ABSTRACT
Background
Understanding the psychological wellbeing of people with cancer is a key component of assessment and intervention in quality cancer care. However, the unique experiences of rural cancer populations are less often explored than those from urban centres. The aim of this study was to perform a meta-analysis of Australian studies that compared the psychological wellbeing experiences of people with cancer from rural and urban locations.
Methods
Five databases were searched, and 19 studies, involving 16,947 participants, assessing and comparing the psychological wellbeing of rural and urban populations with cancer were included.
Results
The analysis indicated that Australian rural cancer populations have greater odds of worse psychological wellbeing than those from urban areas (OR = 1.54, 95% CI [1.01, 2.35], p = 0.044). This disparity remains when cancer types are analysed separately, with a slightly smaller odds ratio for rural people with breast cancer (OR = 1.29, 95%CI [1.01, 1.64], p = 0.046) and a slightly larger odds ratio when cancers excluding breast cancer were reviewed (OR = 1.78, 95% CI [1.59, 2.01], p = <.001). Significant heterogeneity was found.
Conclusions
Despite increasing emphasis in Australia on psychological wellbeing throughout the cancer journey, there remain significant disparities whereby rural people experience greater impacts upon their psychological wellbeing. The wellbeing of Australian rural populations with cancer remains an area in which clinical and political focus is imperative. Whilst screening is a necessary first step, additional clinical implications for improving rural access to appropriately skilled health professionals who provide oncology-specific assessment and intervention are suggested.
Key Points
What is already known:
Cancer is a major public health issue, and its psychosocial impacts are substantial, not just on patients but on their families and the broader community.
The prevalence of clinically significant psychological distress is higher amongst people with cancer than the general population. However, identification, treatment, and provision of psychological support is inconsistent across services and geographical areas, and notably lacking in rural areas.
Disparities in screening, assessment and intervention for psychological wellbeing in people with cancer remain, despite the fact that systematic application of screening, appropriate referral, and intervention can improve quality of life and reduce healthcare costs associated with inpatient and outpatient cancer care.
What this paper adds:
This article extends outcomes from previous systematic reviews and analyses from Australia and internationally with the addition of meta-analytic methods. It was specifically designed to solely focus on Australian cancer populations.
The results suggest that Australian rural populations with cancer may have anywhere from 30% to 70% greater odds of experiencing poorer psychological wellbeing than those from urban areas.
This paper highlights ongoing disparities in rural psycho-oncology that may be impacting wellbeing outcomes from rural people in Australia, and urges psychologists, other health professionals, and policy-makers to proactively address these inequities with improved screening, assessment and intervention for their rural populations.
Introduction
Cancer is a major public health issue as a leading cause of illness and death in Australia (Australian Institute of Health and Welfare [AIHW], Citation2020). Data from the Australian Institute of Health and Welfare (AIHW, Citation2020) identified that cancer costs more than $4.5 billion in direct health system costs, without factoring in any indirect costs, such as those resulting from the substantial psychosocial burdens carried by patients, their families, and their communities. With about 150,000 Australians diagnosed with cancer every year, equating to one new diagnosis every 4 min (AIHW, Citation2020), and global cancer burdens escalating, it is important to reduce this burden across economic, medical and, just as crucially, psychosocial impacts.
Cancer disease types are not spread uniformly across populations, with known sex disparities, age, and mortality risks (AIHW, Citation2020). With evolutions in cancer detection and treatment, mortality rates are decreasing (AIHW, Citation2020). Decreasing mortality rates, however, are not necessarily associated with comparable decreases in psychosocial burdens (Rogiers et al., Citation2020). Furthermore, decreasing mortality trends are not consistent across Australia. Generally speaking, those living in rural areas of Australia have shorter life expectancies and higher levels of disease and injury, compounded by poorer access to and use of health services, than their metropolitan counterparts (AIHW, Citation2020). This inequitable trend is also found in cancer care and treatment outcomes (Heifetz et al., Citation2020). Despite this, much cancer research is not disaggregated for patient location, and the unique experiences of rural cancer populations are less often explored than those from urban centres (Loehrer et al., Citation2020). Moreover, there remains a gap in understanding whether the rural challenges associated with health service access and health outcomes disproportionately decrease psychosocial wellbeing, or alternatively, whether rural settings by their very nature provide a level of protection (Wilkins et al., Citation2019). Research appears to suggest that rural residents may indeed hold distinct views on health and welbeing (Gessert et al., Citation2015) and arguably “rural” psychological traits, such as stoicism and self-reliance may have a role to play in why psychosocial wellbeing concerns for rural people with cancer is under-reported and potentially under-detected and under-treated (Corboy et al., Citation2019).
The term psychosocial distress relating specifically to cancer describes a multifactorial continuum of unpleasant experiences of a psychological, social, spiritual, and/or physical nature that interferes with coping, symptoms and/or treatment (National Comprehensive Cancer Network [NCCN], Citation2020). Varying levels of reduced psychosocial wellbeing and increased psychological distress are experienced at all stages of the cancer journey, from pre-diagnosis to survivorship, and before, during and after treatment.
Screening for wellbeing and distress in people with cancer may assist in identifying key concerns, inform specialised referral to psychologists, and provide timely management of distress symptoms, particularly those that may hamper treatment and outcome trajectory (McCarter et al., Citation2018). Australia has been a world leader in recognising and developing comprehensive psychosocial care guidelines for adults with cancer, that are inclusive of distress screening and referral for intervention, and considered to be an equally important component of comprehensive cancer care (Fradgley et al., Citation2019). Despite this, psychological distress in people with cancer often goes undetected, creating a high level of unmet psychological need (Zucca et al., Citation2015, Citation2016). Moreover, despite general consistency in recommendations for universal models of wellbeing and distress screening and intervention guidelines in Australia and worldwide (NCCN, Citation2020), the majority of studies remain focussed on physical disease aspects and survival, and fewer consider geographical differences and impacts (e.g., Girgis, Citation1999; Rowe et al., Citation2022).
