Abstract
Background: To assure a high quality in tonsil surgery, it is necessary to monitor trends in clinical practice, complications and outcome.
Aims/objectives: To describe rates and trends regarding indications, methods, techniques, complications, and outcome of tonsil surgery.
Material and method: 98 979 surgeries from the National Tonsil Surgery Register 2009–2018. Groups were categorised by indication and method.
Results: The proportion of patients undergoing tonsillotomy with adenoidectomy due to obstruction-snoring (mean age 5.3 y.) increased from 2009–2018. Hot tonsillectomy, but not tonsillotomy, techniques were related to a higher risk for postoperative bleeding. The use of cold techniques increased for all types of surgeries. The rates of patients reporting contact due to postoperative pain were associated with indication and method, with the lowest rate reported for tonsillotomy (4.5% in 2018) and the highest for tonsillectomy (34.5% in 2009). The rate of patients reporting that their symptoms were gone 6 months after surgery decreased.
Conclusions and significance: All hot tonsillectomy techniques should be avoided as they are related to a higher risk for postoperative bleeding. The high rate of postoperative contacts due to pain after tonsillectomy indicates a need for improvement in pain management. The declining rates of symptom relief must be investigated further.
Chinese abstract
背景:为确保扁桃体手术的高质量, 有必要监测临床实践、并发症和预后的趋势。
目的:描述扁桃体手术的适应症、方法、技术、并发症和结果的发生率和趋势。
材料和方法:2009-2018年美国国家扁桃体手术登记册中的98 979例手术。根据适应症和方法对组群进行分类。
结果:由于阻塞性打鼾(平均年龄5.3岁)而进行腺样体切除术的扁桃体切开术患者比例从2009年至2018年有所增加。热扁桃体切除术而不是扁桃体切开术导致更高的术后出血风险。对于所有类型的手术, 使用冷技术的人数都有所增加。报告因术后疼痛而接触的患者的发生率与适应症和方法相关, 其中扁桃体切开术的发生率最低(2018年为4.5%), 扁桃体切除术的发生率最高(2009年为34.5%)。术后6个月报告其症状消失的患者比例下降。
结论和意义:应避免使用所有热扁桃体切除术, 因为它们会增加术后出血的风险。扁桃体切除术后因疼痛引起的术后接触率很高, 这表明需要改善疼痛处理。症状缓解率下降的情况必须进一步调查。
Introduction
To assure health care quality, it is necessary to monitor outcomes and complications of surgical procedures. Considering the high number of tonsil operations performed worldwide, there is a need of analysing trends in clinical practice and related changes in complications and outcome. Most studies on tonsil surgery have been single-centre studies, randomised controlled trials based on a relatively small number of patients or cross-sectional in design. Such studies are not suitable for evaluating trends in clinical practice or detecting the consequences of changes in clinical practice over time. Given the relatively low frequency of observed adverse events after tonsil surgery, most studies, including many randomised controlled trials, also carry the risk of being underpowered. The IDEAL framework emphasizes the superior role of medical registers in evaluating trends in outcomes of surgical interventions [Citation1]. The National Tonsil Surgery Register in Sweden (NTSRS) is a large-scale national comprehensive multicentre register designed for this purpose.
There is in many aspects a gap in knowledge regarding how changes in tonsil surgery practice relates to changes in outcome and complication rates. We know from previous studies, that tonsil surgery practices are constantly changing. In recent years, outpatient surgery has replaced inpatient surgery. Furthermore, in many countries, a higher proportion of patients undergo surgery for upper airway obstruction compared to tonsillitis and tonsillotomy has in several European countries replaced tonsillectomy as the preferred surgical treatment of upper airway obstruction [Citation2–4]. Several studies published within the last 20 years have reported higher rates of postoperative bleeding after tonsil surgery performed with electrosurgical (hot) instruments compared to cold steel [Citation5–9]. Nevertheless, hot instruments seem to have become increasingly popular and whether this change in clinical practice have raised the overall rates of bleeding complications has not been investigated. Interestingly within the last ten years several studies report bleeding rates above 10% after tonsillectomy which are significantly higher numbers than previously reported [Citation10].
This study describes and analyses trends in indications, surgical methods, surgical techniques, as well as outcome, complications and outcome using data from the NTSRS. We specifically aim to analyse bleeding complications in relation to surgical techniques.
