Abstract
Hospitals work to provide quality, safety, and availability to patients with a wide variety of care needs, which makes efficient prioritisation and resource utilisation essential. Anticipation of each patients’ trajectory, while monitoring available resources across the hospital, are major challenges for patient flow management. This study focuses on how hospital patient flow management is realised in situ with the help of concepts from cognitive systems engineering. Five semi-structured interviews with high level managers and shadowing observations of seven full work-shifts with management teams were conducted, to explore how patient flow is coordinated and communicated across the hospital. The data has been analysed using qualitative content analysis. The results describe patient flow management using an adapted Extended Control Model (ECOM) and reveal how authority and information might be better placed closer to clinical work for increased efficiency of patient flow.
Practitioner summary: This study describes how a large tertiary paediatric hospital’s patient flow management functions. The results offer a new understanding of how patient flow management is communicated and coordinated across organisational levels of the hospital and how authority and information might be better placed closer to clinical work for increased efficiency.
Introduction
Hospitals are large complex organisations whose overall performance relies on teams of experts, i.e. nurses, doctors and first line management for coordinating demands and resources, such as equipment, specialised localities, clinical expertise and staff time (Plsek and Greenhalgh Citation2001). Access to resources is an essential aspect of providing safe and timely care. The consequences of combining limited resources with time critical treatments and unpredictable influx of patients include risks associated with queues, overcrowding, out localisation of patients to inappropriate wards and boarding in the emergency department (Nugus et al. Citation2011).
Hospitals organise patient flow management to provide patients with access to appropriate care. ‘Patient flow’ refers to how hospitals transfer patients between nursing wards, emergency departments (ED) and surgical departments (Villa et al. Citation2014). It is influenced by variations in the severity of patients’ conditions and the type and level of care provided in various wards. The purpose of patient flow management is to find suitable beds for patients, to maintain the quality of care while avoiding bottlenecks, long waiting times and delayed diagnoses or treatments. Suitable beds are beds associated with the right resources, staff and localities for diagnosis and treatment (Harade, 2–3).
Patient flow management approaches are commonly based on engineering and mathematical principles from operations research (OR) that describe ways in which patients can move through the hospital in logical/linear structures and processes (Saghafian, Austin, and Traub Citation2015). Management approaches like these normally fail to account for the complexities of sociotechnical systems (Mahajan et al. Citation2017). In healthcare, several traits of sociotechnical systems complicate the preconditions for OR approaches (Mazzocato et al. Citation2014). Firstly, success of patient flow management is often evaluated through lagging output indicators, such as patients’ experiences, readmission rates and lengths of stay. These indicators do not in themselves translate well into evaluation of how good the whole hospital functions (Winasti et al. Citation2018). Secondly, the inherent complexities of care processes limit the value of importing and adapting models from other industries for managing patient flow (Mazzocato et al. Citation2014). Thirdly, clinical care is managed by individual actors such as nurses, doctors and patients, who are creative beings and autonomous decision makers that act in social hierarchies. They operate on perceived needs and sense of acuity of their tasks and thus express self-organising behaviour. This means that they adapt to each other’s behaviour with experience of what usually works as they are experimenting and learning new ways of manoeuvring the hospital (Mahajan et al. Citation2017; Rouse Citation2008).
When patients enter the hospital in multiple ways and move between different departments and units, they become part of a large organisation that is difficult to oversee. Coordinating activities linked to patient flow management are a fundamental part of everyday work in healthcare management. Scientific work in the domain of team-coordination points to the process of sustaining common ground as integral to joint action (Klein et al. Citation2005). Healthcare work has been described as quite messy with underspecified details, such as when and where things happen, how the work is configured, as well as shifting priorities and time constraints (Nemeth, Cook, and Woods Citation2004). Very little is known about how the prioritisation and coordination functions are performed in-situ by patient flow managers, what information and strategies they use, and which of the work practices they develop that are successful or not. More knowledge is needed about the kind of decision support and skills that are necessary for safe and successful management of patient flow (Reiman et al. Citation2015).
A large, interconnected and adaptive team of managers are tasked on a daily basis with maintaining patient flow through the hospital. Together with their tools, training and organisation the team form a system that perform functions such as recognising, prioritising and deciding. This study aims to explore and describe how patient flow management works through a lens of cognitive systems engineering.
Theoretical frame of reference
Cognitive systems engineering
Cognitive systems engineering (CSE) focuses on understanding the work of sociotechnical systems that are already operational. Sociotechnical systems are defined as combinations of human-, and technological agents that perform work activities within a physical environment, in synergy with organisational structures and processes towards common goals (Carayon et al. Citation2015). The sociotechnical system encompasses two sub-systems: the technical sub-system of equipment, machines, tools, technology and work organisation; and the social sub-system of individuals, teams, and social coordination (Mumford Citation2006). CSE emphasises that system performance emerges from interactions between humans and machines as they are introduced as components in a social environment (Smith and Hoffman Citation2017, 3–5).
Joint cognitive systems
Within CSE, sociotechnical systems are defined as Joint Cognitive Systems (JCS) to emphasise that today’s ‘human-artefact’ co-agency can only be understood as joint units, therefore, not to be decomposable into parts. Instead, the attention is drawn to systems as functional units defined by what they do, rather than what they consist of. JCSs consist of at least one cognitive system, i.e. a system that is capable of antientropic behaviour (Hollnagel and Woods Citation2007, 42–44).
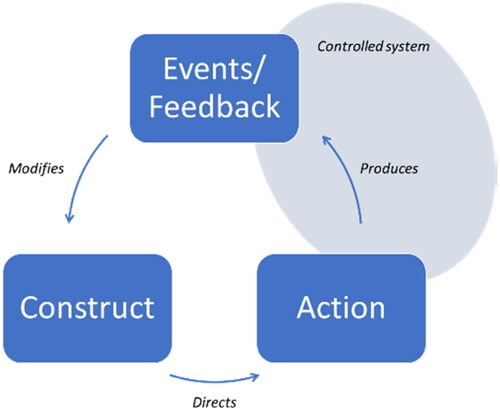
Control is a central concept for JCS and is defined as ‘the ability to direct and manage the development of events, and especially to compensate for disturbances and disruptions in a timely and effective manner’ (Hollnagel and Woods Citation2007, 29). The meaning of staying in control is for the JCS maintain a constant performance output, based on a dynamic and varying input, regardless of disturbances and disruptions. Hollnagel and Woods (2007) explain that control is maintained through a cyclical process called the ‘Contextual Control Model’ (COCOM) ().
