Abstract
Objective
To provide optimal health care for patients with acute cholecystitis in need of acute cholecystectomy, resource allocation has to be optimized. The aim of this study was to assess possible regional inequity regarding the treatment of acute cholecystitis and explore regional differences in the management of acute cholecystitis.
Methods
Data were retrieved from the Swedish National Register for Gallstone Surgery and Endoscopic Retrograde CholangioPancreatography. Between January 2010 and December 2019, 22,985 patients who underwent cholecystectomy for acute cholecystitis and without prior history of acute cholecystitis were included in the study. The ratio of cholecystectomies with acute cholecystitis performed within two days of admission to hospital compared to population density was studied. Furthermore, the proportion of acute performed cholecystectomies within two days of admission in regions, with or without tertiary care centers, was also examined.
Results
No correlation between population density and proportion of acute performed cholecystectomies was found. Regions without tertiary care centers had a higher proportion of acute cholecystectomies performed within two days (5–10%). The difference in the ratio of acute cholecystectomies within two days of admission was significant for all years investigated except 2010.
Conclusions
The presence of a tertiary referral center within the region had a greater influence than the population density on the chance of undergoing acute cholecystectomy for patients with acute cholecystitis. There are several potential explanations for this, one being an interference of the needs of patients requiring tertiary referral center care with the needs of patients in need of acute care surgery.
Introduction
Laparoscopic cholecystectomy as a treatment for symptomatic gallstone disease is among one of the most common procedures within general surgery [Citation1]. The NIH Consensus Statement from 1992 further stated that patients with symptomatic gallstone disease should be treated preferably with laparoscopic cholecystectomy by properly trained surgeons since this technique decreases pain and disability without increasing morbidity or mortality [Citation2].
Acute cholecystitis is caused by an obstruction of the gallbladder neck or the cystic duct, in most cases due to gallstones, leading to distension and an ensuing bacterial or chemical inflammation of the gallbladder. If left untreated, it can cause perforations, fistulae, abscess formation or chronic cholecystitis. In the early stages of acute cholecystitis, the gallbladder is surrounded by oedema, making it easier to identify the different tissue layers, resulting in generally less complicated surgery [Citation3,Citation4]. If surgery is delayed, the local inflammation causes a gradual replacement of the oedema with regenerative tissue, which makes it more problematic to identify the tissue layers and the surgical dissection thus more challenging. According to the WSES updated guidelines [Citation5] as well as the 2018 Tokyo guidelines [Citation6], early laparoscopic cholecystectomy is the standard of care for patients with acute calculous cholecystitis.
Research on patients with gallstone disease with mild to moderate symptoms is currently limited. This risks to create diverging standards of care, where the decision to undergo surgery depends on local practice or personal preference of competence of the individual surgeon. There are currently few studies present regarding the potential influence that regional administrative and geographical circumstances might have on the management of patients in need of acute care for gallstone disease. In Sweden there is, at least in theory, standardized routines concerning treatment and management of patients with uncomplicated as well as complicated gallstone disease. However, the demographic structure of Sweden, like in many countries with vast areas and uneven population density, poses challenges in offering equal healthcare to all its citizens.
This study intended to detect possible regional inequity regarding the treatment of acute cholecystitis and try to find a common denominator that might explain these differences.
Methods
This population-based register study used data collected from the Swedish National Register for Gallstone Surgery and Endoscopic Retrograde Cholangiopancreatography (GallRiks). GallRiks is a database containing prospectively assembled data registered online by the responsible surgeon in direct conjunction with the procedures. An independent coordinator registers a 30-day follow-up at each participating unit. At this mandatory postoperative control, the coordinator reviews the medical records of each patient and occasionally contacts patients by phone not to miss any intra- or post-operative complications [Citation7]. GallRiks has a more than 90% national coverage of all cholecystectomies in Sweden [Citation8] and validation of GallRiks-data has demonstrated high completeness and correctness of the data and no failure to report serious adverse events [Citation9].
The data in this study are obtained from 2010 to 2019. Altogether 121,724 cholecystectomies were registered in GallRiks during this period. Data included 22,985 patients who had ongoing acute cholecystitis, underwent cholecystectomy, and had no prior history of acute cholecystitis.
Outcome measure was procedures carried out within two days after admission for patients with acute cholecystitis in the 21 administrative Swedish regions. Population density, presence of tertiary care centers within the region and year of admittance were predictors. Confounders adjusted for in the multivariate regression analyses were ASA classification, age and sex.
