ABSTRACT
Objective: Family violence causes brain injury and trauma for many victim survivors. Neuropsychologists play a central role in helping with these issues. We aimed to evaluate rates of family violence training, knowledge and clinical skills in Australian neuropsychologists.
Method: An online, brief, self-report survey of psychologists practicing clinically in the area of neuropsychology Australia wide. The survey assessed prior training, knowledge and confidence together with awareness of specific family violence clinical skills, and barriers to competent practice.
Results: Responses were received from every state and territory and represented more than 10% of the total registered endorsed clinical neuropsychology workforce (N = 92). Over 90% of respondents had undertaken family violence training, however 57% reported having little or no knowledge and 67% little or no confidence working clinically in the area. Knowledge of specific family violence skills was reduced, with only 20% indicating that they knew how to respond, when clients disclosed experiencing family violence.
Conclusions: Further work is needed to improve the ability of the Australian neuropsychology workforce to respond to this important health issue. Response of neuropsychologists may be sub-optimal, particularly in regard to the provision of psychological support following disclosures a central tenant of World Health Organization guidelines.
KEY POINTS
What is already known about this topic:
Family violence is a significant public health issue in Australia.
Family violence can cause both brain injuries and psychological trauma and attenuated cognitive functioning has been associated with both of these conditions.
Clinical neuropsychologists commonly work with clients who experience cognitive attenuation.
What this paper adds:
This paper is the first, to our knowledge, to survey training, knowledge, confidence levels and specific family violence clinical skills in Australian neuropsychologists.
Over 10% of the endorsed clinical neuropsychology Australian workforce participated in this self-report online survey.
Results indicated that most had received some family violence training, however, self-rated knowledge, confidence and awareness of specific family violence skills were relatively low and further training and professional development in this area is required.
Introduction
Family violence is a significant public health problem, particularly in Australia. As defined by the Victorian Family Violence Protection Act (Citation2008) family violence includes physical, sexual, emotional, psychological or economically abusive behaviour towards a family member. It also includes behaviour that is threatening, coercive, or in any other way controls or dominates a family member that causes them to feel fear for their safety and well-being (Family Violence Protection Act, Citation2008, Citation2008). Family violence occurs across the lifespan and can be perpetrated against a person of any gender or sexual orientation, but is most commonly directed at women and children (Crime Statistics Victoria, Citation2017; Office for National +Statistics, Citation2017). In Australia, one-quarter of women have experienced physical or sexual violence perpetrated by an intimate partner, with the same proportion also experiencing emotional abuse (Australian Bureau of Statistics, Citation2012; Cox, Citation2016). One in four children in Australia has been exposed to family violence, with more than half of the women who experience violence having children in their care (Campo, Citation2015; Cox, Citation2016; Office for National Statistics, Citation2017). The health and economic costs of family violence are very high. Family violence contributes more strongly to death, disability and illness in women in the 15 to 44-year-old age group than any other preventable risk factor (VicHealth, Citation2004). The total combined health, administration and social welfare costs of violence against women have been estimated to be 21.7 USD billion a year (PricewaterhouseCoopers, Citation2015).
The World Health Organisation (WHO) has established clinical and policy guidelines for responding to family violence (World Health Organization [WHO], Citation2013, Citation2014). From an Australian context, the Multi-Agency Risk Assessment and Management Framework (MARAM) further outlines minimum clinical competencies to establish a system-wide shared understanding of family violence (Victorian Government, Citation2020). Accordingly, best practice recommendations indicate that clinicians should be aware of clinical indicators of family violence and inquire about violence when assessing clinical conditions associated with violence (including but not limited to trauma-related injury, alcohol and other substance abuse). Moreover, health care workers should, as a minimum, offer first-line support for any woman disclosing violence through sensitive inquiry. In this regard, the WHO propose a multidimensional approach to management, using the acronym LIVES which advises that clinicians: Listen to and believe victim survivors, Inquire about their needs and concerns, Validate their experience, Enhance safety, and offer ongoing Support (WHO, Citation2014). Guidelines further highlight the role of clinician training, competence and confidence in managing family violence (Victorian Government, Citation2020; WHO, Citation2013), with clear implications for the likelihood of ongoing engagement and disclosure in victim-survivors (Trevillion et al., Citation2012).
