Abstract
Background
Ultra-high-resolution computed tomography (U-HRCT) utilizes a 1024 × 1024 matrix with 0.25-mm section thickness, offering better spatial resolution than conventional multi-detector row CT to detect anatomic data for otologic surgery.
Aims
We examined stapes footplate thickness using U-HRCT in relation to stapedotomy to predict the difficulty of the surgical procedure.
Materials and methods
Subjects were 12 otosclerosis patients and 25 controls who underwent diagnostic U-HRCT. A profile curve (Hounsfield units) was used to measure stapes footplate thickness along a perpendicular line across the stapes footplate in a plane parallel to the lateral semicircular canal.
Results
Footplate thickness was smaller at the midpoint than just before the anterior crus and just after the posterior crus. Interobserver variability was lowest at the midpoint, where foot plate thickness was significantly greater in the affected ear in otosclerosis patients compared with controls (0.60 ± 0.09 mm vs 0.46 ± 0.04 mm; p < .001). Otosclerosis patients were detected using U-HRCT with a high area under the curve. Difficulty in the stapes opening procedure correlated with stapes footplate thickness.
Conclusions
Footplate thickness on U-HRCT correlated with temporal bone anatomy and corresponded to surgical difficulty.
Significance: U-HRCT-derived anatomic data is useful for evaluating the stapes.
Chinese abstract
背景:超高分辨率计算机断层扫描(U-HRCT)利用截面厚度为0.25毫米的1024 x1024矩阵, 比常规的多探测器行CT 提供更好的空间分辨率, 以检测用于耳科手术的解剖数据。
目的:我们使用U-HRCT检查与镫骨切开术相关的镫骨足板厚度, 以预测外科手术的难度。
材料和方法:受试者为接受诊断性U-HRCT的12名耳硬化症患者和25名对照者。轮廓曲线(Hounsfield单位)用于测量沿与侧半规管平行的平面上穿过镫骨足板的垂直线的镫骨足板厚度。
结果:足板厚度在中点处比前结节之前和后结节之后更小。观察者之间的差异性在中点处最低。与对照组相比, 耳硬化症患者的受累耳的该处足板厚度明显更大, 分别为0.60±0.09毫米和0.46±0.04毫米, p <.001。使用曲线下大面积的U-HRCT来检测耳硬化症患者。 镫骨打开手术的难度与镫骨足板厚度相关。
结论:U-HRCT的足板厚度与颞骨解剖结构相关, 并与手术难度相对应。
意义:U-HRCT得出的解剖数据对于评估镫骨非常有用。
Introduction
Otosclerosis is a multifactorial temporal bone disorder with genetic and environmental causes involving endochondral bone of the otic and labyrinthine capsules. The prevalence of clinical otosclerosis is approximately 0.3–0.4% in the United States, although the prevalence of subclinical histologically confirmed disease is higher [Citation1]. In 1841, Toynbee found stapes fixation in 39 of the 1659 temporal bones (2%) and thus established the link between deafness and stapes fixation [Citation2]. It is important to clarify the fine architectural changes in the temporal bone in order to enable accurate differential diagnosis of several middle and inner ear disorders from otosclerosis [Citation3]. The incidence of otosclerosis is estimated to be much lower in Japanese than in Caucasians [Citation4]. This is considered to be due to the low incidence of involvement of foci anterior to the oval window, low activity, and small lesion size without involvement of the foot plate and/or membranous labyrinth of the inner ear [Citation5]. Although otosclerosis is uncommon in the Japanese population, its incidence has been increasing [Citation4].
Stapedectomy and stapedotomy are both standard surgeries for otosclerosis, and stapedotomy provides better improvement in high frequency hearing and has low complication rates [Citation6]. The most important point in stapedotomy is adequate opening of the oval window to avoid damage to the inner ear [Citation7]. Stapes footplate thickness affects the difficulty of the surgical procedure for opening the footplate. Preoperative imaging is thus important for adequately examining the condition of the stapes footplate.