Figure 1. Contextual Control Model adapted from (Hollnagel and Woods Citation2007, 19). The JCS’s behaviour (actions) is directed through its understanding of the current situation, the construct. The construct is built on the collective experience and expertise within the cognitive system. It is updated and modified through feedback and events from the operational environment (controlled system). Feedback can consist of information about disturbances, normal operations and expected outcomes (Hollnagel and Woods Citation2007, 145–148).
How control is maintained varies and changes depending on the operational context. It can be classified into four distinct control modes which characterises the system’s behaviour (). Most systems exercise a combination of control modes and can change between them in response to variations in the operational environment.
Table 1. Contextual control modes modified from (Hollnagel and Woods Citation2007, 148).
The COCOM explains adaptive processes and corrective actions at a single system level, for example a ‘doctor-patient’ unit. When the doctor-patient unit is expanded to include several doctors, patients and wards with different needs and priorities they form a larger system that span across organisational levels and scales. The larger system can be explored with the help of the Extended Control Model (ECOM) (). ECOM explains how goals and targets of higher organisational levels become action plans for lower levels and therefore guiding their courses of actions (Hollnagel and Woods Citation2007).
Figure 2. Extended Control Model adapted from (Hollnagel and Woods Citation2007, 153). The model depicts four layers of control. The activities at each layer can be performed at any organisational level but normally relate to an organisational hierarchy. Targets are often set and monitored by high level management while people close to the patients track and regulate the development of everyday work. However, targets can be set and monitored anywhere between hospital directorate, divisions, and departments. Therefore, the ECOM layers may not always correspond directly to the organisational hierarchy.
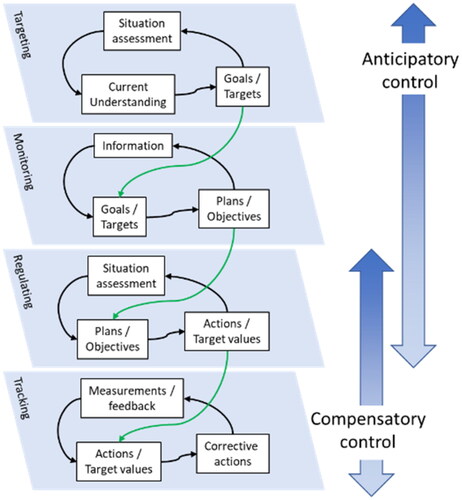
All systems use a combination of feedback and feedforward control to meet current and developing demands. Feedback (compensatory) control occurs when the system recognises differences between intended and actual states. Feedforward (anticipatory) control supports the system in predicting potential future disturbances and deviations. Feedforward activities are strategic and time demanding when new targets are formulated and the situation is monitored. Lower-layer ECOM activities in are closer to the action and use faster compensatory control to regulate and track what is happening in real-time, often in-situ (Hollnagel and Woods Citation2007).
The concept of JCS emphasises a functional approach to modelling the system’s behaviour. Therefore, the unit of analysis is its performance characteristics (Hollnagel and Woods Citation2007, 59). Studies on JCS have been conducted in high-risk industries such as air traffic control (Adriaensen et al. Citation2019), maritime traffic control (Praetorius, Hollnagel, and Dahlman Citation2015) and incident management (Son et al. Citation2018).
Patient flow management as JCS
Hospitals includes many teams that must maintain a constant performance output across multiple levels of organisation (Weaver et al. Citation2018). The hospital cannot stop or halt its functioning which means that it must work in a cyclical manner to adapt to disturbances and accommodate for new demands as they arise (Mahajan et al. Citation2017).
Patient flow management can be understood as a JCS spanning three organisational levels within the hospital. For this study, the lower level of patient care is part of ward management, which is part of hospital management (). Patient care represent the inflow of patients to different wards. It is the inflow of patients at the lowest level of that motivate ward management activities. The huddle is considered an actor for the hospital management where first line managers meet, take census and organise.
The JCS perspective is expected to be useful for focussing the analysis on function rather that structure and therefore suggesting improvements in areas such as agency, distribution of authority, responsibility, and situation assessment.
Methods
Study design
This study was approved by the regional ethical review board of Stockholm (2016/1832-32). It has employed an explorative ethnographic approach using by using multiple divergent data collection methods such as participant observation in the form of shadowing observations and semi-structured interviews (Patton Citation2014; Spradley Citation1980). Artefacts used to support coordinating tasks in daily practice were explored, such as handwritten notes, patient rosters and staff allocation charts (Patton Citation2014, 860–862).
The data collection and analysis were conducted from spring 2019 to fall 2020. This project is reported according to the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist (Supplementary Appendix A) (Tong, Sainsbury, and Craig Citation2007).
Setting and participants
The study was conducted in a large tertiary paediatric hospital caring for approximately 180,000 patients annually with two emergency departments (ED) on different sides of a capital city. The EDs have an annual flow of about 55,000 patient visits. It has surgical capacity, units for neurology, oncology, neonatology, internal medicine, trauma and intensive care. Patient flow management is formally conducted through a bi-daily management team meeting (huddle) with bed-coordinators, ward coordinators and high-level managers. The bed-coordinators are situated at the ED as it is the hospital’s largest inlet for patients, they do however have responsibility for hospital wide bed-coordination. Data collection was primarily conducted in the ED, as the bed-coordinators and the management team huddle form an essential core of patient flow management. During the time of the data collection the hospital was operating close to full or at full census.
Participants
Bed-coordinators (n = 4) were purposefully selected for shadowing observations because their responsibilities span the whole hospitals patient flow and three had at least five years of experience. One (fourth) bed-coordinator was still under training ().
Table 2. Overview of participants for semi-structured-interviews and observations.
Five senior high-level managers were purposefully recruited for individual interviews due to their key function as chairmen for the bi-daily huddle. Four of the participants were medical doctors, and one was a registered nurse (). All interview participants serve as ‘head of department’ with strategic responsibilities for quality and safety. The sample size for the shadowing observations was initially planned to be between 5 and 10 shifts evenly distributed between the participating coordinators. The idea was to allow for the researchers to capture a wide range of experience across all weekdays within a timeframe of a month. This was deemed reasonable because the hospital occupancy varies over time (days to weeks) and the ED occupancy has a high daily variability.