There is a link between family violence and brain injury, although the accuracy and generalisability of incidence and prevalence statistics have been difficult to elucidate (Ayton et al., Citation2021). Australian data indicate that in women hospitalised due to partner or spousal assault, two-thirds experienced head and neck injuries, with 7% resulting in brain injuries (Australian Institute of Health and Welfare, Citation2019). For women hospitalised as a result of assault-related brain injury in 2016-17, the perpetrator of the assault was their spouse or domestic partner in 47% of cases (compared to 2% of cases for men) (Australian Institute of Health and Welfare, Citation2019). A Victorian hospital data audit of family violence-related injuries, between 2006 and 2016, indicated that family violence was a common cause of brain injury (Gabbe et al., Citation2018). Of the family violence victim survivors attending Victorian hospitals during the 10-year audit period, 40% (6,409 out of 16,296) had sustained a brain injury, including 25% of child victim survivors (1,252 out of 5,007). Brain injury accounted for 82% of the family violence-related deaths. A bidirectional relationship between brain injury and family violence has recently been established by Pritchard and colleagues (Pritchard et al., Citation2019). According to this model (termed the “nexus model”) the presence of family violence makes the likelihood of brain injury more common, and vice-versa. The model also highlighted cultural, psychological (mental health, posttraumatic stress, alcohol and drug use), biological and relationship factors, exposure and life stressors that increased the likelihood of both family violence and brain injury. This model serves to not only to highlight the shared relationship between brain injury and family violence but also provides a useful framework to evaluate their co-occurrence.
Family violence can result in brain injuries and brain injuries can cause cognitive impairment (Draper & Ponsford, Citation2008; Kinnunen et al., Citation2010). Furthermore, family violence causes psychological trauma which can also attenuate cognition (Brandes et al., Citation2002; Twamley et al., Citation2009). Thus, it is easy to see why family violence is a health epidemic with implications for neuropsychological practice. Given the high prevalence of family violence in the Australian population, and the proportion of their clients with brain injuries, it is likely that clinical neuropsychologists will regularly encounter clients who either have, or are, experiencing or perpetrating family violence. As such, the cognitive impact of family violence, as a result of both acquired brain injuries and high levels of psychological trauma, is an important clinical consideration, as is the capacity of neuropsychologists to respond appropriately and provide support to clients who disclose experiencing or perpetrating violence. Despite this clearly delineated need, the level of skill, confidence and training in family violence among Australian practicing neuropsychologists is unknown. The current national survey sought to answer this question by cross-sectionally examining clinician confidence, skills, training and barriers in the assessment and management of family violence.
Method
Ethics approval was obtained for this study from Melbourne Health Human Research Ethics Committee (HREC/17/MH/283). Participants were sought for the survey who were Australian Health Practitioner Regulation Agency (AHPRA) registered psychologists working in a clinical neuropsychology, patient-facing role. This included:
psychologists with clinical neuropsychology endorsement
psychologists with a degree in clinical neuropsychology who were undertaking registrar training for clinical neuropsychology endorsement
psychologists with a degree in clinical neuropsychology who were working clinically in a neuropsychological capacity, yet to undertake registrar training for endorsement
Participants for the Survey were sought via the NPinOz Google Group. This is an email list server for people interested in clinical neuropsychology in Australia. It is privately administered with 1113 members (as of 17.12.2019), although membership is open to all via application on the Google Groups platform.
The survey instrument was a short, targeted online survey collecting demographic and professional role information, in addition to knowledge, confidence and practices working clinically in the area of family violence. These areas were chosen to reflect best practice guidelines as outlined by the WHO (Citation2014) and MARAM framework (Victorian Government, Citation2020). This survey has previously been used in two settings, a large metropolitan tertiary teaching hospital (534 clinician respondents) and a child and family health service (35 staff respondents) (Fisher, Rudkin, et al., Citation2020; Withiel et al., Citation2020; Withiel, Gill, & Fisher, Citationin press). This measurement tool demonstrated high internal reliability in this study (Cronbach’s alpha = .805), with comprehensive psychometric evaluation to follow by this research team in the near future. The survey content is included throughout the results section, below.
The survey link was emailed to the NPinOz membership list, with information explaining the study, including the voluntary nature of participation and anonymous nature of the responses. Information was also provided about both state specific and national services participants could contact if they were distressed as a result of participation. The data were collected over 6 weeks (October–November 2019), and two reminder emails were sent to the list over this time.
Descriptive statistics were calculated for all nominal and Likert type response questions. Free text responses were analysed using qualitative content analysis (Graneheim & Lundman, Citation2004), with categories developed inductively. For each free text question, all answers were extracted and compiled into one text. The text was initially read for familiarity with the content and meaning units (words/phrases) were identified. Through reading the text, categories were developed to label meaning units, then themes were identified to describe the underlying content of the categories for each question. The categories and themes for each question were discussed and agreed upon by two researchers to enhance the reliability of the analyses. The utilised categories were those derived from groups of content that shared a commonality, including the manifest content of the text expressed to a descriptive level of the content. Themes, which could occur across categories, represented an underlying thread of meaning, encompassing the latent context of the text (Graneheim & Lundman, Citation2004).
