ABSTRACT
Generalized pustular psoriasis (GPP) is a rare chronic inflammatory skin disease that can lead to life-threatening complications and require emergency medical treatment. Recurrent GPP flares are characterized by the sudden onset of widespread erythematous skin rash with sterile pustules, at times associated with fever, chills, general malaise, and other systemic inflammatory manifestations. Systemic complications such as cardiorespiratory failure, infections, and sepsis are potentially life-threatening and can result in an emergency department visit and/or hospitalization. Acute GPP episodes can be difficult to recognize and diagnose. The low incidence of the disease, its relapsing nature, the unpredictability of flare onset, and the lack of standardized diagnostic criteria are major obstacles to achieving rapid recognition and diagnosis in both the emergency department and the hospital setting.
There is scarce evidence supporting the efficacy and safety of treatments commonly used for GPP; consequently, there is an unmet need for therapies that specifically target the condition. Our aim is to present a multidisciplinary approach to GPP to achieve a rapid diagnosis ensuring that the patient receives the most appropriate treatment for their pathology. The main recommendation for primary care and emergency physicians is to contact a dermatologist immediately for advice or to refer the patient when GPP or a flare is suspected.
Plain Language Summary
Generalized pustular psoriasis (GPP) is a rare and serious skin disease that can cause life-threatening complications and require urgent medical treatment. When someone has a flare-up of GPP, their skin suddenly becomes red and covered with pus-filled bumps not caused by infection. They may also experience fever and chills and feel generally unwell. These flares can be very difficult to diagnose and lead to serious complications such as infections and organ failure, which may require a visit to the emergency department and/or admission to hospital. The diagnosis of GPP can be challenging as it is a rare and unpredictable disease with different types of flare-ups, making it difficult to identify in the emergency department and the hospital. This article shows that the best recommendation for primary care and emergency doctors is to improve their knowledge of this rare condition. Primary care and emergency doctors should immediately contact a dermatologist for advice or referral if they suspect that a patient has GPP or a flare-up of the disease. An approach involving doctors from different specialties can help ensure that patients receive the appropriate and timely care they need.
1. Introduction
Pustular psoriasis is a rare type of chronic psoriasis with sterile pustules that can be either localized or generalized [Citation1–3]. Classically recognized subtypes of pustular psoriasis include generalized pustular psoriasis (GPP), palmoplantar pustular psoriasis, and acrodermatitis continua of Hallopeau [Citation1–4]. The main characteristic of GPP is the eruption of painful sterile pustules all over the body surface, sometimes together with systemic inflammatory symptoms [Citation4–8]. The clinical course of GPP is heterogeneous, with relapsing or persistent flares.
GPP can present with symptoms other than cutaneous symptoms. These may require urgent assessment, immediate consultation with a dermatologist, and even admission to the intensive care unit [Citation1–4]. Extracutaneous symptoms of GPP include fever, leukocytosis, general malaise, and multiple organ involvement [Citation5–8]. GPP flares can prove fatal owing to severe complications such as systemic infections, sepsis, and renal, respiratory, and cardiovascular involvement requiring hospitalization [Citation9–14].
GPP is considered an auto-inflammatory disease and is associated to an irregular innate immune response [Citation3,Citation5,Citation6]. Recent findings on GPP pathogenesis showed that interleukin (IL) 36 pathway plays a central pathogenetic role and the mutation of the IL-36 receptor (IL36RN) is associated with severe presentations of the disease [Citation5–7]. These advances in GPP pathogenesis opened new possibilities for therapeutic targets and recent studies showed that biologic agents that target the IL-36 axis are effective in patients with GPP [Citation5–7].
Despite being a potentially serious condition, the low incidence of the disease, its relapsing nature, the unpredictability of flares, and the lack of standardized diagnostic criteria are significant obstacles to rapid recognition and accurate diagnosis by emergency department and primary care professionals [Citation11–17].
The objective of this review is to update current knowledge on the evaluation and diagnosis of GPP in the primary care setting and the emergency department. Emphasis is placed on practical recommendations for recognizing the disease and seeking advice from a dermatologist in the management of GPP in Spain.
2. Methods
Based on the objectives of our narrative review, we performed a qualitative non-structured search to identify scientific publications on GPP in the PubMed and Embase databases using specific filters (English language, published in the last 5 years) and search terms. The search term ‘generalized pustular psoriasis’ was combined with ‘emergency’, ‘intensive care’, and ‘primary care’ to ensure that the publications found were in line with the objectives of the paper. A flow chart of the search process can be seen in the Supplementary Material annex.