Data collection
Shadowing observations
Shadowing observations is a method often used in cognitive work studies and means; ‘following people, wherever they are, whatever they are doing’ (Arman, 301). KH conducted the shadowing observations of bed coordinators involved in patient flow management.
Four ED-bed coordinators were observed for a total of 56 h (). The observer followed the participants throughout their work shifts (n = 7) and documented in fieldnotes any actions, tasks, communications and use of artefacts. The shadowing observations aimed to capture an in-depth view of what the bed-coordinators do, how they perform coordinating tasks and to understand the underlying reasoning to their choices of strategies. The observations were guided by a semi-structured protocol that included the following themes: ‘What decision is made regarding patient allocation’, ‘What alternatives are discussed’, ‘How are values and priorities discussed’ (Arman, Vie, and Åsvoll Citation2012).
Observation of meetings
KH participated in regular meetings during the shadowing observations. Observed meetings were the ‘start-up meeting’ for the staff at the ED and the bi-daily management team huddle (). These observations focussed on the workflow, discussions, and decisions. Fieldnotes were taken and informal conversational interviews were conducted with involved meeting participants to clarify the observations, after receiving verbal consent.
Informal conversational interviews
The shadowing observations was complimented by informal conversational interviews, a type of spontaneous interview that relies on ‘questions in the natural flow of an interaction, often as part of ongoing participant observation fieldwork’ (Patton Citation2014, 953–954).These focussed on the situation or the ongoing tasks and aimed to gain a deeper understanding of the coordination work. The informal conversational interviews varied in length and depth. They could constitute just one question/answer up to 5 minutes conversation. Questions asked during these interviews were for example ‘Why did you open this patient’s chart?’, ‘What did you look for in the roster?’, ‘How do you think this patients plan will unfold after the huddle?’. The questions were used to clarify participants personal experiences of how events usually unfold and their intuition of risks and benefits of decisions. The informal conversational interviews were audio-recorded after verbal consent on each occasion.
Exploration of artefacts
Twelve artefacts were collected during the interviews and observations. They were purposely selected to further clarify the function of the human-artefact ensemble, participants were asked to think aloud when they used the artefacts during the shadowing observations and during the interviews.
Semi-structured interviews
The five semi-structured interviews aimed to provide additional information from a strategic management perspective, to compliment the shadowing observations’ operational view. The semi-structured interviews were guided by three question areas (Kvale Citation2009):
Purpose of the team huddle
Collaboration among the meeting participants
The role of chairman and their medical competence.
During the interview the participants were asked to reflect on the question areas with the help of short scenarios of patient flow dilemmas taken from the shadowing observations. For example, a discussion between surgeons of different specialities where they had to agree who’s patient to operate considering there were only one postoperative bed available. Probing questions were asked to help the participants to problematise regular events and dig deeper into their experience of how the patient flow management system works. All interviews received written consent, were audio-recorded and transcribed verbatim prior to the analysis.
Data analysis
The analysis was conducted with the use of MaxQDA and Excel. It encompassed two steps, characterised by an abductive process.
The first step was an inductive content analysis (Shannon and Hsieh Citation2005). The fieldnotes were used to arrange the final transcript as ‘narratives of whole work shifts’. This use of field-notes was helpful for the research team in identifying specific chains of events, for example when participants discussed alternative patient flow solutions and later reached decisions during team huddles. Meaning units when patient flow was mentioned were identified and condensed by KH, the condensed meaning units were regularly checked with the research team. Clarifying questions were posed to the ED bed coordinators as the data collection and analysis took place simultaneously.
During the second step, the results from the inductive analysis were compared with the emerging corpus of data. The condensed meaning units were interpreted as of what they mean in the context of the whole work shift. Codes and categories were revised accordingly, see for an example of the analysis. It was in this second step that the final five categories presented in the results () were achieved.
Table 3. Example of analysis from meaning unit to condensed meaning unit, analytical interpretation, code and category.
Operationalizing the ECOM layers
In the deductive step of the analysis, the ECOM layers tracking, regulating, monitoring, and targeting were used to understand the interdependency of how categories of activities in patient flow management took place, and how to describe the links between levels of organisation (). The research team used an operationalisation of the ECOM layers to allow for transparency and for critically review the coding in relation to the identified ECOM-layers (Supplementary Appendix D, including additional examples of analysis).
Table 4. Example of codes included in the category ‘Recognizing critical situations’ and their distribution across the ECOM layers.
See Supplementary Appendix B for the code and category scheme with distribution of codes across the ECOM layers. Information of how the codes and categories relate to the different data sources and the ECOM model are found in Supplementary Appendix C.
Graneheim Lindgren, and Lundman (2017) point to the risk of achieving inconsistency of data and analysis when data collection is ongoing over longer time periods. This was managed by meetings where the team would go back through the dataset and reflect on how new data and codes fit in to the bigger picture of emerging categories. Therefore, the analysis entailed regular meetings where the team coded parts of the data together. KH (main author, ICU specialist nurse) and GP (human factors specialist and CSE) met several times during the first iteration of analysis. KHP (patient safety researcher and paediatrician) and ME (professor of patient safety and expert in qualitative methodology) joined several meetings towards the later stages of coding and categorisation to facilitate a sceptical discussion of coding and categorisation as well as negative cases or inconsistencies in the analysis (Devers Citation1999).
Results
The results are presented as five categories of activities in patient flow management. represents the core activities of the management system at the ward- and hospital levels that are Recognising critical situations, taking stock, defining constraints, evaluating alternative action plans and identifying new targets.
Categories of activities in patient flow management
Recognising critical situations
Recognising critical situations is about agreeing when the risks of not meeting previous targets of for example occupancy, waiting times or number of patients per nurse or doctor becomes too great.
Ward management
A frequently observed function of the ED is to mark a patient with a ‘decision to admit’ which will start the process of finding a bed and therefore function as feedback data for the team huddle. The number of patients in cue for a bed while having a ‘decision to admit’ is therefore an important part of recognising how critical the patient flow situation is.
(Ward coordinator) So what we have is another tool too. But it’s just in the ED. [The coordinator opens a webpage ‘Ready at the ED’]. Right now, we have 14 patients on our ED here. Six have not been seen to, three have been here over eight hours and two need admission to a ward. One is this iatrogenic harm that I got a bed for ward 11. The other is the injured forearm planned for day surgery. So, then I know they are done. (Code 102)
The patient flow management team recognises when situations are about to become critical in response to earlier actions as they meet in team discussions, either in the clinical context at the wards or at the strategic context of the team huddle. Situations in the clinical context are visible for the team as concrete physical limitations, for example the number of patients in queue, available rooms and staffing. The work of managing patient flow at the ward level are supported by close-to-real-time data from occupancy charts and bed planning tools from the clinical level. Data from these systems are primarily results of medical decisions; for example, to admit or discharge a patient with or without treatment.