Results
Demographics
Responses were received from a total of 92 eligible and consenting psychologists practicing clinically in the area of neuropsychology. Specifically, this included 74 Endorsed Clinical Neuropsychologists (80.43%), 16 Clinical Neuropsychology Registrars (17.93%) and two Generally Registered Psychologists working clinically in a neuropsychological capacity (2.17%). The response rate is unclear, as not all members of the NPinOz Google Group are practising Australian neuropsychologists. However, the response rate represents 10.54% of all Endorsed Clinical Neuropsychologists in Australia (N = 702) at the time the survey was administered (Psychology Board of Australia, Citation2019).
Responses were received from every state and territory in Australia. shows the responses by state, relative to the national state-by-state proportion of the endorsed clinical neuropsychology workforce. The highest proportion of respondents came from Victoria, and the lowest from the Northern Territory. Queensland was moderately underrepresented in the survey, relative to workforce size, and New South Wales mildly underrepresented, while South Australia was moderately overrepresented, and Victoria mildly overrepresented. The response rates of all of the remaining states roughly paralleled their national proportional percentage.
Table 1. Survey responses by state
Demographically the sample comprised of 90.22% female and 9.78% male respondents, with no respondents endorsing a non-binary/gender fluid or different gender identity. The majority of the sample (63.04%) had completed their neuropsychology training in Victoria and nearly quarter in New South Wales (22.85%) with small proportions in other states or countries (ACT = 1.09%; QLD = 1.09%; SA = 3.26%; WA = 6.52%; Other or Overseas = 2.17%). A clinical doctorate was the most common highest qualification in clinical neuropsychology (45.65%), followed by a master’s degree (38.04%), clinical PhD (11.96%) and masters combined (4.35%). Just over half of the sample had 10 years or more experience in the profession (51.09%), a further 16.30% had six to 10 years, 29.35% one to 5 years and 3.26% and less than 1 year.
Respondents were asked to nominate the client groups they work with, and were able to nominate more than one area. A wide range of clinical areas were endorsed (see ). The most common clinical area was traumatic brain injury, followed by rehabilitation and neurology. In the “Other” category (9.78%) medico-legal, forensic mental health, general adult private practice, drug and alcohol and adult Down Syndrome services were nominated.
Table 2. Respondents’ areas of clinical practice
Training exposure, knowledge and confidences ratings
The far majority of respondents indicated that they had received some family violence training (91.31% n = 84), with 58.70% having received training in the last two years. The most frequent type of training was self-taught, followed by in-service sessions at the respondents’ hospital or clinic (see ). While “self-taught” was not further defined in the survey, leaving this to the interpretation of the respondents, it was anticipated by the researchers that this would encompass ad-hoc, self-guided and unstructured learning that an individual may undertake. More than three-quarters of respondents reported that they did not receive any family violence education as part of their professional training. Respondents’ hours of training were summed (taking the medium number in each training bracket, e.g., 2 hours for the 1-3 hours bracket, other than 16+ responses, which were taken as 16 hours), to provide some idea of overall training exposure. Respondents’ training hours ranged from 0 to 42.5 hours, with the mean number of training hours 7.84 hours (SD = 8.82).
Table 3. Percentage of respondents’ hours of family violence training by location/provider
More than half of the respondents rated themselves as having little or no knowledge of working clinically in the area of family violence (see ). More than two-thirds rated themselves as having little or no confidence working in the area. One in six respondents indicated that they often or always screened clients for family violence, although 45% indicated that they never or rarely screened clients. Ninety-three percent of respondents indicated that they work with clients who have disclosed family violence experiences at least some of the time.
Table 4. Respondents self-ratings of knowledge, confidence and experience in family violence
Specific family violence clinical skills
Respondents were asked to provide information about their knowledge of specific family violence clinical skills. To the question, Do you believe you know how to appropriately ask patients/clients about family violence?, just under one-quarter of the sample responded Yes (22.83%), half of the sample responded Somewhat (50.00%) and the remainder responded No (27.17%). Those responding Yes or Somewhat were asked to provide details about the process of asking the clients, and 49 responses were received. Five categories were developed for the text data responses that were encompassed by two broader themes.