Materials and methods
This study is based on prospectively collected data from the NTSRS comprehensive national cohort. The NTSRS was initiated in 1997 by the Swedish Association for Otorhinolaryngology Head and Neck Surgery with the ambition to improve ENT care by monitoring trends in clinical practice, postoperative complications, and the outcome of tonsil surgery. The NTSRS aims to include all benign tonsil surgeries performed in Sweden. Participation in the NTSRS is voluntary for both surgical centres and patients; however, in recent years, the vast majority of Swedish ENT surgical centres have participated in the register, and approximately, 75% of all performed tonsil surgeries in Sweden since 2011 are included in the register.
All patients registered in the NTSRS between 1st March 2009 (commission date of the revised NTSRS) and 31st December 2018 were included. Data collection was based on three questionnaires. The first questionnaire was completed by the surgeon at the time of surgery and the second and third (PROM-questionnaires) answered by the patient or the caregiver 30 days and 6 months after surgery, respectively. Data on age, gender, indication, surgical method, surgical technique for dissection and haemostasis of the tonsils, and bleedings during the hospital stay were collected from the first questionnaire. The surgical technique for concomitant adenoidectomy is not registered in the NTSRS. The selectable indications for surgery are airway obstruction/snoring/tonsil hypertrophy (hereafter referred to as obstruction-snoring), recurrent tonsillitis, chronic tonsillitis, peritonsillitis, systemic complications to tonsillitis, and ‘other’. The definitions of these indications are (as described in the NTSRS manual): obstruction – snoring = sleep disordered breathing due to enlarged tonsils, recurrent tonsillitis = at least three episodes of tonsillitis the last year, chronic tonsillitis = at least three months with inflammation in the tonsils that affects daily activities, peritonsillitis = peritonsillar abscess and incipient peritonsillar abscess, systemic complication to tonsillitis = systemic disease that worsens due to tonsillitis, for example, psoriasis. The selectable methods of operation are tonsillectomy with or without adenoidectomy (TEA and TE) and tonsillotomy with or without adenoidectomy (TTA and TT). Tonsillotomy includes subtotal/intracapsular/partial tonsillectomy as long as a rim of tonsil tissue is preserved along the inner surface of the capsule. The second questionnaire contains several variables but, in this study, the dichotomous variables ‘contact with medical care due to pain’, ‘contact with medical care due to bleeding from the throat’ and ‘admission to hospital due to bleeding from the throat’ were chosen as measurements of postoperative complications. Bleeding complications reported by the patient (‘contact’ and ‘admission’ due to bleeding) was considered as late post-operative bleeding. From the third questionnaire, the proportion of patients reporting ‘The symptoms are gone’ 6 months after surgery were used as outcome measure of efficacy. The other outcome alternatives from which the patients could choose were “My symptoms are almost gone’, ‘My symptoms remain’, and ‘My symptoms have worsened’. A detailed description of the variables and the data collection procedure is available at the NTSRS website (https://ton.registercentrum.se/). The mean response rates for the second and third questionnaire (2009–2018) were 55% and 46% respectively.
In 2015, the results from an extended adjusted multivariable analysis on NTSRS data showed that both cold dissection with hot haemostasis (unipolar and bipolar diathermy) and hot dissection (bipolar diathermy scissors, coblation, ultracision) and thus per se hot haemostasis were associated with significantly higher odds ratio for ‘admission due to bleeding’ compared to purely cold techniques for surgery [Citation5]. Therefore, in this study, the surgical techniques were categorised into the following groups: cold/cold (cold dissection with cold haemostasis), cold/hot (cold dissection with hot haemostasis), and hot/hot (hot dissection with per se hot haemostasis).
In this study, patients were categorised by both indication and surgical method. There are six indications and four surgical methods in the register. A preliminary analysis of the 24 possible combinations of indication and surgical method revealed that the following eight groups of combinations comprised 96.3% of the total population; TE chronic tonsillitis, TE snoring, TE peritonsillitis, TE recurrent tonsillitis, TT obstruction-snoring, TTA obstruction-snoring, TEA obstruction-snoring, and TEA recurrent tonsillitis. These eight groups were used for all analyses in this study with the exception for the analyses regarding surgical techniques.
