Abstract
Background
Subglottic stenosis (SGS) is a narrowing of the airway just below the vocal folds. The cause of SGS and the optimal care for these patients, have remained elusive. Endoscopic surgery of SGS using either balloon or CO2 laser is associated with recurrence.
Aims and objectives
Our aim is to compare surgery free intervals (SFI) between these two methods applied in two different timeframes. The knowledge gained from this project can support decision-making regarding surgical method choice.
Material and methods
Participants were retrospectively identified using medical records between 1999 – 2021. We used pre-defined broad inclusion criteria to identify cases using the International Classification of Disease (ICD-10). Primary outcome was surgery free intervals.
Results
141 patients were identified, 63 met the criteria for SGS, and were included in the analysis. Results show no significant difference in SFI, comparing balloon dilatation and CO2 laser.
Conclusion
These findings demonstrate no detected difference in treatment intervals (SFI) when comparing these two commonly used surgical alternatives for SGS.
Significance
The outcome of this report supports surgical freedom of choice based on the surgeon’s experience and skill and ushes for further studies on patient experience regarding these two therapeutic approaches.
Chinese Abstract
背景:声门下狭窄 (SGS) 是声带下方的气道变窄。 SGS 的病因以及对患者的最佳护理, 仍然不太确定。 使用球囊或 CO2 激光的SGS内窥镜手术与复发有关。
目的:比较在两个不同的时段内采用两种方法之间的无手术间隔期 (SFI)。 从这个项目中获得的知识可有助于做出关于手术方式选择的决定。
材料和方法:根据1999 年– 2021 年期间的病历对参与者进行回顾性识别。我们根据预定义的广泛纳入标准, 使用国际疾病分类(ICD-10)来识别病例。 主要结果是无手术间隔期。
结果:确认了 141 名患者, 其中 63 名符合 SGS 标准, 并被纳入分析。结果显示, 比较球囊扩张和 CO2 激光两种方法, SFI 没有显著差异。
结论:这些发现表明, 当比较这两种常用的 SGS 手术方法时, 并没有检测出手术间隔期 (SFI)的差异。
意义:本报告的结果支持外科医生可以根据自己的经验和技能, 自由选择手术方式。本报告还呼吁进一步研究患者对这两种治疗方法的经历。
Introduction
Subglottic stenosis (SGS) is a recurrent disease characterized by progressive reduction of the airway due to soft tissue inflammation [Citation1]. Patients suffer from intensifying loss of breath, dyspnoea, wheezing, chronic cough, and affected voice. SGS is in most cases initially perceived as treatment-resistant asthma by both patients and providers; further diagnostics and treatment are therefore often delayed. New diagnostic methods are warranted and are under development [Citation2,Citation3]. The incidence of idiopathic SGS (iSGS) ranges from 2–2.5 cases per 1,000,000 individuals annually, with proposed local increase in a study from Canada [Citation4]. Including all known causes the incidence is reported to be 4.9 cases per 1,000,000 individuals annually with major impact on quality of life as well as on healthcare facilities [Citation3,Citation5]. The annual healthcare costs for patients with SGS are comparable to the financial challenges addressed patients with chronic diseases such as chronic obstructive pulmonary disease (COPD) and diabetes mellitus [Citation6]. SGS can develop after iatrogenic injuries, for example endotracheal intubation damage. Autoimmune disorders, such as granulomatosis with polyangiitis (GPA), are also recognized risk factors. However, in the majority of cases, the cause of SGS remains unknown. The unknown cause adds complexity in decision making regarding therapy, highlighting the need to map the therapeutic interventions available [Citation1].
SGS can be surgically managed through an endoscopic as well as an open surgical approach, where open surgery is reserved for more severe cases [Citation7]. Endoscopic surgical approaches are useful for limited soft airway lesions since the technique is less invasive, and usually facilitates quicker healing and recovery time compared to open surgical approaches [Citation8]. Medical treatment, most often corticosteroids or Mitomycin C, can be administered as single therapy, but are often used as adjuvant therapy to surgery, to reduce the associated inflammation of the SGS. The many available treatment options are in fact very much a reflection of the fact that there is no existing gold standard for treating SGS patients [Citation9]. Our clinic has used both surgical approaches, with CO2 laser as the main method between 1999 and 2009, and since then endoscopic balloon dilatation with adjuvant medical treatment is the preferred surgical approach. The cause for the change in regime was multifactorial, involving scientific reports at that time, local tradition and surgical preferences. Since there is no widespread consensus regarding treatment protocols today, the study outcome could have significant impact on choice of surgical method and SGS caregiving.
