Abstract
Aim
The clinical relevance of small right-to-left shunt (RLS) in young patients with cryptogenic stroke is unknown. We aimed to analyze and understand the relationship between cryptogenic stroke and small RLS by studying specific cases.
Materials and methods
Clinical data from two cases of small RLS-related cryptogenic stroke in young patients were collected prospectively and analyzed. We followed up the patients for >1 year after discharge.
Results
Case 1. A 50-year-old man was admitted for slurred speech and right hemiplegia and was diagnosed with acute cerebral infarction. Contrast-enhanced transcranial Doppler (c-TCD) and contrast-enhanced transthoracic echocardiography (c-TTE) revealed a microbubble and 20–30 microbubbles per section, respectively, in the resting state. Three months later, he was readmitted for stroke recurrence. Transesophageal echocardiography (TEE) confirmed a patent foramen ovale (PFO), and he underwent transcatheter closure of the PFO. Case 2. A 48-year-old man was admitted for right hemiplegia with slurred speech. Brain magnetic resonance imaging showed acute cerebral infarction. c-TCD and contrast-enhanced TEE (c-TEE) revealed <10 microbubbles and approximately 20 microbubbles per section, respectively. These findings suggested a PFO. Two months later, he was readmitted for stroke recurrence. He underwent transcatheter closure of the PFO. Follow-up of cases 1 and 2 at >1 and >1.5 years after discharge, respectively, showed no stroke recurrence.
Conclusion
We suspected that a small RLS may cause cryptogenic stroke. A small RLS in c-TCD in stroke patients may not be actually small, and c-TEE/c-TTE may be valuable in finding larger RLSs.
Introduction
Paradoxical thrombotic embolism via cardiac right-to-left shunts (RLSs) is a known cause of cryptogenic stroke in young patients [Citation1]. An RLS representing a patent foramen ovale (PFO) is usually a remnant of embryological development, and it is clinically important, particularly in paradoxical brain embolism and other conditions [Citation2]. Contrast-enhanced transcranial Doppler sonography (c-TCD) is an attractive alternative in the identification of RLS. However, the clinical relevance of small RLS in young patients with cryptogenic stroke is unknown. This report of two cases aimed to provide a deeper understanding of this condition.
Case reports
Case 1
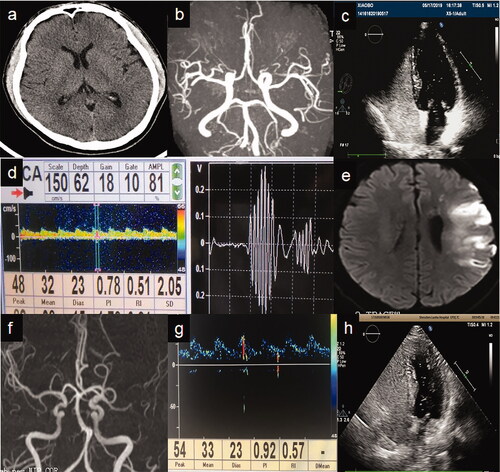
A 50-year-old man was admitted to the hospital for sudden slurred speech and right hemiplegia for 3.5 h in February 2019. He had no relevant family history or any personal history of chronic disease, infectious disease, operation, major trauma or blood transfusion. He was a smoker (30 cigarettes/day) for 30 years. Head computed tomography (CT) performed in the emergency department revealed no obvious abnormality (). Red blood cell count, white blood cell count, C-reactive protein (CRP), coagulation function and blood electrolyte were within normal limits. Physical examination on arrival revealed a body temperature of 36.8 °C, blood pressure of 138/85 mmHg, clear consciousness, motor aphasia, right central facial palsy and decreased superficial sense of the right face and limbs. Muscle strength on the right upper and lower limbs was determined as 4/5. There were no other obvious positive neurological signs. The National Institutes of Health Stroke Scale (NIHSS) score was 6. Intravenous thrombolysis with recombinant tissue plasminogen activator was performed immediately; after which, the patient’s motor and sensory disorders improved remarkably and NIHSS score decreased to 3. The results of the laboratory analysis, urine and faecal analysis and faecal occult blood test were