The first theme was How. This related to how the question was asked including the decision-making of the clinician regarding professional judgement about asking the question (n = 11) and specific processes that the clinician followed when asking (n = 43). Examples include:
It depends on the client and the context. I would routinely ask in the context of gathering information regarding relationship status, also when getting family history …
Sensitively inquire, ensure question is asked in an appropriate area away from perpetrator …
Checking in with family members about violence toward family in context of assessment of behaviours of concern …
Within NSW Health there is a standard DV screening tool we use.
The second theme was What. Responses consistent with this theme related to specifically what was asked of clients during an enquiry. This included framing the question in relation to safety, or asking about safety directly (n = 33), using a patient-initiated strategy, where the clinician builds on information the client has already provided to ask further questions or asking if the client is comfortable to talk/answer questions about the topic (n = 4), and asking the client if they are aware of support (n = 3). Text categorised as Process commonly fit under both themes and described processes the clinician followed whilst enquiring. Examples include:
Ask questions about whether they feel safe, whether there have been times when they were worried about their safety …
I preface questions with concern that people may be harmed in the family and ask direct questions.
… check they are aware of resources or how to seek help if they feel the need (usually GP as a minimum).
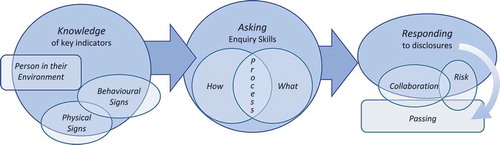
For the question, Do believe you are aware of the key indicators of family violence that may indicate a patient/client is at risk?, just one in six respondents endorsed Yes (16.30%). Half of the respondents endorsed Somewhat (48.91%), while a third responded No (34.78%). Further text information was provided by 44 respondents. Four categories were identified in the responses, encompassed by three themes, see . The first theme was the Person in their Environment, and included any psychological, social, economic or cultural factors that may make family violence more likely for a particular individual (n = 27). Examples include:
… if going through or recently have separated - during pregnancy or soon post birth of a child.
… non English speaking background with limited community.
Substance misuse, symptoms of trauma, mental health issues.
The second theme was Physical Signs. This included any indications suggestive of physical injury or medical illness (n = 22). Examples include:
Physical signs (bruising, repeated injuries or presentations) …
… physical injuries with unusual explanations …
The third theme was Behaviour. This included client behaviour that was verbal or non-verbal and directly observed by staff (n = 24). It also included the observed dynamic between clients and their family member(s) (n = 15). Examples include:
… if family member presents and insists on speaking on other person’s behalf.
… psychological manipulation and violence including restricting finances, restricted social support, verbal aggression from family members, threats of suicide from family members.
To the question, Do you have knowledge of what to do if/when a patient/client discloses family violence?, one-fifth of the sample answered Yes (19.57%), one fifth answered No (19.57%), while the remainder answered Somewhat (60.87%). Respondents answering Yes or Somewhat were asked to provide details about what they would do. A total of 62 responses were received in this section. Six categories were developed for this response set, grouping into three main themes, see .
The first theme was Collaboration, which included the response categories of Patient Led and Support. Responses falling under this theme included those that described the clinician providing support to the client and/or providing education about what supports are available (n = 33), as well as responses that took the patient’s direction or ideas into account (n = 21). Examples included:
… offer validation and supportive communication …
… discuss linking in with hospital/community based supports with client.
… the response depends on what the patient wants (and is capable of doing/deciding) …
The second theme was Passing. This included responses that involved passing information through the health service in the form of a referral to, or seeking assistance from, another discipline or supervisor (n = 23), the passing of information via referral to an external service (n = 35), and the passing of information via the documentation of the disclosure in the patient’s file/record (n = 3). Examples included:
Report to supervisor and clinical lead
Refer to Social Work …
Refer to specialist service
Document in neuropsychology file notes.
The third theme was Risk. This included responses that described assessing for family violence frequency, type and severity (n = 27) and those attempting to ascertain existing/available safety options (n = 23). Examples included:
Assess history of past abuse. Check if there is family support and a safe place to stay away from home.
Risk assessment if disclosed harm to others.
The text responses for all questions relating to specific family violence clinical skills, where constructed into diagrammatic representation, provided in . This figure summarises the main themes and categories from the provided responses, and highlights family violence as a complex and nuanced issue that requires a specific clinical skill set, for best practice responses (WHO, Citation2014).
Respondents were also asked to indicate factors that may act as challenges for them in addressing family violence, see . The most commonly endorsed challenge was the clinician’s perception that clients will be reluctant to disclose family violence issues when asked. This was followed by time limitations and the suspected perpetrator being present. Concerns about privacy issues in the clinical area, as well as concerns about staff safety when asking the question were the least commonly endorsed barriers from the provided options in the survey. In the Other category barriers included lack of knowledge of policies and procedures, difficulties working safely in this area in private practice, family violence already being well-documented, cultural barriers, not wanting to trigger distress in the client when a neuropsychology assessment needs to be conducted, lack of peer support, and clinician’s lived experience of family violence resulting in concerns that working in this area clinically would be triggering for them.
