Abstract
Objective: Routine antibiotic treatment of acute uncomplicated diverticulitis (AUD) has been shown ineffective. In this study, the adherence to a new treatment protocol for uncomplicated diverticulitis was evaluated and the incidence of complications in patients treated with and without antibiotics was investigated.
Materials and methods: A retrospective study of in-patients diagnosed with AUD at Helsingborg Hospital, Sweden between 01 January 2013 and 06 January 2015 was performed. Antibiotics were routinely administrated until 01 May 2014. Thereafter, a new antibiotic-free treatment protocol for uncomplicated diverticulitis was introduced. All the patients were followed regarding complications for minimum one year.
Results: A total of 50 patients were studied after the new protocol implementation and, 60% (n = 31) of the patients were treated without antibiotics. Specialists initiated antibiotic therapy significantly more often than registrars (p=.03). More patients in the antibiotic group had comorbidities (p=.03), apart from that, no significant differences in baseline characteristics were noted between treatment groups. Patients treated with antibiotics after introduction of the new protocol had significantly higher C-reactive protein than patients managed without antibiotics (median 117 mg/L vs. 70, p=.005). The hospital stay was shorter in the non-antibiotic group (three days vs. two days; p=.008). No significant differences in complications were observed.
Conclusions: Protocol compliance was lower than expected, indicating that implementation of new treatment regimens is challenging. This study confirms that complications are rare in AUD treated without antibiotics. However, the selection of the sickest patients to the treatment with antibiotics limits the interpretation of the results.
Keywords:
Introduction
During the twentieth century, the incidence of acute diverticulitis has been rising and so have the treatment costs [Citation1–3]. Acute diverticulitis is classified as uncomplicated or complicated. In uncomplicated disease, inflammation is limited to the wall of the colon and the surrounding tissue in absence of abscesses or perforation of the bowel [Citation4,Citation5]. Standard in-hospital care of acute uncomplicated diverticulitis (AUD) has been antibiotic therapy, bowel rest and intravenous (i.v.) fluids [Citation4,Citation6–9]. Historically, bacteria have been the implied catalysator in addition to prerequisite diverticula but lately AUD has been suggested to originate from mucosa inflammation [Citation10]. Furthermore, antibiotic resistance and adverse effects such as anaphylaxis and Clostridium difficile infections are increasing [Citation11]. Subsequently, the rationale behind AUD treatment with antibiotics has been questioned and recent studies have shown that antibiotics are not mandatory [Citation5,Citation12–16]. Two randomized controlled trials (RCTs) found no difference in recovery or adverse outcomes when omitting antibiotics [Citation12,Citation13]. The Swedish AVOD trial included 623 patients and concluded that antibiotic treatment did not shorten hospital stay nor reduce complication- or recurrence rates in AUD. Accordingly, the recommendation of routine use of antibiotics in AUD has been removed in some [Citation17–19], but far from all international guidelines [Citation7,Citation20–22].
Limited use of antibiotics in AUD may help to decrease antibiotic resistance and antibiotic associated adverse events. Furthermore, it may shorten the hospital stay and lead to lower public costs. In the current study, we present a retrospective before–after analysis of antibiotic therapy vs. treatment with bowel rest and i.v. fluids only in order to analyze the adherence to a new treatment protocol for AUD in our hospital. A secondary objective was to study complications and the recurrence rate.
Materials and methods
This is a retrospective study including consecutive patients admitted to Helsingborg teaching Hospital, Sweden between 01 January 2013 and 06 January 2015 with CT verified AUD. During the first 16 months of the study period, antibiotic therapy during hospitalization was the therapy of choice. In 01 May 2014, a new protocol was introduced stating that patients with suspected AUD should be treated without antibiotics. All physicians working at the emergency or surgical department received an email and oral information about the protocol before it was introduced. The protocol was posted on the internal web page and put in folders at the emergency department and the surgical emergency ward. An e-mail reminder was sent out monthly to all physicians for the whole study period. The two treatment groups were followed for a minimum of 12 months after discharge. The adherence to the new protocol was registered and the number of complications during the time of follow-up was compared between the treatment groups.
