Abstract
Background
Diverticulosis is a common condition and is thought to be increasing in the Western population. Several studies have attempted to estimate the prevalence of diverticulosis and it’s inflamed state, diverticulitis, with results varying depending on study population and methodology, The aim of this study was to investigate the prevalence of diverticulosis in patients undergoing colonoscopy at a Swedish academic referral centre and to study the incidence of diverticulitis in a 10-year follow-up.
Methods
All patients who had undergone colonoscopy at the Endoscopy unit, Skåne University Hospital, Sweden, during 01 January 2010 through 31 December 2011 were identified. The colonoscopy referrals, colonoscopy reports, and medical records until 14 June 2022 were reviewed.
Results
In all, 2648 patients were included in the study, whereof 910 patients had reported diverticulosis (34.4%). During the 10-year follow-up, the overall incidence of computed tomography verified diverticulitis was 4.4%, and 0.6% for patients with and without diverticulosis at index colonoscopy, respectively. Of the 50 patients that developed diverticulitis, 21 were complicated and 29 uncomplicated
Conclusion
Diverticulosis is a common condition in the population, although most patients will not develop diverticulitis.
Keywords:
Introduction
Diverticula, outpouchings of the intestinal wall, are known anatomical variants since the beginning of the twentieth century but were at that time seldom encountered [Citation1]. What is today frequently referred to as diverticulosis is the presence of false diverticula, that is, herniation of the mucosa and submucosa through the muscular layer of the colonic wall, most often found in the sigmoid colon [Citation2]. The frequency of diverticulosis increases with age and the incidence of complications to diverticulosis (i.e. diverticular disease) is increasing in the western population [Citation3]. As diverticulosis is often asymptomatic, the true prevalence of the condition is elusive. An autopsy study from Australia in 1969 examining 200 specimens found diverticulosis in 90 (45%) [Citation4]. However, it is thought that diverticulosis has become more frequent today, considering increased life expectancy, western diet and sedentary life style, which are all known risk factors of diverticulosis [Citation5]. There are few modern prevalence studies, thus knowledge is lacking regarding how common diverticulosis is in different populations [Citation6].
Previously the lifetime risk of diverticulitis in an individual with diverticulosis was approximated to 25% [Citation5,Citation7]. However, these estimates are based on data collected as far back as from the 1930s. More recent studies have concluded that incidentally detected diverticulosis is rarely complicated (4-7%) by diverticulitis [Citation8–10]. However, study cohorts were small apart from the Californian study by Shahedi et al. [Citation8].
The aim of the present study was to examine the prevalence of diverticulosis in a Swedish study population undergoing colonoscopy at an Academic referral centre in order to investigate the incidence of diverticulitis in a 10-year follow-up.
Materials and methods
All patients referred to the Endoscopy unit, Skåne University Hospital Malmö, Sweden for a colonoscopy during the time period 01 January 2010 to 31 December 2011 were considered eligible for inclusion. The patients’ medical records (from the Region of Skåne; that is, also from surrounding hospitals) and colonoscopy reports were reviewed (by HD, GL, and HS). Inclusion criteria were completed colonoscopy and accessible colonoscopy reports as well as medical records. Patients with previous diverticulitis and those who had undergone sigmoid resection were excluded.
For patients with multiple colonoscopies during the study period, only the first with an available report was used. Data was collected from the date of colonoscopy until 14 June 2022. A 10-year follow-up time period was chosen in concordance with previous similar study set-ups [Citation8].
Diverticulosis was defined as findings of diverticula according to the standardised colonoscopy report. The medical charts were scrutinized for previous episodes of diverticulitis as well as diverticulitis episodes after the colonoscopy. Diverticulitis had to have been verified with computed tomography. Complicated diverticulitis was distinguished from uncomplicated based on abscess formation, perforation, or fistulation, according to the medical records. If a patient had multiple diagnoses of diverticulitis during the follow-up period, the first episode of complicated diverticulitis was used if present, otherwise, the first episode of uncomplicated diverticulitis was used.
In ten patients diagnosed with diverticulitis, with no diverticulosis stated in the colonoscopy report, the photo documentation from the examinations were reviewed. Furthermore, the presence of diverticulosis was randomly confirmed by reviewing the photo documentation of the colonoscopy in ten patients (by CFR).
Statistics
Statistical analyses were made using IBM SPSS statistics version 28.
Cox regression analysis was used to visualize the difference in risk for diverticulitis in patients with or without diverticulosis. Hazard ratios (HR) were calculated and were adjusted for sex, age, and previous diverticulitis.