Some excellent systematic reviews and meta-analyses have been conducted, in Australia and internationally, on the impacts of psychosocial distress in cancer journeys and the effectivness of psychosocial interventions (Barsevick et al., Citation2002; McCarter et al., Citation2018; Meijer et al., Citation2013; Osborn et al., Citation2006). However, outcomes have been reported without disaggregating for patient geographical location and the specifically Australian context remains a gap for meta-analytic reviews.
Conversely and importantly, Butow et al. (Citation2012) conducted a systematic review of urban versus rural supportive care needs in various countries identifying worse psychosocial outcomes (including poorer mental health functioning, worry and stress, and quality of life) for rural patients. However, they noted that most studies of single cancer diagnoses reviewed focused on breast cancer. Of those, few addressed psychological co-morbidities and co-occurrences, which is known to be complicated by a number of statistical and methodological problems that can potentially misrepresent observed relationships between phenomena (Brown & Thorsteinsson, Citation2020). Whilst highlighting the many discrepancies faced by people living in rural Australia, this systematic review incorporated studies about rural areas from other countries leaving scope for seeking additional understandings of the uniquely Australian context. As Butow et al. (Citation2012) recognised, remote Australia is likely to be vastly different to what might be classified as remote in the United Kingdom, for arguments sake.
A decade on with a further systematic review, this difference was seemingly less pronounced with rural and urban people with cancer across the world evidencing equally high levels of psychosocial concerns (Van Der Kruk et al., Citation2021). This provides some hope for improved future trends for rural oncology. Less recently, but with a solely Australian focus, Girgis et al. (Citation2000) found rural women similar unmet psychological needs as their urban counterparts, but experienced higher unmet physical and daily living needs, perhaps reflective of unique qualities of a rural lifestyle (Girgis et al., Citation2000), distance, and isolation (Girgis, Citation1999). Whilst a more recent systematic review suggested that Australian rural cancer survivors are also experiencing unmet information needs as they transition between treatment services and locations (Goodwin et al., Citation2023).
Generalisability of breast cancer data for broader Australian cancer populations is generally considered inappropriate as there is recognition that breast cancer has high prominence in terms of social and medical recognisability, leaving other cancers “forgotten” (Tariq et al., Citation2019). Moreover, issues of generalisability are particularly problematic given the disproportionately poorer access to cancer care services and subsequent health outcomes that has been identified in Australian Aboriginal and Torres Strait Islander people living in rural areas (Garvey et al., Citation2020).
Previous research has indicated that, given the need for support far outweighs the psychological support services available, there is an opportunity to consider models that support timely and cost-effective training in psycho-oncology to experienced rurally based psychologists (Adams, Citation2010). This is an important consideration given some studies suggest that the disparity in cancer outcomes for rural and urban populations has not changed since the beginning of this century (Fox & Boyce, Citation2014). Regardless, the provision of appropriate and equitable psychosocial care to all people with cancer is an inarguable imperative, whilst at the same time recognising the role of the uniquely rural cultural traits described above in the understanding of wellbeing.
Hence, an opportunity exists to examine psychological distress and wellbeing need differentials between those living in urban and those living in rural areas. This review acknowledges that quality cancer care involves more than just medical intervention, with psychological and supportive care needs being key components, and recognises differing levels of services available in rural and metropolitan areas, whilst identifying that much of the research in this area is limited to breast cancer and clarity remains lacking in understanding the Australian context and its urban and rural settings.
We hypothesised that Australian rural and urban populations experience unequal levels of psychosocial wellbeing in their cancer journeys. We further hypothesised that cancer type influences psychological wellbeing of people in rural and in urban areas, specifically comparing studies of rural and urban people with breast cancer and with cancers other than breast cancer.
Methods
The review was guided by the 2020 standards of the Preferred Reporting Items for Systematic Review and Meta-analyses Statement (PRISMA) (Page et al., Citation2021). The protocol was registered in PROSPERO (Registration number: CRD42021268400), noting some evolution in determining the most effective methodology given the length of time between initial registration and final publication. Ethics approval was not required for this study.
Search strategy
A systematic search of five electronic bibliographic databases was conducted; RURAL: Rural and Remote Health Database, PsycINFO, PubMed and Scopus, and Google Scholar from inception to December 2022. The search terms in keyword (PsycINFO), Title/Abstract/Author Keywords (PubMed, Scopus) and any field (RURAL) included: cancer* AND (qol or (quality of life) or wellbeing or well-being or psycho* or social or emotion* or adjust* or depress* or anx* or (unmet need*) or need* or morbidity or distress) AND (rural or regional or remote or travel) AND Australia* NOT (child* or indigenous* or aborigi* or screening*). The search was limited to full-text studies and scholarly articles in English involving people over 18 years old age. The reference lists and authors of obtained studies were searched for additional studies. Initial searching was completed by the first author; MB and KR completed subsequent screening and searching and discussion to reach consensus, and ET was consulted to resolve any disagreements including any subsequent exclusion of studies that had initially been deemed by original consensus to meet criteria.
Inclusion and exclusion criteria
Studies were included if they quantitatively assessed psychosocial burden or wellbeing needs in a population of rural or regional cancer patients, with a focus on comparing cancer patients from rural areas with those from urban areas. Conference presentations, qualitative studies, systematic reviews, and expert opinions were excluded, along with studies that did not provide sufficient data required for effect size calculation. Studies solely focussed on psychosocial care during the COVID-19 pandemic were also excluded, given the huge shifts in health service provision priorities during this time.