Titles and abstracts of the citations identified in the initial set were screened according to predefined criteria, and potentially relevant articles that met the eligibility criteria were selected for full-text review. Supplementary searches were conducted in PubMed, Embase, and Google Scholar based on the references of selected articles. Additional papers were subsequently added based on the judgment and experience of the authors.
3. What is GPP?
Since GPP was first described by Leopold von Zumbusch in 1910, its characteristics have not been consistently defined, and numerous descriptions and diagnostic criteria have been published [Citation1–9]. According to the diagnostic criteria of an international consensus by the European Rare and Severe Psoriasis Expert Network (ERASPEN) [Citation1], GPP is a chronic and rare form of psoriasis with the following characteristics:
Primary, sterile, macroscopically visible pustules on non-acral skin
Presence or absence of systemic inflammation (fever >38°C and leukocytosis (WBC >12 × 109/L)
Presence or absence of psoriasis vulgaris
Relapsing (>1 episode) or persistent (>3 months)
Current clinical, histological, and genetic evidence indicates that, as a clinical entity, GPP is distinct from plaque psoriasis (psoriasis vulgaris) and requires a specific diagnostic approach [Citation18,Citation19]. GPP can appear with or without systemic inflammation. The course of the disease is identified as relapsing (more than 1 episode) or persistent (symptoms lasting more than 3 months) [Citation1]. The nature of flares is unpredictable and heterogeneous, and the disease can manifest in a number of ways, ranging from a single pustule to a life-threatening condition ().
Figure 1. The life-threatening nature of GPP flares is illustrated by this 18-year-old woman with relapsing GPP, who presented with a severe flare. This progressed to sepsis with massive pulmonary involvement, resulting in the death. (image on the right side is reproduced from Romiti et al. Anais Brasileiros de dermatologia 2022;97:63–74. Published under CCBY license https://creativecommons.org/licenses/by/4.0/; left image provided with permission, courtesy of Professor Ricardo Romiti (University of São Paulo, Brazil).
GPP usually affects adults, peaking in the fifth decade of life. Studies have shown a higher prevalence in women than in men, although some series show a similar prevalence for both sexes, with a male:female ratio ranging between 1:1 and 2:1 [Citation1–5,Citation18–20]. The prevalence is greater in Asian than in Caucasian populations (7.46/million in Japan versus 1.76/million in France). In Spain, a recent survey involving 33 dermatologists from 28 different hospitals found that the estimated prevalence in adults was 13.05 cases per million [Citation11]. Data on mortality rates are limited, although ranges of 3% to 7% have been reported [Citation3,Citation10,Citation15–20].
Evidence on the characteristics of GPP in the emergency department is scarce. A retrospective observational cohort study conducted recently by Zema et al [Citation16] concluded that the most common signs and symptoms documented during flares were pain (61% of flare episodes), skin eruption or erythema (46%), and fever (45%). Edema is also frequently recorded. The most common treatments administered during flares were topical corticosteroids (35%), opioids (21%), immunosuppressants (eg, methotrexate, cyclosporine, tacrolimus; 13%), and oral corticosteroids (11%). Compared with patients who do not experience flares, patients with flares had a higher comorbidity burden (including psoriasis and autoimmune conditions), were almost three times more likely to be hospitalized, and were more than twice as likely to visit the emergency department.
A recent cross-sectional study of GPP-related hospital admissions from 2016 to 2020 in Spain conducted by Montero-Vilchez et al [Citation10] showed that in a population of 744 primary diagnoses of GPP, critical care unit admissions were ordered for 6.1% of patients, and 4.8% died; in addition, 23.3% of intensive care admission were readmissions. Patients hospitalized with GPP had a mean age of 62.2 years, and 51.3% were females [Citation10].
Hanna et al [Citation15] recently conducted a retrospective cross-sectional study to analyze the characteristics of hospitalizations and emergency department visits due to GPP in the United States, where 71 GPP-related hospitalizations and 64 GPP-related emergency department visits were reported. The most common commonly used medications during hospitalizations were topical and systemic corticosteroids, non-biologic and biologic immunosuppressants, analgesics, opioids, and antibiotics. The mean length of stay for hospitalizations was 8.6 days (median of 5 days). Three hospitalizations involved an intensive care unit admission, and two proved fatal, illustrating the life-threatening nature of GPP flares [Citation15]. The authors considered that life-threatening complications of GPP should not be underestimated, since appropriate treatment could potentially avoid hospitalizations or reduce the length of hospital stay [Citation15].