Ultra-high-resolution computed tomography (U-HRCT) scanning with ultra-small detector elements (0.25 × 0.25 mm) is currently achievable using the 160-row U-HRCT scanner (Aquilion Precision®; Canon Medical Systems, Tochigi, Japan) [Citation8]. U-HRCT affords better spatial resolution than multi-detector row CT, and has been successfully introduced into clinical use, for example, for imaging small lung lesions and small vessels in the brain and body [Citation9–11]. While smaller detector elements enhance the spatial resolution of CT images by reducing the partial volume effect, the utility of U-HRCT for evaluation of the middle and inner ear structures has not been fully evaluated. In otology, U-HRCT has been beneficial for detecting abnormalities of the ossicular chain and inner ear structures [Citation12,Citation13]. These anatomic data obtained by using U-HRCT may help in surgical planning for ear surgery.
In this study, we measured the thickness of the stapes footplate and bony change around the oval window in patients with otosclerosis. The aim was to examine the stapes footplate thickness detected by U-HRCT in relation to stapedotomy to predict the difficulty of the surgical procedure.
Subjects and methods
Subjects were 23 affected ears in 12 patients with otosclerosis who were clinically diagnosed based on tympanic membrane findings, audiometric examinations, and temporal bone imaging obtained by using a U-HRCT scanner between August 2017 and February 2020. Of the 12 patients with otosclerosis, eight underwent stapedotomy (unilateral seven and bilateral one) performed by four surgeons (TH, SK, AG, and MS). As controls, temporal bone images of 50 ears in 25 patients with ear drum perforation, sudden deafness, or facial palsy were analysed. These control subjects did not have any lesions around the stapes that would interfere with measurements. Clinical charts including digital recordings of the surgical procedure and operative records were reviewed and compared with U-HRCT findings.
All CT scans were performed with a U-HRCT scanner with 0.25-mm collimation (160 detector rows along the z axis, and 1792 channels with a 0.25-mm detector size in the x–y plane). The U-HRCT scanner settings were as follows: tube voltage = 120 kVp; tube current = 260 mA; collimation = 160 × 0.25 mm (step-and-shoot non-helical scanning); rotation time = 1.5 sec; imaging field of view (FOV) = 80 × 80 mm (matrix size of 512); slice thickness = 0.25 mm, reconstruction kernel = FC30; and image reconstruction = filtered back projection [Citation9].
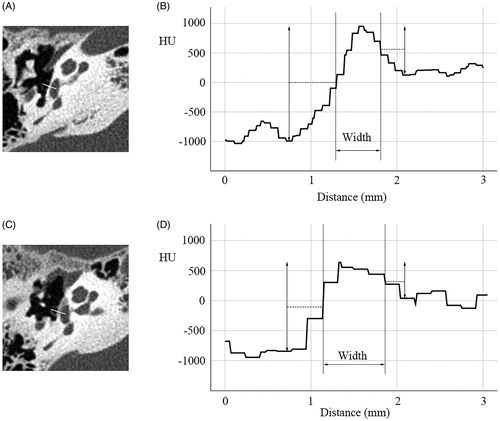
The Hounsfield unit (HU), which is a universally used dimensionless unit, enables quantitative measurement of radio density in the interpretation of CT images. On the HU scale, water is defined as 0 HU, and air is defined as −1000 HU, respectively. Retrospective image analysis was carried out using Ziostation 2 software (Ziosoft Inc., Tokyo, Japan). The HU value was measured along a perpendicular line across the stapes footplate in a plane parallel to the lateral semicircular canal (). The plane for measurement was selected so that the anterior crus (AC) and posterior crus (PC) in the footplate could be observed simultaneously. Profile curves, which demonstrated the HU value, were automatically created by the software along the perpendicular line. Based on the full width at half maximum (FWHM) method, the thickness of the footplate was semi-automatically measured on the profile curve ().