Statistical analyses
Pearson’s chi-square test as well as multivariable regression analyses was used. The analyses were based on patients undergoing cholecystectomy for ongoing acute cholecystitis and without a known history of previous cholecystitis in regions with or without tertiary care centers. The postoperative complication rate within 30 days after the cholecystectomy was determined by extracting data from the GallRiks database. The time of surgery was dichotomized to patients undergoing surgery within two days on arrival to the hospital or not. Age was dichotomized to if the patient was older than the mean age, i.e., 55 years. In the multivariable logistic regression analysis, the odds ratio for undergoing surgery within two days or not was determined, adjusted for sex, age and ASA-score. Statistical significance was defined as p<.05. Statistical analysis was performed using JMP Pro 16.0.0 (SAS Institute, Inc., Cary, NC).
Ethics
All data were anonymized, and all analyses were conducted at the group level. This study was approved by the Ethics Committee (Etikprövningsmyndigheten), Uppsala, Sweden (Dnr: 2020-05899) and was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki [Citation10].
Results
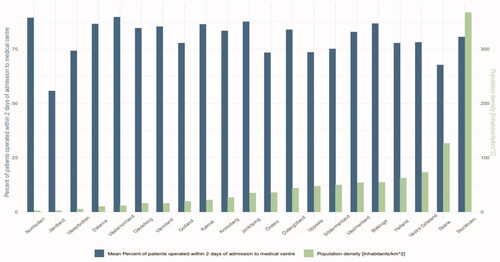
Demographics of the included patients with acute ongoing cholecystitis during the studied time period, year by year, are given in . Patients operated for acute cholecystitis were slightly older in the regions without tertiary care center (). This paper's definition of acute performed cholecystectomy is: ‘Cholecystectomy performed within two days on admission to a hospital with a surgical unit’. Data were analyzed from 2010 to 2019 regarding a possible correlation between the ratio of acute performed cholecystectomies and population density over time. The acute cholecystectomy ratio varied considerably between the regions, and no correlation between population density and ratio of acute cholecystectomies was seen ().
Table 1. Demographics of all the included patients with acute ongoing cholecystitis 2010–2019.
Table 2. The demographics of the included patients with ongoing cholecystitis divided regarding if they were operated in regions with or without TRC.
However, there existed a discrepancy between when on admission acute cholecystectomies in regions with and without tertiary care centers were performed (). The regions without tertiary care centers had a significantly higher proportion of performed acute cholecystectomies within two days on admission for all years investigated 2010–2019, except 2010 (). These differences remained in the multivariable analysis where we also found that during most years the patients with ASA III or higher with acute cholecystitis were less likely to be operated within two days (). There were also large individual differences between the different 21 administrative regions in how quickly on admission the patients with acute cholecystitis were operated ().
Figure 2. Acute cholecystitis – operated days on admission (%). Regions with or without tertiary referral centers (TRC).
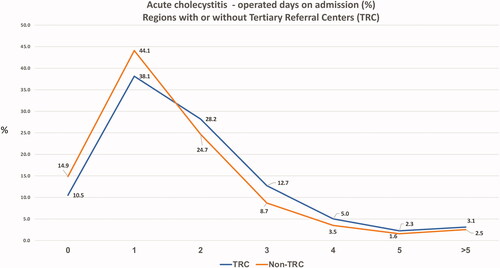
Figure 3. Performed acute cholecystectomies within two days on admission on patients with acute cholecystitis 2010–2019 in regions with or without TRC.
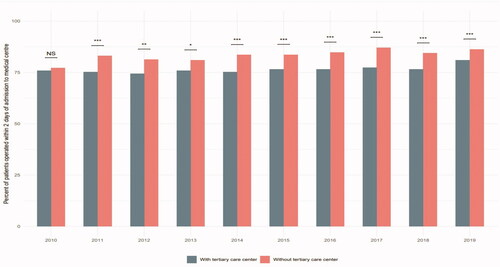
Table 3. Multivariable analysis of sex, age, ASA-class and regions with- or without tertiary care centers, and postoperative complications regarding the variable operated within two days.
Table 4. Acute cholecystitis – operated days on admission in the 21 administrative regions (%).
The postoperative complication rate did not differ between regions with or without tertiary care centers during the time-period 2010–2014. However, during the time-period 2015–2019, regions without tertiary care centers had a significantly lower postoperative complication rate ().
Table 5. Postoperative complications in regions with and without TRC during the studied time period.