Statistical analyses
Analyses were performed utilising Comprehensive Meta-Analysis software version 4 (Borenstein et al., Citation2022), with a random-effects model applied to account for expected heterogeneity between studies. Odds ratios were calculated for reported data, along with 95% confidence intervals. In cases where more than one wellbeing measure was reported in a study, outcome data was combined if appropriate, or the most salient measure was prioritised if it specified “psychological” or “emotional” problems. An estimate of between-study variance in this random-effects meta-analysis was calculated utilising a tau-squared statistic and I2 statistic.
Quality and bias
Studies were analysed using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Analytical Cross Sectional Studies (Moola et al., Citation2020), which involves assessment of the extent to which included studies have addressed the possibilities of biases in study design, conduct and analysis. Publication bias was recognised as a widespread problem when reviewing available evidence, given positive and negative findings are not equally likely to be published (Thornton & Lee, Citation2000). Publication bias was evaluated using funnel plots and calculation of the failsafe number, that is, the number of unpublished studies with null findings that would reduce the results to an effect of limited or no clinical importance.
Results
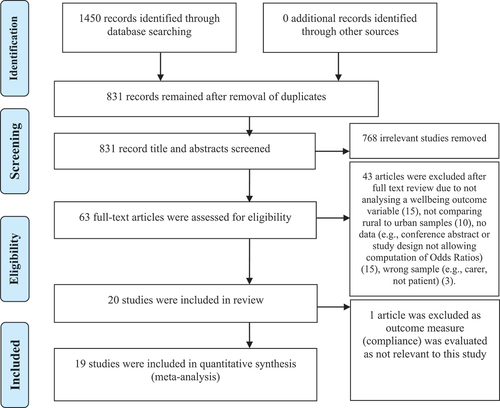
The search of the electronic databases yielded 1,450 articles, of which 63 remained following screening of titles and abstracts and removal of duplicates (). The assessment of the full-text of 63 articles was conducted. Qualitative studies were excluded (e.g., Pascal et al., Citation2015), and others were excluded (e.g., Ahern et al., Citation2016; Corboy et al., Citation2019) as the data did not allow computation of odds ratios (e.g., utilised measurement of rurality on a continuous scale). A total of 20 articles were identified as meeting the initial criteria for analysis. One (Goodwin et al., Citation2019) was then ultimately excluded as their psychological measure, compliance, was determined to be outside the wellbeing definition scope of this study, leaving 19 articles in the meta-analysis ().
Table 1. Key descriptive characteristics of studies and meta-analytic results.
Study characteristics
Study characteristics are presented in . Psychological wellbeing measures included distress, quality of life, burden, anxiety, emotional problems, and unmet psychological needs. There was a total of 16,947 participants, and the average sample size across the studies for rural participants was 326 and for urban participants was 598. A number of cancer types were included in the analysis, with nine studies reporting various or multiple cancer types, five studies focussed on breast cancer, three on haematological cancers, one study on head/neck cancers, and one prostate cancer. The studies were published in the last 20 years, with the oldest being published in 2000 and the most recent in 2022.
Study quality
None of the included studies were considered of poor methodology in terms of the JBI criteria (Moola et al., Citation2020) for bias risk. Four studies were considered to be of good methodological quality and the remaining studies were assessed as very good methodology (). In addition to the JBI criteria, whether studies were sufficiently powered was considered. Only one study reported a power analysis with their study satisfactorily powered for their design (Hall et al., Citation2016), and another study noted a power analysis in their study protocol but did not refer to the outcome of this in their publication (Eggins et al., Citation2022).
Rural and urban population findings
A random-effects model comparing the psychosocial wellbeing of rural and urban populations suggested that there is a significant difference between rural and urban samples (OR = 1.54, 95% CI [1.01, 2.35], Z = 2.01, p = 0.044), indicating that rural cancer patients are significantly more likely to experience adverse psychosocial sequaele than urban patients. There was significant heterogeneity identified (Tau2 = 0.77; I2 = 95%; Q = 377,24, df = 18, p < 0.001). An estimate of the prediction interval was 0.227–10.445; the true effect size in 95% of all comparable populations falls within this interval. Visual inspection of the Funnel Plot of Standard Error by Log odds ratio showed two studies falling to the right of the distribution and three falling to the left. Calculation utilising Rosenberg’s (Citation2005) method suggested a Fail-safe N of 311 (Z = 8.16), which provides confidence for this analysis.
Separate analyses, as per Hypothesis 2, were conducted for breast cancer studies and for studies incorporating various cancers. Studies solely focussed on breast cancer () indicated rural people with breast cancer are experiencing greater impact on their psychosocial wellbeing than urban people, with OR = 1.29, 95%CI [1.01, 1.64], Z = 2.00, p = 0.046. Heterogeneity appeared between these studies (I2 = 59%; Tau2 = 0.042, Q = 9.67, df = 4, p = .046). When analysing studies that included other cancers (), the OR for rural people increased to 1.78, 95% CI [1.59, 2.01, Z = 9.53, p = <.001. As expected, significant heterogeneity was apparent in these studies (I2 = 96%; Q = 339.76, df = 13, p < 0.001).