The study aim was to compare the treatment intervals between surgery using balloon dilatation (with adjuvant use of corticosteroid) and surgery using CO2 laser. Since we suspect that the CO2 laser approach can cause more scaring, our hypothesis is that the use of CO2 laser is associated with shorter surgery free interval (SFI).
Material and methods
Ethical approval
This study was performed according to the principles of the Declaration of Helsinki. The study was approved by the Regional Ethical Review Board of Umeå University, Sweden, approval number nr; 2020-00253 (2020-04-14). We confirm that all methods were performed in accordance with the relevant guidelines and regulations according to the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) checklist.
Study design
Retrospective observational, analytic case series.
Data collection
A flowchart for screening and inclusion of cases is presented in . Case demographics are shown in . Flowcharts for transparency of inclusion and exclusion criteria, case characteristics and determined sample sizes are provided in and .
Figure 1. Flow chart illustrating which diagnosis (ICD-10) patients were included also showing excluded cases.
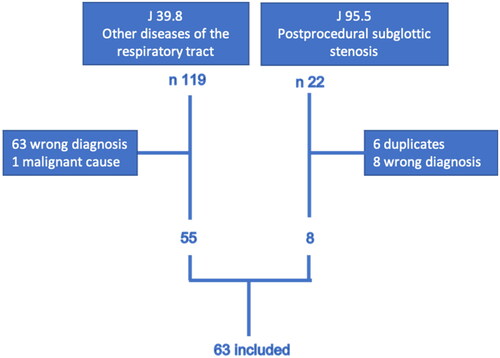
Table 1. Case characteristics.
Participant recruitment
Inclusion criteria for analysis were diagnosis codes defined by international classification of disease (ICD-10) in combination with medical records for evaluation of their accuracy, within the inclusion periods. The ICD-10 codes investigated were J39.8 (Other diseases of the respiratory tract), J95.5 (post-procedural subglottic stenosis), C32.1 (Malignant neoplasm; supraglottic), C32.2 (Malignant neoplasm: subglottic) and D14.1 (Benign neoplasm: larynx). The diagnosis was objectively confirmed by endoscopic and/or radiological findings in addition to subjective symptoms of airway obstruction. Due to the retrospective study design, we were not able to include other objectives than computer tomography and endoscopy using angle hook (5 mm). Several anatomical classifications have been proposed in an endeavour to classify the severity of SGS, of which Cotton-Mayer grading system is traditionally used worldwide[Citation1]. All patients with SGS as defined by declared ICD-10 codes, requiring surgical interventions at the Department of Otorhinolaryngology, University Hospital of Umeå, a tertiary referral hospital in Sweden, were included, between 1999 – 2021. The inclusion was based on presenting symptoms and/or pre-planned previous surgery follow up, objective findings endoscopically pre- as well as peri-operatively, confirming preoperative radiology and subjective respiratory distress. Patients with previous surgery as well as newly diagnosed cases were included when fulfilling the inclusion criteria within the given timeframe. A flow chart of eligible SGS samples is provided in . Exclusion criteria included static or dynamic stenosis in other parts of the airway such as in the thoracic trachea, glottis, supraglottic region, as well as narrowing due to external pressure or a malignant cause of the stenosis.