Hospital management
The management team huddle keeps track of the acute patient flow and the discrete flow of low-acuity patients ‘in-queue’. Here, all patients receive a priority based on the overall hospital wide situation. For example, some patients have increasingly long waiting times because they keep being postponed by the constant influx of new acute patients with higher priority. The high- and low-acuity flows are often separated as they need to use different wards.
Hospital management assesses the bigger picture of patient flows and workload across departments. Information at the team huddle is a mixture of individual patients’ narratives and categorical data such as queues and available beds. A situation is recognised as critical when the team is unable to negotiate reasonable solutions for patients with imperative needs. For example, the paradoxical situation when there is a lack of available overnight beds, ‘low acuity day surgery’ can then be prioritised over more acute and complex patients that need to overnight at the hospital.
(Ward Coordinator) We will have four patients in three beds now.
(Chairman) So it’s a bit full house so to speak. So, this facial surgical patient could be housed in ward 12 then? I think it will go to…
(Surgeon) Facial surgical patient?
(Chairman) Yes, the one that is currently in the ED. It has a fractured jaw. So, we need to fix that acute. As we can see there is already full house and still a lot that is already planned. Eh, and we are reducing our beds tomorrow for the weekend. So, we can’t really operate on something that we know will have to overnight. Something that is not imperative. (Code 26)
Taking stock
Taking stock represents the census of how many beds and patients that are in the hospital or on the way in or out. Part of taking stock is about agreeing on definitions such as patient’s acuity levels and if a bed shortage is lack of physical space or staff.
Patient care
Each patient at the clinical level is represented through journals and individual handwritten notes. The individual note on each patient is used to communicate care needs and other qualitative aspects of care that help with prioritisation decisions at the team huddle. Furthermore, the individual notes are used as report cards as they are physically handed to the receiving nurse in patient transfers.
(Ward Coordinator) Hi, will the forearm be operated on day-surgery?
(ED Doctor) We are just arranging transport.
(Ward Coordinator) Fantastic [takes out a bundle of post-it notes] I often have little notes like this. Each note is a patient. So Ill note social security number, name. A little note on the diagnose and procedure, a forearm. Fasting. Surgery on day-op. Then I’ll know, nursing team three, NN who is doctor in charge.
(Ward Coordinator) Sometimes I’ll have like seven admissions in the morning. I’ll also add the time of arrival at the ED. Then I’ll walk around to the doctors to ask who is most in need of a bed. Lots of patients can just have gotten fluids during the night and feel better already. (Code 97)
Ward management
The coordinator at the clinical level collaborates with lead nurses and medical doctors to take stock of the current situation at the ED. Information is continuously updated and documented in a way that can be transferred between work shifts. The following quote is an example of how the team update their construct (understanding) of the system state.
(Ward Coordinator) We start with checking with the senior resident at 8:30 [in the morning]. I’ll write in the notebook. Here in this column, I’ll write with permanent ink [the column with established beds]. But now I didn’t really know the situation. So, ink… ink… and not here were I erase a lot [the column indicating free beds]. Then in the evening I’ll tear this page and give it to the nightshifts lead nurse so that she can be up to speed. (Code 95)
Hospital management
At the hospital management level, patients are presented as categorical data, such as queue positions, overcrowding, established- and available beds. The team huddle begins with taking stock of the situation at the different wards and units with the question ‘How many available beds do you have?’.
The team huddle uses an excel spreadsheet to document the daily census of the hospital’s beds and planned patient flows while discussing the interpretation of available beds and individual patient narratives. In the case below, the team does not initially agree on how to calculate three of the beds on ward 10 as they are daybeds. Daybeds are only available during office hours for patients that will be discharged the same day.
(Chairman) Good, so ward 10?
(Ward Coordinator) It is 22 patients now.
(Chairman) On 23 beds?
(Ward Coordinator) Yes
(Chairman) So you have one bed to spare?
(Ward Coordinator) No, we have [staffing for] 18 plus 2.
(Chairman) But it says 18 + 2+3? [indicates a row of numbers in the column for available beds in the excel spreadsheet].
(Ward Coordinator) Okey, but then we have full occupancy on those as well. I did not count those three. So, in that case we have 25 patients on 23 beds. (Code 19)
As the discussion continues the team finally agrees on how to calculate the beds and conclude that ward 10 has 22 patients on their 18 + 2 beds (18 staffed and two extras for overcrowding), not counting the three daybeds. This type of discussion is typically nuanced by the ward coordinator’s notes on individual patient’s needs.
Defining constraints
Defining constraints is about agreeing on what limits the team’s ability to manoeuvre, for example time constraints and bottlenecks such as bed shortage.
Patient care
Bed shortage at the patient care level is commonly solved by out localising patients to the first available bed, regardless of ward speciality. Each patient is cared for by a medical doctor that is responsible for making rounds regardless of where the patient is. This exposes a limit to how many different types (specialities) of patients one nursing team can manage. In the example below, the clinical team discuss how many different types of medical doctors they can coordinate with.
(Assistant nurse) It’s probably the rounds that messes up the day. They are so many and have no fixed schedules. They [medical doctors] just stand there looking at you [.] wanting to do rounds now, or they will have to leave.
(Ward coordinator) Yes that is my opinion to […] right now there are patient of all categories on almost all wards […] one nurse can have four different doctors to do rounds with. (Code 165)
Hospital management
Bed shortage at the hospital management level exposes a critical time constraint.
(Bed Coordinator) Yes, most of [the wards] … they are already there with [full capacity]. The time is already too late and when the nightshift arrives so…
(Ward representative) We are aware of that. So, we cannot make any new revolutionary… [plans]. (Code 144)
As the hospital is open every hour of the day and the next shift is always approaching, the teams are always pressured for decisions. Time pressure in combination with acute patients around the clock on top of planned patient flows create urgency to move on and identify new targets or action-plans.