Discussion
The results of this meta-analysis suggest that rural people exhibit a higher risk of poorer psychosocial wellbeing than their urban counterparts. The odds of rural people with cancer experiencing negative psychosocial sequaele during their cancer journey may be anywhere up to 70% higher than those from urban areas. This is slightly lower for rural people with breast cancer, perhaps reflective of breast cancer’s social visibility and acceptability as not being one of the “forgotten” cancers (Australian Institute of Health and Welfare [AIHW], Citation2013; Sklan, Citation2014). Unfortunately, this more positive trend does not remain for rural people with other cancers. Irrespective of cancer type, the poorer overall wellbeing outcomes for rural people in Australia with cancer is clearly a challenge that needs the attention of policy makers and health care providers. Understanding the causes associated with these lower outcomes remains a challenge, and are likely multifaceted. At a service delivery level, diagnostic delays as a result of undersupply of medical practitioners and fewer multidisciplinary diagnostic and treatment services (Fox & Boyce, Citation2014; NSW Parliament, Citation2022), may be reasonably assumed to be contributors to the inequities between urban and rural healthcare outcomes. However, other factors such as rural cultural traits like stoicism are also likely to be important contributors. Rural residence could be reasonably assumed to be related to poorer psychological wellbeing outcomes throughout a person’s cancer journey. This problem could be significant for rural people generally, but may even be expounded for Aboriginal and Torres Strait Islander people with cancer (Fox & Boyce, Citation2014). Thus, not only must psychologists and health professionals in oncology be aware of the potential negative impact of a person’s rural residential location on cancer treatment, but the higher risk of psychological concerns emphasises the need for proactive psycho-social oncology services for all their rural patients. Addressing service inequality is a necessary step in addressing the overall mortality risk and psychological inequality apparent for rural people.
Whilst the results of the systematic search yielded a small number of published articles in this area, the data also suggest that high visibility cancers, such as breast cancer, are arguably making headway in reducing psychosocial discrepancies between rural and urban people. Rural people with breast cancer are around 30% more likely to experience negative psychosocial sequaele than their urban counterparts, and this increases for the general rural cancer population to nearly 80% more likely to experience psychologically taxing experiences than those from urban areas. Breast cancer remains the cancer type with the highest level of health system expenditure (Australian Institute of Health and Welfare [AIHW], Citation2021). Therefore, there may be some lessons to be learnt to reduce rural psychosocial risk from the way breast cancer is diagnosed and treated within Australia, with not only its high community visibility (such as hugely successful fundraising initiatives like the annual Jane McGrath Day at national cricket matches) and national screening programs, but the level of funding allocated to breast cancer and the capacity for psychosocial care. Clearly, provision of equitable access for rural people with cancer to all aspects of care, from pre-diagnosis through to survivorship, requires a multifactorial approach inclusive of quality psychosocial services.
Whilst interpersonal factors (e.g., general health behaviours) and non-cancer factors (e.g., education levels) have been raised as key clinically meaningful areas for understanding discrepancies, external factors, such as access to and utilisation of psycho-oncology services are also pertinent for this population as a recent parliamentary report so clearly found (NSW Parliament, Citation2022). The Australian oncology healthcare system is complex and the challenge of comprehensive service provision in rural areas is recognised (Hunter et al., Citation2019). Rural patients receiving reduced rates of standard-of-care, compared to their urban counterparts, is not unique to Australia and it has been suggested that health outcome discrepancies may reduce when congruent standardised care is available in all geographical settings (McCullough & Flowers, Citation2018). In particular, integrated and equitable psychosocial care across the cancer journey into survivorship remains an outstanding action in Australian cancer service delivery (Hunter et al., Citation2019). Health equity requires a direct policy focus to reduce the impact that minimal, piecemeal, and non-existent psycho-oncology services in rural cancer settings is having on rural people with cancer. Models with the potential to increase access to psychologists with training in psycho-oncology have been trialled in rural areas in the past with success (e.g., Adams, Citation2010), and these should be further explored.
The psychologically taxing impact of distress, travel and financial burdens, and emotional concerns compound the cancer journey of rural people with cancer. Moreover, professional psychosocial support is often lacking in rural areas with rural people with cancer largely caring for themselves or receiving only informal support, leaving many psychosocial needs unmet (Pascal et al., Citation2015). Rural disparities remain tenaciously resistant and clinicians working with rural populations need to ensure high vigilance in appropriately assessing and treating wellbeing issues for their rural patients. Therefore, it could be argued that psycho-oncology standards for psychological screening do not go far enough for rural people. Screening and rescreening for every rural patient should consider, beyond basic distress screening, broader factors that are psychologically taxing (e.g., role change, physical needs), and how these factors might play out uniquely in rural people with cancer.
Moreover, given the sharp decline in services as one moves more and more geographically remote, referral for psychological services should be carefully considered, with particular consideration given to varying flexibility and variety of services that might be available (NSW Parliament, Citation2022). This is, of course, a challenge for clinicians providing services to rural people in “hub-and-spoke” and fly-in/fly-out models where clinicians are less likely to have local knowledge of what might be available to be utilised (O’Sullivan et al., Citation2015; Weinhold & Gurtner, Citation2014). Recognition of the important role of community in rural areas is a further consideration in referral options. Service access remains a concern for rural people, and highlighting, pre-empting and proactively addressing barriers is essential. Even when screening is conducted routinely, the availability of appropriate, qualified professionals who can provided skilful and timely intervention remains a challenge. The global coronavirus pandemic has provided an unexpected push to improve the availability and quality of telehealth infrastructure, its acceptability for clinicians and consumers alike, and has been supported in Australia with Medicare telehealth incentives. One might argue these changes would have occurred perhaps more glacially otherwise. Services are encouraged to embrace these changes whilst recognising that this technology is not a “one-size-fits-all” solution for rural populations (Barnes et al., Citation2022), particularly if they are simply another barrier to be overcome (NSW Parliament, Citation2022).
Limitations
This meta-analysis has limitations. Specifically, some quality studies were excluded as their data did not allow computation (e.g., measured rurality on a continuous scale). This was a missed opportunity to apply a method to transform continuous measures of rurality to binary (e.g., split at a justifiable middle point) in order to include these studies in the analysis. An additional interdisciplinary database, such as Web of Science, may have been beneficial to include in the search, as well as the addition of medical subject headings in the search strategy. It is also recognised that there are multiple facets of psychosocial wellbeing, measured by a range of instruments, in this analysis. A future analysis that separates these measures into separate domains will be useful in understanding these areas individually. The separate analysis of breast cancer may require revisiting in the future given it has been argued that analyses with less than 10 studies should be treated with caution (Borenstein et al., Citation2022). It is recognised that this study explicity excluded research that was solely focussed on Indigenous Australian people with cancer, due to a concern of conflating Indigenous health inequity issues with rural inequity issues. Of significant concern is that none of the studies that were included analysed disaggregated data for Aboriginal and Torres Strait Islander people in their samples. This is an important population requiring separate research and analysis of their unique challenges and barriers to accessing psychosocial care.