normal. Uric acid (480 µmol/L), total cholesterol (5.41 mmol/L) and triglyceride (3.42 mmol/L) levels increased, and thyroxine (59.80 nmol/L) and fibrinogen (1.05 g/L) levels decreased. Thrombin time (29.4 s) increased. Serum bilirubin, serum creatinine, fasting blood glucose, glycosylated haemoglobin and serum homocysteine levels were all normal. The patient was negative for syphilis and human immunodeficiency virus antibodies. Echocardiography revealed decreased left ventricular diastolic function. Colour Doppler ultrasound of the carotid artery, vertebral artery and subclavian artery showed no obvious abnormality. Colour Doppler ultrasound of arteries and veins of the lower limbs showed plaque formation on the right common femoral artery. Chest CT revealed emphysema in the upper lobe of both lungs with multiple bullae. Ophthalmoscope examination revealed no obvious bleeding or infiltration in the bilateral fundus. Twenty-four-hour dynamic electrocardiogram monitoring showed no obvious abnormality. c-TCD (Delica Medical Equipment Co., Ltd, Shenzhen, China) revealed that a microbubble overflowed in the resting state (), and there was no increase after Valsalva manoeuver (VM). Contrast-enhanced transthoracic echocardiography (c-TTE) revealed 20–30 microbubbles per section in the resting state in the left atrium at the second cardiac cycle (), which suggested the presence of a PFO. He was given aspirin (antiplatelet), atorvastatin calcium (hypolipidemic), edaravone (oxygen free radical scavenger), vinpocetine (to improve cerebral circulation) and oxiracetam (to improve cerebral metabolism) for 7 days. Physical examination showed shallow forehead wrinkles and 4/5 muscle strength of the right lower extremity (NIHSS score, 2). He was diagnosed with acute cerebral infarction. He was discharged 7 days after hospitalisation. Three months after discharge, he was readmitted for sudden right hemiplegia with slurred speech for 2 days. Emergency head CT revealed no obvious abnormality. He was again diagnosed with acute cerebral infarction and was treated with medications to counter platelet aggregation, lower cholesterol, eliminate oxygen free radicals and improve cerebral circulation. His symptoms improved rapidly after 5 days of treatment. Further auxiliary inspection revealed normal prostate-specific antigen and alpha-fetaprotein levels. The carcinoembryonic antigen level (5.80 ng/mL) was slightly increased. Thromboelastogram revealed no obvious abnormality. Transesophageal echocardiography (TEE) revealed colour Doppler flow (1.4 mm wide) into the right atrium in the atrial septum, suggesting PFO. He underwent transcatheter closure of the PFO 2 months after the onset of the second stroke. Postoperative follow-up after >1 year showed no stroke recurrence.
Figure 1. Patient 1. (a) Emergency head computed tomography before intravenous thrombolysis showing no obvious abnormality. (b) Brain magnetic resonance angiography (MRA) showing no obvious abnormality. (c) Contrast-enhanced transcranial Doppler (c-TCD) showing a signal of a microbubble that overflowed in the resting state. (d) Contrast-enhanced transthoracic echocardiography showing 20–30 microbubbles per section in the resting state in the left atrium at the second cardiac cycle. Patient 2. (e) Diffusion-weighted imaging sequence showing an acute infarction in the left temporal lobe and frontotemporal junction. (f) MRA showing severe stenosis of the M2 segment of the left middle cerebral artery (MCA), which had sparse distal branches. (g) c-TCD showing a small amount of microbubbles in the resting state. (h) Contrast-enhanced transesophageal ultrasound showing approximately 20 microbubbles per section per frame.