4. Disease characteristics
4.1. Pathogenesis
The etiology and pathogenesis of GPP is closely related to those of psoriasis but remain unclear. An inflammatory state in response to a hyperactivation of the innate immune system, in which the interleukin (IL) 36 axis plays a central role, appears to be the main driver of the condition. In GPP skin lesions, the involvement of IL-36 has been shown by the identification of loss-of-function mutations in the IL-36 receptor antagonist gene (IL36RN) and the overexpression of IL-36 cytokines [Citation5,Citation21,Citation22]. Mutations of the CARD 14, AP1S3 and SERPINA 3 genes have also been associated to the pathogenesis of GPP. CARD14 provides instructions for synthetizing CARD 14 protein, a protein particularly abundant in the skin that activates the nuclear factor-kappa-B (NF-κB) protein complex and play important roles in regulating inflammatory reactions in the skin. AP1S3 encodes a subunit of the adaptor protein complex 1 (AP-1), a keratinocyte adaptor protein, while SERPINA3 encodes alpha-1-antichymotrypsin (ACT), an inhibitor of cathepsin G, a proteolytic enzyme that belongs to the neutrophil serine proteases family [Citation5,Citation6,Citation21,Citation22].
4.2. Comorbidities and triggers
The most common comorbidities and triggers of GPP reported in the context of GPP-related hospitalizations appear in [Citation2–4,Citation14–16,Citation23–29].
Table 1. Most common comorbidities and triggers associated with a GPP-related hospitalization. [Citation2–4, Citation14–16].
Potential triggers of GPP flares include initiation or withdrawal of medications, especially sudden withdrawal of systemic corticosteroids (), acute infections, stress, and pregnancy [Citation15–18,Citation21–26]. GPP is also associated with skin disease, such as inflammatory skin conditions, skin and subcutaneous tissue infections, cellulitis, plaque psoriasis, psoriatic arthritis, and contact dermatitis.
Figure 2. Sudden withdrawal of corticosteroids and other systemic therapies triggering GPP flares. A 52-year-old man with long-standing, ongoing psoriasis stopped retinoid treatment and started to apply topical corticosteroids periodically without consulting his clinician. The patient was admitted to hospital at the onset of a GPP flare. (images provided with permission, courtesy of Professor Aikaterini Patsatsi (Aristotle University School of Medicine, Thessaloniki, Greece).
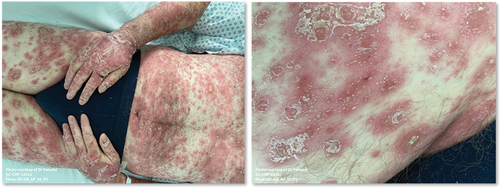
Considering that various types of drugs have been found to trigger GPP flares, a comprehensive medication history should be taken. For example, GPP flares can be triggered by rapid tapering or sudden withdrawal of vaccines, cyclosporine, lithium, beta-blockers, and anti-malarial drugs [Citation2–4,Citation15,Citation16].
Many infections have been associated with GPP flares (eg, streptococcal, cytomegalovirus, fungal, Epstein – Barr virus, varicella zoster virus, and SARS-CoV-2). Although infections can trigger a flare, the characteristic pustules of GPP are sterile. A flare can also be generated or triggered by stress, medical conditions (eg, hypocalcemia and hypoparathyroidism), sun exposure, and pregnancy [Citation1–5,Citation26,Citation27].
5. Clinical evaluation and diagnosis
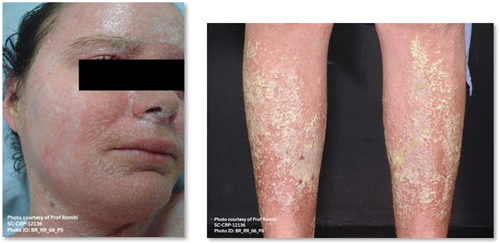
GPP is an under-recognized and misdiagnosed disease, and affected individuals are often not diagnosed for years. () [1–3, 23–24]. The clinical presentation and course of GPP are heterogeneous and unpredictable [Citation1–4,Citation26,Citation27].
