Everyone is aware that antibiotic resistance is a major clinical, and economic, problem. Recent publications have foretold huge costs and clinical disasters if we do not better manage the tools we have.[Citation1–Citation4] Strangely, we continue to prescribe antibiotics poorly. By that, I refer to an adage from the grandfather of antimicrobial chemotherapy, Paul Ehrlich. Over a century ago, he predicted that unless we optimally use these drugs the ‘enemy’ will render them useless. He advocated ‘frappe fort et frappe vite’ which roughly translated means using the most powerful, yet safe, agent at the shortest optimal dose to eradicate all the less susceptible isolates.[Citation5] In addition to this lack of application of pharmacodynamics science, at the empirical level, we infrequently seem to use resistance data guide our choices. Nationally, there may be susceptibility data, but in the local data for the key bacteria such as Streptococcus pneumoniae, Haemophilus influenzae, and Escherichia coli, there is either a paucity of data or it is not disseminated broadly enough Add to this challenge, almost 30 million Americans [Citation6] travelled abroad in 2015 as well as over 1.5 billion person trips within the US,[Citation7] thus potentially exposing some patients to more resistant pathogens.
As prescribers, we are trained to think about drug resistance and other risk factors, but travel or location at which infection occurred is such an easily recognizable parameter that it should be used to help prescribe with less empiricism.
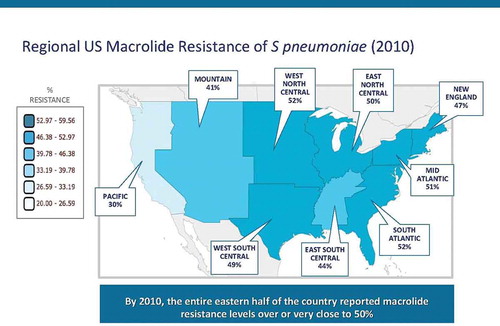
Presently in the United States, there are no national surveillance programs for the most common pathogens across most states, let alone all 48 contiguous states. For 20 years, Centers for Disease Control and Prevention (CDC) has organized the ABCS program, which focuses on nine representative States for invasive isolates,[Citation8] but the program does not ‘drill down’ for noninvasive species. Yet, it is these organisms that cause the bulk of infections. Recent data have demonstrated the steady decline in susceptibility of key pathogens such as S. pneumoniae [Citation9] even over a four-year period in the United States. Susceptibility among S. pneumoniae isolates to penicillin has decreased to 33.1%, erythromycin (also azithromycin) 38.4%, tetracycline 66.2%, and trimethoprim-sulfamethoxazole 57.0%. In addition, there are clear regional differences in resistance patterns, which should help prescribers assess the possible risk of bacterial susceptibility and the best empirical options. The map of the United States illustrates the widely ranging incidence of antibiotic resistant strains of S. pneumoniae by CDC census region with the South East of the country showing macrolide resistance as high as 60% with a national average around 50% () [Citation10]. Thus, Floridians or recent visitors to the ‘sunshine state’ maybe infected with resistant strains of pneumococci. Clearly not every resistant infection is going to be a clinical failure, but the odds of an unsuccessful outcome are likely higher. Indeed, in today’s electronic era, we should be able to follow a patient’s journey after their antibiotic prescription and ascertain such outcomes; however, the lack of quality specimens and the ability to tie drug therapy to outcome may still be a stretch.
Figure 1. Distribution of macrolide resistant Streptococcus pneumoniae in USA. Adapted from The Center for Disease Dynamics, Economics and Policy website (http://www.cddep.org/projects/resistance_map/macrolide_resistant_streptococcus_pneumoniae#sthash.RoFaPhmK.dpbs). Accessed May 27, 2015.