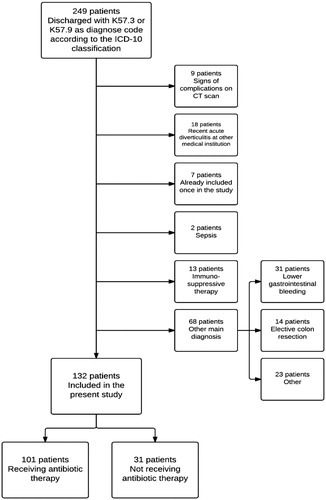
Patients with diverticular disease of the colon (K57.2, K57.3, K57.8 and K57.9 according to the ICD-10 classification) were identified from an in-patient registry of diagnoses. All patients with CT verified AUD identified manually from the patients’ records, were included. Patient was excluded if they had signs of complicated diverticulitis on an abdominal CT (free air, abscess, stenosis) or at clinical examination (sepsis, generalized peritonitis) (). Other exclusion criteria were pregnancy, ongoing immunosuppressive therapy and ongoing antibiotic therapy at admission or treatment for AUD the last month. No patient was included more than once in the study. All data were retrieved retrospectively from patient charts and transferred to a modified case report form (CRF) previously used in the AVOD study (Supplement 1) [Citation12]. Follow-up was done by manual review of patient charts, after minimum one year. Patients were characterized as septic if presenting with clinical signs of infection, fulfilling the systemic inflammatory response syndrome (SIRS) criteria [Citation23].
Table 1. Inclusion and exclusion criteria.
Statistical analysis
Continuous variables are presented as median and interquartile range (IQR). The assessment of differences between groups was performed using the Mann–Whitney U-test. Dichotomous variables are presented as absolute and relative frequencies, while comparisons between groups are described using Pearson’s χ2. In all statistical analyses, a p value<.05 was considered significant. Survival analysis was performed using the Kaplan–Meier estimator. All analyses were performed using IBM SPSS software version 22 for Windows (IBM Corp, Armonk, NY) and Stata 12 (StataCorp, College Station, TX).
The study was approved by the local ethical committee.
Results
During the study period, 249 patients admitted to Helsingborg hospital with diverticular disease of the colon were identified. After exclusions, 132 patients with CT verified AUD were included in the study, 101 of whom received antibiotic therapy together with bowel rest and i.v. fluids. The remaining 31 patients were managed with i.v. fluids and bowel rest only (). During the study period, none of the patients died, nor were any patients operated for complications of AUD. After the introduction of the protocol, 60% (31/50) of the patients were managed without antibiotics. During the first 8 months with the new protocol, the proportion of patients treated without antibiotics varied between 44% and 83% per month. Specialists initiated antibiotic therapy significantly more often than registrars (p=.03).
Between the groups, no statistically significant differences in median age, sex, body mass index (BMI), CRP, WBC, body temperature, or previous episodes of diverticulitis were observed (). Patients receiving antibiotic therapy had significantly more comorbidities of any kind, than patients handled without antibiotics 60% (61 patients) vs. 39% (12 patients) p=.03 ().
Table 2a. Background characteristics of the whole study population.
Among patients treated after introduction of the new treatment protocol (n = 50), the CRP level was significantly higher in patients treated with antibiotics (p=.008); (). Median duration of symptoms, clinical findings and frequency of CT scan performed at admission did not differ significantly between the treatment groups (). Patients treated without antibiotics had a significantly shorter median length of hospital stay than patients treated with antibiotics (two days [IQR =1–3] vs. three days [IQR =2–4]; p=.04) (). Median treatment duration with antibiotics was 10 days (IQR =8–12). In the antibiotic group, 91% of patients received i.v. therapy which was continued orally in 85% whereas 9% had only oral therapy.