The primary outcome measure was surgery free intervals (SFI). Dates of surgery were identified and SFI were calculated and compared between the two methods. If a case had been treated with both methods the SFI was calculated separately for both methods, therefore the same case can be included in both groups where most cases were treated repeatedly. Since firstly, the scientific outcome is often affected by power failure, where small sample size undermines the reliability of the report and secondly, the fact that none of the cold steel instruments is associated with more scarring than the other in comparison to CO2 laser, we embraced radial incision followed by dilatation using (i) balloon technology, (ii) rigid dilatation with bronchoscopy and (iii) submucosal resection (including dilatation with bronchoscopy) as one group, reducing the purity of the groups and increasing risk of confounders. But it also equalises group sizes and increase sample size and as such enlarges the statistical power and reliability of the study outcome. Without hampering the purpose to compare CO2 laser with expected thermal effects and increased fibrosis to a dilatation procedure without thermal exposure independently of dilatation technology, including all accessible cases retrospectively.
Medical records were also evaluated for smoking status, age, age at onset, presence of systemic disease and age adjusted Charlson co-morbidity index (ACCI) [Citation10].
Surgical settings
CO2 laser wedge excision [Citation11] and balloon dilatation are the two predominant methods used during our study period. All cases were treated under general anaesthesia using total intravenous anaesthesia with muscle relaxant medication described as combination of anaesthetic drugs given intravenously without inhalation preparations. Regardless of surgical method all patients were assessed peri-operatively with microscope, rigid operating laryngoscope designed for use with the Twin Stream ventilator (balloon procedure) and 0° degree optic rigid laryngoscope for larynx surgery. Ventilation was managed with jet ventilation technique (at present Twinstream ref: CTNS-110-000) via catheter (CO2 laser) or superimposed supraglottic ventilation (balloon procedure). A Sharplan 40 C Surgitouch CO2 laser was used 1999–2009 with a transition to a more updated CO2 laser unit (Lumenis acupulse 40 AES-A with acupulse DUO module) in the final phase of the earlier timeframe. The surgery was performed using a line-of-sight micromanipulator (Lumenis EcoSport 712 L micromanipulator ref: AA3042000) attached to the microscope, and 3 radial incisions are made with the CO2 laser in the stenotic area.
The balloon dilatation procedure is the more recently preferred method for SGS surgery at our clinic, preceded by radial incisions made by a cold steel knife. The dilatation is carried out under apnoeic conditions, using a high-pressure balloon, inflated with saline until the pre-defined pressure and balloon size is reached. This creates consistent radial pressure to the stenosis for approximately 2 min. A total of 0.4–0.5 ml of methylprednisolone 40 mg/ml is injected before dilataion is completed. The balloon used is a Boston Scientific pulmonary Balloon dilatation catheter 12–15 mm diameter 3 cm long (ref M00550330) or 15–18 mm diameter 5,5 cm long (ref M00550310). Size of the balloon was chosen based on the appearance of the stenosis during surgery.
Statistical analysis
The mean surgery free interval (SFI) for each case was calculated using SPSS version 28. To increase the number of calculated datapoints besides mean SFI we adopted a model that allowed us to include all surgical events and baseline characteristics in the analysis. This resulted in a Cox proportional hazards (PH) model, employing the Andersen–Gill extension to allow for multiple events per subject [Citation12]. Besides the main exposure variable, SFI, the model also included age, sex, smoking status, age adjusted Charlson Comorbidity Index (ACCI) group classification, and presence of systemic disease to be able to compare balloon dilatation and CO2 laser procedures in a larger overall perspective. The assumption of proportional hazards was tested for each individual covariate using Schoenfeld residuals [Citation13]. In case the assumption of proportional hazards was not met, an additional stratified analysis was performed using the covariate in question as a stratification variable - thus excluding the possibility of computing a hazard ratio with associated confidence interval/significance test for that covariate. For such cases, the estimated baseline hazards for different strata are presented graphically for visual comparison. Analyses were performed applying the survival package in the R software, version 4.0.2. A result was considered statistically significant if the corresponding p-value was below 0.05. As one case experienced a very large number of events compared to all other cases in the study, analyses were performed both including and excluding that case from the analysis to assess sensitivity.
Results
Patient characteristics
Out of 141 patients screened, 63 met the criteria for inclusion (). Demographic data is presented in . Twenty-two percent (14/63) were males and 78% (49/63) were females. The mean age was 60.1 years for the whole study group, 59.3 for males and 60.4 for females. Age was calculated from the cross-sectional date 210302. Age at onset was defined as age at first visit at our clinic and was 51.1 years for the whole study group, 47.9 years for males and 52.0 years for females.