Evaluating alternative action plans
Action plans are discussed before there is a decision to identify new targets. For example, the initial response to bed shortage in the ED is to select from a range of established strategies, such as filling wards with low acuity patients, overcrowding wards that have free beds sorted in order of perceived overall workload; or delaying surgery that is not imperative, or to construct a domino effect of linked patient transfers. Evaluating action plans normally takes place on the hospital management level of the JCS, but may have consequences for the other layers
Hospital management
Action plans at the hospital management level quickly escalate to complex chains of transfers because of high overall occupancy. Plans to transfer patients in times of overcrowding are typically based on expected developments in patients’ conditions. Chains or domino effects increases the workload of the management teams to keep track of each patient’s plan.
(Ward representative) And then we have two more coming in tomorrow as well.
(Ward representative 2) I know that, but we don’t count those [patients] until they are confirmed. It is one heart valve to be arriving at 06:30 and one other in 08:30.
(Ward representative) They usually stay for one day. We hope that one of them can discharge directly from the post-op. But otherwise, it is an overnighter.
(Chairman) [checking ward nine’s occupancy chart] So is that the one you thought could go home?
(Ward representative) Yes, the one in room 12 [the patient is on the list as ‘coming’.]
Identifying new targets
Some situations require actions that are outside of the ward management’s authority. The question of finding new targets is then escalated to the hospital management by the ED bed coordinator, ward coordinators or surgeons. The team huddle decides how to approach novel patient flow solutions and overcrowding by setting targets the ED-bed coordinator are not formally allowed to use.
Hospital management
When acceptable plans for action have been discussed at the team huddle and the critical situation persists, the meeting advances to find more novel or complex solutions. That can be to halt certain surgical procedures and diverting patients to hospitals in other regions. Some of the new targets must be escalated to a tactical level above the team huddle, the level of chief medical officers and hospital directorate. Therefore, creating further delay before new action targets can be made available to the ward management.
(Chairman) It looks quite calm at the ED in NN [another hospital]. So, let’s call them and see if they can muster a few beds. We must check our list if something is transferable. But for now, ward 10 must be the buffer. And I will take the question with me about the decision we talked about [regarding stopping elective surgery and diverting patients to other hospitals]. (Code 19)
Linking the three layers of organisation
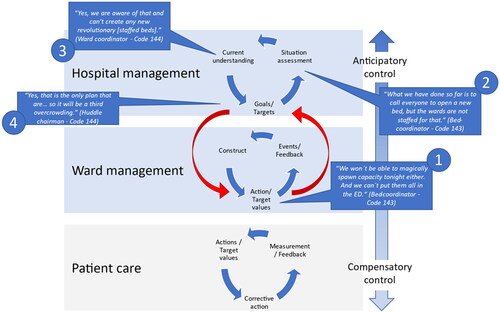
Links between organisational levels are established when, for example, the ward management teams need new options from the hospital management in response to demands from clinical care. depicts an instantiation of the link between the two levels of organisation above clinical patient care.
In the example below, the ED bed coordinator identifies limitations of the hospital capacity. The coordinator uses her experience to assess the situation and discuss potential new action targets such as ‘magically spawn capacity’, ‘put all patients in the ED’ or ‘controlled distribution of overcrowding by opening an extra bed on each of the wards’. Among the three alternatives discussed here, only the option of systematically controlling the overcrowding by adding one extra patient per ward is documented as a policy and therefore sanctioned for the bed-coordinator to use without activating higher control layers. However, the situation would require more than a third extra patient on each of the wards, which is the limit of what the formal policy allows, therefore it triggers a need for escalation to the management team huddle (). Opportunistic control of this type is characterised by short-time frame and management on the spot rather than on a tactical or strategic considerations, as the coordinator alone lacks the authority for higher level decisions outside the written policy. The situation is escalated to the management team huddle in which the chairman uses verbal reports from the ward coordinators and data from occupancy charts to assess the situation. The chairman then sanctions a temporary third overcrowding in each of the hospitals’ wards. Therefore, allowing new actions to be taken at the first line management level.
Different situations were observed when the connection between organisational layers provided support for ward managers as exemplified in . For example, when several patients simultaneously moved from the ED to surgery to post operative wards and finally a nursing unit; while simultaneously others came directly from home via surgical waiting lists, and some entered the hospital from outpatient clinics needing nursing units and highly specialised medical interventionists. One of the lead medical doctors in the ED described this as ‘we live on the brink of a small constant crisis’.
Discussion
For this study the hospital is identified as a multi-layered JCS. The study’s aim was to explore and describe how patient flow is communicated and coordinated in situ from a CSE perspective.
Ward level management
The wards cannot pause or halt acute patients that are nested within elective and low acuity patient flow. Therefore, they operate mostly in an opportunistic control mode. Opportunistic control (Hollnagel and Woods Citation2007, 145–148) means that individual managers use experience, personal networks and domain knowledge to quickly find practical, in-situ solutions to solve potential conflicts, such as acute bed shortage. The behaviour of first line managers and clinicians becomes a way of working the system and shows the adaptive capacity of the JCS. It is however problematic from a management perspective as it is difficult to observe and measure adaptations in real time. It can also be questioned if this adaptive behaviour can be considered ‘safe’ from a patient’s point of view.Solutions made in opportunistic control tend not to take a longer time-horizon and multiple consequences of actions into concern – it is spontaneous and deemed as necessary in specific situations.
Opportunistic control changes over time as teams of individuals learn to manoeuvre the system. A previous study observed how a group of first line managers in a single ward reached a state of reorganisation when the work pressure left them with no more reasonable trade-offs or risks to manoeuvre with. The incremental steps towards higher control encompassed both goal setting, communication channels and the management team’s own composition (Hybinette, Pukk Härenstam, and Ekstedt Citation2021). Here we have observed how first line managers and clinicians on one end of the system, for example the ED, interpret a patient flow situation as successful when in fact it creates higher level problems in other places, such as in the nursing wards. Using an ECOM model to expose this type of double bind offers health systems designers a way to think about how local improvements may affect the wider system. The model helps by exposing ‘control problems’ rather than a ‘production problems’.
Opportunistic controls are normal for sociotechnical systems in highly complex work settings. However, there is a risk of falling further down into a scrambled mode if the context of operations changes, e.g. in case of a rapid increased influx of patients or changes in bed availability across the hospital. Often being on the brink of losing control is an important difference between patient flow management in the hospital and management in other complex systems as in for example disaster medicine (MacKinnon et al. Citation2022) or emergency services (Son et al. Citation2018). These examples of emergency systems have more clearly articulated boundaries between ‘normal’ and ‘disaster’. Were ‘disaster’ represent a defined system state with its associated information needs, required staff skills and communication channels. What constitutes a disastrous situation in the hospital’s patient flow is in our study rather defined by first line managers experience of being on a course towards unacceptable quality- and safety trade-offs. In this case the very need of activating certain communication channels or raising certain questions to the team huddle, can be viewed as early warning signals for higher level management to pick up on.