Table 2b. Background characteristics in acute uncomplicated diverticulitis patients after protocol introduction.
Table 3. Findings at admission and hospital length of stay.
During the study period, no patients developed abscesses, stenosis or sepsis. Two patients (2%) developed perforation, both of whom had received antibiotic therapy. One patient (1%), treated with antibiotics, developed a fistula. In total, 14% of the patients were readmitted due to recurrent diverticulitis within the study period. Among patients treated with antibiotics, 16% had a recurrence compared to 6% of the patients without antibiotic treatment ().
Table 4. Complications following an episode of acute uncomplicated diverticulitis within 12 months.
Discussion
This study shows that the introduction of a new treatment protocol for AUD without antibiotics was challenging. The protocol was adhered to in only 60% of eligible patients. There was no significant differences in the number of complications in AUD patients treated with or without antibiotics. However, patients with antibiotic treatment suffered from significantly more comorbidities and tended to have higher CRP indicating a selection bias towards milder AUD in the non-antibiotic group. The patients treated without antibiotics had a significantly shorter hospital stay. As far as we know, this is the first study in Sweden performed at a hospital not participating in the AVOD study, introducing a non-antibiotic treatment of AUD in routine hospital care.
The compliance to the new treatment protocol varied throughout the study period, without any signs of increasing compliance. Thus, it seems to be difficult to make physicians follow new treatment regimens and despite thorough information about the new protocol, 40% of the patients treated for AUD at Helsingborg Hospital were still treated with antibiotics. Consultants initiated antibiotic therapy significantly more often than registrars. Possibly, young doctors embrace new treatment regimens more easily than more experienced physicians. Another explanation might be that the more experienced doctors are likely to look after patients with severe disease. Notably, despite several studies [Citation12–14,Citation16] in favor of non-antibiotic treatment approach for AUD this has not been widely accepted in Sweden. Studies evaluating adherence to new treatment protocols are scarce and the reasons for low cohesion in this study need further investigations.
The majority of complications in this study consisted of recurrent disease. Few other complications were observed. In other studies, the rate of recurrent diverticulitis varies between 7 and 45% [Citation12,Citation24] compared to 16% in our study. Previous studies suggest that AUD recurrences occur in the first few months after the initial episode [Citation12,Citation24]. The patient numbers in the non-antibiotic group was small, with only 31 participants. It could not be excluded that the lower comorbidities and CRP levels in that non-antibiotic group per se could influence the incidence of complications, disguising a difference between the groups. This would concur with the results of a recent metaanalysis looking at a total of nine studies in which two were RCTs, where regression analysis of factors for treatment failure without antibiotics shows that the only significant factor is associated comorbidities [Citation25].
This is a retrospective study, with all the limitations associated with such a design. In the absence of randomizing and blinding, there is naturally a risk of selection bias. In contrast to the AVOD study, our retrospective study included a detailed exclusion analysis with strict criteria and sepsis was defined according to established criteria. Consequently, we did encounter a high exclusion rate (47%). However, the majority of exclusions (58%) were due to false diagnostic coding. A strength of the present study is that we present a consecutive AUD series that reflects daily clinical praxis.
Conclusions
In summary, the compliance of physicians to the newly introduced protocol prescribing no antibiotics to AUD-patients in daily clinical praxis was lower than anticipated. This study indicates that it is feasible to treat AUD without antibiotics in terms of complications. There were however significant differences in backgrounds factors between the patient groups.
Supplemental Material
Download MS Word (47 KB)Acknowledgements
We thank Mr. Abbas Chabook for letting us use the CRF from the AVOD study.
Disclosure statement
The authors report no conflict of interest.
References
- Bollom A, Austrie J, Hirsch W, et al. Emergency department burden of diverticulitis in the USA, 2006–2013. Dig Dis Sci. 2017;62(10):2694–2703.
- Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–1187.e1–3.
- Biondo S, Golda T, Kreisler E, et al. Outpatient versus hospitalization management for uncomplicated diverticulitis: a prospective, multicenter randomized clinical trial (DIVER Trial). Ann Surg. 2014;259:38–44.