Figure 3. A 29-year-old woman with a clinical form of annular GPP and large imprecise areas of sterile pustules with erythema. The patient had a history of psoriasis on the scalp and limbs and recurrent GPP flares. (images reproduced from Choon et al. Experimental dermatology 2023;32:1284–1295. Published under CCBY license https://creativecommons.org/licenses/by/4.0/).

Currently, four clinical subtypes are considered according to the features of the presentation, characteristics of the skin lesions, systemic compromise, and course of the flare [Citation1–9]
Von Zumbusch subtype is the more common, acute (7 days or less) and severe clinical form. It shows a rapid onset of erythematous, inflamed skin with widespread manifestation of macroscopically visible small pustules (2–3 mm). Lesions appear on the trunk and limbs associated to pain, burning and itching. Systemic symptoms such as fever, chills, fatigue, myalgia and arthralgia may appear during the flares.
Annular GPP (Lapière-Millian) shows a subacute course (7 days to 3 months), predominates in childhood, and is characterized by a generalized flare of circinate or serpentine erythematous plaques with peripheral pustules and scaling. Systemic involvement is uncommon.
Chronic acral GPP start with erythematous plaques in acral areas and may progressively spread with time (more than 3 months) to form a generalized pustular flare,
‘Mixed-type GPP’ shows features associated with more than one of the above clinical forms.
In general, GPP is diagnosed based mainly on clinical and histological findings. The main cutaneous features are large ill-defined areas of sterile noninfectious pustules, with surrounding erythema and edema. Previous or concomitant plaque psoriasis can also facilitate the diagnosis of GPP although not all GPP patients have a history of plaque psoriasis [Citation1–4,Citation7–9,Citation13,Citation15–18].
Cutaneous symptoms may include pain, crusts, burning, and itching and be associated or not with systemic symptoms, such as fever, chills, fatigue, loss of appetite, and general malaise. ()
Table 2. Clinical signs and symptoms of GPP comprising the heterogeneous manifestation of the disease.
Symptoms and their severity may vary with each acute episode for a given individual, and flares may appear several times per year or with long inactive intervals between each episode [Citation1–4,Citation7–9,Citation13].
Additionally, mucosal involvement may be found (for example, conjunctivitis, geographic tongue or cheilitis). Extracutaneous manifestations, such as uveitis, jaundice, arthritis, arthralgia or myalgia, can also be observed [Citation1–5,Citation12,Citation13].
Skin biopsies are also necessary to establish a histopathologic diagnosis of GPP. Examination reveals the presence of sterile spongiform pustules of Kogoj resulting from the accumulation of neutrophils beneath the stratum corneum [Citation7–9,Citation23].
5.1. Additional studies
Additional studies may be necessary for assessment of GPP. () Bacterial culture of pustules and/or blood can reveal superinfection. This is important, because in patients attending primary care or the emergency department, GPP is often mistaken for an infection [Citation7–9,Citation23]. Laboratory tests are also helpful when assessing the level of systemic inflammation and possible systemic complications of the disease [Citation6–9]. If the patient presents with fever, tests such as blood culture or procalcitonin should also be requested to rule out sepsis [Citation7–9,Citation23].
Table 3. Additional studies that may be required for assessment of GPP.
5.2. Differential diagnosis
There are many types of generalized pustulosis and various classifications. The descriptions can vary and may not be clear enough for non-dermatologists. Therefore, the most important concept to keep in mind is that it is not necessary to reach a definitive diagnosis in the emergency department, although it is extremely important to contact a dermatologist immediately. Some pustular conditions, for example acute generalized exanthematous pustulosis, are triggered by drugs, which must be discontinued.
Several pustular skin conditions present with similar clinical characteristics and symptoms, highlighting the importance of the differential diagnosis () [Citation1–4,Citation14–17]. Given the burden and risks associated with pustular conditions, the recommendation for primary care and emergency physicians is to consult a dermatologist without delay when a patient presents with any of these conditions [Citation14–17].
Table 4. Differential diagnosis of pustular conditions similar to GPP. For all these pustular conditions and mixed forms, the recommendation is to consult a dermatologist immediately.
6. Approach to the patient with suspected GPP
6.1. Practical recommendations for primary care and emergency physicians
Considering the potentially life-threatening complications of GPP flares, rapid referral to dermatology is essential whenever the condition is suspected. According to Crowley et al, [Citation14] early referral to a dermatologist is mandatory to ensure adequate diagnosis and treatment.