Case 2
A 48-year-old man was admitted to the hospital for right limb weakness with slurred speech lasting for a day in April 2018. He had cerebral infarction 5 years previously, which lead to memory decline. He had no relevant family history or any personal history of chronic disease, operation or major trauma. Emergency head CT revealed infarctions in the frontal, temporal and parietal lobes and in the left basal ganglia. The electrocardiogram result was normal. The patient’s blood glucose, red blood cell count, white blood cell count, coagulation function and blood electrolyte levels were within normal limits. Physical examination on admission revealed blood pressure of 153/95 mmHg, clear consciousness, motor aphasia, right-sided central facial palsy, and dysphagia. Muscle strength on the right upper and lower limbs was 3/5. No other obvious positive neurological signs were found. Laboratory analysis, fasting blood glucose, glycosylated haemoglobin, CRP, free thyroxine and thyroid-stimulating hormone levels showed normal results. The patient was negative for anti-nuclear, autoimmune vasculitis, thyroid, syphilis and human immunodeficiency virus antibodies. Activated partial thromboplastin time (19.4 s) and prothrombin activity (122%) increased. Ferritin (459.20 ng/mL), total bilirubin (43.3 µmol/L), direct bilirubin (6.9 µmol/L), indirect bilirubin (36.4 µmol/L), creatine kinase isoenzyme (35 U/L) and homocysteine (32 µmol/L) levels increased. Thromboelastogram revealed no obvious abnormality. Twenty-four-hour Holter monitoring revealed occasional atrial premature contraction, but there were no remarkable ST–T changes. Chest radiograph revealed enlargement of heart shadow. Colour Doppler ultrasound of the carotid artery, vertebral artery and subclavian artery revealed uneven thickening of the intima-media of the bilateral carotid arteries and formation of atherosclerotic plaque. Colour Doppler ultrasound of bilateral lower extremity veins revealed no thrombus. Brain magnetic resonance imaging revealed acute left frontotemporal junction. Brain magnetic resonance angiography (MRA) revealed severe stenosis of the M2 segment of the left middle cerebral artery (MCA), which had sparse distal branches. c-TCD revealed small RLSs (<10 microbubbles per section). Contrast-enhanced TEE (c-TEE) revealed a PFO with RLS (approximately 20 microbubbles per section per frame). Computed tomography angiography (CTA) of the pulmonary artery revealed no obvious abnormality. CTA of the carotid artery revealed a small atherosclerosis in the C7 segment of the right internal carotid artery. The results of the brain CTA and MRA were the same. He gradually recovered to pre-onset level after 3 weeks of treatment with donepezil (to improve cognitive function), aspirin (antiplatelet), rosuvastatin (hypolipidemic), vinpocetine (to improve cerebral circulation), oxiracetam (to improve cerebral metabolism) and urinary kallidinogenase (to improve cerebral collateral circulation). However, 2 months after the first discharge, he was readmitted for right limb numbness and weakness that lasted for 3 days. Further c-TEE examination revealed 20 microbubbles per section entered the left atrium after VM. He underwent transcatheter closure of the PFO 1 month after the second discharge. Postoperative follow-up after >1.5 years showed no stroke recurrence.
Discussion
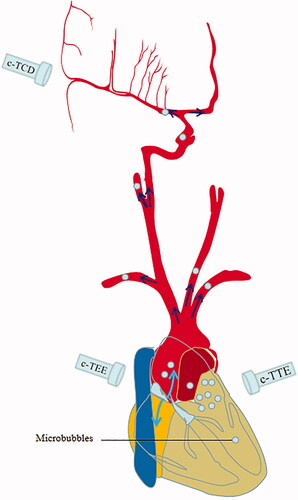
Cryptogenic strokes comprise 30%–40% of all ischaemic strokes [Citation3,Citation4], with a 30% rate of stroke recurrence in the first year. RLS may play a role in cryptogenic strokes. c-TCD can detect RLS in cardiac and extracardiac locations and plays an important role in the diagnosis of cryptogenic stroke. RLS was detected in roughly one-quarter of adult patients [Citation5]. The two patients in this report underwent various examinations and diagnostic tests, which eliminated the common causes of stroke, such as atrial fibrillation, hypercoagulable state, cerebrovascular malformation and so on. In this report, c-TCD of the two patients revealed small [Citation6] RLSs (1–10 microbubbles), but c-TTE/c-TEE revealed moderate to large (>10 microbubbles and no curtain) RLSs; furthermore, both patients had unexplained recurrence of ischaemic stroke in within a very short period, and neither had stroke recurrence in the long-term follow-up after occlusion of the PFO. Therefore, we consider that the small RLSs as revealed by c-TCD may have been the cause of the stroke. The effect of a small RLS in young patients with cryptogenic stroke and its treatment were unknown. One of the indications for occlusion of PFO is acute ischaemic stroke or transient ischaemic attack with moderate to large RLS [Citation7]. Because the MCA or the vertebral artery detected by c-TCD is only a small branch of the aorta (), further examination using c-TTE/c-TEE may reveal moderate to large RLS. Furthermore, many factors affect the results of c-TCD such as patient position (i.e. upright sitting position is superior to supine position [Citation8], MCA recording (i.e. bilateral is superior to unilateral recording), contrast agent (i.e. Echovist-300 is superior to Echovist-200 and agitated saline [Citation5,Citation9,Citation10], quantity of contrast agent (i.e. 10 mL is superior to 5, 2.5 and 1.2 mL), provocation manoeuver (i.e. conventional VM is superior to coughing and standardized VM), VM timing (i.e. 5 s of VM starting at 5 s after the beginning of injection [Citation9,Citation11], diagnostic time window (i.e. 40 s after the beginning of injection [Citation9], number of tests [Citation9,Citation11] (i.e. two c-TCD tests are superior to single c-TCD test [Citation10]), number of occasions for bubbles to enter a possible shunt, sensitivity of the TCD device to detect microbubbles [Citation5], body size [Citation12], size of the PFO and so on. Careful treatment of small RLS in young and middle-aged patients with cryptogenic stroke is important. The contrast agent for C-TCD, c-TEE and c-TTE used in this study was agitated saline mixed with blood, and the procedure of making the contrast medium and of the VM was based on the clear and fixed instructions. All c-TCD, C-TTE and c-TEE results were examined by a single operator in this study.
