Abstract
Background
Early glottic cancer can be treated with laser resection or radiotherapy. In an earlier study, we found that voice function after laser resection was inferior to that after radiotherapy.
Objectives
This study was designed to determine if reduced margins at laser resection improved voice function without impairing oncologic results.
Method
A total of 268 patients with previously untreated T1–T2 glottic carcinoma were studied. They were primarily treated with either radiotherapy (n = 119) or laser resection (n = 149). Survival, need for additional treatment (radiotherapy and/or total layngectomi) and voice function was compared.
Result
Median follow up time was 7 years with range 0.5–16.6. There was no difference in the overall survival (p = .065) or disease-specific survival. (p = .126). After radiotherapy 32/119 patients and after laser resection 57/149 patients had recurrence. Total rate of laryngectomy was 24% in the radiotherapy group, and 8% in the laser resection group (p = .001). Voice analysis (T1A) showed more roughness in the radiotherapy group, otherwise no difference.
Conclusions
By reducing the surgical margins, we have achieved a better voice function (T1A) but more patients have needed repeated laser excisions and some have also needed supplementary radiotherapy. The risk of laryngectomy and survival were apparently not affected.
Chinese Abstract
背景
早期声门癌可以通过激光切除或放射疗法来治疗。 在以前的一项研究中, 我们发现激光切除后的发声功能比放射治疗后的要差。
目的
本研究旨在确定激光切除切缘的缩小是否可以改善声音功能而不损害肿瘤学结果。
方法
对 268 名既往未接受治疗的 T1-T2 声门癌患者进行了研究。 他们主要接受放射治疗 (n = 119) 或激光切除 (n = 149)。 比较了生存率, 即需要额外的治疗(放射治疗和/或全喉切除术)的需要和声音功能。
结果
中位随访时间为 7 年, 范围为 0.5-16.6。总体生存率 (p = .065) 或疾病特异性生存率(p = .126)没有什么区别。 放射治疗后119名患者中有 32名及激光切除后149例患者中有57名出现复发。 放疗组中喉切除总率为24%, 而激光切除组为 8% (p = .001)。 语音分析(T1A)显示放疗组更多的粗糙度, 其他方面无差异。
结论
通过减小手术切缘, 我们获得了更好的发声功能 (T1A), 但更多的患者需要重复激光切除, 有些还需要补充放射治疗。 喉切除术的风险和生存显然没有受到影响。
Introduction
When treating early glottic laryngeal cancer, we currently have two major treatment options that both provide good oncological and functional results, radiotherapy and endoscopic laser resection. Conventional conservation surgery as open partial horizontal laryngectomy is used very rarely in recent years. In this material, we did not have a single case and we therefore do not reason further about that option. There are a large number of retrospective studies describing radiotherapy or/and endoscopic laser resection but few prospective randomised studies [Citation1–4]. There are also a very large number of studies on laser surgery of laryngeal cancer, but where no comparison was made with radiotherapy; therefore, we do not refer to these for reasons of space (maximum 20 references).
In our study published in 1995, there was a great difference in voice quality between the groups, a major disadvantage for patients undergoing surgery with laser resection [Citation5]. Our original surgical technique was based on the work of Strong and Jako [Citation6]. The results of our own study and the minimally invasive technique presented by Steiner and coworkers led us to gradually expand the indications and reduce the surgical margins [Citation7]. This gave rise to the following questions:
Is it possible to reduce the margins in laser surgery
To improve voice quality?
Without increasing the risk of recurrence?
Without risking higher frequency of laryngectomy?
Without risking increased mortality in the disease?
In order to try to answer these four questions, we reviewed the journals of all 372 patients with glottic cancer diagnosed in the South Health Care region of Sweden, all of which were treated at our hospital.
Material and methods
Patients diagnosed with glottic cancer between January 1998 and March 2010 in South Health Care region of Sweden and treated at Skane University Hospital, Lund and Malmö, Sweden were studied. Patients with laryngeal carcinoma were identified through the hospital’s computer system. The hospital is third referral centre in the South healthcare region (population 2010 around: 1.7 million people). All incident cases in the region were previously untreated, reviewed by the ENT and Oncology department, and treated after discussion and decision at a multidisciplinary conference.
Overall, we identified 372 previously untreated patients. Of these, 99 patients were excluded (), leaving 273 patients with T1–T2 glottic carcinoma. In accordance with the decision of the Swedish Ethical Review Authority, patients received written information and the opportunity to waive participation through an opt-out procedure. Five patients did opt-out giving a final number of 268 patients participating.