The priority is to assess systemic compromise and stabilize the patient during evaluation by the dermatologist. In addition to dermatology, specialties such as rheumatology, internal medicine, ophthalmology, and others should be involved, depending on the manifestations of the condition.
The decision to admit the patient must be based on the severity of illness, vital sign stability, fluid and electrolyte status, and signs of systemic infection. Supportive skin care measures such as moisturizers and wet wraps may help to relieve cutaneous symptoms in patients with GPP.
It is important to identify and discontinue the drug in cases of drug-induced GPP flare. While systemic corticosteroids can be involved in triggering GPP, they are sometimes used initially as anti-inflammatory agents until diagnosis is confirmed. In these cases, the best way to discontinue systemic corticosteroids is slowly or by maintaining the dose until the disease is controlled, with administration of specific therapies to manage skin disease. Corticosteroids should be withdrawn gradually and after consultation with a dermatologist.
It is also mandatory to rule-out systemic infection or sepsis if the patient has fever and to start empiric antibiotic treatment if these conditions are suspected.
GPP-related hospitalizations are commonly associated with comorbidities and concurrent diagnosis of plaque psoriasis, unspecified inflammatory skin conditions, and infections that may hamper diagnosis and treatment. Hence, it is crucial for primary care physicians to become familiar with the clinical manifestations of GPP, because they are frequently the first medical contact for a GPP patient. Primary care physicians have a vital opportunity to ensure early recognition and appropriate management of patients with GPP [Citation14].
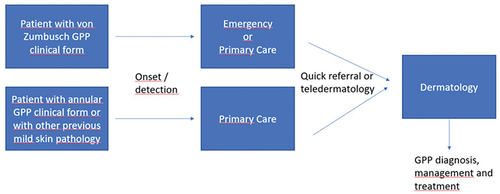
6.2. Care pathway algorithm for patients with GPP
A care pathway algorithm for patients with GPP is presented in . It is advisable to quickly refer patients to dermatology for assessment. Referral to specialized dermatology units is mandatory in difficult or complex cases with indolent progress or a poor initial response.
It is essential to diagnose the patient as soon as possible, and a dermatologist’s expertise is necessary to achieve this goal. When the condition is already diagnosed, the most important step is to treat the patient appropriately and, as soon as possible, with the therapeutic options prescribed by the dermatologist.
Therefore, it is essential to establish rapid communication between the emergency department and the dermatologist, ideally internally, if available, or online to avoid delays. Involving other specialists would depend on the extent of the patient’s systemic compromise.
6.3. Recommendations for referral from primary care to dermatology
The recommendations for referring a patient with suspected GPP from primary care to dermatology are the following:
Presentation of erythema and pustules (with or without suspected diagnosis of GPP)
Once suspected diagnosis of GPP with worsening lesions: refer to dermatology urgently, or consider tele dermatology for rapid access
A patient already diagnosed with GPP who has a worsening skin condition should also be seen immediately by a dermatologist
Patients with pustular lesions on an erythematous base associated with malaise and a poor general condition (fever, asthenia)
6.4. Recommendations for referral from primary care to the emergency department
The recommendations for referral from primary care to the emergency department in patients with systemic and inflammatory symptoms such as fever, malaise, rheumatoid symptoms, or poor general condition should be as follows:
Worsening of previous skin lesions (investigate the history of previously used drugs or treatments that could be related to the worsening of the skin condition in order to discontinue them as soon as possible.).
Patients with pustular lesions on an erythematous base and fever and malaise.
Patients with pustular lesions and extracutaneous manifestations such as arthritis and uveitis.
Hemodynamically unstable patient.
6.5. Recommendations for treatment of a GPP patient in the emergency department
Emergency department physicians should exercise extreme precaution with systemic corticosteroids in the management of GPP or any other form of psoriasis and should not hesitate to contact a dermatologist immediately for guidance and referral.
If the patient is hemodynamically stable, emergency department physicians should communicate with the dermatologist online through telemedicine (when available) so that they will indicate the assessment procedure. On the other hand, if the patient presents with fever, general malaise, or asthenia, he/she must be referred to the hospital emergency department.
Treatment for GPP is usually based on conventional systemic drugs used for plaque psoriasis. Currently, biologic agents and small molecules represent promising therapeutic options for patients with plaque psoriasis or GPP [Citation3,Citation6]. Although many biologics are used in psoriasis management, the only biologic agent approved for GPP is spesolimab, a monoclonal antibody that blocks human IL36R signaling pathway [Citation6].
