation4]. A selection bias of highly motivated patients is expected for the tonsillotomy treatment-group since most of these were redirected especially to that specific hospital for outpatient laser treatment of their tonsils. The indication for surgery was significantly different between both groups (halithosis and tonsillolithiasis was predominantly treated with tonsillotomy) which makes the suspicion of selection bias stronger. Furthermore CO2-lasertonsillotomy, an intervention with a clear learning-curve was not solely performed by an experienced laser surgeons, but also by less experienced residents. Follow-up was 1 year, but tonsillitis has been shown to recur postoperatively predominantly after 1 year [Citation15].
The study by Johnston et al. has a retrospective study design with its inherent information bias and patient- and treatment-selection bias. This study sought to evaluate differences between teens and adults treated with powered intra-capsular tonsillectomy or monopolar electrocautery tonsillotomy and all analysis were based on this grouping. Therefore, no analysis was performed between both treatments and thus nothing can be said about statistical significance of the reported finding. The sizes of the groups were very disparate and the indications for intervention varied greatly as well [Citation12].
In summary, the selected randomized controlled studies and cohort studies on tonsillotomy in adults are very diverse with regard to study population, surgical methods used and outcomes measured. Thus, they cannot be compared to each other, and therefore the efficacy could not be evaluated by means of a meta-analysis. A better powered, well-designed randomized controlled trial needs to be undertaken to compare the efficacy and safety of tonsillotomy and tonsillectomy in adults and to allow for generalizable conclusions regarding the preferential surgical approach for tonsil surgery in adults. Especially recovery and complication rates should be evaluated and put in light of socio-economic perspectives. Furthermore, confounding by indication should be assessed beforehand, during patient inclusion.
Several procedural differences between tonsillotomy and tonsillectomy may explain the rather positive results that were reported in the few studies that we identified. Compared to tonsillectomy, tonsillotomy entails the removal of a smaller amount of tissue, while the major nerves and vessels running in the tonsillar bed to the tonsillar capsule are retained and only the smaller nerves and vessels that radiate into the lymphoid outer part of the tonsil are affected. This may limit the risk of PTH and post-operative pain. This assumption is supported by comparative studies of both interventions in paediatric populations, where this topic has been studied much more thoroughly. However, the anatomy of the palatine tonsillar region is strikingly different in children and adults. In children, the palatine tonsils lay relatively loose in the tonsillar bed and are only loosely connected by the vessel-nerve bundle between tonsillar bed and tonsillar capsule. In adults, on the other hand, the palatine tonsils are often more rigidly connected to the tonsillar bed, and this connection is often enhanced by recurrent or chronic tonsillar infections. Therefore, tonsillectomy in adults is generally more time-consuming, has a longer post-operative recovery time and is more frequently accompanied by PTH [Citation16]. Consequently, clinicians are generally much more reticent in performing tonsillectomy in adults than in performing the same operation in children [Citation13,Citation14].
Different methods for tonsillectomy and tonsillotomy have been described. The literature comprises reports on the use of CO2-laser, coblation, shaver (microdebrider), diode-laser, and radiofrequency. All these methods can be used for extra-capsular tonsillectomy as well as for intra-capsular tonsillotomy. However, regardless of the method used, tonsillotomy will result in less pain and lower post-operative bleeding rates. At present, conclusive evidence supporting the supremacy of any surgical technique is lacking. Two recent Cochrane reviews on tonsillectomy could not find a difference in morbidity between cold knife dissection and diathermy tonsillectomy, nor could they find a difference in post-operative pain or in the speed and safety of recovery between coblation and other tonsillectomy interventions. Magdy et al. could not find a difference in tonsillar fossa healing when comparing coblation, dissection and laser-assisted tonsillectomy, but monopolar cautery did show a slower healing process after 7 and 15 d [Citation17]. Coblation was associated with less thermal damage to surrounding tissue, which was presumed to be the result of the relatively low temperatures needed for sustaining the necessary plasma field. Currently, there is no sufficient evidence in favour of any method for tonsillectomy or tonsillotomy, and the choice of a surgical method is, at present, only based on the surgeon’s preference and the availability of equipment.