Table 1. Patients excluded from the initial 372 patients identified with laryngeal cancer and the exclusion critera.
When the patient with suspected or biopsy-verified cancer was sent to the university hospital, the resectability of the tumour was assessed. At a multidisciplinary conference, the most appropriate treatment was discussed, and the patient was suggested either laser resection or radiotherapy, depending on which was considered preferable. The distribution into T stage and the primary treatment is shown in , gender and age in .
Table 2. Descriptive statistics of the 268 patients participating.
Table 3. The final 77 patients of 155 in the voice analysis group.
The European Laryngological Society classification of endoscopic cordectomies was not published at the start of this study and therefore could not be used. The majority of the resections in the latter part of the study have been Type II or Type III, occasional Type I and Type VI and very few Type V. Even if we were to classify the resections retrospectively, the number of patients would be too few for stratification according to ELS to give any valuable information.
In the period of the study published in 1995 [5] all patients who had positive or close margins in the specimen after laser resection where treated with radiotherapy, thus not included in the material. In this study, we had another protocol. The patients were followed with clinical office checks with laryngoscopy. If there were positive or close margins, the patients were followed with shorter intervals, but reoperations were only performed if there were clinical findings during the office laryngoscopy.
All patients in the RT group were treated with the same protocol, all at the Oncology department in Lund. They were given fractions of 2 Gy 5 d a week to at total of 64 Gy, the volume adjusted to T stage. None of them was submitted to concomitant chemotherapy.
To compare voice quality after respective laser surgery or radiotherapy, voice recordings were analysed from patients with glottic T1a. In the groups with T1b and T2 cancers, the number of patients in each sub-group was such that comparison was not meaningful. In addition, the inclusion criteria were that the patients would have been recorded 1–2 years after the end of treatment and they would not have been treated for a recurrence. Among the original 155 patients with T1a, 87 satisfied the inclusion criteria. Ten recordings could not be retrieved or were technically incomplete, why 77 recordings remained for analysis (). The recordings had been done in connection with return visits to the phoniatric department, approximately 24 months (between 12 and 36 months) after completion of primary treatment. During the recording, the patient was in a soundproof room, with a head-mounted microphone placed thirty centimetres from the mouth. The recordings were about 50 s long and consisted of running speech. The majority read the standard text ‘The Northern Wind and The Sun’, with the exception of three recordings where patients spoke freely about a subject. One of these recordings was in a language other than Swedish. Due to a change in technology in 2005, recordings were downloaded both from VoiceJournal and from mini-discs. The recordings found in VoiceJournal were converted in AudaCity (http://audacity.sourceforge.net/?lang=en 2013-03-05) with sampling frequency 16 kHz and channel mono. The recordings that were saved on the minidisk were transferred to a computer via SoundSwell, with a sampling frequency of 16 kHz and channel mono. All recordings were cut and deidentified using SoundSwell. For the assessment, the recordings were randomised to a list, with randomised order in terms of treatment, age and treatment date.
For the perceptual assessment of the vocal material, two groups of listeners were recruited: One assessment group was speech therapy students from Lund University. Five speech therapy students, all from the eighth semester of the program, participated in the study.
The second group consisted of naive listeners, i.e. individuals without formal training in voice assessment. To recruit this group five individuals from the authors’ circle of acquaintances were interviewed. Apart from the exclusion criterion that applied to knowledge and/or experience of voice assessment, no other demands were made on the naive listeners. All naive listeners were students at Lund University and/or Malmö University.
Hiranos’ GRBAS scale in an abbreviated version was used for the assessment. For speech therapy students, the parameters Grade (G), Roughness (R) and Breathiness (B) were used according to ELS definition [Citation8]. GRBAS ‘last two parameters, Asthenia (A) and Strain (S), were not used because previous studies have shown low validity in these. Each parameter was estimated according to a four-point scale from 0 to 3, where 0 stood for ‘normal’, 1 stood for ‘mild deviation’, 2 stood for ‘moderate deviation’ and 3 stood for ‘strong deviation’. The naive listeners rated the voices only according to the parameter grade (G).
The material consisted of 87 recordings, of which 10 were duplicated to check intra-rater reliability, a total of 77 unique recordings.
Individual patients were referred for voice treatment by a speech therapist and a few underwent surgical interventions to improve the voice. It was not included in our general treatment plan and the number of patients was so small that it did not affect the results.