Sixty-three percent (40/63) were identified as non-smoking and 1.6% (1/63) declared status as active smoker. Smoking status could not be categorized for 23.5% (15/63) of the cases due to insufficient data in the medical records. For comorbidity by ACCI, the majority of cases had no or mild comorbidity (). Sixteen percent (10/63) had a systemic disease, defined as affecting the entire body, rather than a single organ or body part. Forty percent (4/10) of these 10 cases had granulomatosis with polyangiitis (GPA).
In total there were 159 surgical events and 63 patients investigated for the study. Thirteen (21%) patients were treated with both methods, 7 (11%) with only CO2 laser and 29 (46%) were selectively treated with balloon dilatation. Five (8%) were treated with rigid dilatations and 11 (17%) with submucosal resections, these cases are considered cold treatment options and were therefore included in the balloon dilatation methods group. Fourteen (22%) patients were not treated and therefore not included in the statistical analysis comparing balloon dilatation and CO2 laser procedures but included in the demographic data.
Main outcome
The mean SFI value for the different treatments were 599.53 days (standard error of mean 117.93) for laser and 530.15 days (std. error of mean 145.19) for balloon dilatation methods.
Statistics including all cases
When including all cases in the multivariate analysis, there was no association between SFI and surgical method (hazard ratio for balloon dilatation: 1.67, 95% CI: 0.82–3.43, p = .16) None of the other confounders had a statistically significant association to SFI.
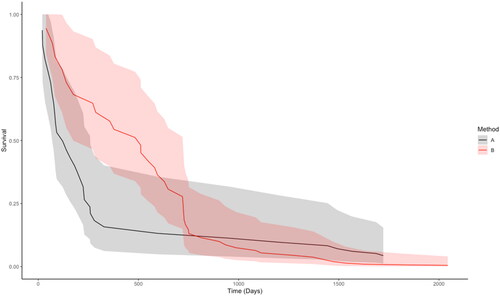
The surgical method variable did not pass the proportional hazards assumption test, indicating a violation of the assumption. The Cox PH regression was rerun using method as a stratification variable, and the resulting estimated survival functions are presented with approximate 95% confidence bands in . We see that balloon dilatation was associated with higher estimated survival up until approximately 700 days, after which balloon dilatation had lower estimated survival, though the confidence bands for the respective groups are overlapping throughout. In the stratified analysis, none of the other covariates had a statistically significant association with time to surgery.
Figure 2. Estimated survival functions with corresponding approximate 95% confidence bands for the respective surgical method, obtained from stratifying the Cox PH analysis on method. Including rigid dilatation and submucosal resections in the balloon dilatation group. Method B (balloon dilation) has a greater estimated survival up until approximately 700 days, after which method B (balloon dilatation) in fact has a lower estimated survival. However, the confidence bands for the respective methods are overlapping throughout. A = CO2 Laser treatment. B = Balloon dilatation.
Statistics excluding divergent case
One patient was treated 28 times during a very brief period of time which is considered an outlier, therefore the analysis was carried out a second time excluding this case as a clarification of deviant data.
In the Cox PH model, the association between time to surgery and surgical method was not statistically significant (HR for balloon dilatation: 0.91, 95% CI: 0.53–1.56, p = .72). The surgical method variable was stable and did not pass the proportional hazards assumption test. The Cox PH regression was rerun using method as a stratification variable, data not shown. Balloon dilatation had greater survival up until approximately 950 days, after which Balloon dilatation had a lower survival, though the confidence bands for the respective methods are overlapping during most of the assessment period, with an exception for the time period 300–500 days.
Statistics excluding rigid dilation and submucosal resection
To further investigate the reliability and purity of our group characteristics, we excluded the cold steel dilatations 5/63 (8%) and submucosal resections 11/63 (17%) leaving subjects only treated with balloon dilatation 29/63 (46%) to be compared with CO2 laser 7/63 (11%). This revealed very similar results as when we include rigid dilatation and submucosal resection. Association between time to surgery and surgical method was not statistically significant in this case either (HR for balloon dilatation: 1.21, 95% CI: 0.75–1.97, p = .43). As expected, the surgical method variable did not pass the proportional hazards assumption test, indicating a violation of the assumption. The Cox PH regression was rerun using method as a stratification variable, and the resulting estimated survival functions are presented with approximate 95% confidence bands in .