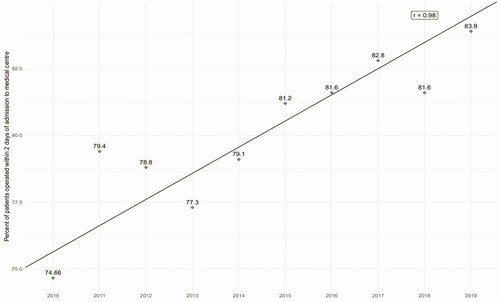
The overall mean average of acute cholecystitis operated within two days in all Swedish regions combined, has increased by 9.2% from 2010 to 2019 ().
Discussion
This study did not support the original hypothesis that population density correlates with the ratio of timely performed cholecystectomies for acute cholecystitis. Nevertheless, the study showed a significantly higher probability of undergoing surgery within two days for patients admitted for acute cholecystitis in a region without a tertiary care center compared to regions without one. Furthermore, the study shows that the chance of undergoing surgery within two days steadily increased over time. During the second half of the study period, the postoperative complication rate was significantly lower for cholecystectomies operated in regions without a tertiary care center.
Early intervention has been shown to be beneficial for patients with acute cholecystitis by reducing length of stay, morbidity and mortality [Citation11–13]. Thus, it is of utmost importance that efforts should be made to perform cholecystectomy early in patients with acute cholecystitis. The present study suggests that this is more easily accomplished at units where the resources do not have to be shared with patients requiring the specialized competence and equipment of tertiary care centers.
Sweden is a country with a population with only just over 10 million citizens and 21 administrative and geographical regions with varying population densities [Citation14,Citation15]. To provide highly specialized surgery for patients with advanced GI-malignancies, seven of these 21 regions have tertiary care centers to which these patients are to be referred. All tertiary care centers also have resources for providing acute surgery, including cholecystectomy on patients with acute ongoing cholecystitis. However, there is always a risk that competing interests of acute benign and acute malignant surgery will be set against each other and that the need of surgery for acute ongoing cholecystitis is at risk of being given lower priority. This study, to some extent, supports this hypothesis since patients with ongoing acute cholecystitis in regions without a tertiary care center were significantly more often operated within two days on admission when compared to regions with tertiary care centers. This is of course probably not the only explanation for this difference. Patients in the group without a tertiary care center were older, which could explain why a greater proportion is managed conservatively.
We have no definite explanation for the diverging surgical practice. However, one plausible theory is that in the tertiary hospitals, with a higher volume of more advanced surgery, cholecystectomies of acute cholecystitis are de-prioritized in favor of surgery requiring the greater competence and resources. An additional contributing factor may also be the intense reorganization and centralization of major surgery that has taken place in Sweden in recent years. This could explain why the postoperative complication rate was slightly but significantly higher (11.8% vs. 10.0%; p=.0016) in the group with tertiary care centers during the second half of the study period.
Structural obstacles similar to those seen in Sweden have also been observed in the United Kingdom, where the chance of undergoing cholecystectomy in due time after being admitted for acute cholecystitis was more dependent on organization of health care rather than the individual need of the patient [Citation16]. Guidelines based on evidence seem not to be sufficient to provide patients with cholecystitis timely treatment, there is also a need for a well-organized structure where the patient flow is not disturbed by patients with conditions requiring other priorities and resources. In a quality improvement program conducted in the United Kingdom, it was shown that the management of patients with acute cholecystitis could be improved substantially by clarifying the purposes of the quality improvement to the stakeholders, creating additional resources to carry out emergency cholecystectomies and coordinating patient pathways [Citation17]. The improvement in cost-effectiveness by optimizing the flow of patients with acute cholecystitis may in the long run be expected to reduce health care costs, which ideally could make more resources available for patients requiring the care of tertiary referral centers.
A strength of this study is the extensive amount of validated data collected from GallRiks, which has a national coverage of over 90% and more than 100,000 registered procedures [Citation8].
Limitations
Limitations of this study include the absence of some confounders that might affect or, to a certain degree, explain the difference in results between the patient populations such as BMI, alcohol, smoking and compliance to medical expertise. These limitations were to a certain degree adjusted for by including the confounders age, sex and ASA classification in the analyses.