Statistics
Statistical Package for the Social Sciences (SPSS) was used for calculation of the statistics.
Log Rank (Mantel-Cox) Chi-Square and Cox regression were used for assessment of survival.
For the voice assessments, a descriptive analysis was performed to calculate demographic data as well as median values and quartile deviations. When comparing the treatment groups, median values were used in analysis with Mann–Whitney U test, as the material was not normally distributed and thus not suitable for analysis with parametric analysis methods. To evaluate the inter-assessor reliability on the assessment parameters, all 77 voice recordings were used and the calculation was made with Cronbach’s Alpha. For reliability analysis with Cronbach’s Alpha, values above 0.7 are acceptable, but values above 0.8 are desirable. The intra-assessor reliability was calculated with Spearman’s rho to establish a relationship between each listener’s individual estimate for the duplicate voices the first and second time they were heard. This is because more values are required in the analysis for Cronbach’s Alpha to be suitable. For Spearman’s rho, the correlation coefficients were interpreted as weak correlations at 0.10–0.29, moderate at 0.3–0.49 and strong from 0.5 to 1.0. For all calculations, a significance level of 0.05 has been used, with the exception of the cases where SPSS found significance even at 0.01, which is then marked in the table.
Ethics
The study is approved by the Swedish Ethical Review Authority, Lund, Section 2, number 2014/130. Patients received written information and the opportunity to waive participation through an opt-out procedure.
Results
Distribution between T-classes is shown in . Since the distribution between the groups was not random but was based on the assessment of whether it was possible to laser excise or not, there was an expected different distribution of the T classes in the two treatment groups. There was a clear overrepresentation of the larger tumours in the radiotherapy group and the smaller tumours in the laser excision group.
Table 4. Distribution between T-classes.
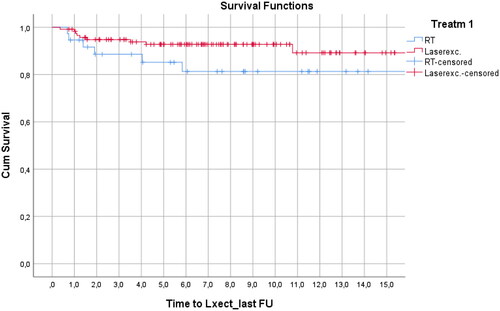
When closing of the study, status of the patients was as described in . Death in intercurrent disease, usually cardiovascular disease or second primary, was more common (46% RT and 40% LT) than death due to laryngeal cancer (12% RT and 7% LT). The overall survival for the RT group was 42%, with survival time 9 years mean 7.6–9.8, 95% confidence interval), and for the LT group 53%, with survival time 10 years mean (9.4–11.4, 95% confidence interval). With overall comparison gives, Log Rank (Mantel-Cox) Chi-square 4.026, df 1 a p value of .045. Overall survival as assessed by Cox regression showed statistically significant differences between age (p = .000) and T-class (p = .029) as expected but no difference between treatments (p = .065). Looking at the disease-specific survival, there was no statistically significant difference between the groups. RT: 88% survival, 14 years survival time (13.2–15.1, 95% confidence interval). LT: 93% survival, 15 years survival time (14.6–16.0, 95% confidence interval). That gives Log Rank (Mantel-Cox) Chi-square 2.239, df 1 a p value of .126. Disease-specific survival as tested for the different T-classes showed no statistically significant differences; Log-rank test: T1a, T1b and T2 give p = .872, .485 and .858, respectively. T1a was the single largest group (n: 155), 37 of these were treated with RT and 118 with laser excision. There was no difference neither in disease-free survival (p: .872) nor laryngectomy-free survival (p: .132) ().
Table 5. Status of the patients when closing the study.
Of 119 patients primary treated with RT 32 had recurrence. The treatment of the first recurrence was, LT (4 patients), laryngectomy (27) and chemotherapy (1). 57/149 patients with primary LT had recurrence. In these cases, the treatment of the first recurrence was, RT (26 patients), LT (29) and laryngectomy (2).
In case of repeated recurrences, laser resection was performed again if possible, but if this was not considered the best treatment, the patients in the group initially treated with laser resection received treatment of recurrence with radiotherapy. In addition to the 26 patients who received radiotherapy after the first recurrence, nine patients were treated, which gave a total of 35 patients (24%) in the original laser resection group who finally received radiotherapy. In the LT group 76% were cured with laser resection only.