Work in scrambled mode as we have observed are unavoidable for short periods of time considering the hospitals drive towards full resource utilisation. To have empty beds reserved ‘just in case’ is not motivated if there are patients in ques. We have observed how this results in high workload situations for which the bed- and ward coordinators have adapted their mode of communication, by reverting to paper notes and phone calls to maintain speed rather than using computer systems for thoroughness. Meaning that they in scrambled mode bypass ways of creating traceability of the patient flow process and lose opportunities for creating data for evaluation and learning. The ability to create traceability and data even in high workload situations is something that could be improved with technical solutions if work in scrambled mode is unavoidable.
Linking ward- and hospital management
The intended function for the management team huddle is to create a census of the hospital and make decisions based on plans, rules and procedures. But, as first line managers tend to wait until the upcoming team huddle to raise patient flow issues, both information on escalating problematic situations and subsequent decision making is delayed. When new action targets are finally formulated at the higher level of control (huddle) and communicated downstream, the conditions at the wards may already have changed. Subsequent patient transfers will be delayed which leaves resources unused, like empty beds or nurses time during overlap between shifts.
The huddle is detached from the flurry of activity around the hospital and is a bi-daily event where people assemble to share the latest information and reach decisions. Therefore, as increased pressure in one ward does not immediately affect others, it might not even be noted until it is too late. An effect that has been described for large industries as ‘tragically delayed transformation, i.e. when the system does not reorganise until the need is apparent’ (Hamel and Välikangas Citation2003).
Information on the state of the system should be supported by artefacts (Lundberg and Johansson Citation2021). The artefacts found in this study (for example post-it notes, and the huddle excel spreadsheet) represent fragmented information of the system’s state. They project lagging data and are used for narrower purposes than ‘overall system view’, such a being patient rosters, hand-over notes for nurses or surgical schedules. This is detrimental for tactical control as the huddle must spend considerable effort on situation assessment. As tactical control is supported by plans, rules and procedures it could be better placed with the first line managers, given proper support. For example, the plan for systematically distributing overcrowding by allowing the ED bed coordinator to overcrowd each of the wards with up to three patients. This is a working strategy that allow the huddle more time to address strategic decisions of for example long term bed-allocation.
Point of control
While higher-level managers struggle to uphold continuous control, the influx of patients create activities between the meetings. Interconnected patient pathways become problematic for higher level management when patients compete for specific wards capacity, when the patient’s need treatment for more than one condition and when the census for the hospital is at full capacity or over. The lack of real time data and objective measures of available beds introduces several complexities for the management huddle. For example, additional surgical capacity may later add to the demands of pre- and post-operative wards and subsequent need for specific nursing wards. The problem for higher level management dealing with these limitations is to decide what level of anticipatory control that can be exerted by the team huddle, and how the system might recognise if there is a need for reorganisation approaching. The point of control depends on the type of decisions exerted and the system boundaries. Our study found that even the management team huddle referred to a higher organisational level for some strategic decisions regarding patient flow and resource allocation. This suggests that some of the mandate for strategic decisions lie outside the boundaries of our defined hospital management.
The ability of single wards to locally adapt to extraordinary circumstances points to a high degree of operational independence. Operational independence is a tenet of so called ‘system of systems’ (Meier Citation1998). Which in our case means that the constituent wards of the hospital are smaller interconnected, goal driven systems in themselves following an internal logic, ending up competing with themselves for resources and decreased workload. The wards do what is best locally and have difficulties in relating to the overall hospital situation. One central task for the management team huddle is to balance between acute patient flow and maximising elective surgical capacity. The distributed nature of patient flow management offers no ‘one point of control’ for tactical or strategic decision makers. Strategic control is based on models and predictions that need elaborate data to compliment the patient narratives that were used consistently in all observed team huddles. For the huddle to maintain strategic control, it would need data-based models to compliment patient narratives for predicting system behaviour. The instantiation of a real case in the ECOM model (scenario in ) highlight how the narrative supersede use of data in the managers discussion, and how the ECOM model could be used in discussions of system improvements.
Reflexions on using ECOM for exploring hospital patient flow
The approach of following decision makers and meetings over time has enabled us to highlight the consequences of actions across organisational levels. The use of cyclical models ( and ) imply that processes happen in a specific order with a certain time between the steps. We observed that these activities were not coordinated in such a way. It is rather the case that separate cycles are simultaneously active at various stages in different wards. The result is that the management team huddle needs to spend considerable effort to agree on for example how many beds that are available and how to interpret the occupancy situation, before the meeting can start setting new overarching priorities and goals.
Figure 3. The figure depicts the actors (to the left), artefacts and units involved in patient flow management (to the right). The artefacts mentioned in the figure represent tools for each level such as patient occupancy charts, rosters and handwritten notes. Some artefacts are visible as information sources for actors at all three levels while some are used locally.
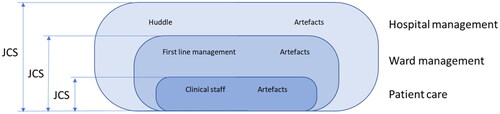
Figure 4. Five categories of activities in patient flow management. The figure should be read as a continuous sequence of activities. The arrows represent both sequence and time-delay.
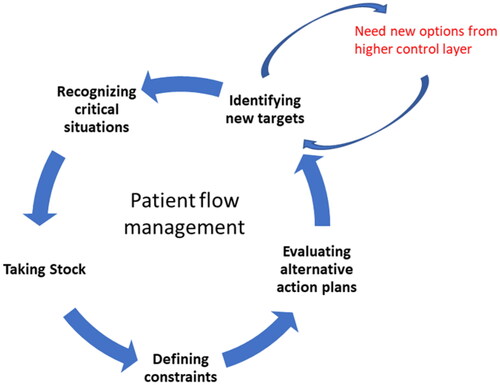
Figure 5. An instantiation of how the patient flow management link the three layers of organisation. The bottom layer is greyed as direct patient care was not explicitly observed but rather form the input of patient flow for the ward management to handle. The quotes in this instantiation are read clockwise from the ward management level.
