Abstract
Introduction
Conservative treatment of acute appendicitis is gaining popularity, and identifying patients with a higher risk of recurrence is becoming increasingly important. Previous studies have suggested that older age, male sex, diabetes, appendicolith and abscess formation may be contributing factors, however, results from the adult population are inconsistent.
Aim
This study aims to identify predictive factors for recurrent appendicitis after conservative treatment.
Methods
This retrospective study included patients with conservatively treated acute appendicitis at Skåne University Hospital, Sweden during 2012-2019. Information on patient demographics at index admission and follow-up data were retrieved from medical charts and radiologic images. Uni -and multivariable logistic regression analysis were performed using Stata Statistical Software.
Results
In total, 379 patients with conservatively treated acute appendicitis were identified, of which 78 (20.6%) had recurrence. All patients were followed-up for a minimum of 41 months after the first diagnosis of acute appendicitis unless appendectomy after successful conservative treatment or death occurred during follow-up. The median time to recurrence was 6.5 (1–17.8) months. After multivariable logistic regression analysis, external appendix diameter >10 mm [OR 2.4 (CI 1.37–4.21), p = .002] and intra-abdominal abscess [OR 2.05 (CI 1.18–3.56), p = .011] on computed tomography were significant independent risk factors for recurrent appendicitis. Appendicolith was not associated with an increased risk of recurrence.
Conclusion
This study suggests abscess formation and appendix distension of >10 mm to be potential risk factors for recurrent acute appendicitis after initial successful conservative treatment.
Introduction
Acute appendicitis has a lifetime risk ranging between 5 and 25%, and appendectomy is the most frequently performed general surgical procedure worldwide [Citation1,Citation2]. After advances in surgical technology, laparoscopic appendectomy is the method of choice for uncomplicated acute appendicitis. Conservative treatment, also referred to as non-operative management (NOM), including antibiotics, has been proven to be a safe alternative in both uncomplicated and complicated acute appendicitis [Citation1,Citation3–6], but adds a risk of treatment failure or recurrent appendicitis [Citation1,Citation7]. A meta-analysis from 2019 demonstrated an overall NOM treatment efficacy of 83% [Citation3], but the difference in efficacy between NOM and appendectomy vary in previous randomized controlled trials (RCTs) [Citation8–10].
Appendectomy offers the advantage of definitive treatment and enables histopathological verification, excluding an underlying appendiceal malignancy, such as neuroendocrine tumours or adenocarcinoma [Citation11,Citation12]. After appendectomy the 30-day mortality is low (0.23–0.3%), but long-term follow-up studies have reported postoperative morbidity of up to 19% including small bowel obstruction, wound rupture, intra-abdominal abscess and bleeding [Citation5,Citation13–16]. Nevertheless, with new approaches to laparoscopic appendectomy, postoperative complications have been significantly reduced [Citation17]. NOM avoids subsequent postoperative complications, but the risk of recurrent appendicitis is reported up to 39% in uncomplicated and 12–24% in complicated acute appendicitis [Citation1].
The choice between appendectomy and NOM, in both uncomplicated and complicated acute appendicitis, has become the subject of several investigations. Consideration of factors such as age, comorbidity, radiologic findings, and patient preference are recommended [Citation3,Citation16,Citation18–22]. Previous studies have suggested that male sex, diabetes, high C-reactive protein (CRP)-value, appendicolith and intra-abdominal abscess on computed tomography (CT) may be contributing factors for recurrent appendicitis, but findings are inconsistent [Citation4,Citation19–23].
Aim
This study aimed to identify clinical, laboratory and radiologic predictive factors for recurrent acute appendicitis after NOM. We expect comorbidity, high CRP-value, appendicolith and intra-abdominal abscess to be potential risk factors for recurrence.
Methods
Study cohort
The study population included all patients ≥18 years of age admitted to Skåne University Hospital (SUS), Sweden with International Classification of Disease (ICD)-10 diagnosis code for acute appendicitis and without operation code for appendectomy or surgery including appendectomy, from January 1st 2012 to December 31st 2019. Data was collected during the year 2022–2023 with the aim of a minimum follow-up time of 3 years. Eligible study participants were identified via the in-patient registry and the ICD-10 coding was independently validated. The diagnosis of acute appendicitis at index admission and at recurrence were verified by ultrasound (US), CT, or perioperatively if appendectomy was performed during recurrence. Exclusion criteria were admission outside the study period, unregistered appendectomy at index admission, deceased at index admission, unavailable medical charts, appendiceal malignancy during follow-up, other diagnosis than appendicitis or clinical diagnosis (no radiologic verification of diagnosis).
Data collection and study variables
Patient data from index admission and follow-up were retrospectively collected by medical chart review according to a predetermined case report form. Information on demographics (age, sex, BMI, previous abdominal surgery, hypertension and comorbidities included in the Charlson Comorbidity Index (CCI) [Citation24]), diagnostics (CRP, white blood cell (WBC) count, abscess formation, appendicholit and appendix external diameter), treatment with antibiotics, length of hospital stay, readmissions and appendectomy after successful NOM were collected. Cases with complex diagnostic images underwent a secondary review by a radiologist.