Laryngectomy was performed as treatment after the first recurrence in 27 patients in the RT group and 2 patients in the LT group. After repeated recurrences, the total rate of laryngectomy was 28 patients (24%) in the RT group, and 12 patients (8%) in the LT group, which is a statistically significant difference (p = .001) but reasonably representing the difference of T1/T2 ratio in the groups.
Perceptual voice analysis
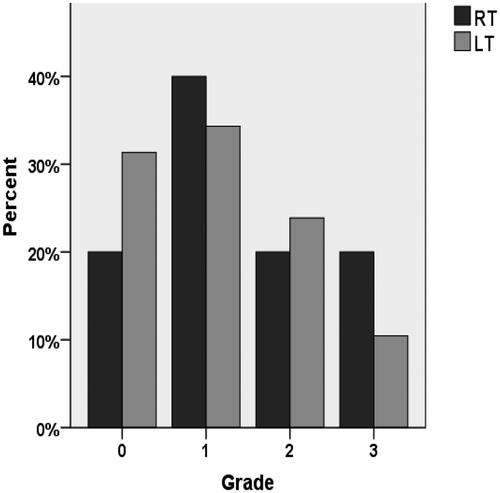
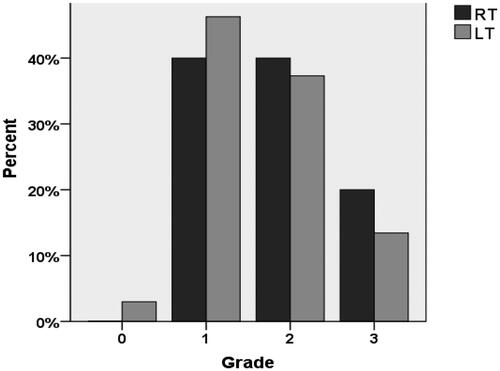
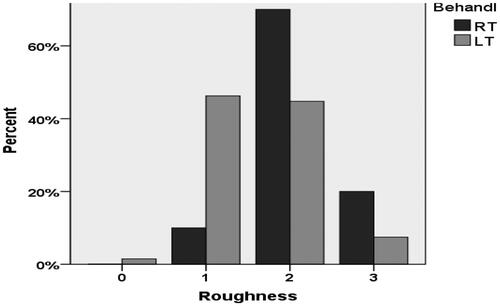
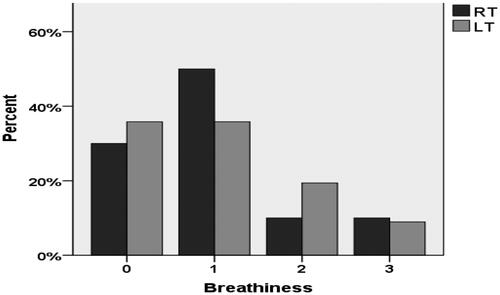
A comparative analysis of the listeners’ assessments for the Grade parameter in patients treated with RT or LT, respectively, is shown in . No statistically significant differences occurred, either in the naive listeners’ (z = −0.744, p = .339) or based on the speech therapy students’ assessments (z = −0.690, p > .05). Roughness showed a statistically significant difference between RT and LT groups, , p = .0014. The patients in the RT group had inferior voices compared to patients in the LT group. A very clear change, compared to our study in 1995 [5], is that the at that point very clear difference in breathiness that we noticed among patients after laser resection now is completely gone (p = .737) (.
Discussion
This study is not a comparison between two treatment options. It is a ‘test of proof’ of a treatment principle; Patients with a tumor judged possible to radically excise with laser excision was primarily offered this treatment option, others radiotherapy.
The strength of this study is that it is population based and all patients were treated at one, single institution. It is thus an unselected representative of treatment in a defined population area. The weakness is the comparatively long inclusion period, 13 years, during which there was a development of both diagnostic and radiotherapeutic techniques, which may have changed the choice between RT and LT.
It is important to once again point out that there is a bias in the selection of patients from the start. Smaller tumors are more often in the LT group, larger tumors in the RT group. With this in mind, we can answer the question: Is it possible to reduce the margins in laser surgery to improve voice quality? The answer is yes. The most obvious effect on voice quality after the original resection technique was a pronounced breathiness compared to patients treated with RT. We do not see this effect in this study since resection margins have decreased. This is in line with the reasoning that the voice gets worse the more tissue that is surgically removed and is supported in the literature [Citation9]. Increased roughness after RT can probably be explained by post-radiological edema or the negative effect on the elastic properties of the connective tissue in the vocal fold. For a good comparison between LT and RT you would need to accurately measure tumor extent and depth [Citation10].