If a patient with suspected GPP or GPP confirmed by a flare is hospitalized after attending the hospital emergency department and the data indicate a serious condition, then he/she should be monitored constantly.
The recommendations proposed are those followed when a patient is seriously ill and may present hemodynamic instability at any time in an emergency department. ()
Table 5. Recommendations for treatment of a patient with GPP in the emergency department.
7. Unmet needs in the management of GPP
Currently, no treatment or guidelines are available for the management of GPP flares [Citation7]. This is clearly an unmet need in GPP. Spesolimab has been authorized in some countries for the treatment of GPP flares or is under evaluation for approval in others.
Conventional drugs such as retinoids, cyclosporine, and methotrexate were the most commonly used therapies in GPP. In addition, many of the biologics approved for plaque psoriasis have been used to treat patients with GPP, although the evidence that supports the use of these therapies in GPP is flawed and based mostly on small, open-label studies or case reports. The Psoriasis Group of the Spanish Academy of Dermatology and Venereology considers GPP a severe disease that should be managed with systemic treatments [Citation1–3,Citation14,Citation22].
Strober et al [Citation25] presented the results of an international workshop convening 13 leading dermatologists from 10 countries with the goal of identifying challenges for healthcare providers in the management of GPP, including unmet educational needs and clinical practice gaps. Experts agreed that lack of experience in GPP among healthcare providers was an important clinical practice gap. Limited understanding of the clinical characteristics and pathogenesis of GPP leads to misdiagnosis and delayed referral and treatment. When patients visit primary care physicians or the emergency department, GPP is often mistaken for an infection [Citation25].
The most important educational need identified for healthcare professionals is to understand that GPP can be life-threatening if appropriate diagnosis and treatment are delayed () and to recognize when to refer patients to a colleague with more experience in managing GPP [Citation22,Citation25].
8. Conclusions
Knowledge of this rare condition must be improved in primary and emergency care to optimize management of affected patients. Primary care and emergency physicians should be alert to sudden onset of generalized erythematous rash with sterile pustules and establish agile communication channels with dermatology.
The low incidence of GPP makes it difficult for primary care and emergency department physicians to gain adequate experience in the recognition and management of this disease. In addition, GPP-related hospitalizations are commonly associated with comorbidities and concurrent findings of plaque psoriasis, other inflammatory conditions, and infections that may make diagnosis and treatment more challenging. Management of GPP requires a multidisciplinary approach involving dermatologists, rheumatologists, and other healthcare professionals.
Indeed, the main strength of our article is that it is a pioneering multidisciplinary approach for the management of GPP in the emergency room and the primary care setting. On the other hand, our paper has the intrinsic limitations of a narrative review such as non-structured literature search, inappropriate consistency in the evaluation of retrieved articles, and possible bias in the interpretation of findings. Nonetheless, we believe it is useful as an up-to-date reference source for a very specific area of interest. Another limitation is the scarce number of patients in GPP population and that data obtained from a limited number of countries (i.e. Spain, Japan, France and the U.S.A.) may not be extrapolated to all countries and regions.
It is essential for primary care physicians to become familiar with the clinical presentations of GPP, since they are frequently the first medical contact for a GPP patient. The severity of GPP flares and their potential life-threatening consequences should not be underestimated in the emergency department. Primary care physicians are perfectly positioned to ensure a rapid diagnosis and proper treatment of patients with GPP. Primary care and emergency physicians should not hesitate to contact a dermatologist immediately for guidance and referral.
Declaration of financial/other relationships
R Rivera-Diaz has worked as investigator/speaker and/or advisor for: Abbvie, Almirall, AnaptysBio, Boehringer Ingelheim, Bristol Myers Squibb, Janssen, Leo-Pharma, Lilly, Novartis, Pfizer, Novartis, and UCB. JA Heras-Hitos has declared advisory boards/speaker/clinical trial conflicts of interest with Abbvie, Almirall, Boehringer Ingelheim, MSD, Novartis, Reig Jofré and Leo-Pharma. AM Martinez Virto has declared advisory boards/speaker/clinical trial conflicts of interest with Alnylam, Takeda, and Leo-Pharma. AJ Davalos Marin has declared advisory boards/speaker/clinical trial conflicts of interest with Abbvie, Almirall, and Leo-Pharma. MR Senan Sanz has declared advisory boards/speaker/clinical trial conflicts of interest with Almirall, Leo-Pharma, and Boehringer. J-M Carrascosa has declared advisory boards/speaker/clinical trial conflicts of interest with Abbvie, Almirall, Amgen, Boehringer Ingelheim, BMS, Janssen, Leo-Pharma, Lilly, Novartis, and UCB. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed. Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
All authors contributed extensively to the work presented in this paper. All authors have contributed significantly to the conception, design, or acquisition of data, or analysis and interpretation of data. All authors have participated in in drafting, reviewing, and/or revising the manuscript and have approved its submission.