As flagged above, rural research is challenged by definition variations, and as well as challenges in the comparison of remote areas of Australia and their differences to more regional areas. Moreover, the issue of “forgotten” cancers (e.g., Tariq et al., Citation2019) is recognised as is the prominence of breast cancer in Australia, as a well-known, well-serviced condition with significant public visibility as the subject of high profile public health campaigns was identified in the analyses.
Future research
Research in rural psycho-oncology is challenging and defining “rural” is inconsistent and complex as definitions of what constitutes regional, rural, and remote vary. In turn, this may result in measurement bias in research and affect the interpretation of research outcomes and the translation of research into practice (Bennett et al., Citation2019). The Australian Psychological Society (APS) Ethical Guidelines for “psychological practice in rural and remote settings” (Citation2016) aims to provide guidance for psychologists working in this space, but even they do not clearly define “rural” or “remote”. This can make comparisons across studies difficult and blurring population groups can inhibit clear understanding of uniquely rural issues. Despite this, understanding any distinctive psychosocial needs of rural cancer patients is essential for quality psycho-oncology care. It is important for future studies to consider how to develop consistency is the definition of “rural” in Australia, and also in international studies, to assist in comparison within and across nations.
Research into the acceptability of telehealth in a post-covid world will assist in understanding how rural people are faring in relation to their urban peers, with clear recognition of the ongoing technology gaps. Even when research is not purposefully exploring rural experience, local and international cancer research would benefit from disaggregating for patient location to ensure that the experiences of rural cancer populations are not less often explored than those from urban centres. Moreover, studies of psychosocial wellbeing should ensure that rural Aboriginal and Torres Strait people are not just included in research, but that consideration is given to the appropriateness of the assessment tools utilised given cultural challenges in communicating distress (Westerman, Citation2021), and in the abilities of services to hear.
Conclusions
Levels of psychosocial wellbeing are not equivalent in urban and rural cancer populations. Rural people remain at significantly higher risk of psychological impacts of their cancer experiences. Both urban and rural people with cancer continue to experience unmet care needs, but additional uniquely rural needs only compound the psychologically taxing experience. Cancer research of patient location, and the unique experiences of rural cancer populations, are less often explored than those from urban centres. The unique experiences of rural cancer populations are important areas for oncology research, and clearly should be investigated as commonly as urban populations, with not least data being disaggregated for rurality as a standard. The psychosocial wellbeing of rural people with cancer remains a key area of disparity in their oncology journey. As Lethborg (Citation2015) argued, health inequities are inequities that are avoidable. Significant progress has been achieved over the past decade, but Australia has an opportunity to continue their leadership in the psycho-oncology sector, with capacity for further clinical and state and national-level policy commitments in the health care delivery for rural people with cancer. Referral to appropriately skilled psychology and other health professionals is necessary to help rural people with cancer manage their complex care needs and optimise psychological wellbeing. An increased recognition and value placed on psychological health is not to the detriment of medical care, but is instead an enhancement. Rural people deserve the equivalent level of psychological care and health outcomes that exist for their urban counterparts.
Author contribution
All authors were involved in the design of the study. All authors contributed to the conceptualisation of the analyses. M.B wrote the main manuscript text and prepared the figures. All authors reviewed the manuscript.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
Data from this study will be made available upon reasonable request at the conclusion of this research project, once all associated research articles are finalised and published.
Additional information
Funding
References
- Adams, C. (2010). Developing brief training programs in psycho-oncology. How can a one or two day workshop be used to increase access to psycho-oncology support? Psycho-Oncology, 19, S309. https://doi.org/10.1002/pom
- Ahern, T., Gardner, A., & Courtney, M. (2015). Geographical comparisons of information and support needs of Australian women following the primary treatment of breast cancer: A 10-year replication study. Health Expectations, 18(6), 2678–2692. https://doi.org/10.1111/hex.12242
- Ahern, T., Gardner, A., & Courtney, M. (2016). Exploring patient support by breast care nurses and geographical residence as moderators of the unmet needs and self-efficacy of Australian women with breast cancer: Results from a cross-sectional, nationwide survey. European Journal of Oncology Nursing, 23, 72–80. https://doi.org/10.1016/j.ejon.2016.05.001