Figure 3. Estimated survival functions with corresponding approximate 95% confidence bands for the respective surgical method, obtained from stratifying the Cox PH analysis on method. In this analysis rigid dilatation and submucosal resection were excluded from the balloon dilatation group. Method B (balloon dilatation) has a greater survival up until approximately 700 days, after which balloon dilatation in fact has a lower survival. However, the confidence bands for the respective methods are overlapping throughout. Method A = CO2 laser treatment. Method B = balloon dilatation.
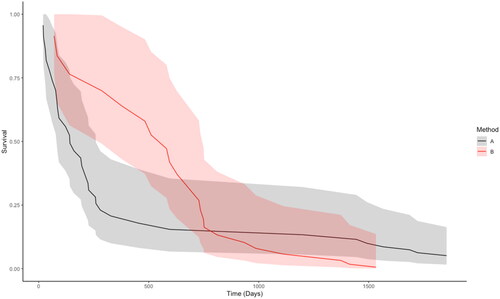
Among the other covariates in this analysis sex, smoking and ACCI group had a statistically significant association to time to surgery. Being female had a HR of 0.19 (95% CI: 0.07–0.54, p = .002) For smoking, not reporting smoking status had a HR of 3.80 (95% CI: 1.10–13.13, p = .035) compared to reporting no smoking, and belong to the ACCI group with mild symptoms had a HR of 0.16 (95% CI: 0.06–0.42, p = .0002) compared to no symptoms.
Discussion
Main findings
We performed a complete retrospective mapping of 141 cases for possible recruitment in the study, where when comparing the diagnostic codes with the medical records 63 met the criteria for SGS. We have studied a timeframe of 10 years for each surgical method, to reduce short-term effects on deviation in treatment outcome as illustrated in and .
We found no statistically significant difference in SFI nor patient characteristics comparing balloon dilatation and CO2 laser as different surgical treatment options, the inclusion/exclusion of rigid dilatation and submucosal resection in the balloon dilatation group did not affect the study outcome. Our findings confirm those from previous studies [Citation7,Citation14], and support the surgical freedom of choice based on the surgeon’s experience and skill. Secondary findings in our study also show that less comorbidity was associated with a significantly longer SFI regardless of the surgical method, indicating that the patient status before surgery is relevant for estimating the treatment effect.
Clinical impact of main findings
SGS can be perceived as asthma by both caregivers and caretakers, and this can contribute to treatment delay. When the diagnosis is confirmed, the airway diameter can be significantly reduced, which can mean a need for urgent surgery, using the optimal available methods. Although the incidence until now has been steady for some time at 4.9/1,000,000 [Citation3,Citation5] a local incidence increase has been reported [Citation4]. The SGS condition has an enormous impact on quality of life and significant health care costs [Citation6] due to repeated need of advanced surgery in relatively young cases, and with no definitive cure.
Treatment of choice
Although management of recurrent moderate and severe SGS often requires intricate surgical techniques, there is no widely accepted standard treatment algorithm. Most SGS cases that require repeated surgical procedures depend on well-coordinated airway teams applying the most optimal surgical setting. The current standard of care is surgical therapy with a goal to improve breathing and preservation of normal structures. The two treatment regimens compared in this study both are associated with high recurrence risk but comes with low risk of surgical complications, both have a relatively short learning curve for airway teams and are frequently used worldwide. Patients with more advanced airway stenosis, and a need of open surgery, acknowledged as having more durable symptom reduction, may also re-stenose. Choosing open surgery offers reported durable results but great perioperative risk and low-quality voice outcome [Citation9,Citation15]. Although surgical management remains the mainstay therapy for SGS, the requirement for adjuvant medical therapy has been highlighted. Gelbard et al. has reported longer SFI using endoscopic laser resection with adjuvant medical therapy [Citation7]. Furthermore, the use of adjuvant repeated intralesional corticosteroids under local anaesthesia has been outlined as successful in SGS treatment [Citation16].