Statistics
Descriptive data were presented with numbers (n) and percentages (%). Trends and shifts in trends were tested by Join Point regression models (Join Point Regression program, version 4.6.– April 2018; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute), that identified points (Join Points) where linear trends of tonsil surgery changed significantly (significance level 0.01) in direction or magnitude. The rate of change for each trend was tested to determine whether the change was significantly different from zero. In the final model each trend was described by an annual percentage change (APC) with a 99% confidence interval (CI) [Citation11].
Relative risks (RR) with 99% CIs were calculated using binomial distribution with link function log as ratios of the haemorrhage rate with cold/cold technique used as reference. A multivariable logistic regression analysis using binominal distribution with link function log was performed to calculate RR adjusted for potential confounding factors (gender, age, adenoidectomy, and indication for surgery). For comparison between groups, Fisher’s exact test was used for dichotomous variables. All statistical analyses except Join Point regression were performed with the SAS System Version 9 (SAS Inst., Cary, North Carolina, USA).
Results
General characteristics
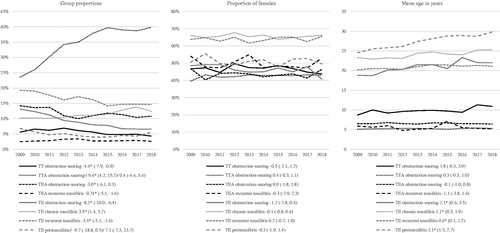
A total of 98,979 surgeries from 70 surgical units were included in the analysis. The number of patients in each group were: TT obstruction-snoring n = 5472 (5.5%), TTA obstruction-snoring n = 34,919 (35.3%), TEA obstruction-snoring n = 11,459 (11.6%), TEA recurrent tonsillitis n = 2814 (2.8%), TE obstruction-snoring n = 8620 (8.7%), TE recurrent tonsillitis n = 15,942 (16.1%), TE chronic tonsillitis n = 11,347 (11.5%), and TE peritonsillitis n = 4717 (4.8%). These groups had distinct age characteristics with four groups characterized by paediatric (<18 y.) mean age and four groups with an adult (≥18 y.) mean age. The age characteristics by group 2009-2018 were for the obstruction- snoring groups: TT mean age 9.9 y. (SD 8.9), TTA mean age 5.3 y. (SD 3.1), TEA mean age 6.6 y. (SD 4.8), TE mean age 20.8 y. (SD 13.8). For TEA rec. tonsillitis the mean age was 8.2 y. (SD 5.6), TE chronic tonsillitis mean age 24.2 y. (SD 11.0), TE rec. tonsillitis mean age 20.9 y. (SD 9.9), and TE peritonsillitis mean age 27.5 y. (SD 13.1). TE chronic- and recurrent tonsillitis groups had a distinct female majority, while the opposite was observed for TT- and TTA obstruction-snoring. Regarding changes in group proportions in the NTSRS, the most conspicuous change was an increased proportion of TTA obstruction-snoring (). This increase, from 24% to 40% of all registered surgeries, occurred in 2009-2014. A statistically significant trend of increased mean age was found for all TE groups (obstruction-snoring, chronic tonsillitis, recurrent tonsillitis and peritonsillitis) (). Notably, these were the groups with an adult mean age. No significant trends were detected, in any of the groups, regarding gender distribution (). No trend shifts were found regarding age or gender distributions.
Surgical technique
A cold/hot surgical technique was the most frequently used TE technique in both TE and TEA procedures, with a proportion varying between 48% and 64% ( and ). The proportions of cold/hot and hot/hot TE surgical techniques were statistically stable, in both TE and TEA procedures, while cold/cold surgical techniques increased. Hot/hot tonsillotomy surgical techniques dominated in both TT and TTA procedures throughout the studied period. The use of cold/cold TT surgical techniques increased significantly but from a very low proportion.
Figure 2. Rates of surgical techniques for TE and TT (in TE/TEA and TT/TTA procedures) 2009-2018. Presented with APCs and 99% CI. ‘Undefinable techniques’ is not presented in figure. *APC significantly different from zero at the 0.01 level. † Trend shift/Join point in in 2013.
