?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background: Ménière’s disease is characterised by episodic rotational vertigo, sensorineural hearing loss, tinnitus, and vegetative symptoms.
Objectives: The aim of our study is to follow-up the effects of the intratympanic steroid treatment of hearing loss in MD.
Material and methods: A group of 105 clinically diagnosed MD patients were enrolled in this investigation. Long-term follow-up was carried out, and pure tone speech audiometry results of the subjects before and after application of steroid were contrasted. Statistical analysis was carried out using the IBM SPSS V24 software.
Results: Based on the audiograms in this population, all stages of hearing loss were presented (from slight to profound). In most of the cases (68.6%), after intratympanic dexamethasone treatment, stagnation in the hearing profile was achieved. Moreover, there was a smaller group demonstrating hearing improvement after the treatment (12.4%). According to logistic regression [p = .001; Odds ratio: 2.75 (95% CI 1.068–4.442,)], there was a strong correlation between hearing improvement and dexamethasone treatment (all patients were treated with intratympanic dexamethasone, while improvement without steroid treatment could never be attained).
Conclusions and significance: Intratympanically administered dexamethasone is a potent agent to prevent the progression of hearing loss in MD.
Chinese abstract
背景: 美尼埃病的特征是间歇性旋转性眩晕、感音神经性听力损失、耳鸣和植物人症状。
目的:探讨鼓室内类固醇治疗MD听力损失的效果。
材料与方法:对105例临床确诊的MD患者进行研究。进行了长期随访, 比较了应用类固醇前后受试者纯音言语测听结果。使用IBM SPSS V24软件进行统计分析。
结果:根据该人群的听力图, 听力损失的各个阶段(从轻微到严重)都有存在。在大多数病例中(68.6%), 经鼓室内地塞米松治疗后, 听力出现停滞。此外, 还有一小部分患者在治疗后听力有所改善(12.4%)。根据逻辑回归[p=.001;优势比:2.75(95%可信区间1.068-4.442, )], 听力改善与地塞米松治疗之间有很强的相关性(所有患者均采用鼓膜内地塞米松治疗, 而不使用类固醇治疗永远不会取得改善)。
结论与意义:鼓室内给予地塞米松是预防MD听力损失恶化的有效药物。
Introduction
Ménière’s disease (MD) is a disorder of the membranous labyrinth of the inner ear, with constellation of cochlear and vestibular symptoms; manifesting themselves as vertigo, sensorineural hearing loss, tinnitus, aural fullness and vegetative symptoms, such as nausea and vomiting [Citation1]. Endolymphatic hydrops of the inner ear is the pathophysiologic entity of MD [Citation2]. It is difficult to estimate the real figures of MD, the literature reports about a prevalence of around 3.5–513/100,000, depending on the geographical location [Citation3]. It is more common in the fourth to sixth decades of life, is usually unilateral, but can be bilateral as well. Both sexes can have in MD, but a strong dominance of females can be observed in MD patients, similarly to other peripheral vestibular disorders [Citation4].
Although the unexpected paroxysm spells of vertigo have been described as the most tormenting symptoms, the hearing loss and tinnitus can be also unpleasant, due to its influence over the social activity of the patients suffering from MD [Citation5]. Hearing loss in MD is described as sensorineural. Initially, it is resolved completely between attacks, and in the early stages, low frequency (200–600 Hz) hearing loss can be detected with fluctuating tendency using pure tone audiometry [Citation6]. This fluctuation can also be defined by audiometry (wide variety, up to 60 dB) [Citation7]. Later, there is a progressive deterioration of hearing loss across the whole frequency spectrum (on 1500–2000 Hz too) [Citation8].