Figure 2. Sketch maps for different inspection effects of contrast-enhanced transcranial Doppler, transesophageal ultrasound, and transthoracic echocardiography (c-TCD, c-TEE and c-TTE, respectively). The middle cerebral artery detected by c-TCD is only a small branch of the aorta, and c-TTE/c-TEE may reveal more right-to-left shunts (more microbubbles) in the left atrium.
This case series is important because it provides information that can help in determining the aetiology of cryptogenic stroke in patients with small RLS. Furthermore, it shows the importance of further examination and follow-up of patients with small RLS.
However, this study has some limitations. Although many examinations and diagnostics tests were performed to determine the causes of stroke in this case series, some may have been omitted and small RLS may be just a bystander. Large sample, comparison, multi-central research is needed in this respect. The patients still need further follow-up to observe for any recurrence of stroke after occlusion of the PFO.
Based on the characteristics of the two cases of cryptogenic stroke and after eliminating technical reasons such as VM, contrast agent, etc., we suspected that a small RLS may cause cryptogenic stroke which should be highly valued. However, a small RLS in c-TCD in stroke patients may not be actually small, and c-TEE/c-TTE may be valuable in finding larger RLSs. The small RLS in c-TCD in stroke patients may be not a real small quantity, and c-TEE/c-TTE may find a larger RLS, and we suspected that small RLS in c-TCD may cause cryptogenic stroke, which should be highly valued.
Ethics approval and consent to participate
The study design was approved by the ethics review board of the 3rd Affiliated Hospital of Shenzhen University (No. 2019-SZLH-LW-006).
The patient provided written informed consent.
Acknowledgements
Not applicable.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
References
- Ward R, Jones D, Haponik EF. Paradoxical embolism. An underrecognized problem. Chest. 1995;108(2):549–558.
- Horton SC, Bunch TJ. Patent foramen ovale and stroke. Mayo Clin Proc. 2004;79(1):79–88.
- Bang OY, Lee PH, Joo SY, et al. Frequency and mechanisms of stroke recurrence after cryptogenic stroke. Ann Neurol. 2003;54(2):227–234.
- Sacco RL, Ellenberg JH, Mohr JP, et al. Infarcts of undetermined cause: the NINCDS Stroke Data Bank. Ann Neurol. 1989;25(4):382–390.
- Droste DW, Kriete JU, Stypmann J, et al. Contrast transcranial doppler ultrasound in the detection of right-to-left shunts comparison of different procedures and different contrast agents. Stroke. 1999;30(9):1827–1832.
- Jauss M, Zanette E. Detection of right-to-left shunt with ultrasound contrast agent and transcranial doppler sonography. Cerebrovasc Dis. 2000;10(6):490–496.
- Zhang Y, Zhu X, Jiang S, et al. Recommendations from Chinese experts on management of patients with patent foramen ovale. Heart J. 2015; 27:373–379.
- Lao AY, Sharma VK, Tsivgoulis G, et al. Effect of body positioning during transcranial Doppler detection of right-to-left Shunts. Eur J Neurol. 2007;14(9):1035–1039.
- Droste DW, Jekentaite R, Stypmann J, et al. Contrast transcranial doppler ultrasound in the detection of right-to-left shunts: comparison of Echovist®-200 and Echovist®-300, timing of the Valsalva maneuver, and general recommendations for the performance of the test. Cerebrovasc Dis. 2002;13(4):235–241.
- Droste DW, Reisener M, Kemény V, et al. Contrast transcranial doppler ultrasound in the detection of right-to-left shunts reproducibility, comparison of 2 agents, and distribution of microemboli. Stroke. 1999;30(5):1014–1018.
- Droste DW, Silling K, Stypmann J, et al. Contrast transcranial Doppler ultrasound in the detection of right-to-left shunts: time window and threshold in microbubble numbers. Stroke. 2000;31(7):1640–1645.
- Iguchi Y, Kimura K, Kobayashi K, et al. Detection of right-to-left shunts may be associated with body size. J Neuroimag. 2010;20(2):130–133.