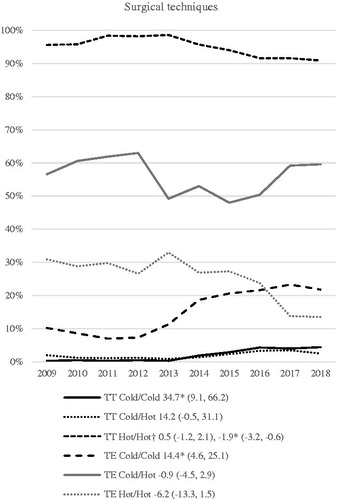
Table 1. Relative risks (RR) for postoperative bleedings related to surgical technique for dissection and haemostasis of the tonsils.
All cold/hot and hot/hot TE surgical techniques were related to a significantly higher risk for ‘contact due to bleeding’ and ‘admission due to bleeding’. Hot/hot surgical techniques were related to a lower risk of ‘bleeding during hospital stay’, while no such effect was noted for cold/hot surgical techniques. The main risk difference regarding both ‘contact due to bleeding’ and ‘admission due to bleeding’ was between cold surgical techniques and surgeries that included a hot surgical technique either for dissection or haemostasis. Moreover, all hot TE techniques registered in the NTSRS were related to an increased risk of late bleeding complications. The same analysis for TT procedures did not show any statistically significant differences between cold/cold and hot/hot surgical techniques for any of the studied bleeding complications.
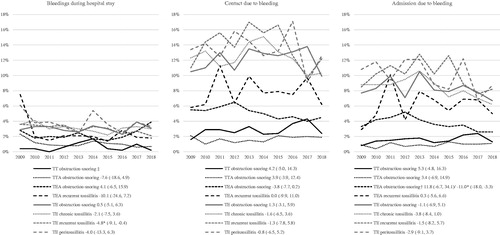
Bleeding complications and pain
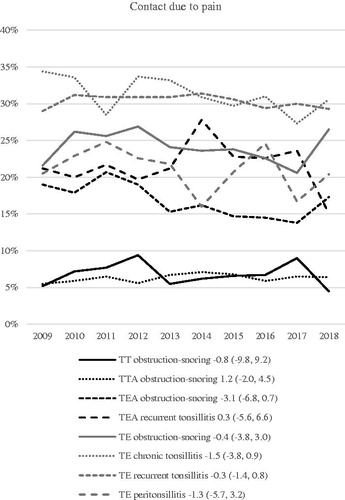
Only two significant trends were noted for all the bleeding complications (). TE recurrent tonsillitis ‘bleeding during hospital stay’ decreased from 2009–2018 (APC, −4.8) while ‘admission due to bleeding’ decreased from 2012 for TEA obstruction-snoring (APC −11.0). As shown in , the proportion of cold/cold TE surgical technique increased from approximately 10% 2009–2012 to 20% 2015–2018. This observed difference induced a post hoc comparison of the rates of both ‘contact’ and ‘admission’ due to bleeding after TE/TEA procedures for these periods (with adjustment for age, gender, indication, and adenoidectomy). The mean rate was 0.6% lower for ‘contact due to bleeding’’ (99% CI −1.6, 0.4, p = .017) and 1.0% lower for ‘admission due to bleeding’ (99% CI −1.9, −0.2, p < .001) in the late period compared to the early period. No statistically significant trend regarding the proportion of patients that reported both ‘contact due to bleeding’ and ‘admission due to bleeding’ was observed during the studied period. Regarding ‘contact due to pain’, no statistically significant trends were noted. Paediatric TT procedures were associated with lower rates (4.5–9.4%), while adult TE procedures were associated with higher rates (16–34%) of “contact due to pain”.
Outcome
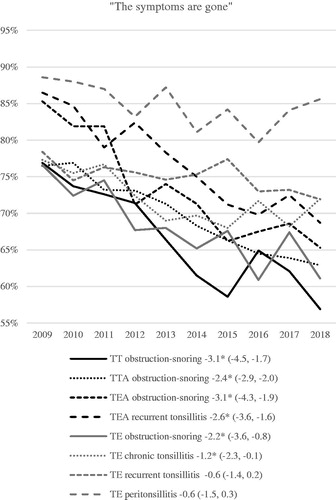
The proportion of patients that reported ‘the symptoms are gone’ 6 months after surgery decreased significantly without trend shifts in all groups, except in the TE recurrent tonsillitis and TE peritonsillitis groups (). The decrease was more pronounced in the paediatric obstruction-snoring groups and most pronounced in the TEA obstruction-snoring group. In this group, the rate decreased from 85% in 2009 to 65% in 2018, a reduction of 20% over 10 years.