But is it possible to reduce the margins in laser surgery without increasing the risk of recurrence? No, compared to our previous experience with resection with microscopically free margins, the risk of recurrence increases. In this study, 57/149 (38%) of patients with primary LT had a first recurrence. This is a high recurrence rate compared to other studies [Citation11–13]. In this study, 20/57 (35%) with recurrency after primary LT was further managed with additional LT. In the end, 75% of patients with T1a tumors were treated with laser only. Lindholm and Elner cured 91% of the patients with laser only, but they had wider resection margins and only 10–15% of the T1A tumors were operated primarily [Citation14]. Only, T1a tumors in the mid-portion of the vocal fold were resected in their study, and the surgical principles were the same as our previous study [Citation5]. If the margin to vocal process, sinus Morgagni, anterior commissure or inferior surface of the vocal fold was not clearly sufficient, the patient was referred to radiotherapy. It is likely that the majority of patients prefer a slightly worse voice in relation to the disadvantage of the high recurrence rates. It often appears during the clinical follow-up. The consequence of this is that since the results of the study became clear, we have slightly increased the surgical margin after preoperative discussion with the patient.
In this study, 24% of T1a tumors were primarily treated with radiotherapy and 76% laser resected, including those growing close to the limits of T1a. The expanded indications for LT combined with narrower margins may explain the increased risk of relapse. Sjögren et al. considered 51% of T1a lesions suitable for laser surgery [Citation15]. Lindholm and Elner also demanded free margins in the specimen, if not, radiotherapy was given. In this study, patients were followed up in the clinic and re-resection, biopsy and/or radiotherapy was performed depending on the clinical picture, and we found no difference in DFS or laryngectomy-free survival.
What about the overall risk of laryngectomy? The total rate of laryngectomy was 24% in the RT group, and 8% in the LT group which is a statistically significant difference (p = .001). Although we consider bias selection, it seems reasonable to assume that the risk of laryngectomy due to postponing any radiotherapy by primarily using laser excision does not appear to increase the risk of laryngectomy in the LT group. This is supported in the literature [Citation16–18] but other studies did not show any difference [Citation19,Citation20]. The T1b and T2 groups were to small for a meaningful analysis of laryngectomy-free survival, but considering the difference in LT/RT ratio between the groups, the difference we found in the entire study population is likely to be found in the more advanced T-stages.
Is it possible to reduce the margins in laser surgery without risking increased mortality in the disease? When we compared the overall survival for the RT group vs. the LT group Log Rank (Mantel-Cox) Chi-Square gave a p = .045, whereas survival as assessed by Cox regression did not show any statistically significant differences between the treatments (p = .065). There was no statistically significant difference between the groups calculated as disease-specific survival (RT: 88%, LT: 93% survival). We can probably assume that LT with reduced margin to healthy tissue does not affect mortality.
Conclusion
At our clinic, we started treating early glottic cancer with laser resection on the condition that there were well-demarcated tumors with a good possibility of excision with a margin. The results regarding tumor control were good, but voice function was greatly impaired compared to patients who were treated with radiotherapy.
By reducing the surgical margins, we have achieved a better voice function in our patients but at the expense of the local control. More patients have needed repeated laser excisions and some have also needed supplementary radiotherapy. The risk of laryngectomy and survival do not seem to have been affected by the fact that we primarily treated with laser excitation.
Acknowledgements
The authors offer sincere thanks to Professor Johan Wennerberg for valuable help with the processing of the material.
Disclosure statement
We have no conflict of interest.
References
- Aaltonen LM, Rautiainen N, Sellman J, et al. Voice quality after treatment of early vocal cord cancer: a randomized trial comparing laser surgery with radiation therapy. Int J Radiat Oncol Biol Phys. 2014;90(2):255–260. doi: 10.1016/j.ijrobp.2014.06.032.
- Abdurehim Y, Hua Z, Yasin Y, et al. Transoral laser surgery versus radiotherapy: systematic review and meta-analysis for treatment options of T1a glottic cancer. Head Neck. 2012;34(1):23–33. doi: 10.1002/hed.21686.