Aetiology
The cause of SGS is unknown, though some known aetiologies include iatrogenic injuries and systemic inflammatory disease. A specific challenge for the diagnosis is the idiopathic phenotype. Recent studies have suggested possible inflammatory pathways including interleukin 17 A, and programmed death receptor (PD-1) and its ligand PD-L1 which can be involved in the scarring process of the subglottic space [Citation17,Citation18]. Despite these findings, there is still no mechanistic pathway which leads to the formation of localized scar tissue characterizing SGS cases.
Clinical significance
The outcome of this report, with no statistical differences in surgical free interval (SFI) between balloon-, and CO2 laser technique urges for mapping differences in patient reported outcome measures between these methods for accuracy in treatment.
This report composes an interesting complement to recently published data on the superior clinical outcome when using balloon dilatation as compared to CO2 laser in SGS treatment[Citation19]. The cause of the divergent outcomes is speculative but might be due to (i) diverse use of the CO2 laser (ii) difference in group size and composition, (iii) but most probably different follow up time frames. In accordance with Ntouniadakis E et al. we also report superior effect using balloon dilatation as compared to CO2 laser up until approximately 700 days. Since we addressed a time span of 10 years, we provide long-term data with no significant difference in surgical free intervals comparing balloon dilatation methods and CO2 laser technology as treatment options of SGS. Supporting the freedom of choice based on the surgeon’s experience and skill on a long-term schedule.
Limitations
One limitation in this study is possible selection bias related to how the surgical method is chosen for the cases in this analysis. During the first inclusion interval (1999–2009) patients were scheduled for surgery on a routine basis. This means that patients could have been treated with surgery both later or earlier than if surgery planning was based on self-reported subjective symptoms. In the second inclusion interval (2010–2021) symptom-relieving surgery was scheduled and performed when the subjective symptoms affected the patient’s functional level. It can be speculated that subjective symptoms could lead to either shorter or longer SFI than predetermined or objectively guided treatment intervals. It is possible that patients tolerated symptoms and waited for planned surgery, whereas others may have sought treatment earlier in their symptom course. Another aspect is that the balloon dilation approach is performed along with an adjuvant medical regime, which is not the case with CO2 laser approach. A small sample size can also increase the risk of a type 2 error. An additional drawback is the fusion of dilatation methods which will reduce the purity of the groups and increase risk of confounders, but it also increases sample size and statistical power of the study outcome. Extracting the cold steel dilation and submucosal resections from the balloon dilatation methods did not de-stabilize methods variable and did not pass the proportional hazards assumption.
Some patients were also treated with both methods and there is no data on how repeated treatments affects SFI, which could be an interesting question to address in the future.
This retrospective study was dependent on available patient variables and assessments, and so objective measurements which are desirable in current evaluation of the SGS, such as EDI (expiratory disproportional index) or dyspné index [Citation2], were not available.
We did not include cases before 1999, which is when digital medical records were introduced. Consistent with STARD, we would expect a systematic loss of data based on inaccessible paper medical records before 1999. These factors affected the difference in sample size for the 2 different surgical methods.
Conclusion
Our hypothesis was that CO2 laser surgery induces more scarring, due to thermal effect in the subglottic space, and therefore would result in a shorter SFI than the balloon technique. We found no difference in SFI when comparing balloon dilatation with CO2 laser treatment. This supports surgical freedom of choice based on the surgeon’s experience and skill. We conclude that the choice of endoscopic surgical method does not seem to affect the SFI on long term follow up.
Consent to participate
Patients gave their consent for tissue banking and research prior to diagnostic surgery at the department of otorhinolaryngology University hospital of Umeå.
Author contributions
All authors contributed to the study conception and design, as well as material preparation, data collection and analysis. The first draft of the manuscript was written by Anders Erlandsson and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Anders Lundqvist, for statistical discussions and aid and Michael Haney for professional language review and support.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available on request from the corresponding author.
Additional information
Funding
References
- Aravena C, Almeida FA, Mukhopadhyay S, et al. Idiopathic subglottic stenosis: a review. J Thorac Dis. 2020;12(3):1100–1111. doi: 10.21037/jtd.2019.11.43.