Discussion
In this study, a decade of trends in tonsil surgery practices, outcome and complications were analysed by clinically relevant groups characterised by both indication and surgical method. The groups had distinct age and gender characteristics, without clinically significant changes during the study period. The proportion of patients undergoing TTA due to obstruction-snoring increased from 24% to 39%. Obstruction-snoring was the most common indication with 60% of all registered surgeries, especially dominant in groups with paediatric mean ages and male gender. Tonsillitis indications on the other hand were more prevalent in groups with adult mean ages and female gender. The outcome of surgery, measured as self-reported degree of symptom relief 6 months after surgery, decreased unexpectedly for almost all indications and methods, most pronounced for the groups operated for obstruction-snoring. Cold/cold TE surgical procedures were related to fewer late bleeding complications compared to any procedure involving a hot technique for either dissection and/or haemostasis. A significant increase use of cold/cold surgical techniques for both TE and TT procedures was noted. Regarding the bleeding complication rates, no statistically significant positive trend (i.e. lower rates of bleeding complications) was observed during the studied decade. However, a post hoc comparison of the rates of ‘contact-’ and ‘admission-’ due to bleeding after TE/TEA procedures 2009–2012 (when approximately 10% of the TE’s were cold/cold) compared to 2015–2018 (when approximately 20% of the TE’s were cold/cold) showed significantly lower rates of both bleeding complications, in the late period.
One important observation is that the rates of admission due to bleeding were stable within the studied period (2009–2018). This stands in contrast to the results from an other Swedish study were data from 1987 through 2013 showed increasing rates of readmission due to bleeding [Citation12]. The authors hypothesised that the observed increase in haemorrhages rate could be related to increased use of hot TE surgical techniques. This theory is supported by our data as we found that TE cold surgical techniques were significantly related to a lower risk of late bleeding complications. As the share of TE cold/cold surgical techniques increased 2009–2018 these findings may to some extent explain the levelling out of the increasing bleeding rates reported by Østvoll et al. [Citation12].
Given these observations, it is especially interesting to discuss the background to the significant increase in the proportion of cold/cold TE techniques. Over the years, several multicentre observational cohort studies have shown that hot techniques are related to increased rates of late bleedings after TE [Citation5–7,Citation9]. Also, information on the benefits of cold surgery was presented to the Swedish ENT surgeons in two NTSRS reports issued 2013 and 2014. In 2013–2014, the NTSRS conducted the first of two quality improvement projects (QIP) to reduce the rate of late bleedings. A major focus was given to strategies to increase the proportion of cold/cold surgeries. The evaluation of the QIPs showed that the participating clinics increased the proportion of cold surgeries resulting in decreased bleeding rates [Citation13]. In total, 13 of the larger Swedish ENT clinics participated in the QIPs. We hypothesise that the observed increase of TE cold/cold surgeries was an effect of the reports and the QIPs. However, the magnitude of change concerning surgical techniques should be considered moderate at best. And, as mentioned before, a related and apparent effect on bleeding rates could not be observed, even though bleeding rates were slightly lower during the late period (with 20% cold/cold surgery) compared to the early period (with 10% cold/cold surgery).
The rates of patients reporting ‘contact due to pain’ must be considered high, especially for adult TE procedures where >30% of the patients reported that they contacted a medical care unit due to pain during the post-operative period. In Sweden, there are national guidelines for post-tonsil surgery pain treatment in children but not in adults. In 2013, the informational website (www.tonsilloperation.se) was launched simultaneously with information of the newly developed Swedish guidelines for pain treatment after tonsil surgery in paediatric patients [Citation14]. One of the aims was to reduce the number of postoperative contacts due to pain as these contacts were supposed to be related to suboptimal information and pain treatment. The Swedish ENT community was made aware of the guidelines through several publications and two national meetings. A previous study on NTSRS data from 2009–2016 on the effect of these guidelines showed that the use of analgesics increased but without affecting the rate of ‘contacts due to pain’ [Citation15]. In our study, no effect of an implementation of the guidelines or the website (e.g. decreasing rates of patients contacting medical care due to pain) was observed in any of the groups with paediatric mean ages. Hypothetically, this could be due to several factors: Swedish ENT clinics have not implemented the guidelines, the variable ‘contact due to pain’ is not valid, the guidelines need to be adjusted or patients (and caregivers) are not following instructions. All of these possibilities will be addressed in future studies. The substantially higher rates of ‘contact due to pain’ in adults compared to children indicate that more focus is needed on treatment of adult post- tonsil surgery pain in the future.