Globally the picture is even more worrying. Groups such as ANSORP in Asia [Citation11] and ECDC [Citation12] in Europe have collected contemporary strains of significant species and shown trends, which suggest that some drug classes may be ineffective in infections commonly presented in offices and hospitals in the United States. Additionally, it is so easy now to travel from a location to the United States while ‘incubating’ an infection acquired in a foreign place. An excellent example of this is the extended spectrum B lactamase Enterobacteriaceae such as Klebsiella pneumoniae, which translocated with ease from India to the United Kingdom and Europe.[Citation13] It takes less than 24 hours to travel 9,000 miles. Similarly, air travel within the United States enables a patient to fly from Miami to Seattle in 6–7 hours and thus could have acquired their infection in the sunshine but presented with a likely resistant organism in Washington State. As we begin to diagnose a patient who presents with a possible infection, of which respiratory infections are the most common, we should integrate ‘have you travelled recently, if so where?’
We can recall the risk factors defined over 15 years ago for recognition of drug-resistant Streptococcus pneumoniae [Citation14] (), perhaps it is now time to add ‘where in the world’ questions to our diagnostic algorithms?
Table 1. Risk factors for drug-resistant Streptococcus pneumoniae.
Awareness is important if one is to avoid misguided empiricism.
Declaration of interests
G Tillotson is an employee of Cempra Pharmaceuticals. The author has no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
References
- World Health Organisation. Antibiotic resistance: a multi-country public awareness survey. Geneva: World Health Organisation; 2015.
- Review on Antimicrobial Resistance. Antimicrobial Resistance: tackling a crisis for the health and wealth of nations. London: Department of Health UK Government. [cited 2016 Mar 11]. Available from: http://amr-review.org/sites/default/files/AMR%20Review%20Paper%20-%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf.
- Antibiotic Resistance. Atlanta (GA): CDC. [cited 2016 Mar 11]. Available from: http://www.cdc.gov/drugresistance/about.html.
- Teillant A, Gandra S, Barter D, et al. Potential burden of antibiotic resistance on surgery and cancer chemotherapy antibiotic prophylaxis in the USA: a literature review and modelling study. Lancet Infect Dis. 2015 Dec;15(12):1429–1437.
- Ehrlich P. Address in pathology, on chemotherapy: delivered before the seventeenth international congress of medicine. Br Med J. 1913 Aug 16;2(2746):353–359.
- US Government Data. [cited 2016 Mar 11]. Available from: http://travel.trade.gov/view/m-2015-O-001/index.html.
- US Travel Association. [cited 2016 Mar]. Available from: https://www.ustravel.org/answersheet.
- Langley G, Schaffner W, Farley MM, et al. Twenty years of active bacterial core surveillance [Internet]. Emerging Infectious Diseases. 2015;21(9). [cited 2016 Mar]. Available from: http://wwwnc.cdc.gov/eid/article/21/9/pdfs/14-1333.pdf.
- Flamm R, Rhomberg P, Huband M, et al. Activity of omadacycline tested against Streptococcus pneumoniae isolates from a global surveillance program (2014). ICAAC. 2015 Abstract C554.
- CDDEP. Washington (DC): CDDEP. [cited 2016 Mar]. Available from: http://resistancemap.cddep.org/.
- Song J-H, Lee NY, Ichiyama S, The ANSORP Study Group. Spread of drug-resistant streptococcus pneumoniae in Asian countries: Asian network for surveillance of resistant pathogens (ANSORP) study. Clin Infect Dis. 1999;28(6):1206–1211.
- European Centres for Disease Control. [cited 2016 Mar]. Available from: http://ecdc.europa.eu/en/press/news/_layouts/forms/News_DispForm.aspx?List=8db7286c%2Dfe2d%2D476c%2D9133%2D18ff4cb1b568&ID=1358&ContentTypeId=0x010082EE625D0C434588A3E95C31FC12D7A70104000C92BA0F0E932049B9C0FB633C874119.
- Doi Y, Paterson DL. Carbapenemase-producing enterobacteriaceae. Semin Respir Crit Care Med. 2015 Feb;36(1):74–84.
- Campbell GD, Silberman R. Drug resistant Streptococcus pneumoniae. Clin Inf Dis. 1998;26:1188–1195.