- Ntouniadakis E, Sundh J, Beckerath VM. Monitoring adult subglottic stenosis with spirometry and dyspnea index: a novel approach. Otolaryngol Head Neck Surg. 2021;167(3):517–523.
- Nunn AC, Nouraei SAR, George PJ, et al. Not always asthma: clinical and legal consequences of delayed diagnosis of laryngotracheal stenosis. Case Rep Otolaryngol. 2014;2014:1–5. doi: 10.1155/2014/325048.
- Chan RK, Ahrens B, MacEachern P, et al. Prevalence and incidence of idiopathic subglottic stenosis in Southern and Central Alberta: a retrospective cohort study. J Otolaryngol Head Neck Surg. 2021;50(1):64.
- Aarnæs MT, Sandvik L, Brøndbo K. Idiopathic subglottic stenosis: an epidemiological single-center study. Eur Arch Otorhinolaryngol. 2017;274(5):2225–2228. doi: 10.1007/s00405-017-4512-0.
- Yin LX, Padula WV, Gadkaree S, et al. Health care costs and cost-effectiveness in laryngotracheal stenosis. Otolaryngol Head Neck Surg. 2019;160(4):679–686. doi: 10.1177/0194599818815068.
- Gelbard A, Anderson C, Berry LD, et al. Comparative treatment outcomes for patients with idiopathic subglottic stenosis. JAMA Otolaryngol Head Neck Surg. 2020;146(1):20–29. doi: 10.1001/jamaoto.2019.3022.
- Feinstein AJ, Goel A, Raghavan G, et al. Endoscopic management of subglottic stenosis. JAMA Otolaryngol Head Neck Surg. 2017;143(5):500–505. doi: 10.1001/jamaoto.2016.4131.
- Hoffman MR, Patro A, Huang LC, et al. Impact of adjuvant medical therapies on surgical outcomes in idiopathic subglottic stenosis. Laryngoscope. 2021;131(12):E2880–E2886. doi: 10.1002/lary.29675.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8.
- Ekbom DC, Bayan SL, Goates AJ, et al. Endoscopic wedge excisions with CO2 laser for subglottic stenosis. Laryngoscope. 2020;131(4):E1062–E1066.
- Andersen PK, Gill RD. Cox’s regression model for counting processes: a large sample study. Ann Statist. 1982;10(4):1100–1120. doi: 10.1214/aos/1176345976.
- Kleinbaum DG, Klein M. Survival analysis: a Self-Learning text. 2nd ed. New York (NY): Springer New York; 2005.
- Lavrysen E, Hens G, Delaere P, et al. Endoscopic treatment of idiopathic subglottic stenosis: a systematic review. Front Surg. 2019;6:75. doi: 10.3389/fsurg.2019.00075.
- Axtell AL, Mathisen DJ. Idiopathic subglottic stenosis: techniques and results. Ann Cardiothorac Surg. 2018;7(2):299–305. doi: 10.21037/acs.2018.03.02.
- Hoffman MR, Francis DO, Mai JP, et al. Office-Based steroid injections for idiopathic subglottic stenosis: patient-Reported outcomes, effect on stenosis, and side effects. Ann Otol Rhinol Laryngol. 2020;129(4):361–368. doi: 10.1177/0003489419889066.
- Morrison RJ, Katsantonis N-G, Motz KM, et al. Pathologic fibroblasts in idiopathic subglottic stenosis amplify local inflammatory signals. Otolaryngol Head Neck Surg. 2019;160(1):107–115. doi: 10.1177/0194599818803584.
- Davis RJ, Lina I, Ding D, et al. Increased expression of PD‐1 and PD‐L1 in patients with laryngotracheal stenosis. Laryngoscope. 2021;131(5):967–974. doi: 10.1002/lary.28790.
- Ntouniadakis E, Sundh J, Magnuson A, et al. Balloon dilatation is superior to CO2 laser excision in the treatment of subglottic stenosis. Eur Arch Otorhinolaryngol. 2023;280(7):3303–3311. doi: 10.1007/s00405-023-07926-w.