The information provided online (www.tonsilloperation.se) might have concealed improvements in both bleeding and pain complications as the guidelines clearly stated that immediate contact with a medical professional should be made in all cases of bleedings and insufficient pain treatment.
An unexpected and somewhat alarming result of this study was that the proportion of patients reporting ‘The symptoms are gone’ of surgery declined in almost all groups, except TE recurrent tonsillitis and TE peritonsillitis. The decline was most pronounced in groups with obstruction-snoring indications and paediatric mean ages. We have no plausible explanation for this result. The Swedish guidelines with indications for tonsil surgery were published in 2009 and have not been revised. The incidence of tonsil surgery in Sweden was relatively stable between 2009 and 2018. By combining data from two surgical registers, the NTSRS and The National Patient Registry in Sweden, with population data from Statistics Sweden we know that the number of tonsil surgeries in Sweden per 100 000 inhabitants were 131 in 2009 and 128 in 2018. The lowest surgery rates were observed in 2011 (125) and the highest in 2012 (143). Among the different surgical methods TTA increased on behalf of TT, TE and TEA. These data indicate that lower thresholds for surgery are not the most plausible explanation (with the possible exception of TTA procedures) for the decreasing efficacy. Another explanation, however hypothetical, is that patients (or caregivers), during the studied decade, raised their expectations on the outcome of tonsil surgery. One way forward in order to investigate these trends could be to include validated questionnaires in the NTSRS to assess disease burden before and after surgery.
Methodological considerations/limitations;
While retrospective cohort studies are suitable to study associations, it must be borne in mind that they cannot tell anything about casual relations. Nevertheless, the NTSRS data reflect everyday clinical practice in a comprehensive national cohort. The size of the database and the consistency in the longitudinal data collection enables analyses not only on relatively rare post-operative complications but also effects of changes in clinical practice and efficacy of surgery over time. In these aspects, the NTSRS is unique and a complement to other types of studies, especially RCTs. A limitation of register data is the lack of randomisation; however, as the NTSRS covers surgery performed in all parts of Sweden, private and public surgical units, there is no reason to expect any systematic biases in this study. Another limitation is the response rate, where approximately half of the patients respond to the questionnaires. A comparison of the characteristics of responders and no responders has not revealed any significant differences related to age or gender.
Clinical applicability of the study and implications for the future
Based on the results of this study, it seems reasonable to recommend that all ENT surgeons use cold/cold surgical techniques for TE. This is in compliance with the recommendation from the British prospective tonsillectomy audit in 2004 [Citation8]. We are aware that other factors also affect complication rates (e.g. patient-related factors, individual surgical skills, and experience of the surgeon), but the group-level evidence on supporting cold/cold TE surgery is firm enough to support a general recommendation [Citation5–9,Citation16]. It has been argued that hot TE techniques give shorter surgical time, but this was not corroborated in a Cochrane review from 2017 [Citation17]. Even if hot surgeries were related to shorter time of surgery, the time gain would have to be clinically significant and large enough to balance the disadvantages, including the higher cost of single-use instruments. There is also evidence for greater pain after use of diathermy versus cold dissection, supporting the recommendation of the use of cold techniques [Citation18]. The decreasing rate of patients reporting that their symptoms are gone 6 months after surgery needs to be addressed.
Conclusions
This study shows that ENT surgeons that use hot techniques for TE should consider changing their practice and that surgical centres should analyse and compare their rates of pain complications and if needed revise their pain management strategies. All Swedish ENT surgeons should reflect on whether the decreasing rates of symptom relief is due to a shift in indications. Also, all ENT surgeons, ENT department heads, and Swedish health care policy makers need to reflect on how to facilitate implementation of the knowledge gained from the NTSRS to improve health care quality.