Table 5. Challenges addressing family violence endorsed by respondents
Discussion
This study sought to explore clinical confidence, skills, knowledge and barriers to assessment and management among psychologists practicing clinically in the area of neuropsychology in Australia. The results indicate that self-reported knowledge and confidence levels working in the area of family violence are relatively low. These results were obtained despite almost all respondents having received some level of family violence training and almost 60% having received training in the last two years. There was a large degree of variation in the type and duration of family violence training that had been undertaken, although the majority of respondents reported that they had not received family violence teaching as part of their professional training course. The majority of respondents were currently practicing in Victoria and the majority had also trained in Victoria. This reflects both the distribution of neuropsychologists nationally, as Victoria has the highest number of endorsed clinical neuropsychologists registered in Australia, as well as the distribution of accredited post-graduate training courses, with Victoria hosting three out of the six accredited clinical neuropsychology training courses currently operating within the country. Findings indicate that clinical training in managing client disclosures is generally not occurring in a formal capacity as a component of current post-graduate training, and consequently falls short of World Health Organisation (WHO) guidelines, which emphasise the need for training at pre-qualification level in first-line support for victim survivors (WHO, Citation2013). Given the clear role of neuropsychology in family violence, there remains an important need for integration of appropriate training into clinical training programs. Moreover, there is an urgent need for continuing professional development and peer supervision to help address low levels of clinician confidence when working in this area.
Only one in six respondents definitively endorsed that they were aware of key indicators of family violence, although a further 50% indicated that they had some knowledge in this area. Close to 30% of the total sample reported psychological, social, cultural or economic factors that may make family violence more likely. Close to a quarter listed physical signs that violence may be present, while behavioural and family dynamic indicators were also commonly listed. The vast majority of responses provided regarding key indicators aligned with what had been identified in the research as factors that are more likely to be present in situations where family violence is occurring (Australian Institute of Health and Welfare, Citation2019; Pritchard et al., Citation2019). Thus, when clinicians report knowledge about key indicators they are largely evidence based, if incomplete.
Despite showing a reasonable understanding of clinical indicators of risk, respondents’ actual clinical skills to ask about family violence were low. Fewer than a quarter of respondents responded definitively that they knew how to ask clients about family violence experiences, although a further half of the sample indicated that they had some knowledge about this. These findings are particularly concerning as research indicates victim survivors believe that partner abuse should be raised in an encounter with a healthcare professional and that enquiry should be repeated, to allow victim survivors time and space to disclose (Feder, Hutson, Ramsay, & Taket, Citation2006). Most of the clinicians who endorsed having at least some knowledge reported a specific process they followed when enquiring about family violence, including following their health service’s screening protocols, using the method of sensitive enquiry, and including enquiry as part of their routine information gathering/history taking. This indicates that for a number of clinicians family violence enquiry is a relatively routine part of their practice, although may occur only when clinical judgement indicates that it is necessary. When enquiry does occur, the primary theme of the questions asked by most clinicians was around safety.
Of concern, less than one-fifth of respondents indicated definitively that they were aware of how to respond to a disclosure of family violence. Disclosures of family violence experiences can occur at any point during a clinical interaction, and not just in situations where a direct enquiry has been made by the clinician. The response of the clinician when a disclosure occurs is known to be a critical factor for determining how comfortable victim survivors will feel to speak about their experiences in the future (Trevillion et al., Citation2012). Victim survivors have indicated their preferences are for responses that are individually tailored, not judgemental or directive, and show an appreciation of the complexity of family violence (Feder, Citation2006). This is also supported by the WHO LIVES guidelines, described above (WHO, Citation2014). Similarly, avoiding collusion when disclosures of perpetrating family violence are received is also important (Hegarty et al., Citation2008; Newman & Iwi, Citation2015). Based on the responses provided from clinicians about what they do when a disclosure is received, just a third of the total sample indicated that their response would provide support to the client, and fewer than a quarter reported that their response would be client led. A similar proportion of respondents indicated that they would investigate either safety or risk in response to a disclosure. Thus, based on the provided data, current responses to family violence disclosures by psychologists practicing clinically in the area of neuropsychology in Australia may be falling short of both patient expectations and best-practice guideline recommendations.