Ethics
The study was approved by the Swedish Ethical Review Authority (Dnr 2022-03019-01)
Results
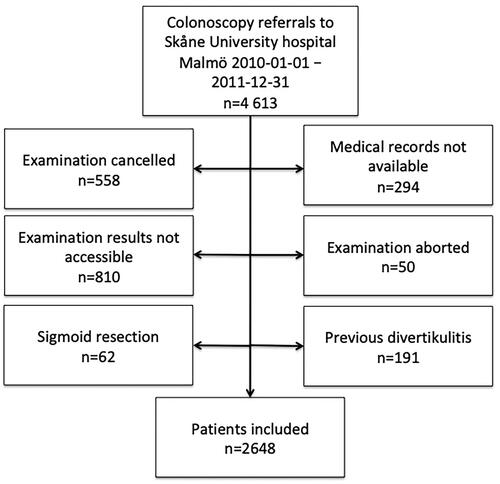
In all, 4614 patients were considered eligible for inclusion. After exclusion, the study population consisted of 2648 patients. Reasons for exclusion are presented in the study flow chart ().
Cancelled examinations included both cancellations made by the patient and by the clinic and numbered 558 cases. In 810 instances in which the examination results could not be retrieved, the examination had been performed at a private practice. In 294 cases, the patient was for unknown reasons not registered in the hospital medical records. In all, 50 examinations had been aborted, mostly due to inadequate laxation, making it impossible to examine the colon. Previous diverticulitis was noted in 191 patients, and 62 patients had previously undergone sigmoid resection, leading to their subsequent exclusion from the study.
The study population included 52.9% women (n = 1400) and 47.1% men (n = 1248). The median age was 62 (range 3–93; IQR 46–73). Characteristics of the study population, with patients diagnosed with diverticulitis presented separately, are shown in . In all, 910 patients had diverticulosis (34.5%).
Table 1. Characteristics of the study population.
In the ten-year follow-up period, 50 patients had an episode of diverticulitis. For the entire study population, the risk of diverticulitis during the follow-up period was 1.9%. However, when stratifying by the presence of diverticulosis at index colonoscopy, the risk was notably higher among those with diverticulosis compared to those without. They encompassed 40 patients, and the risk was 4.4%, compared to patients without diverticulosis which numbered 10 with a risk of 0.6%. Relative risk in patients with diverticulosis by age group is demonstrated in .
Table 2. Risk ratios for the risk of developing diverticulitis by age.
Of the patients diagnosed with diverticulitis, 29 had uncomplicated disease and 21 complicated disease.
Discussion
In this study cohort, the prevalence of diverticulosis was 34.4%. The incidence of computed tomography verified diverticulitis during the 10-year follow-up was 4.4% and 0.6% in patients with and without diverticulosis at index colonoscopy, respectively.
The results of the current study can be compared to two recent studies. In a Swedish study by Järbrink-Sehgal et al. examining 742 randomly selected patients (median age 70 years), only 17.5% had diverticulosis, even though the study was prospective and the examination with colonoscopy was focused on findings of diverticula [Citation11]. The results of the current study are more similar to a North American prospective study from the University of North Carolina, examining 619 screening patients with colonoscopy and identified colonic diverticula in 255 (41%) [Citation12]. One reason for the higher prevalence in the current study compared to the study by Järbring-Sehgal et al. is the fact that there is a significant risk of selection bias in the current study, as all study participants had been referred to and undergone colonoscopy at an Academic referral centre.
In the current study, the risk of diverticulitis in the presence of diverticulosis corresponds well to a German study examining 433 patients (age <75) with diverticulosis undergoing colonoscopy in 1998–2000 with a follow-up time of up to 17 years. Thirty cases (6.9%) were diagnosed with diverticulitis with mean time to diagnosis 5.9 years [Citation9], which can be compared to 4.4% in the current study in a 10-year follow-up.
The largest study investigating risk of diverticulitis in patients with diverticulosis is by Shahedi et al. who retrospectively examined Californian patients who had undergone colonoscopy 1996–2011. In all, 2222 patients with diverticulosis without previous diverticulitis were identified. During an 11-year follow-up, 95 patients (4.2%) were diagnosed with diverticulitis. However, if rigorous criteria, i.e. imaging or surgery, for diagnosis were applied, only 23 met the criteria (1.0%) [Citation8].
Limitations of the current study include its retrospective design and the risk of selection bias, as all study participants had been referred to a colonoscopy due to symptoms or previously known colorectal disease and underwent the examination at an Academic referral centre. Information concerning patient factors such as diet, smoking, bowel habits, and lower gastrointestinal symptoms were not attainable.