Ethics statement
Patients have provided their informed consent to share the details and images.
Supplemental Material
Download MS Word (15.9 KB)Acknowledgments
Writing assistance was provided by Content Ed Net (Madrid, Spain) with funding from Boehringer Ingelheim.
Supplementary Material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/00325481.2023.2285730
Additional information
Funding
References
- Navarini AA, Burden AD, Capon F, et al.; for the ERASPEN Network. European consensus statement on phenotypes of pustular psoriasis. J EurAcad Dermatol Venereol. 2017;31(11):1792–1799.
- Fujita H, Terui T, Hayama K, et al. Japanese guidelines for the management and treatment of generalized pustular psoriasis: the new pathogenesis and treatment of GPP. J Dermatol. 2018 Nov;45(11):1235–1270. doi: 10.1111/1346-8138.14523
- Megna M, Camela E, Ruggiero A, et al. Use of biological therapies for the management of pustular psoriasis: a New era? Clin Cosmet Investig Dermatol. 2023 Jun 28;16:1677–1690. 10.2147/CCID.S407812
- Fujita H, Gooderham M, Romiti R. Diagnosis of generalized pustular psoriasis. Am J Clin Dermatol. 2022 Jan;23(Suppl 1):31–38. doi: 10.1007/s40257-021-00652-1
- Reynolds KA, Pithadia DJ, Lee EB, et al. Generalized pustular psoriasis: a review of the pathophysiology, clinical manifestations, diagnosis, and treatment. Cutis. 2022 Aug;110(2 Suppl):19–25. doi: 10.12788/cutis.0579
- Baum P, Visvanathan S, Garcet S, et al. Pustular psoriasis: Molecular pathways and effects of spesolimab in generalized pustular psoriasis. J Allergy Clin Immunol. 2022 Apr;149(4):1402–1412. doi: 10.1016/j.jaci.2021.09.035
- Krueger J, Puig L, Thaçi D. Treatment options and goals for patients with generalized pustular psoriasis. Am J Clin Dermatol. 2022 Jan;23(Suppl 1):51–64. doi: 10.1007/s40257-021-00658-9
- Choon SE, Navarini AA, Pinter A. Clinical course and characteristics of generalized pustular psoriasis. Am J Clin Dermatol. 2022 Jan;23(Suppl 1):21–29. doi: 10.1007/s40257-021-00654-z
- Zheng M, Jullien D, Eyerich K. The prevalence and disease characteristics of generalized pustular psoriasis. Am J Clin Dermatol. 2022 Jan;23(Suppl 1):5–12. doi: 10.1007/s40257-021-00664-x
- Montero-Vilchez T, Grau-Perez M, Garcia-Doval I. Epidemiology And geographic distribution of generalized pustular psoriasis in Spain: a national population-based study of hospital admissions from 2016 to 2020. Actas Dermosifiliogr. 2023 Feb;114(2):97–101. doi: 10.1016/j.ad.2022.09.012
- Vilarrasa E, Rivera, R, Eiri N, et al. Approach to the epidemiology, disease management, and current challenges in the management of generalized pustular psoriasis through a survey conducted among Spanish dermatologists. Actas Dermosifiliogr. 2023 Nov 2;S0001–7310(23):00854–2. doi: 10.1016/j.ad.2023.10.022. English, Spanish. Epub ahead of print.