The data obtained in this study about barriers to working effectively in the area of family violence generally parallel those obtained in a previous study in large tertiary metropolitan hospital with a multi-disciplinary cohort (Fisher, Rudkin et al., Citation2020). The three most frequently endorsed challenges from the option list were the same across both studies. The perception of health professionals that victim survivors will be reluctant to disclose when asked is interesting and does not appear to be fully confirmed by the research. Recent research indicated that a quarter of health service users had disclosed family violence concerns to staff at the health service, while one-fifth had wanted to disclose concerns but did not feel comfortable to do so (Fisher, Galbraith et al., Citation2020). Of those who had not disclosed, three-quarters had not been screened for family violence at any point during their time at the health service. Thus, the majority of clients who had not disclosed family violence concerns, but had wanted to, had not been asked about family violence as part of their care. Earlier research also indicates that women provide higher ratings of the acceptability of family violence screening compared to clinicians, that victim survivors are more likely to disclose when directly asked, and that blaming attitudes from others and fear of not being believed by the clinician are barriers for disclosures (Bacchus et al., Citation2003; Feder et al., Citation2009; Rose et al., Citation2011). Thus, enquiries about family violence that are conducted by clinicians in a sensitive but direct manner, and are accompanied by a supportive response, are both desired by victim survivors and often lead to disclosures.
Another important consideration raised by the responses to the survey was that clinicians’ own lived experience of family violence may be a barrier to them seeking further training, or exposure to working in this area with clients. Given high prevalence of family violence in Australia, it is probable that a proportion of clinicians have experienced family violence personally (McLindon et al., Citation2018). Importantly, however, there is likely to be variation in the way clinician victim survivors approach this issue. Research by McLindon et al. (Citation2019) indicated that clinician victim survivors report a greater preparedness to assist patients experiencing family violence in a manner consistent with ideal clinical care. This lead study authors to suggest that personal family violence experiences are not necessarily a barrier to the provision of clinical care to patients. As such, sensitivity and consideration should be given to these issues when family violence training is offered, participation should always be optional, and attendees should be informed that they are welcome to leave straining sessions if they become distressed.
There are several limitations of this study, one is the sample size. The sample size is appropriate for the continuous data obtained to be generalisable to endorsed clinical neuropsychologists within Australia, with alpha = 0.10 and a margin of error = 0.03 (t = 1.65) (Bartlett et al., Citation2001). However, a slightly larger sample size would have been required to allow generalisation of the of the data to an alpha of 0.05, and approximately double the sample size would have been required to allow the nominal data to be considered generalisable at a p = 0.50, and margin of error = 0.05 (Bartlett et al., Citation2001). Every effort was made to ensure that all available psychologists practicing clinically in the area of neuropsychology linked in with the NPinOZ Google Group were aware of the survey, through reminder emails and a 6 weeks administration window. The response volumes to the survey decreased dramatically following the initial weeks after the survey launch, with only a small spike in responses received after the second reminder. Thus, it was considered of limited utility to extend the survey time. Practicing neuropsychologists in Australia who were not NPinOZ members may not have been aware of the survey, and thus, a reasonable proportion of the workforce may not have had the opportunity to participate. A second limitation is that the full statistical properties of the survey tool remain unknown. While Cronbach’s alpha was derived for the current sample data, full understanding about the reliability and validity of this measure requires elucidation. The tool has been used in two previous characterisation studies (total combined N = 569) (Fisher, Rudkin et al., Citation2020; Withiel et al., Citation2020), and a study evaluating a healthcare family violence clinical champions training model (N = 45) over a 12- to 15-month follow-up period. However, the latter study, and an analysis of the psychometric properties of the scale, also being undertaken, are not yet published. The previous use of the tool allows for some comparison to other clinician samples, but the utility of the tool to the broader literature is yet to be determined. Finally, the nature of the data collection does not allow for further understanding of respondent features which may have influenced outcomes. For instance, it is unclear if any respondents had dual qualifications or psychology endorsements which may have influenced their perceptions and skills in family violence.