- Australian Institute of Health and Welfare. (2013). Health system expenditure on cancer and other neoplasms in Australia: 2008–09 (Cancer Series, 81). https://www.aihw.gov.au/reports/health-welfare-expenditure/health-system-expenditure-cancer-2008-09/summary
- Australian Institute of Health and Welfare. (2020). Australia’s health 2020 data insights (Australia’s Health Series, Issue Cat No AUS231). https://www.aihw.gov.au/reports/australias-health/australias-health-2020-data-insights/summary
- Australian Institute of Health and Welfare. (2021). Health system expenditure on cancer and other neoplasms in Australia (Cancer Series no. 131., Issue Cat. no. CAN 142). https://www.aihw.gov.au/reports/cancer/health-system-expenditure-cancer-other-neoplasms/summary
- Australian Psychological Society. (2016). Ethical guidelines for psychological practice in rural and remote settings. https://psychology.org.au/for-members/resource-finder/resources/ethics/ethical-guidelines-psychological-practice-rural
- Barnes, M., Rice, K., Murray, C., & Thorsteinsson, E. (2022). “Double whammy”: A rapid review of rural vs urban psychosocial cancer experiences and telehealth service in five countries during the COVID-19 pandemic. PeerJ, 10, e14382. https://doi.org/10.7717/peerj.14382
- Barsevick, A. M., Sweeney, C., Haney, E., & Chung, E. (2002, January–February). A systematic qualitative analysis of psychoeducational interventions for depression in patients with cancer. Oncology Nursing Forum, 29(1), 73–84, quiz 85–77. https://doi.org/10.1188/02.Onf.73-87
- Bennett, K. J., Borders, T. F., Holmes, G. M., Kozhimannil, K. B., & Ziller, E. (2019). What is rural? Challenges and implications of definitions that inadequately encompass rural people and places. Health Affairs, 38(12), 1985–1992. https://doi.org/10.1377/hlthaff.2019.00910
- Borenstein, M., Hedges, L. E., Higgins, J. P. T., & Rothstein, H. R. (2022). Comprehensive meta‐analysis version 4. In Biostat, Inc. www.Meta-Analysis.com
- Brown, R., & Thorsteinsson, E. (2020). Comorbidity: Symptoms, conditions, behaviour and treatments (1st ed.). Palgrave MacMillan. https://doi.org/10.1007/978-3-030-32545-9
- Bui, K. T., Dhillon, H. M., Brown, C., Xu, K., Shafiei, M., Kiely, B. E., & Blinman, P. (2020). Prevalence and severity of scanxiety in people with advanced cancers: Final results of a multi-centre survey [Conference abstract]. Asia-Pacific Journal of Clinical Oncology, 16(Suppl. 2), 23–24. https://doi.org/10.1111/ajco.13416
- Butow, P. N., Phillips, F., Schweder, J., White, K., Underhill, C., & Goldstein, D. (2012). Psychosocial well-being and supportive care needs of cancer patients living in urban and rural/regional areas: A systematic review. Supportive Care in Cancer, 20(1), 1–22. https://doi.org/10.1007/s00520-011-1270-1
- Corboy, D., McLaren, S., Jenkins, M., & McDonald, J. (2014). The relationship between geographic remoteness and intentions to use a telephone support service among Australian men following radical prostatectomy. Psycho-Oncology, 23(11), 1259–1266. https://doi.org/10.1002/pon.3559
- Corboy, D., Meier, J., & McLaren, S. (2019). Self-reliance and stoicism as predictors of distress following radical prostatectomy in the context of place of residence. Psychology of Men & Masculinities, 20(4), 637–646. https://doi.org/10.1037/men0000197
- DiSipio, T., Hayes, S. C., Newman, B., Aitken, J., & Janda, M. (2010). Does quality of life among breast cancer survivors one year after diagnosis differ depending on urban and non-urban residence? A comparative study. Health and Quality of Life Outcomes, 8(1), 3. https://doi.org/10.1186/1477-7525-8-3
- Eggins, R., Fowler, H., Cameron, J., Aitken, J. F., Youl, P., Turrell, G., Chambers, S. K., Dunn, J., Pyke, C., Baade, P. D., & Goodwin, B. (2022, November). Supportive care needs and psychosocial outcomes of rural versus urban women with breast cancer. Psychooncology, 31(11), 1951–1957. https://doi.org/10.1002/pon.5977
- Elder-Robinson, E., Diaz, A., Howard, K., Parikh, D. R., Kar, G., & Garvey, G. (2022). Quality of life in the first year of cancer diagnosis among aboriginal and non-aboriginal people living in regional and remote areas of Australia. International Journal of Environmental Research and Public Health, 19(1). https://doi.org/10.3390/ijerph19010330
- Fox, P., & Boyce, A. (2014). Cancer health inequality persists in regional and remote Australia. The Medical Journal of Australia, 201(8), 445–446. https://doi.org/10.5694/mja14.01217
- Fradgley, E. A., Bultz, B. D., Kelly, B. J., Loscalzo, M. J., Grassi, L., & Sitaram, B. (2019). Progress toward integrating distress as the sixth vital sign: A global snapshot of triumphs and tribulations in precision supportive care. Journal of Psychosocial Oncology Research and Practice, 1(1), e2. https://doi.org/10.1097/OR9.0000000000000002
- Garvey, G., Cunningham, J., Mayer, C., Letendre, A., Shaw, J., Anderson, K., & Kelly, B. (2020). Psychosocial aspects of delivering cancer care to indigenous people: An overview. JCO Global Oncology, 6(6), 148–154. https://doi.org/10.1200/JGO.19.00130
- Gessert, C., Waring, S., Bailey-Davis, L., Conway, P., Roberts, M., & VanWormer, J. (2015). Rural definition of health: A systematic literature review. BMC Public Health, 15(1), 1–14. https://doi.org/10.1186/s12889-015-1658-9
- Girgis, A. (1999). Self-reported cervical screening practices and beliefs of women from urban, rural and remote regions. Journal of Obstetrics and Gynaecology, 19(2), 172–179. https://doi.org/10.1080/01443619965543