Several different endoscopists performed the colonoscopies and no standardised colonoscopy study protocols were used. In a prospective setting it is possible that there would be a higher diverticulosis detection rate. In addition, an everyday clinical practise endoscopist may overlook the presence of small diverticula or fail to mention them in the report. It is therefore possible that the prevalence of diverticulosis found in our study is not generalisable to a larger population. However, at the Endoscopy unit in Malmö, findings during colonoscopy are routinely photographed. Random sampling and review of colonoscopy images in patients with diverticulitis without diverticulosis confirmed the results.
Only diverticulitis requiring at least one visit to the emergency department was identified due to lack of access to medical records from primary care givers. Also, computed tomography verification was required for the diagnosis of diverticulitis. Hence, some patients with only clinically suspected diverticulitis are not included. Subsequently, patients affected by uncomplicated diverticulitis not needing hospitalization may be missed, potentially underestimating the risk of uncomplicated diverticulitis. However, as clinical diagnosis of diverticulitis has poor diagnostic precision (up to 50% misdiagnoses) [Citation13], to include patients with only clinically suspected diverticulitis would render too much uncertainty in the results.
The frequency of complicated diverticulitis is considered more robust. It is unlikely that a physician would spare a computed tomography if a patient had signs of abscess, perforation or fistulation.
Despite the limitations of the study, the results are considered of interest to physicians involved in the care of patients with diverticulosis.
In conclusion, the results of this study indicate that even though diverticulosis is present in about a third of patients in a population referred to colonoscopy, the risk of diverticulitis in the following ten years is low.
Acknowledgement
We would like to acknowledge statistician Anna Åkesson at Forum Söder for advice and analyses.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data will be available upon request.
Additional information
Funding
References
- Telling M. Discussion on diverticulitis. Proc R Soc Med. 1920;13(Surg Sect):96–98.
- Stollman N, Raskin JB. Diverticular disease of the Colon. Lancet. 2004;363(9409):631–639. doi: 10.1016/S0140-6736(04)15597-9.
- Munie ST, Nalamati SPM. Epidemiology and pathophysiology of diverticular disease. Clin Colon Rectal Surg. 2018;31(4):209–213. doi: 10.1055/s-0037-1607464.
- Hughes LE. Postmortem survey of diverticular disease of the Colon. I. Diverticulosis and diverticulitis. Gut. 1969;10(5):336–344. doi: 10.1136/gut.10.5.336.
- Strate LL, Morris AM. Epidemiology, pathophysiology, and treatment of diverticulitis. Gastroenterology. 2019;156(5):1282–1298 e1. doi: 10.1053/j.gastro.2018.12.033.
- Tursi A, Scarpignato C, Strate LL, et al. Colonic diverticular disease. Nat Rev Dis Primers. 2020;6(1):20. doi: 10.1038/s41572-020-0153-5.
- Tursi A, Papa A, Danese S. Review article: the pathophysiology and medical management of diverticulosis and diverticular disease of the Colon. Aliment Pharmacol Ther. 2015;42(6):664–684. doi: 10.1111/apt.13322.
- Shahedi K, Fuller G, Bolus R, et al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol. 2013;11(12):1609–1613. doi: 10.1016/j.cgh.2013.06.020.
- Loffeld RJ. Long-term follow-up and development of diverticulitis in patients diagnosed with diverticulosis of the colon. Int J Colorectal Dis. 2016;31(1):15–17. doi: 10.1007/s00384-015-2397-1.
- Sharara AI, Ziade N, Shayto RH, et al. The natural history of incidental colonic diverticulosis on screening colonoscopy. Can J Gastroenterol Hepatol. 2018;2018:3690202–3690204. doi: 10.1155/2018/3690202.
- Järbrink-Sehgal ME, Andreasson A, Talley NJ, et al. Symptomatic diverticulosis Is characterized By loose stools. Clin Gastroenterol Hepatol. 2016;14(12):1763–1770 e1. doi: 10.1016/j.cgh.2016.06.014.
- Peery AF, Keku TO, Addamo C, et al. Colonic diverticula are not associated With mucosal inflammation or chronic gastrointestinal symptoms. Clin Gastroenterol Hepatol. 2018;16(6):884–891 e1. doi: 10.1016/j.cgh.2017.05.051.
- Werner A, Diehl SJ, Farag-Soliman M, et al. Multi-slice spiral CT in routine diagnosis of suspected acute left-sided colonic diverticulitis: a prospective study of 120 patients. Eur Radiol. 2003;13(12):2596–2603. doi: 10.1007/s00330-003-1887-7.