Tonsillotomy as a surgical method for tonsil-related diseases and afflictions is associated with several limitations. First, tonsillotomy is contraindicated when tonsil-related malignancy is suspected. In these cases, the tonsil should be preserved for examination by a pathologist, and tumour spread needs to be prevented. Second, although there is currently no evidence to support transmission of Creutzfeldt–Jakob disease through inhalation of vaporized tissue, some have suggested that this may be a theoretical risk. This risk is thought to be extremely low, but guidelines indicate that there is no hard data available. Third, the possibility of post-operative tonsillitis caused by residual tissue should be taken into account. Even though tonsillar remnants are also found after tonsillectomy, tonsil residues are always present in tonsillotomy and may (theoretically) lead to post-operative tonsillitis. No increase in post-operative tonsillitis rates was reported in the included studies, but there is no strong evidence that there is no difference in post-operative tonsillitis. Fourth, the possibility of regrowth of tonsils after tonsillotomy is often mentioned. Unfortunately, the risk of regrowth of tonsils in adults after tonsillotomy has not been reported in the literature and is thus a matter of ‘expert’ opinion. In adults, however, natural involution of the (palatine) tonsils is seen, and thus significant regrowth of tonsils in adults would be unexpected [Citation7,Citation18]. In children there are some data on regrowth: Doshi et al. reviewed 636 medical records of children that underwent tonsillotomy and concluded that there is a small risk of tonsillar regrowth and that regrowth is five times more likely at an age <5 years. Their findings were in concordance with the findings of other authors. Patients in the study on the Swedish cohort had surgery primarily for obstructive symptoms. At 6-year follow-up, no differences in snoring index or HRQL were found between the two treatments [Citation9]. This finding was in concordance with the studies by Hultcrantz et al. and Eviater et al., which found a similar effectivity of tonsillotomy compared to tonsillectomy in children with pOSAS after 10 years of follow-up. Based on these data and on our own clinical experience with tonsillotomy, we expect the need for secondary tonsillotomy caused by regrowth in adults to be low.
As was mentioned before, different surgical methods for tonsillotomy have been put into practice, but the inter-comparability between studies is lacking. The less invasive nature of a tonsillotomy enables surgeons to perform tonsillotomies in an outclinic setting using only local anaesthesia without sedation [Citation4,Citation19,Citation20], thereby reducing the morbidity of tonsil surgery. Tonsillotomy under local anaesthesia can drastically reduce the costs of tonsil surgery since the need for general anaesthesia and its associated specialty care disappears.
Other cost containments can possibly be found in the change in surgical tools, in the reduction of pain and in the reduced risk of PTH. A decrease in PTH does not only lead to a significant decrease in morbidity and mortality, but also reduces the costs of in-hospital stay, readmission and re-intervention. A reduction in pain leads to a decreased use of pain-medication, earlier discharge from the hospital and earlier return to work and or school and study, which results in considerable socioeconomic gain.
Conclusion
Current evidence suggests that the efficacy of tonsillotomy and tonsillectomy in adults is equal and that tonsillotomy is preferable in terms of pain, use of analgesics, patient satisfaction, operation time and post-operative complications. Post-operative haemorrhages were more frequent after tonsillectomy. This review only identified nine randomized controlled trials and cohort studies comparing the efficacy and safety of tonsillotomy and tonsillectomy in adults suffering from tonsil-related diseases and afflictions. An adequate powered, thorough and well-designed randomized controlled trial should be performed to conclusively bridge the knowledge gap necessary to clinically decide which method should be used in which patient.
Disclosure statement
No potential conflict of interest was reported by the authors.
All authors take responsibility for the integrity of the content of the review.
References
- Kaygusuz I, Alpay HC, Gödekmerdan A, et al. Evaluation of long-term impacts of tonsillectomy on immune functions of children: a follow-up study. Int J Pediatr Otorhinolaryngol. 2009;73:445–449.
- Bhattacharyya N, Kepnes LJ. Revisits and postoperative hemorrhage after adult tonsillectomy. Laryngoscope. 2014;124:1554–1556.