Locally administered steroid is one of the first-line treatments of the sensorineural hearing loss, and of the hearing loss of MD [Citation9–11]. Intratympanic drug therapies are based on the passage of intratympanically administered drugs into the inner ear, which are administered through the tympanic membrane and by diffusion from the middle ear into the inner ear through the round window. Clinically, intratympanically administered steroid injections have been proposed with good results [Citation12]. There are two main potential advantages of topical medication: reaching higher concentration in the perilymph with lower doses (in case of systemic therapy, high enough concentration could be achieved only with higher blood concentrations, which often causes side effects). Therefore, the systemic adverse effects could be avoidable (e.g. immunosuppression, Cushing-syndrome, osteoporosis, diabetes, hypertension, gastric ulcer and sarcopenia) [Citation13]. Although there are some possible complications of intratympanic use as well (post-ITI – intratympanic injection vertigo, tinnitus, burning sensation, small perforation, pain), these are not common, and most of them are transient [Citation14]. The effects of the steroids in the inner ear could be explained by two facts: high fat solubility and the low molecular weight of dexamethasone and the steroid receptors in the inner ear (Type I: low affinity receptors for mineralocorticoids, Type II: high affinity ones for e.g. dexamethasone) [Citation15]. The mechanism of action is complex, and little is known about the glucocorticoid effects in the inner ear: it could have effects on intra- and extra-cellular osmolarity, neural activity and electrochemical gradients [Citation16].
Despite the importance of the topic, little literature is available on the effectiveness of steroid injections in the treatment of hearing loss in MD. This study was undertaken to verify the possible efficacy of intratympanically administered steroids (dexamethasone) in the treatment of progressive sensorineural hearing loss of patients suffering from MD.
Materials and methods
Patients and data collection
A total of 105 patients (31 male and 74 female patients, mean SD age, 57.4
11.05) with definite Ménière’s disease according to the diagnostic scale of the Bárány Society were enrolled in this scientific investigation. Conducting the study was permitted by the Regional and Institutional Committee of Science and Research Ethics at Semmelweis University: 47/2018.
Administration of intratympanic steroids
The application of intratympanic steroid was performed under a microscope, and with the patients in supine position. After confirming the intact tympanic membrane and the status of the middle ear, local anaesthesia with 10% lidocaine pump spray was administered. After the anaesthetization, 4 mg/ml dexamethasone was instilled through the anteroinferior quadrant of the tympanic membrane. The procedure was carried out five times. Because in this population there was only unilateral MD and no bilateral, so intratympanic treatment was used always on the affected side (right: 42%, left: 58%). Before and 6–8 weeks after the treatment, pure tone audiometry was performed. Previously, before the IT treatment no other intratympanical therapy has been used; only conservative treatment based on international guidelines was performed to reduce the symptoms [Citation17].
Statistical analysis
The statistical analysis was completed by using the IBM SPSS V24 software. To illustrate our results, Kaplan-Meier curves were included, and log-rank test was used as well. The significance level was specified as p < .05.
Results
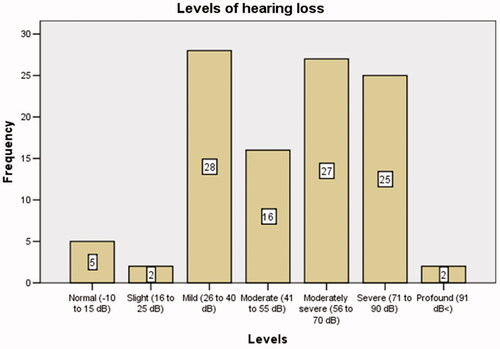
Through its progression, the hearing loss will affect all the frequencies, including those of human speech, which are of utmost importance. As shown in in our population, all levels of hearing loss could be detected.
We analysed the changes in the degree of the hearing loss after the treatment was concluded. In most of the cases (68.6%, n = 74), after the intratympanic dexamethasone treatment, stagnation in the hearing profile was achieved. This, of course, means that the already developed hearing loss could not be repaired, but we succeeded in stopping any further progression. Significant change in hearing profile was defined as follows: more than 10 dB improvement on the lower frequencies (250–1000 Hz) and more than 15 dB on the higher ones (2000–8000). In the ‘unchanged group’ there was lower than 10 dB improvement or impairment. There was a smaller population marked as ‘improved’ (12.4%, n = 14). The details of the results of the patients from the ‘improved group’ are shown in . Based on the pure tone audiograms (dB) the mean change in hearing was defined as 25.23 7.48 SD. The usual monitoring periods were 56.8
31.5 months, with five check-ups (which means control audiograms) in the process on average. Based on the control examinations the hearing improvement was permanent in all of the cases. In the ‘unchanged group’ in some of the cases there seemed to be a change during control audiograms, but these were transient and not enough to be significant. Unfortunately, in the ‘impaired group’ (19%, n = 17) a slow, gradual impairment was seen during the follow-up in most of the cases, but there was no impairment immediately after the IT treatment.