Data sharing
Data from the NTSRS is regulated by Swedish law. Research using NTSRS data may be carried out following approval by an ethics committee. Please contact the Centre of Registers Västra Götaland for more information ([email protected]).
Disclosure statement
There are no known conflicts of interest associated with this publication.
References
- McCulloch P, Altman DG, Campbell WB, et al. No surgical innovation without evaluation: the IDEAL recommendations. Lancet. 2009;374(9695):1105–1112.
- Bhattacharyya N, Lin HW. Changes and consistencies in the epidemiology of pediatric adenotonsillar surgery, 1996-2006. Otolaryngol Head Neck Surg. 2010;143(5):680–684.
- Borgstrom A, Nerfeldt P, Friberg D, et al. Trends and changes in paediatric tonsil surgery in Sweden 1987-2013: a population-based cohort study. BMJ Open. 2017;7(1):e013346. 2044-6055.
- Hultcrantz E, Ericsson E, Hemlin C, et al. Paradigm shift in Sweden from tonsillectomy to tonsillotomy for children with upper airway obstructive symptoms due to tonsillar hypertrophy. Eur Arch Otorhinolaryngol. 2013;270(9):2531–2536.
- Soderman AC, Odhagen E, Ericsson E, et al. Post-tonsillectomy haemorrhage rates are related to technique for dissection and for haemostasis. An analysis of 15734 patients in the National Tonsil Surgery Register in Sweden. Clin Otolaryngol. 2015;40(3):248–254.
- Lowe D, van der Meulen J. Tonsillectomy technique as a risk factor for postoperative haemorrhage. Lancet. 2004;364(9435):697–702.
- Sarny S, Ossimitz G, Habermann W, et al. Hemorrhage following tonsil surgery: a multicenter prospective study. Laryngoscope. 2011;121(12):2553–2560.
- Lowe D, van der Meulen J, Cromwell D, et al. Key messages from the National Prospective Tonsillectomy Audit. Laryngoscope. 2007;117(4):717–724.
- Tomkinson A, Harrison W, Owens D, et al. Risk factors for postoperative hemorrhage following tonsillectomy. Laryngoscope. 2011;121(2):279–288.
- Ostvoll E. Tonsil Surgery Register studies of Complications and Outcomes [dissertation]. Gothenburg: Sahlgrenska Academy, Institute of Clinical Science; 2019.
- Joinpoint Trend Analysis [Internet]. National Institutes of Health National Cancer Institute (US) [cited 2019 Dec 27]. Available from: https://surveillance.cancer.gov/joinpoint/.
- Ostvoll E, Sunnergren O, Stalfors J. Increasing readmission rates for hemorrhage after tonsil Surgery: A Longitudinal (26 Years) National Study. Otolaryngol Head Neck Surg. 2018;158(1):167–176.
- Odhagen E, Sunnergren O, Soderman AH, et al. Reducing post-tonsillectomy haemorrhage rates through a quality improvement project using a Swedish National quality register: a case study. Eur Arch Otorhinolaryngol. 2018;275(6):1631–1639.
- Ericsson E, Brattwall M, Lundeberg S. Swedish guidelines for the treatment of pain in tonsil surgery in pediatric patients up to 18 years. Int J Pediatr Otorhinolaryngol. 2015;79(4):443–450.
- Alm F, Jaensson M, Lundeberg S, et al. Adherence to Swedish guidelines for pain treatment in relation to pediatric tonsil surgery: A survey of the multidisciplinary team. Int J Pediatr Otorhinolaryngol. 2017;101:123–131.
- Elinder K, Soderman AC, Stalfors J, et al. Factors influencing morbidity after paediatric tonsillectomy: a study of 18,712 patients in the National Tonsil Surgery Register in Sweden. Eur Arch Otorhinolaryngol. (8)2016;273:2249–2256.
- Pynnonen M, Brinkmeier JV, Thorne MC, et al. Coblation versus other surgical techniques for tonsillectomy. Cochrane Database Syst Rev. 2017;8:CD004619.
- Pinder DK, Wilson H, Hilton MP. Dissection versus diathermy for tonsillectomy. Cochrane Database Syst Rev. 2011;3:CD002211.