- Windfuhr JP, Savva K. [An update on tonsillotomy studies]. HNO. 2016;65:30–40.
- Lourijsen ES, Wong Chung JERE, Koopman JP, et al. Post-operative morbidity and 1-year outcomes in CO2-laser tonsillotomy versus dissection tonsillectomy. Acta Otolaryngol (Stockh). 2016;136:983–990.
- Wood JM, Cho M, Carney AS. Role of subtotal tonsillectomy ('tonsillotomy’) in children with sleep disordered breathing. J Laryngol Otol. 2014;128(Suppl 1):S3–S7.
- Windfuhr JP, Savva K, Dahm JD, et al. Tonsillotomy: facts and fiction. Eur Arch Otorhinolaryngol. 2015;272:949–969.
- Ericsson E, Hultcrantz E. Tonsil surgery in youths: good results with a less invasive method. Laryngoscope. 2007;117:654–661.
- Ericsson E, Ledin T, Hultcrantz E. Long-term improvement of quality of life as a result of tonsillotomy (with radiofrequency technique) and tonsillectomy in youths. Laryngoscope. 2007;117:1272–1279.
- Wireklint S, Ericsson E. Health-related quality of life after tonsillotomy versus tonsillectomy in young adults: 6 years postsurgery follow-up. Eur Arch Otorhinolaryngol. 2012;269:1951–1958.
- Arya A, Donne AJ, Nigam A. Double-blind randomized controlled study of coblation tonsillotomy versus coblation tonsillectomy on postoperative pain. Clin Otolaryngol. 2003;28:503–506.
- Hall DJ, Littlefield PD, Birkmire-Peters DP, et al. Radiofrequency ablation versus electrocautery in tonsillectomy. Otolaryngol Head Neck Surg. 2004;130:300–305.
- Johnston DR, Gaslin M, Boon M, et al. Postoperative complications of powered intracapsular tonsillectomy and monopolar electrocautery tonsillectomy in teens versus adults. Ann Otol Rhinol Laryngol. 2010;119:485–489.
- Bender B, Blassnigg EC, Bechthold J, et al. Microdebrider-assisted intracapsular tonsillectomy in adults with chronic or recurrent tonsillitis. Laryngoscope. 2015;125:2284–2290.
- Nemati S, Banan R, Kousha A. Bipolar radiofrequency tonsillotomy compared with traditional cold dissection tonsillectomy in adults with recurrent tonsillitis. Otolaryngol Head Neck Surg. 2010;143:42–47.
- Windfuhr JP, Werner JA. Tonsillotomy: it’s time to clarify the facts. Eur Arch Otorhinolaryngol. 2013;270:2985–2996.
- Windfuhr JP, Chen YS. Incidence of post-tonsillectomy hemorrhage in children and adults: a study of 4,848 patients. Ear Nose Throat J. 2002;81:626–628, 630, 632 passim.
- Magdy EA, Elwany S, El-Daly AS, et al. Coblation tonsillectomy: a prospective, double-blind, randomized, clinical and histopathological comparison with dissection–ligation, monopolar electrocautery and laser tonsillectomies [Internet]. 2008 [cited 2016 Nov 30]. Available from: /core/journals/journal-of-laryngology-and-otology/article/coblation-tonsillectomy-a-prospective-double-blind-randomized-clinical-and-histopathological-comparison-with-dissectionligation-monopolar-electrocautery-and-laser-tonsillectomies/EFB5CAAD6E4351DE28747E975D5F2226/core-reader
- Koempel JA, Solares CA, Koltai PJ. The evolution of tonsil surgery and rethinking the surgical approach to obstructive sleep-disordered breathing in children. J Laryngol Otol. 2006;120:993–1000.
- Remacle M, Keghian J, Lawson G, et al. Carbon-dioxide laser-assisted tonsil ablation for adults with chronic tonsillitis: a 6-month follow-up study. Eur Arch Otorhinolaryngol. 2003;260:456–459.
- Andrews PJ, Latif A. Outpatient laser tonsillar ablation under local anaesthetic. Eur Arch Otorhinolaryngol. 2004;261:551–554.