- Girgis, A., Boyes, A., Sanson‐Fisher, R. W., & Burrows, S. (2000). Perceived needs of women diagnosed with breast cancer: Rural versus urban location. Australian and New Zealand Journal of Public Health, 24(2), 166–173. https://doi.org/10.1111/j.1467-842X.2000.tb00137.x
- Goodwin, B. C., March, S., Ireland, M., Manksi, D., Ford, M., & Dunn, J. (2019). Geographic variation in compliance with Australian colorectal cancer screening programs: The role of attitudinal and cognitive traits. Rural and Remote Health, 19(3), 4957–4957. https://doi.org/10.22605/RRH4957
- Goodwin, B. C., Zajdlewicz, L., Stiller, A., Johnston, E. A., Myers, L., Aitken, J. F., Bergin, R. J., Chan, R. J., Crawford‐Williams, F., & Emery, J. D. (2023). What are the post‐treatment information needs of rural cancer survivors in Australia? A systematic literature review. Psycho‐Oncology, 32(7), 1001–1012. https://doi.org/10.1002/pon.6169
- Gunn, K. M., Berry, N. M., Meng, X., Wilson, C. J., Dollman, J., Woodman, R. J., Clark, R. A., & Koczwara, B. (2020). Differences in the health, mental health and health-promoting behaviours of rural versus urban cancer survivors in Australia. Supportive Care in Cancer, 28(2), 633–643. https://doi.org/10.1007/s00520-019-04822-0
- Hall, A. E., Sanson-Fisher, R. W., Carey, M. L., Paul, C., Williamson, A., Bradstock, K., & Campbell, H. S. (2016). Prevalence and associates of psychological distress in haematological cancer survivors. Supportive Care in Cancer, 24(10), 4413–4422. https://doi.org/10.1007/s00520-016-3282-3
- Heifetz, L. J., Koppel, A. B., Kaime, E. M., Palmer, D., Semrad, T. J., Lara, P., & Bold, R. J. (2020). Addressing rural disparities in cancer care via telehealth. Journal of Clinical Oncology, 38(Suppl. 15), e19090. https://doi.org/10.1200/JCO.2020.38.15_suppl.e19090
- Hunter, J., Smith, C., Delaney, G. P., Templeman, K., Grant, S., & Ussher, J. M. (2019). Coverage of cancer services in Australia and providers’ views on service gaps: Findings from a national cross-sectional survey. BMC Cancer, 19(1), 1–11. https://doi.org/10.1186/s12885-019-5649-6
- Lashbrook, M., Bernardes, C. M., Kirshbaum, M. N., & Valery, P. C. (2018). Physical functioning and psychological morbidity among regional and rural cancer survivors: A report from a regional cancer centre. The Australian Journal of Rural Health, 26(3), 211–219. https://doi.org/10.1111/ajr.12419
- Leach, M. J., Gillam, M., Gonzalez‐Chica, D. A., Walsh, S., Muyambi, K., & Jones, M. (2020). Health care need and health disparities: Findings from the Regional South Australia Health (RESONATE) survey. Health & Social Care in the Community. https://doi.org/10.1111/hsc.13124
- Lethborg, C. (2015). Socio-economic perspectives that influence cancer patient outcomes in Australia, including health literacy [Conference abstract]. Asia-Pacific Journal of Clinical Oncology, 11, 66. https://doi.org/10.1111/ajco.12432
- Loehrer, A. P., Colla, C. H., & Wong, S. L. (2020). Rural cancer care: The role of space and place in care delivery. Annals of Surgical Oncology, 27(6), 1724–1725. https://doi.org/10.1245/s10434-020-08392-y
- McCarter, K., Britton, B., Baker, A. L., Halpin, S. A., Beck, A. K., Carter, G., Wratten, C., Bauer, J., Forbes, E., Booth, D., & Wolfenden, L. (2018). Interventions to improve screening and appropriate referral of patients with cancer for psychosocial distress: Systematic review. British Medical Journal Open, 8(1), e017959. https://doi.org/10.1136/bmjopen-2017-017959
- McCullough, L. E., & Flowers, C. R. (2018). Identifying and addressing disparities in survival outcomes for rural patients with cancer. JAMA Network Open, 1(4), e181243. https://doi.org/10.1001/jamanetworkopen.2018.1243
- Meijer, A., Roseman, M., Delisle, V. C., Milette, K., Levis, B., Syamchandra, A., Stefanek, M. E., Stewart, D. E., de Jonge, P., Coyne, J. C., & Thombs, B. D. (2013). Effects of screening for psychological distress on patient outcomes in cancer: A systematic review. Journal of Psychosomatic Research, 75(1), 1–17. https://doi.org/10.1016/j.jpsychores.2013.01.012
- Moola, S., Munn, Z., Tufanaru, C., Aromataris, E., Sears, K., & Sfetcu, R. (2020). Chapter 7: Systematic reviews of etiology and risk. JBI manual for evidence synthesis. 2020. In E. Aromataris & Z. Munn (Eds.), JBI manual for evidence synthesis. https://doi.org/10.46658/JBIMES-20-01
- National Comprehensive Cancer Network. (2020). National Comprehensive Care Network clinical practice guidelines in oncology: Distress management. https://www.nccn.org/professionals/physician_gls/pdf/distress.pdf
- NSW Parliament. (2022). Health outcomes and access to health and hospital services in rural, regional and remote New South Wales. https://www.parliament.nsw.gov.au/lcdocs/inquiries/2615/Report%20no%2057%20-%20PC%202%20-%20Health%20outcomes%20and%20access%20to%20services.pdf
- O’Sullivan, B. G., McGrail, M. R., Joyce, C. M., & Stoelwinder, J. (2015). Service distribution and models of rural outreach by specialist doctors in Australia: A national cross-sectional study. Australian Health Review, 40(3), 330–336. https://doi.org/10.1071/AH15100
- Osborn, R. L., Demoncada, A. C., & Feuerstein, M. (2006). Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: Meta-analyses. International Journal of Psychiatry in Medicine, 36(1), 13–34. https://doi.org/10.2190/eufn-rv1k-y3tr-fk0l
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., & Brennan, S. E. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372. https://doi.org/10.1186/s13643-021-01626-4