Table 1. Details of the audiometric results of patients from the ‘improved’ group.
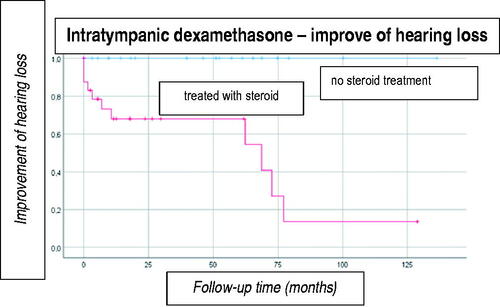
According to the analysis (), there is a very apparent correlation between the intratympanically administered steroid and the improvement of hearing loss: all patients from the ‘improved’ group were treated with intratympanic dexamethasone, while improvement without steroid treatment could never be attained. According to the log-rank test, significant correlation could be detected between the application of the dexamethasone and the improvement of the hearing loss [p = .001; Odds ratio: 2.75 (95% CI 1.068–4.442)].
In the following, we would like to expound a case from the ‘improved’ patient group, illustrated by pure tone speech audiograms before and after treatment.
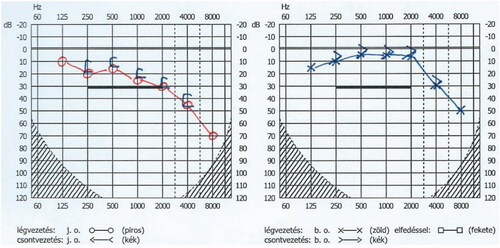
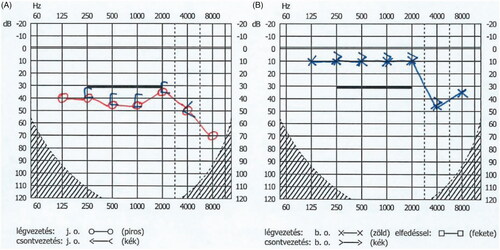
The patient whose audiograms are shown in and is a 69 years old male patient with a clinical diagnosis of MD on the right side for 3 years. He was in an attack-free period; however, he was complaining about disturbing hearing loss and aural fullness. He was hospitalised and treated by intratympanically administered dexamethasone. After the treatment, a 30 dB improvement on the involved side was achieved.
Figure 3. Audiogram of the patient before the dexamethasone treatment: moderate hearing loss on all frequencies on the affected side (A: right side). Normal hearing on the unaffected side in EH (B: left side). O: air conduction, [: bone conduction (right), x: air conduction, >: bone conduction (left).
Discussion
Based on our case report and long-term follow-up, intratympanically administered dexamethasone is effective in controlling the progression of hearing loss. Moreover, improvement could be achieved in some cases. Based on the statistical analysis, it was stated that every subject whose hearing loss was improved was treated with dexamethasone. Due to the local application, the side effects were negligible. In some of the cases, a short-lived vertigo occurred, but this complaint was transient. Other complications (just like perforation of the tympanic membrane) were not occurred.
The potential efficacy of intratympanic steroid was previously investigated by some authors. The results of Marco Antonio Garduño-Anaya demonstrated that, after dexamethasone inner ear perfusion, a subjective improvement in the hearing profile was attained; however the differences in the pure tone audiometry and speech discrimination test scores were not statistically significant [Citation18]. Later, Carlos Herraiz et al. found that transtympanic methylprednisolone is a potent and safe agent in the treatment of hearing loss: almost 50% of their cases showed a 10 + dB improvement in the hearing thresholds [Citation19].
Local administration is important to prevent side effects, however, systemic application do not have advantages. This type of application is based on the fact that microcirculation of the cochlea could be impaired by changes in the viscosity of the plasma, vasospasm, the sludging of red blood cells, etc. However, previously in SSNHL, no significant abnormality was found in blood cell count or in electrolyte levels [Citation16].