- Janes SE, Meagher A, Frizelle FA. Management of diverticulitis. BMJ. 2006;332:271–275.
- Brochmann ND, Schultz JK, Jakobsen GS, et al. Management of acute uncomplicated diverticulitis without antibiotics: a single-centre cohort study. Colorectal Dis. 2016;18:1101–1107.
- Young-Fadok TM, Roberts PL, Spencer MP, et al. Colonic diverticular disease. Curr Probl Surg. 2000;37:457–514.
- Vennix S, Morton DG, Hahnloser D, et al. Systematic review of evidence and consensus on diverticulitis: an analysis of national and international guidelines. Colorectal Dis. 2014;16:866–878.
- Stollman N, Raskin JB. Diverticular disease of the colon. Lancet. 2004;363:631–639.
- Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007;357:2057–2066.
- Walker MM, Harris AK. Pathogenesis of diverticulosis and diverticular disease. Minerva Gastroenterol Dietol. 2017;63:99–109.
- Goossens H. Antibiotic consumption and link to resistance. Clin Microbiol Infect. 2009;15(Suppl.):12–15.
- Chabok A, Påhlman L, Hjern F, et al. Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg. 2012;99:532–539.
- Daniels L, Unlu C, de Korte N, et al. Randomized clinical trial of observational versus antibiotic treatment for a first episode of CT-proven uncomplicated acute diverticulitis. Br J Surg. 2017;104:52–61.
- Isacson D, Andreasson K, Nikberg M, et al. No antibiotics in acute uncomplicated diverticulitis: does it work? Scand J Gastroenterol. 2014;49:1441–1446.
- Hjern F, Josephson T, Altman D, et al. Conservative treatment of acute colonic diverticulitis: are antibiotics always mandatory? Scand J Gastroenterol. 2007;42:41–47.
- de Korte N, Unlü C, Boermeester MA, et al. Use of antibiotics in uncomplicated diverticulitis. Br J Surg. 2011;98:761–767.
- Andeweg CS, Mulder IM, Felt-Bersma RJ, et al. Guidelines of diagnostics and treatment of acute left-sided colonic diverticulitis. Dig Surg. 2013;30:278–292.
- Andersen JC, Bundgaard L, Elbrond H, et al. Danish national guidelines for treatment of diverticular disease. Dan Med J. 2012;59:C4453.
- Kruis W, Germer CT, Leifeld L, et al. Diverticular disease: guidelines of the German Society for Gastroenterology, Digestive and Metabolic Diseases and the German Society for General and Visceral Surgery. Digestion. 2014;90:190–207.
- Rafferty J, Shellito P, Hyman NH, et al. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939–944.
- Sartelli M, Viale P, Koike K, et al. WSES consensus conference: guidelines for first-line management of intra-abdominal infections. World J Emerg Surg. 2011;6:2.
- Agresta F, Ansaloni L, Baiocchi GL, et al. Laparoscopic approach to acute abdomen from the Consensus Development Conference of the Societa Italiana di Chirurgia Endoscopica e nuove tecnologie (SICE), Associazione Chirurghi Ospedalieri Italiani (ACOI), Societa Italiana di Chirurgia (SIC), Societa Italiana di Chirurgia d'Urgenza e del Trauma (SICUT), Societa Italiana di Chirurgia nell'Ospedalita Privata (SICOP), and the European Association for Endoscopic Surgery (EAES). Surg Endosc. 2012;26:2134–2164.
- Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31:1250–1256.
- Eglinton T, Nguyen T, Raniga S, et al. Patterns of recurrence in patients with acute diverticulitis. Br J Surg. 2010;97:952–957.
- Emile SH, Elfeki H, Sakr A, et al. Management of acute uncomplicated diverticulitis without antibiotics: a systematic review, meta-analysis, and meta-regression of predictors of treatment failure. Tech Coloproctol. 2018;22:499–509.