A system of this type theoretically resists centralised control, but rather requires mechanisms for cooperation. The system needs a continuous (or frequent enough) link between organisational levels so that it does not create unnecessary delay in distributing authority and information to lower levels. Our results points towards the need of organising the system for more efficient communication of real care needs. Therefore, it is advisable that higher level management pay specific attention to how people make sense of what is going on, on shared decision making and tools for sensemaking at the wards to mitigate the hampering effect of the huddle. Our results can potentially be operationalised for describing the time it takes for patient flow data to be transformed into patient flow solutions and to measure for example ‘time from new action targets to feedback on completion’. This perspective adds to earlier work in a way that complexities and interactions are made salient.
Strengths and limitations
This is a single centre study taking an explorative ethnographic approach for describing how a hospital realises patient flow management in situ. The study has been conducted in the form of a case study, utilising several interview and observation techniques, as well as different analysis strategies to ensure the results’ trustworthiness.
Lincoln (Citation1995) suggest that trustworthiness in qualitative studies can be discussed in terms of credibility, transferability, dependability and confirmability. This case study presents findings from a single setting with a limited sample of observations and interviews. As a single setting study, the results may not be directly transferable to other settings, but they may yet still provide a new lens and reasoning on how to uncover the complexities of everyday patient flow management. The patterns emerging within the limited data may affect the generalisability of the results. However, the triangulation between 56 h of observations, conversational interviews and five semi-structured interviews, allowed us to arrive at thick descriptions of the setting, the work of the JCS at different levels, as well as the trade-offs, dilemmas and strategies that the experts faced as part of their everyday work. Especially the scenarios used within the semi-structured interviews can be identified as a strategy to increase the study’s credibility and confirmability as experts were presented with information obtained through the observations and asked to reason about these.
Qualitative research in health systems require several strategies and techniques to ensure scientific rigour (Devers Citation1999). summarises how these have been addressed in this study.
Table 5. Summary of strategies applied in this study for scientific rigour according to Devers (Citation1999).
Methodological discussion
Our approach to data collection is intense and generates large amounts of data. There is a described risk that the workload of preparing the data set negatively affects 'reflection in the field' and time for analysis between shadowing sessions (McDonald and Simpson Citation2014). This was mitigated using a semi-structured observation template and by frequent analysis team meetings interspersing data collection. Research group meetings between shadowing observations provided focus for subsequent data collection and opportunity for the research team to discuss KHs observations and potential observer bias. The ethnographic design with several iterations of data collection and analysis did enable the research team to let the conceptual frameworks of CSE to guide observations, and to continuously visualise observed dependencies within the multi-layered organisation (Roth and Patterson Citation2005).
Furthermore, the use of the operationalisation allowed for continuous reflection and self-criticism in research team meetings, that aimed towards verifying codes and categorisation as well as control for the influence of KHs pre-understanding (Graneheim, et al. Citation2017).
Conclusion and future research
While ward management focuses on finding resources for upholding patient flow, hospital management struggle to keep up strategic control by spending considerable effort on collective sensemaking supported by low fidelity communication tools and patient narratives. Managers of patient flow systems may benefit from using scenario-based training of real cases that triangulate complex time-critical events from multiple perspectives in supporting multiple levels of control.
A specific question for future research is to determine how qualitative aspects of patient narratives might be used to support patient flow coordination?
Ethics approval
This study was approved by the regional ethical review board of Stockholm (2016/1832-32).
Supplemental Material
Download Zip (552.9 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The original data is in Swedish and will be provided upon reasonable request.
Additional information
Funding
References
- Adriaensen, A., R. Patriarca, A. Smoker, and J. Bergström. 2019. “A Socio-technical Analysis of Functional Properties in a Joint Cognitive System : A Case Study in an Aircraft Cockpit.” Ergonomics 62 (12): 1598–1616. doi:10.1080/00140139.2019.1661527.
- Arman, R., O.E. Vie, and H. Åsvoll. 2012. “Refining Shadowing Methods for Studying Managerial Work.”. In The Work of Managers towards a Practice Theory of Management, edited by Tengblad S, 301–317. New York: Oxford University Press. doi:10.1093/acprof:oso/9780199639724.003.0016.
- Carayon, P., P. Hancock, N. Leveson, I. Noy, L. Sznelwar, and G. van Hootegem. 2015. “Advancing a Sociotechnical Systems Approach to Workplace Safety – Developing the Conceptual Framework.” Ergonomics 58 (4): 548–564. doi:10.1080/00140139.2015.1015623.
- Devers, K. 1999. “Qualitative Research When We See It? Beginning the Dialogue in Health Services Research Terms.” Health Services Research 34 (5): 1153–1188.
- Graneheim, U.H., B.M. Lindgren, and B. Lundman. 2017. “Methodological Challenges in Qualitative Content Analysis: A Discussion Paper.” Nurse Education Today 56: 29–34. doi:10.1016/j.nedt.2017.06.002.
- Hamel, G., and L. Välikangas. 2003. “The Quest for Resilience.” Harvard Business Review 81 (9): 52–63, 131.
- Hollnagel, E., and D.D. Woods. 2007. Joint Cognitive Systems: Foundations of Cognitive Systems Engineering. Vol. 15. Boca Raton: CRC Press. doi:10.1177/106480460701500208.
- Hybinette, K., K. Pukk Härenstam, and M. Ekstedt. 2021. “A First-line Management Team’s Strategies for Sustaining Resilience in a Specialised Intensive Care Unit-A Qualitative Observational Study.” BMJ Open 11 (3): e040358. doi:10.1136/bmjopen-2020-040358.
- Klein, G., P.J. Feltovich, J.M. Bradshaw, and D.D. Woods. 2005. “Common Ground and Coordination in Joint Activity.” In Organizational Simulation, edited by W.B. Rouse and K.R. Boff, 139–184. New York: John Wiley & Sons, Inc. doi:10.1002/0471739448.ch6.
- Kvale, S. 2009. Den Kvalitativa Forskningsintervjun - Andra Upplagan. 2nd ed. Lund: Studentlitteratur AB.
- Lincoln, Y.S. 1995. “Emerging Criteria for Quality in Qualitative and Interpretive Research.” Qualitative Inquiry 1 (3): 275–289. doi:10.1177/107780049500100301.
- Lundberg, J., and B.J.E. Johansson. 2021. “A Framework for Describing Interaction between Human Operators and Autonomous, Automated, and Manual Control Systems.” Cognition, Technology & Work 23 (3): 381–401. doi:10.1007/s10111-020-00637-w.