- Pascal, J., Johnson, N., Dickson‐Swift, V., & Kenny, A. (2015). Returning home: Psychosocial care during the re‐entry phase of cancer survivorship in rural Australia. European Journal of Cancer Care, 24(1), 39–49. https://doi.org/10.1111/ecc.12232
- Pateman, K. A., Cockburn, N. L., Batstone, M. D., & Ford, P. J. (2018). Quality of life of head and neck cancer patients in urban and regional areas: An Australian perspective. The Australian Journal of Rural Health, 26(3), 157–164. https://doi.org/10.1111/ajr.12340
- Paul, C. L., Hall, A. E., Carey, M. L., Cameron, E. C., & Clinton McHarg, T. (2013). Access to care and impacts of cancer on daily life: Do they differ for metropolitan versus regional hematological cancer survivors? The Journal of Rural Health, 29(Suppl 1), s43–50. https://doi.org/10.1111/jrh.12020
- Rogiers, A., Leys, C., De Cremer, J., Awada, G., Schembri, A., Theuns, P., De Ridder, M., & Neyns, B. (2020, July). Health-related quality of life, emotional burden, and neurocognitive function in the first generation of metastatic melanoma survivors treated with pembrolizumab: A longitudinal pilot study. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer, 28(7), 3267–3278. https://doi.org/10.1007/s00520-019-05168-3
- Rosenberg, M. S. (2005). The file‐drawer problem revisited: A general weighted method for calculating fail‐safe numbers in meta‐analysis. Evolution, 59(2), 464–468. https://doi.org/10.1111/j.0014-3820.2005.tb01004.x
- Rowe, A., Crawford-Williams, F., Goodwin, B. C., Myers, L., Stiller, A., Dunn, J., Aitken, J. F., & March, S. (2022, March). Survivorship care plans and information for rural cancer survivors. Journal of Cancer Survivorship: Research and Practice, 17(2), 441–448. https://doi.org/10.1007/s11764-022-01204-0
- Sklan, A. (2014). Inadequate funding for rare cancers in Australia. The Lancet Oncology, 15(12), e534. https://doi.org/10.1016/S1470-2045(14)70497-8
- Tariq, A., Khan, S., Vela, I., & Williams, E. (2019). Assessment of the use of the Internet and social media among people with bladder cancer and their carers, and the quality of available patient-centric online resources: A systematic review. BJU International, 123(S5), 10–18. https://doi.org/10.1111/bju.14720
- Thornton, A., & Lee, P. (2000). Publication bias in meta-analysis: Its causes and consequences. Journal of Clinical Epidemiology, 53(2), 207–216. https://doi.org/10.1016/S0895-4356(99)00161-4
- Tzelepis, F., Paul, C. L., Sanson-Fisher, R. W., Campbell, H. S., Bradstock, K., Carey, M. L., & Williamson, A. (2018). Unmet supportive care needs of haematological cancer survivors: Rural versus urban residents. Annals of Hematology, 97(7), 1283–1292. https://doi.org/10.1007/s00277-018-3285-x
- Van Der Kruk, S., Butow, P., Mesters, I., Boyle, T., Olver, I., White, K., Sabesan, S., Zielinski, R., Chan, B. A., & Spronk, K. (2021). Psychosocial well-being and supportive care needs of cancer patients and survivors living in rural or regional areas: A systematic review from 2010 to 2021. Supportive Care in Cancer, 30(2), 1–44. https://doi.org/10.1007/s00520-021-06440-1
- Watts, K. J., Good, L. H., McKiernan, S., Miller, L., O'Connor, M., Kane, R., Kruger, D. J., Adams, B. R., & Musiello, T. (2016). ”Undressing” distress among cancer patients living in urban, regional, and remote locations in Western Australia. Support Care Cancer, 24(5), 1963–1973. https://doi.org/10.1007/s00520-015-2982-4
- Weinhold, I., & Gurtner, S. (2014). Understanding shortages of sufficient health care in rural areas. Health Policy, 118(2), 201–214. https://doi.org/10.1016/j.healthpol.2014.07.018
- Westerman, T. (2021). Culture-bound syndromes in Aboriginal Australian populations. Clinical Psychologist, 25(1), 19–35. https://doi.org/10.1080/13284207.2020.1843967
- White, K., Roydhouse, J., D'Abrew, N., Katris, P., O'Connor, M., & Emery, L. (2011). Unmet psychological and practical needs of patients with cancer in rural and remote areas of Western Australia. Rural and Remote Health, 1, 1–11. https://doi.org/10.3316/informit.334387320826109
- Wilkins, R., Lass, I., Butterworth, P., & Vera-Toscano, E. (2019). The Household, Income and Labour Dynamics in Australia Survey: Selected Findings from Waves 1 to 17 (2205-0558 (print)). https://melbourneinstitute.unimelb.edu.au/__data/assets/pdf_file/0011/3127664/HILDA-Statistical-Report-2019.pdf
- Youl, P., Morris, B., Anderson, J., & Morstyn, L. (2019). What factors influence the treatment decisions of women with breast cancer? Does residential location play a role? Rural and Remote Health, 19(2). https://doi.org/10.3316/informit.143417998400817
- Zajdleiwcz, L., Dunn, J., Hyde, M., & Aitken, J. (2015). The 1000-survivor study [Conference abstract]. Psycho-Oncology, 24, 234–235. https://doi.org/10.1002/pon.3874
- Zucca, A., Boyes, A., Newling, G., Hall, A., & Girgis, A. (2011). Travelling all over the countryside: Travel‐related burden and financial difficulties reported by cancer patients in New South Wales and Victoria. The Australian Journal of Rural Health, 19(6), 298–305. https://doi.org/10.1111/j.1440-1584.2011.01232.x
- Zucca, A., Sanson‐Fisher, R., Waller, A., Carey, M., Boyes, A. W., & Proietto, A. (2016). Does screening for physical and psychosocial symptoms vary between medical oncology treatment centres? Psycho‐Oncology, 25(5), 521–528. https://doi.org/10.1002/pon.3948
- Zucca, A., Sanson-Fisher, R., Waller, A., Carey, M., Fradgley, E., & Regan, T. (2015). Medical oncology patients: Are they offered help and does it provide relief? Journal of Pain and Symptom Management, 50(4), 436–444. https://doi.org/10.1016/j.jpainsymman.2015.04.018