Limitations
The study was retrospective, but this way of investigation facilitates the long-time following of subjects, which is important because of the chronic nature of the disorder and the long-time efficiency of the therapy. The fluctuating progression of the disorder should be taken into consideration as well.
Disclosure statement
No potential conflict of interest was reported by the authors.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Harcourt J, Barraclough K, Bronstein AM. Meniere's disease. BMJ. 2014;349:g6544. doi:10.1136/bmj.g6544
- Oberman BS, Patel VA, Cureoglu S, et al. The aetiopathologies of Ménière's disease: a contemporary review. Acta Otorhinolaryngol Ital. 2017;37:250–263.
- Alexander TH, Harris JP. Current epidemiology of Meniere's syndrome. Otolaryngol Clin North Am. 2010;43:965–970.
- Molnár A, Maihoub S, Tamás L, et al. Possible effect of diabetes and hypertension on the quality of life of patients suffering from Ménière's disease. Orv Hetil. 2019;160:144–150.
- Havia M, Kentala E. Progression of symptoms of dizziness in Ménière's disease. Arch Otolaryngol Head Neck Surg. 2004;130:431–435.
- Mateijsen DJ, Van Hengel PW, Van Huffelen WM, et al. Pure-tone and speech audiometry in patients with Menière's disease. Clin Otolaryngol Allied Sci. 2001;26:379–387.
- McNeill C, Freeman SR, McMahon C. Short-term hearing fluctuation in Meniere's disease. Int J Audiol. 2009;48:594–600.
- Schuknecht HF. Meniere's disease: a correlation of symptomatology and pathology. Laryngoscope. 1963;73:651–665.
- Stachler RJ, Chandrasekhar SS, Archer SM, et al. Clinical practice guideline: Sudden hearing loss. Otolaryngol Head Neck Surg. 2012;146:S1–S35.
- Memari F, Hassannia F. Effect of intratympanic dexamethasone on controlling tinnitus and hearing loss in Meniere’s disease. Iran J Otorhinolaryngol. 2014;26:129–133.
- Filipo R, Covelli E, Balsamo G, et al. Intratympanic prednisolone therapy for sudden sensorineural hearing loss: A new protocol. Acta Otolaryngol. 2010;130:1209–1213.
- Dispenza F, Amodio E, De Stefano A, et al. Treatment of sudden sensorineural hearing loss with transtympanic injection of steroids as single therapy: a randomized clinical study. Eur Arch Otorhinolaryngol. 2011;268:1273–1278.
- Hoes JN, Jacobs JW, Verstappen SM, et al. Adverse events of low- to medium-dose oral glucocorticoids in inflammatory diseases: a meta-analysis. Ann Rheum Dis. 2009;68:1833–1838.
- Liu YC, Chi FH, Yang TH, et al. Assessment of complications due to intratympanic injections. World J Otorhinolaryngol Head Neck Surg. 2016;2:13–16.
- Pitovski DZ, Drescher MJ, Drescher DG. Glucocorticoid receptors in the mammalian inner ear: RU 28362 binding sites. Hear Res. 1994;77:216–220.
- Alexiou C, Arnold W, Fauser C, et al. Sudden Sensorineural Hearing loss: does application of glucocorticoids make sense? Arch Otolaryngol Head Neck Surg. 2001;127:253–258.
- Nevoux J, Barbara M, Dornhoffer J, et al. International consensus (ICON) on treatment of Ménière’s Disease. Eur Ann Otorhinolaryngol Head Neck Dis. 2018;135:29–32.
- Garduño-Anaya MA, Couthino De Toledo H, Hinojosa-González R, et al. Dexamethasone inner ear perfusion by intratympanic injection in unilateral Ménière’s disease: A two-year prospective, placebocontrolled, double-blind, randomized trial. Otolaryngol Head Neck Surg. 2005;133:285–294.
- Herraiz C, Plaza G, Aparicio JM, et al. Transtympanic Steroids for Ménière’s Disease. Otol Neurotol. 2010;31:162–167.