Figure 1. Measurement of stapes footplate thickness. (A) Normal control. Line in A represents a perpendicular line across the stapes footplate at the midpoint between the anterior and posterior crura. (B) Profile curve in A. Longitudinal axis shows HU value along the perpendicular line shown in A. Width was measured as representing stapes footplate thickness using the full width at half maximum (FWHM) method. (C) Otosclerosis patient. Line in C represents a perpendicular line across the stapes footplate at the midpoint between the anterior and posterior crura. (D) Profile curve in C. Longitudinal axis shows HU value along the perpendicular line shown in C. Width was measured using the FWHM method, resulting in much thicker width than in the normal control (B).
Footplate thickness was measured just before the AC, at the midpoint between the AC and PC, and just after the PC by three neuro-otologic surgeons (YA, TH, and SK) who were blinded to the patients’ clinical information. Interobserver variability at the three measurements points was investigated. Data were analysed using the SPSS statistical package (SPSS for Windows version 25.0; SPSS Inc., Chicago, IL).
This retrospective study was approved by the Institutional Review Board of University of the Ryukyus and carried out in accordance with the 1975 Declaration of Helsinki, as revised in 2008. Written informed consent from enrolled participants was waived and opt-out opportunities provided to these subjects.
Results
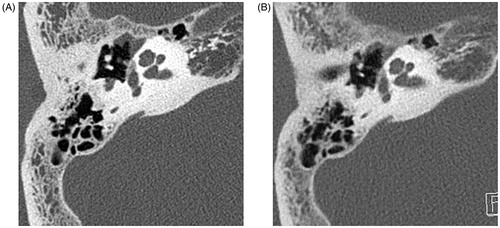
Mean age of patients (four males and eight females) with otosclerosis was 53 (range, 32–78) years while that of the controls (eight males and 17 females) was 50 (range, 10–78) years. There were no significant differences in age and sex distribution between the otosclerosis patients and controls. Of the 12 patients (23 ears) with otosclerosis, all had fenestral lesions, and one patient (two ears) had retrofenestral involvement in addition to fenestral lesion. The fenestral lesion was clearly identified on the U-HRCT image ().
Figure 2. Images from ultra-high-resolution CT (A) and conventional high-resolution CT (B) of the same patient. A. U-HRCT image (0.25-mm slice thickness) in the lateral semicircular canal plane. Decreased HU value in the fissula ante fenestram and stapes was noted. B. HRCT image (1-mm thickness) in the lateral semicircular canal plane. This image was obtained 3 months before A at another hospital. Lesions at the stapes and fissula ante fenestram are not clear on this image.
Footplate thickness in the controls
Mean footplate thickness determined by the three neuro-otologists in the control group was 0.61 mm at AC, 0.46 mm at the midpoint, and 0.64 mm at the PC (). Although there was no significant difference in footplate thickness between the AC and PC, footplate thickness was significantly smaller at the midpoint than at the AC and PC (Friedman test, p < .001). There was no significant difference in thickness between the right and left ears.
Table 1. Footplate thickness at three points in controls and otosclerosis patients.
Footplate thickness in the otosclerosis patients
Mean footplate thickness in the otosclerosis group was 0.94 mm at the AC, 0.60 mm at the midpoint, and 0.72 mm at the PC (). Footplate thickness was significantly greater at the AC than at the PC as well as at the midpoint (Wilcoxon’s test, p < .001). Also, footplate thickness was smaller at the midpoint than at the PC (Wilcoxon’s test, p < .001). Footplate thickness at the AC, midpoint, and PC was significantly greater in patients with otosclerosis than in the control group, respectively (Kruskal–Wallis, p < .001; p < .001; p < .002, respectively).
Interobserver variability at the three measurement points
Interobserver variability for all subjects including controls and otosclerosis patients was 0.306 at the AC, 0.536 at the midpoint, and 0.436 at the PC, which demonstrated fair to moderate interobserver agreement. Interobserver variability in patients with otosclerosis was 0.043 at the AC, 0.469 at the midpoint, and 0.310 at the PC, respectively. Thus, interobserver agreement was highest at the midpoint among the three-point measurements.