- Bachelez H, Barker J, Burden AD, et al. Generalized pustular psoriasis is a disease distinct from psoriasis vulgaris: evidence and expert opinion. Expert Rev Clin Immunol. 2022 Oct;18(10):1033–1047. doi: 10.1080/1744666X.2022.2116003
- Burden AD, Choon SE, Gottlieb AB, et al. Clinical disease measures in generalized pustular psoriasis. Am J Clin Dermatol. 2022 Jan;23(Suppl 1):39–50. doi: 10.1007/s40257-021-00653-0
- Crowley JJ, Pariser DM, Yamauchi PS. A brief guide to pustular psoriasis for primary care providers. Postgrad Med. 2021 Apr;133(3):330–344. doi: 10.1080/00325481.2020.1831315
- Hanna ML, Singer D, Bender SD, et al. Characteristics of hospitalizations and emergency department visits due to generalized pustular psoriasis in the United States. Curr Med Res Opin. 2021 Oct;37(10):1697–1703. doi: 10.1080/03007995.2021.1951192
- Zema CL, Valdecantos WC, Weiss J, et al. Understanding flares in patients with generalized pustular psoriasis documented in US electronic health records. JAMA Dermatol. 2022 Oct 1;158(10):1142–1148. doi: 10.1001/jamadermatol.2022.3142
- Abo-Tabik M, Parisi R, Morgan C, et al. Global psoriasis atlas. Mapping opportunities for the earlier diagnosis of psoriasis in primary care settings in the UK: results from two matched case-control studies. Br J Gen Pract. 2022 Oct 27;72(724):e834–e841. doi: 10.3399/BJGP.2022.0137
- Ruiz Genao DP, Carretero G, Rivera-Diaz R, et al. BIOBADADERM StudyGroup. Differences in epidemiology, comorbidities and treatment choice between plaque psoriasis and pustular psoriasis: results from the BIOBADADERM registry. Br J Dermatol. 2022 Nov;187(5):817–820. doi: 10.1111/bjd.21763
- Fernández D, Lecaros C. Psoriasis Pustulosa Generalizada. Rev Chilena Dermatol. 2014;30(1):36–45.
- Hoegler KM, John AM, Handler MZ, et al. Generalized pustular psoriasis: a review and update on treatment. J Eur Acad Dermatol Venereol. 2018 Oct;32(10):1645–1651. doi: 10.1111/jdv.14949
- Marrakchi S, Puig L. Pathophysiology of generalized pustular psoriasis. Am J Clin Dermatol. 2022 Jan;23(Suppl 1):13–19. doi: 10.1007/s40257-021-00655-y
- Genovese G, Moltrasio C, Cassano N, et al. Pustular psoriasis: from pathophysiology to treatment. Biomedicines. 2021 Nov 23;9(12):1746. doi: 10.3390/biomedicines9121746
- Strober B, Kotowsky N, Medeiros R, et al. Unmet medical needs in the treatment and management of generalized pustular psoriasis flares: evidence from a survey of corrona registry dermatologists. Dermatol Ther. 2021;11(2):529–541. doi: 10.1007/s13555-021-00493-0
- Reisner DV, Johnsson FD, Kotowsky N, et al. Impact of generalized pustular psoriasis from the perspective of people living with the condition: results of an online survey. Am J Clin Dermatol. 2022 Jan;23(Suppl 1):65–71. doi: 10.1007/s40257-021-00663-y
- Strober B, Leman J, Mockenhaupt M, et al. Unmet educational needs and clinical practice gaps in the management of generalized pustular psoriasis: global perspectives from the front line. Dermatol Ther. 2022 Feb;12(2):381–393. doi: 10.1007/s13555-021-00661-2
- Okubo Y, Kotowsky N, Gao R, et al. Clinical characteristics and health-care resource utilization in patients with generalized pustular psoriasis using real-world evidence from the Japanese medical data center database. J Dermatol. 2021 Nov;48(11):1675–1687. doi: 10.1111/1346-8138.16084
- Kharawala S, Golembesky AK, Bohn RL, et al. The clinical, humanistic, and economic burden of generalized pustular psoriasis: a structured review. Expert Red Clin Immunol. 2020 Mar;16(3):239–252. doi: 10.1080/1744666X.2019.1708193
- Roujeau JC, Bioulac-Sage P, Bourseau C, et al. Acute generalized exanthematous pustulosis. Analysis of 63 cases. Arch Dermatol. 1991 Sep;127(9):1333–1338. doi: 10.1001/archderm.1991.01680080069004
- Creadore A, Desai S, Alloo A, et al. Clinical characteristics, disease course, and outcomes of patients with acute generalized exanthematous pustulosis in the US. JAMA Dermatol. 2022 Feb 1;158(2):176–183. doi: 10.1001/jamadermatol.2021.5390