- De Santis RJ, Poon I. Comparison of survival between radiation therapy and trans-oral laser microsurgery for early glottic cancer patients; a retrospective cohort study. J Otolaryngol - Head Neck Surg. 2016;45:42.
- Warner L, Chudasama J, Kelly CG, et al. Radiotherapy versus open surgery versus endolaryngeal surgery (with or without laser) for early laryngeal squamous cell cancer. Cochrane Database Syst Rev. 2014;2014(12):CD002027.
- Rydell R, Schalén L, Fex S, et al. Voice evaluation before and after laser excision vs. radiotherapy of T1A glottic carcinoma. Acta Otolaryngol. 1995;115(4):560–565. doi: 10.3109/00016489509139367.
- Strong MS, Jako GJ. Laser surgery in the larynx. Early clinical experience with continuous CO2 laser. Ann Otol Rhinol Laryngol. 1972;81(6):791–798. doi: 10.1177/000348947208100606.
- Steiner W. Results of curative laser microsurgery of laryngeal carcinomas. Am J Otolaryngol. 1993;14(2):116–121. doi: 10.1016/0196-0709(93)90050-h.
- Dejonckere PH, Bradley P, Clemente P, et al. A basic protocol for functional assessment of voice pathology, especially for investigating the efficacy of (phonosurgical) treatments and evaluating new assessment techniques. Guideline elaborated by the committee on phoniatrics of the European Laryngological Society (ELS). Eur Arch Otorhinolaryngol. 2001;258:77–82.
- Tomifuji M, Araki K, Niwa K, et al. Comparison of voice quality after laser cordectomy with that after radiotherapy or chemoradiotherapy for early glottic carcinoma. ORL J Otorhinolaryngol Relat Spec. 2013;75(1):18–26. doi: 10.1159/000346934.
- van Loon Y, Sjögren EV, Langeveld TPM, et al. Functional outcomes after radiotherapy or laser surgery in early glottic carcinoma: a systematic review. Head Neck. 2012;34(8):1179–1189. doi: 10.1002/hed.21783.
- Brøndbo K, Benninger MS. Laser resection of T1a glottic carcinomas: results and postoperative voice quality. Acta Otolaryngol. 2004;124(8):976–979. doi: 10.1080/00016480410017413.
- Canis M, Ihler F, Martin A, et al. Transoral laser microsurgery for T1a glottic cancer: review of 404 cases. Head Neck. 2015;37(6):889–895. doi: 10.1002/hed.23688.
- del Mundo DAA, Morimoto K, Masuda K, et al. Oncologic and functional outcomes of transoral CO2 laser cordectomy for early glottic cancer. Auris Nasus Larynx. 2020;47(2):276–281. doi: 10.1016/j.anl.2019.08.005.
- Lindholm CE, Elner A. Transoral laser surgery of laryngeal carcinomas. State of the art in Sweden. Adv Otorhinolaryngol. 1995;49:250–253. doi: 10.1159/000424384.
- Sjögren EV, Langeveld TPM, Baatenburg de Jong RJ. Clinical outcome of T1 glottic carcinoma since the introduction of endoscopic CO2 laser surgery as treatment option. Head Neck. 2008;30(9):1167–1174. doi: 10.1002/hed.20852.
- Ding Y, Wang B. Efficacy of laser surgery versus radiotherapy for treatment of glottic carcinoma: a systematic review and meta-analysis. Lasers Med Sci. 2019;34(5):847–854. doi: 10.1007/s10103-018-2695-2.
- Guimarães AV, Dedivitis RA, Matos LL, et al. Comparison between transoral laser surgery and radiotherapy in the treatment of early glottic cancer: a systematic review and meta-analysis. Sci Rep. 2018;8(1):11900. doi: 10.1038/s41598-018-30218-x.
- Vaculik MF, MacKay CA, Taylor SM, et al. Systematic review and meta-analysis of T1 glottic cancer outcomes comparing CO2 transoral laser microsurgery and radiotherapy. J Otolaryngol - Head Neck Surg. 2019;48:44.
- Elicin O, Giger R. Comparison of current surgical and non-surgical treatment strategies for early and locally advanced stage glottic laryngeal cancer and their outcome. Cancers (Basel). 2020;12(3):732. doi: 10.3390/cancers12030732.
- Feng Y, Wang B, Wen S. Laser surgery versus radiotherapy for T1-T2N0 glottic cancer: a meta-analysis. ORL J Otorhinolaryngol Relat Spec. 2011;73(6):336–342. doi: 10.1159/000327097.