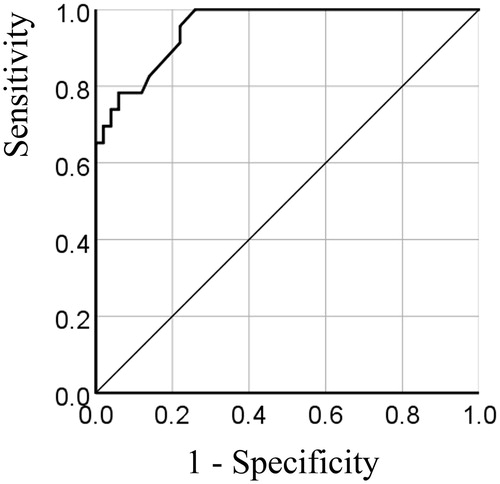
Receiver operating characteristic (ROC) analysis for stapes footplate thickness in controls and otosclerosis patients
Interobserver agreement was highest at the midpoint between the AC and PC, so stapes footplate thickness was measured at the midpoint for ROC analysis (). The ROC curve analysis yielded an area under the curve of 0.953 (95% confidence interval, 0.911–0.996). The maximum sum of specificity and sensitivity was observed at footplate thickness of 0.48. The sensitivity, specificity, positive predictive value, and negative predictive value for detecting otosclerosis were 100%, 74%, 64%, and 100%, respectively.
U-HRCT findings of stapes footplate thickness and surgical procedure
Of the 12 patients with otosclerosis, eight patients underwent stapedotomy (seven unilateral and one bilateral). No patient required revision surgery. Operators experienced some difficulty with the stapes opening procedure in one of the nine stapedotomy surgeries. This patient had a stapes footplate thickness of 0.81 mm at the midpoint, which was the greatest in this series.
Discussion
Evaluation of stapes footplate thickness in addition to adequate selection of prosthesis length is crucial in stapedotomy. In this study, stapes footplate thickness was successfully measured and was significantly greater in otosclerosis than in controls on U-HRCT. From the results of interobserver variability, the midpoint was the best point for measuring footplate thickness among the three points. ROC analysis revealed that patients with otosclerosis could be detected using U-HRCT. This is the first report to demonstrate the efficacy of stapes footplate thickness measurement by U-HRCT. Schuknecht and Barber reported on 164 (12.3%) otosclerotic lesions in the 1330 temporal bones in their collection, with and without stapes fixation [Citation14]. Otosclerotic foci were observed in 1.48% of 1011 temporal bones in a Japanese cohort [Citation5]. In our study, fenestral involvement was observed in all patients, but only one patient had retrofenestral involvement and the sample size was limited. Disease severity in patients with otosclerosis in this study was mild and the findings are consistent with previous studies in the Japanese population [Citation4,Citation5].
U-HRCT provides increased spatial resolution because of the halved collimation (0.25 mm) compared with that of conventional HRCT. The shape, thickness, and curvature of the footplate are variable. The medial surface of the footplate is curved and the annular rim has the greatest thickness in the posterior region and the smallest thickness in the anterior region [Citation15]. According to anatomic data of the stapes, the footplate thickness ranges from 0.228 to 0.411 mm [Citation16,Citation17]. Mean footplate thickness at the midpoint in our study was 0.46 mm in the controls. Thickness measured on U-HRCT was consistent with anatomic observations. A previous study using conventional HRCT for normal controls demonstrated that stapes footplate thickness was 0.27 mm on the stapes axial plane and 0.42 mm on the lateral semicircular canal plane [Citation18]. The plane in our study was similar to the semicircular canal plane used in this previous study. Because our data were similar to their footplate thickness data, the stapes axial plane in U-HRCT might be more helpful for determining the exact footplate size. However, stapes footplate thickness was successfully measured in otosclerosis patients as well as controls and differed significantly between the groups. The lateral semicircular canal plane is conventional and easy to use, and the semicircular canal plane in U-HRCT is also available for assessing the condition of the footplate because of the small partial volume effect.
Our findings suggest that stapes footplate thickness detected using U-HRCT corresponded to surgical difficulty, although the number of cases was small and the degree of otosclerosis was relatively mild. Our results also demonstrated that imaging data obtained using U-HRCT is consistent with the anatomy of the temporal bone, because it has smaller collimation, more channels and detector rows, and a smaller focus size than conventional CT. Further research is required to determine the usefulness of U-HRCT in otologic surgery, for example, selection of prosthesis length in stapes surgery and evaluation of postoperative prosthesis status, such as vestibular intrusion.