The current work does not occur in isolation, and is a part of broader awareness of the impact of family violence on health, across Australian healthcare services. There have been several recent state government-led initiatives that have investigated in detail the impact of family violence, and provided recommendations for improvements to responses within the healthcare system (Queensland Special Taskforce, Citation2015; Victorian Government, Citation2016). Further, as highlighted in the data presented above, New South Wales Health has a standardised family violence assessment tool, resulting in a consistent assessment response across the state. Thus, a number of positive changes in this clinical area in Australia have been made recently. However, the current data highlights a strong need for further training and focus on this area for psychologists practicing clinically in the area of neuropsychology. A health service or clinic may be the only service a victim survivor has contact with and they need to be provided with support and made aware of community organisations that can assist them with their family violence-related needs moving forward. Clients may not desire a referral to social work, and/or they may not have access to this service. Thus, neuropsychologists need to be equipped and adequately trained to support people experiencing family violence by providing a supportive response to disclosures, understanding risk assessment and safety planning, and being aware of available health or community services to refer clients to. This study provided the impetus to incorporate family violence training into clinical training programs to build knowledge and confidence for emerging clinicians. Work of this nature has recently been commenced, with evaluation imbedded, by the research team and three university training partners across Australia. Further research is also needed to better understand the prevalence of family violence among individuals presenting for neuropsychological assessment.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Australian Bureau of Statistics. (2012). 4906.0 - Personal safety, Australia, 2012.
- Australian Institute of Health and Welfare. (2019). Family, domestic and sexual violence in Australia: Continuing the national story 2019. Cat. no. FDV 3. AIHW.
- Ayton, D., Pritchard, E., & Tsindos, T. (2021). Acquired brain injury in the context of family violence : A systematic scoping review of incidence, prevalence, and contributing factors. Trauma, Violence & Abuse, 22(1), 3–17. https://doi.org/10.1177/1524838018821951
- Bacchus, L., Mezey, G., & Bewley, S. (2003). Experiences of seeking help from health professionals in a sample of women. Health & Social Care in the Community, 11(1), 10–18. https://doi.org/10.1046/j.1365-2524.2003.00402.x
- Bartlett, J., Kotrlik, J., & Higgins, C. (2001). Organizational research: Determining appropriate sample size in survey research. Information technology. Learning and Performance Journal, 19(1), 43–50.
- Brandes, D., Ben-Schachar, G., Gilboa, A., Bonne, O., Freedman, S., & Shalev, A. Y. (2002). PTSD symptoms and cognitive performance in recent trauma survivors. Psychiatry Research, 110(3), 231–238. https://doi.org/10.1016/S0165-1781(02)00125-7
- Campo, M. (2015). Children’s exposure to domestic and family violence: Key issues and responses. Child Family Community Australia: Information Exchange. www.aifs.gov.au
- Cox, P. (2016). Violence against women: Additional analysis of the Australian Bureau of Statistics’ personal safety survey, 2012. ANROWS.
- Crime Statistics Victoria. (2017). Crime statistics Victoria: Year ending 31 December 2017. https://doi.org/https://www.police.wa.gov.au/Crime/CrimeStatistics#/
- Draper, K., & Ponsford, J. (2008). Cognitive functioning ten years following traumatic brain injury and rehabilitation. Neuropsychology, 22(5), 618. https://doi.org/10.1037/0894-4105.22.5.618
- Family Violence Protection Act. (2008). Victorian State Parliament §. Australia.
- Feder, G., Ramsay, J., Dunne, D., Rose, M., Arsene, C., Norman, R., Kuntze, S., Spencer, A., Bacchus, L., Hague, G., Warburton, A., & Taket, A. (2009). How far does screening women for domestic (partner) violence in different health-care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria. Health Technology Assessment, 13(16). https://doi.org/10.3310/hta13160
- Feder, G. S. (2006). Women exposed to intimate partner violence. Archives of Internal Medicine, 166(1), 22. https://doi.org/10.1001/archinte.166.1.22
- Feder, G. S., Hutson, M., Ramsay, J., & Taket, A. R. (2006). Women exposed to intimate partner violence: Expectations and experiences when they encounter health care professionals: A meta-analysis of qualitative studies. Archives of Internal Medicine,166(1), 22–37. https://doi.org/10.1001/archinte.166.1.22
- Fisher, C. A., Galbraith, G., Hocking, A., May, A., O’Brien, E., & Willis, K. (2020). Family violence screening and disclosure in a large metropolitan hospital: A health service users’ survey. Women’s Health, 16, 1745506520952285. https://doi.org/10.1177/1745506520952285