- MacKinnon, R.J., D. Slater, K. Pukk-Härenstam, U. von Thiele Schwarz, and T. Stenfors. 2022. “Adaptations to Practice and Resilience in a Paediatric Major Trauma Centre during a Mass Casualty Incident.” British Journal of Anaesthesia 128 (2): e120–e126. doi:10.1016/j.bja.2021.07.024.
- Mahajan, A., S.D. Islam, M.J. Schwartz, and M. Cannesson. 2017. “A Hospital Is Not Just a Factory, but a Complex Adaptive system - Implications for Perioperative Care.” Anesthesia and Analgesia 125 (1): 333–341. doi:10.1213/ANE.0000000000002144.
- Mazzocato, P., J. Thor, U. Bäckman, M. Brommels, J. Carlsson, F. Jonsson, M. Hagmar, and C. Savage. 2014. “Complexity Complicates Lean: Lessons from Seven Emergency Services.” Journal of Health Organization and Management 28 (2): 266–288. doi:10.1108/JHOM-03-2013-0060.
- McDonald, S., and B. Simpson. 2014. “Shadowing Research in Organizations: The Methodological Debates.” Qualitative Research in Organizations and Management: An International Journal 9 (1): 3–20. doi:10.1108/QROM-02-2014-1204.
- Meier, M. 1998. “Architecting Principles for Systems of Systems.” Systems Engineering 1 (4): 267–284.
- Mumford, E. 2006. “The Story of Socio-Technical Design: Reflections on Its Successes, Failures and Potential.” Information Systems Journal 16 (4): 317–342. doi:10.1111/j.1365-2575.2006.00221.x.
- Nemeth, C., R. Cook, and D. Woods. 2004. “The Messy Details: Insights from Technical Work in Healthcare.” In Special Issue on Studies in Healthcare Technical Work. IEEE Transactions on Systems, Man, and Cybernetics - Part A: Systems and Humans, edited by C. Nemeth, R. Cook, and D. Woods, 6th ed., Vol. 34, 689–692. Los Angeles: Human Factors and Ergonomics Society. doi:10.1109/TSMCA.2004.836802.
- Nugus, P., A. Holdgate, M. Fry, R. Forero, S. McCarthy, and J. Braithwaite. 2011. “Work Pressure and Patient Flow Management in the Emergency Department: Findings from an Ethnographic Study.” Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine 18 (10): 1045–1052. doi:10.1111/j.1553-2712.2011.01171.x.
- Patton, M.Q. 2014. Qualitative Research & Evaluation Methods: Integrating Theory and Practice. United Kingdom: SAGE Publications.
- Plsek, P.E., and T. Greenhalgh. 2001. “Complexity Science: The Challenge of Complexity in Health Care.” BMJ (Clinical Research ed.) 323 (7313): 625–628. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1121189/pdf/625.pdf%0Ahttp://www.ncbi.nlm.nih.gov/pubmed/11557716.
- Praetorius, G., E. Hollnagel, and J. Dahlman. 2015. “Modelling Vessel Traffic Service to Understand Resilience in Everyday Operations.” Reliability Engineering & System Safety 141: 10–21. doi:10.1016/j.ress.2015.03.020.
- Reiman, T., C. Rollenhagen, E. Pietikäinen, and J. Heikkilä. 2015. “Principles of Adaptive Management in Complex Safety-critical Organizations.” Safety Science 71 (PB): 80–92. doi:10.1016/j.ssci.2014.07.021.
- Roth, E.M., and E.S. Patterson. 2005. “Using Observational Study as a Tool for Discovery: Uncovering Cognitive and Collaborative Demands and Adaptive Strategies.” In How Professionals Make Decision. Volume 5, edited by B.B. Henry Montgomery and Raanan Lipshitz, 5th ed., 379–393.Boca Raton: CRC Press.
- Rouse, W. 2008. “Health Care as a Complex Adaptive System: implications for Design and Management.” Bridge-Washington-National Academy of Engineering 38 (1): 17.
- Saghafian, S., G. Austin, and S.J. Traub. 2015. “Operations Research/Management Contributions to Emergency Department Patient Flow Optimization: Review and Research Prospects.” IIE Transactions on Healthcare Systems Engineering 5 (2): 101–123. doi:10.1080/19488300.2015.1017676.
- Shannon, S.E., and H.-F. Hsieh. 2005. “Three Approaches to Qualitative Content Analysis.” Qualitative Health Research 15 (9): 1277–1288. doi:10.1177/1049732305276687.
- Smith, P.J., and R.R. Hoffman. 2017. “The evolution and maturation of CSE.” In Cognitive Systems Engineering: The Future for a Changing World, edited by P. J. Smith,and R.R.Hoffman, 3–53. Boca Raton: CRC Press. doi:10.1201/9781315572529.
- Son, C., F. Sasangohar, J. Moon, M.S. Mannan, S.C. Peres, and T.J. Neville. 2018. “Journal of Loss Prevention in the Process Industries Modeling an Incident Management Team as a Joint Cognitive System.” Journal of Loss Prevention in the Process Industries 56 (July): 231–241. doi:10.1016/j.jlp.2018.07.021.
- Spradley, J.P. 1980. Participant Observation. USA: Waveland Press, Inc.
- Tong, A., P. Sainsbury, and J. Craig. 2007. “Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups.” International Journal for Quality in Health Care: Journal of the International Society for Quality in Health Care 19 (6): 349–357. doi:10.1093/intqhc/mzm042.
- Villa, S., A. Prenestini, and I. Giusepi. 2014. “A Framework to Analyze Hospital-Wide Patient Flow Logistics: Evidence from an Italian Comparative Study.” Health Policy 115 (2–3): 196–205. doi:10.1016/j.healthpol.2013.12.010.
- Weaver, S., X. Che, L. Petersen, and S. Hysong. 2018. “Unpacking Care Coordination through a Multiteam System Lens: A Conceptual Framework and Systematic Review.” Medical Care 56 (3): 247–259. doi:10.1097/MLR.0000000000000874.
- Winasti, W., S. Elkhuizen, L. Berrevoets, G. van Merode, and H. Berden. 2018. “Inpatient Flow Management: A Systematic Review.” International Journal of Health Care Quality Assurance 31 (7): 718–734. doi:10.1108/IJHCQA-03-2017-0054.