Methodological considerations/limitations
The number of patients with otosclerosis was too small to adequately evaluate the surgical procedure. In addition, the semicircular canal plane was examined, not the stapes axial plane, and there was significant difference between patients with otosclerosis and controls.
Acknowledgements
We thank the Ryukyu Society for the Promotion of Oto-Rhino-Laryngology for writing assistance and technical support.
Disclosure statement
The authors report no conflict of interest.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
References
- Quesnel AM, Ishai R, McKenna MJ. Otosclerosis: temporal bone pathology. Otolaryngol Clin North Am. 2018;51(2):291–303.
- Nazarian R, McElveen JT, Jr., Eshraghi AA. History of otosclerosis and stapes surgery. Otolaryngol Clin North Am. 2018;51(2):275–290.
- Revesz P, Liktor B, Liktor B, et al. Comparative analysis of preoperative diagnostic values of HRCT and CBCT in patients with histologically diagnosed otosclerotic stapes footplates. Eur Arch Otorhinolaryngol. 2016;273(1):63–72.
- Yagi T. Incidence and characteristics of otosclerosis in the Japanese population. Auris Nasus Larynx. 2002;29(3):257–260.
- Ohtani I, Baba Y, Suzuki T, et al. Why is otosclerosis of low prevalence in Japanese? Otol Neurotol. 2003;24(3):377–381.
- Cheng HCS, Agrawal SK, Parnes LS. Stapedectomy versus stapedotomy. Otolaryngol Clin North Am. 2018;51(2):375–392.
- Rask-Andersen H, Schart-Moren N, Stromback K, et al. Special anatomic considerations in otosclerosis surgery. Otolaryngol Clin North Am. 2018;51(2):357–374.
- Tanaka R, Yoshioka K, Takagi H, et al. Novel developments in non-invasive imaging of peripheral arterial disease with CT: experience with state-of-the-art, ultra-high-resolution CT and subtraction imaging. Clin Radiol. 2019;74(1):51–58.
- Xu Y, Yamashiro T, Moriya H, et al. Quantitative emphysema measurement on ultra-high-resolution CT scans. COPD. 2019;14:2283–2290.
- Meijer FJA, Schuijf JD, de Vries J, et al. Ultra-high-resolution subtraction CT angiography in the follow-up of treated intracranial aneurysms. Insights Imaging. 2019;10(1):2.
- Takagi H, Tanaka R, Nagata K, et al. Diagnostic performance of coronary CT angiography with ultra-high-resolution CT: comparison with invasive coronary angiography. Eur J Radiol. 2018;101:30–37.
- Hiraumi H, Obara M, Yoshioka K, et al. Detectability of minute temporal bone structures with ultra-high resolution CT. Auris Nasus Larynx. 2019;46(6):830–835.
- Yamashita K, Hiwatashi A, Togao O, et al. Ultrahigh-resolution CT scan of the temporal bone. Eur Arch Otorhinolaryngol. 2018;275(11):2797–2803.
- Schuknecht HF, Barber W. Histologic variants in otosclerosis. Laryngoscope. 1985;95(11):1307–1317.
- Sim JH, Roosli C, Chatzimichalis M, et al. Characterization of stapes anatomy: investigation of human and guinea pig. J Assoc Res Otolaryngol. 2013;14(2):159–173.
- Farahani RM, Nooranipour M. Anatomy and anthropometry of human stapes. Am J Otolaryngol. 2008;29(1):42–47.
- Veillon F, Riehm S, Emachescu B, et al. Imaging of the windows of the temporal bone. Semin Ultrasound CT Mr. 2001;22(3):271–280.
- Rousset J, Garetier M, Gentric JC, et al. Biometry of the normal stapes using stapes axial plane, high-resolution computed tomography. J Laryngol Otol. 2014;128(5):425–430.