- Fisher, C. A., Rudkin, N., Withiel, T. D., May, A., Barson, E., Allen, B., O’Brien, E., & Willis, K. (2020). Assisting patients experiencing family violence: A survey of training levels, perceived knowledge, and confidence of clinical staff in a large metropolitan hospital. Women’s Health, 16, 1745506520926051. https://doi.org/10.1177/1745506520926051
- Gabbe, B., Ayton, D., Pritchard, E. K., Tsindos, T., O’Brien, P., King, M., Braaf, S., Berecki-Gisolf, J., & Hayman, J. (2018). The prevalence of acquired brain injury among victims and perpetrators of family violence. Brain Injury Australia. https://www.braininjuryaustralia.org.au/wp-content/uploads/BRAININJURYAUSTRALIAfamilyviolencebraininjuryFINAL.pdf
- Graneheim, U. H., & Lundman, B. (2004). Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today, 24(2), 105–112. https://doi.org/10.1016/j.nedt.2003.10.001
- Hegarty, K., Taft, A., & Feder, G. (2008). Violence between intimate partners: Working with the whole family. Bmj, 337(7665), 346–351. https://doi.org/10.1136/bmj.a839
- Kinnunen, K. M., Greenwood, R., Powell, J. H., Leech, R., Hawkins, P. C., Bonnelle, V., Patel, M. C., Counsell, S. J. & Sharp, D. J. (2010). White matter damage and cognitive impairment after traumatic brain injury. Brain, 134(2), 449–463. https://doi.org/10.1093/brain/awq347
- McLindon, E., Humphreys, C., & Hegarty, K. (2018). “It happens to clinicians too”: An Australian prevalence study of intimate partner and family violence against health professionals. BMC Women’s Health, 18(1), 1–7. https://doi.org/10.1186/s12905-018-0588-y
- McLindon, E., Humphreys, C., & Hegarty, K. (2019). Is a clinician’s personal history of domestic violence associated with their clinical care of patients: A cross-sectional study. BMJ Open, 9(7), 1–9. https://doi.org/10.1136/bmjopen-2019-029276
- Newman, C., & Iwi, K. (2015). Engaging with perpetrators of domestic violence: Practical techniques for early intervention. Jessica Kingsley Publishers.
- Office for National Statistics. (2017). Compendium: Domestic abuse, sexual assault and stalking.
- PricewaterhouseCoopers. (2015). The economic case for preventing violence against women/November 2015: A high price to pay.
- Pritchard, E., Tsindos, T., & Ayton, D. (2019). Practitioner perspectives on the nexus between acquired brain injury and family violence. Health & Social Care in the Community, 27(5), 1283–1294. https://doi.org/10.1111/hsc.12770
- Psychology Board of Australia. (2019). Psychology Board of Australia registrant data: 01 January 2019 to 31 March 2019, (September), 1–10. https://www.psychologyboard.gov.au/About/Statistics.aspx
- Queensland Special Taskforce. (2015). NOT NOW, NOT EVER. Putting an end to domestic and family violence in Queensland.
- Rose, D., Trevillion, K., Woodall, A., Morgan, C., Feder, G., & Howard, L. (2011). Barriers and facilitators of disclosures of domestic violence by mental health service users: Qualitative study. British Journal of Psychiatry, 198(3), 189–194. https://doi.org/10.1192/bjp.bp.109.072389
- Trevillion, K., Howard, L. M., Morgan, C., Feder, G., Woodall, A., & Rose, D. (2012). The response of mental health services to domestic violence: A qualitative study of service users’ and professionals’ experiences. Journal of the American Psychiatric Nurses Association, 18(6), 326–336. https://doi.org/10.1177/1078390312459747
- Twamley, E. W., Allard, C. B., Thorp, S. R., Norman, S. B., Cissell, S. H., Berardi, K. H., Grimes, E. M., & Stein, M. B. (2009). Cognitive impairment and functioning in PTSD related to intimate partner violence. Journal of the International Neuropsychological Society, 15(6), 879–887. https://doi.org/10.1017/S135561770999049X
- VicHealth. (2004). The health costs of violence: Measuring the burden of disease caused by intimate partner violence. A summary of findings. Victorian Government.
- Victorian Government. (2016). Royal Commission into family violence: Summary and recommendations. Victorian Government.
- Victorian Government. (2020). MARAM practice guides. Chapter summaries. Victorian Government.
- Withiel, T. D., Allen, B., Evans, K., Rudkin, N., Willis, K., Hooker, L., & Fisher, C. (2020). Assisting clients experiencing family violence: Clinician and client survey responses in a child and family health service. Journal of Clinical Nursing, 29(21–22), 4076–4089. https://doi.org/10.1111/jocn.15434
- Withiel, T. D., Gill, H., & Fisher, C. A. (in press). Responding to Family Violence: Variations in knowledge, confidence and skills across clinical professions in a large tertiary public hospital. SAGE Open Medicine. https://doi.org/10.1177/20503121211000923
- World Health Organization. (2013). Responding to intimate partner violence and sexual violence against women: WHO clinical and policy guidelines. www.who.int/reproductivehealth
- World Health Organization. (2014). Health care for women subjected to intimate partner violence or sexual violence: A clinical handbook. www.who.int/reproductivehealth