In conclusion, the question remains why these differences between different regions with or without tertiary care centers exist; down-prioritization of cholecystectomies due to intense reorganization and centralization of major surgery? Nevertheless, a positive signal is that although there are differences between regions with and without a tertiary care center in how they treat patients with ongoing acute cholecystitis, the percentage of patients undergoing surgery within two days of admission is slowly increasing. Further research is warranted to explain the difference in the ratio of acute cholecystectomies between regions with and without tertiary care centers.
Authors contributions
Study concept: JHL and LE. Study design: LE. Data acquisition: JHL and LE. Quality control of data and algorithms: JHL, JÖ, GS and LE. Data analysis and interpretation: JÖ, GS and LE. Statistical analysis: LE. Manuscript preparation: JHL and LE. Manuscript editing: JÖ, GS and LE. Manuscript review: GS and LE.
| Abbreviations | ||
| ERCP | = | Endoscopic Retrograde CholangioPancreatography |
| NIH | = | National Institutes of Health |
| GallRiks | = | The Swedish National Register for Gallstone Surgery and Endoscopic Retrograde Cholangiopancreatography |
| ASA | = | American Society of Anesthesiologists |
| GI | = | Gastrointestinal |
| WSES | = | World Society of Emergency Surgery |
| BMI | = | Body mass index |
Acknowledgements
We would like to acknowledge Statistician Robert Lundqvist, Region Norrbotten, Sweden for fruitful discussions regarding statistics.
Disclosure statement
The authors declare that there is no conflict of interest.
Additional information
Funding
References
- Keus F, Gooszen HG, van Laarhoven CJ. Open, small-incision, or laparoscopic cholecystectomy for patients with symptomatic cholecystolithiasis. An overview of Cochrane Hepato-Biliary Group reviews. Cochrane Database Syst Rev. 2010;2010:CD008318.
- Gallstones and laparoscopic cholecystectomy. NIH Consensus Statement. 1992;10:1–28.
- Halpin V. Acute cholecystitis. BMJ Clin Evid. 2014;2014:411.
- Burmeister G, Hinz S, Schafmayer C. Acute cholecystitis. Zentralbl Chir. 2018;143(4):392–399.
- Pisano M, Allievi N, Gurusamy K, et al. 2020 World Society of Emergency Surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World J Emerg Surg. 2020;15(1):61.
- Okamoto K, Suzuki K, Takada T, et al. Tokyo guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2018;25(1):55–72.
- Enochsson L, Thulin A, Österberg J, et al. The Swedish Registry of Gallstone Surgery and Endoscopic Retrograde Cholangiopancreatography (GallRiks): a nationwide registry for quality assurance of gallstone surgery. JAMA Surg. 2013;148(5):471–478.
- Österberg J, Sandblom G, Enochsson L. Annual report 2021. GallRiks; 2021. Available from: https://www.ucr.uu.se/gallriks/fou/arsrapporter/arsrapporter/arsrapport-2020
- Rystedt J, Montgomery A, Persson G. Completeness and correctness of cholecystectomy data in a national register-GallRiks. Scand J Surg. 2014;103(4):237–244.
- World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–2194.
- Casillas RA, Yegiyants S, Collins JC. Early laparoscopic cholecystectomy is the preferred management of acute cholecystitis. Arch Surg. 2008;143(6):533–537.
- Polo M, Duclos A, Polazzi S, et al. Acute cholecystitis-optimal timing for early cholecystectomy: a French Nationwide Study. J Gastrointest Surg. 2015;19(11):2003–2010.
- Blohm M, Österberg J, Sandblom G, et al. The sooner, the better? The importance of optimal timing of cholecystectomy in acute cholecystitis: data from the National Swedish Registry for Gallstone Surgery, GallRiks. J Gastrointest Surg. 2017;21(1):33–40.
- Statistiska Centralbyrån. Befolkningstäthet i Sverige (Population density in Sweden); 2019. Available from: http://www.scb.se/hitta-statistik/sverige-i-siffror/manniskorna-i-sverige/befolkningstathet-i-sverige/
- SCB. The people of Sweden (Människorna i Sverige); 2021. Available from: https://www.scb.se/hitta-statistik/sverige-i-siffror/manniskorna-i-sverige/
- Bamber JR, Stephens TJ, Cromwell DA, et al. Effectiveness of a quality improvement collaborative in reducing time to surgery for patients requiring emergency cholecystectomy. BJS Open. 2019;3(6):802–811.
- Stephens TJ, Bamber JR, Beckingham IJ, et al. Understanding the influences on successful quality improvement in emergency general surgery: learning from the RCS Chole-QuIC project. Implement Sci. 2019;14(1):84.