Statistical analysis
Statistical analysis was performed using SPSS (IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp) and Stata (StataCorp. 2023. Stata Statistical Software: Release 18. College Station, TX: StataCorp LLC). Lilliefors corrected Kolmogorov-Smirnov test and Shapiro-Wilks test, as well as, visual inspection of distribution with histograms, was used to determine the normality of the data distribution. Continuous numerical variables were presented as median and first to third quartile (Q1–Q3) or mean with a 95% confidence interval (CI). Dichotomous and categorical variables were presented as frequency and percentage. Differences between patients with and without recurrence were determined by univariable and multivariable logistic regression analysis presented in odds ratio (OR), 95% CI and p-value, with level of significance <.05. Multiple regression analysis was adjusted for age, gender and variables with a statistical significant p-value. Power calculations were not applied because of the retrospective study design.
Ethical considerations
This study was approved by the Regional Ethics Committee at Lund University (Dnr 2019-03583) on 19th August 2019.
Results
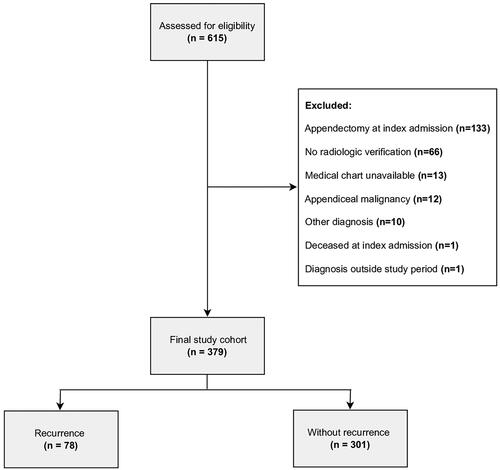
A total of 615 admissions, with acute appendicitis diagnosis and without appendectomy code, at SUS hospital were identified via the in-patient registry. Patients were excluded due to admission outside the study period (n = 1), unregistered appendectomy at index admission (n = 133), deceased at index admission (n = 1), unavailable medical charts (n = 13), appendiceal malignancy during follow-up (n = 12), other diagnosis than appendicitis (n = 10) or clinical diagnosis (no radiologic verification; n = 66). After exclusions, 379 patients constituted the final study cohort ().
Figure 1. Study flow chart demonstrating defined cohort of patients with conservatively treated acute appendicitis.
General characteristics
The study population had a mean age of 53 years (51–56), a median BMI of 25.5 (22.7-29.7), and almost half (49.3%) were female. Approximately one fourth (24%) had comorbidities, the most common being hypertension (20.3%) and diabetes (6.1%). The median CCI of the total study cohort was zero. Eighty-one (21.4%) patients had previously undergone abdominal surgery. Radiologic examinations at index admission demonstrated a total of 196 (51.7%) patients with intra-abdominal abscess and 53 (16.2%) patients with appendicolith (). The most frequent method used for diagnosing appendicitis was CT (97%).
Table 1. Characteristics of study cohort at index admission.
Follow-up and recurrence
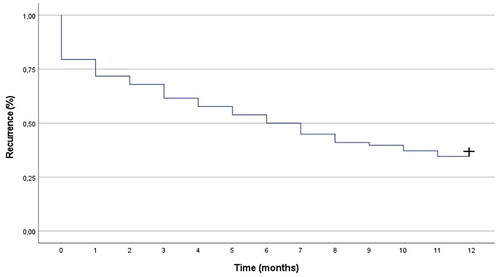
All patients were followed-up for a minimum of 41 months after the first diagnosis of acute appendicitis unless appendectomy after successful NOM or death occurred during follow-up. The median time of follow-up in the study population was 68 (45–98) months. In all, 78 (20.6%) patients experienced recurrent appendicitis, and the median time to recurrence was 6.5 (1–17.8) months (Table 1). A Kaplan–Meier curve showed a recurrence rate of 38.5% at three months, 50% at six months and 65.4% at one year (). After successful NOM at index admission, appendectomy during the follow-up period was registered in 68 (17.9%) patients (Table 1), of which 51 (75%) had recurrent appendicitis and 43 (63.2%) were performed acutely (data not shown).
Predictive factors for recurrence
In univariable logistic regression analysis, external appendix diameter >10 mm [OR 2.47 (CI 1.42–4.3), p = .001] and intra-abdominal abscess [OR 1.65 (CI 0.99–2.75), p = .053] on CT were identified as potentially significant predictors of recurrent appendicitis. No significant differences were found regarding age, gender, BMI, CRP, CCI, previous abdominal surgery, appendicolith and length of stay. After multivariable logistic regression analysis, external appendix diameter >10 mm [OR 2.4 (CI 1.37–4.21), p = .002] and intra-abdominal abscess [OR 2.05 (CI 1.18–3.56), p = .011] remained significant independent predictors of recurrent acute appendicitis (). The ability of the multivariable logistic regression model was investigated using a receiver operating characteristics (ROC) curve, with an area under curve (AUC) value of 0.66 (). The type of follow-up after conservative treatment was not significantly related to recurrence (data not shown).
Figure 3. Receiver operating characteristic (ROC) curve representing the predictive ability of the multivariable logistic regression model.
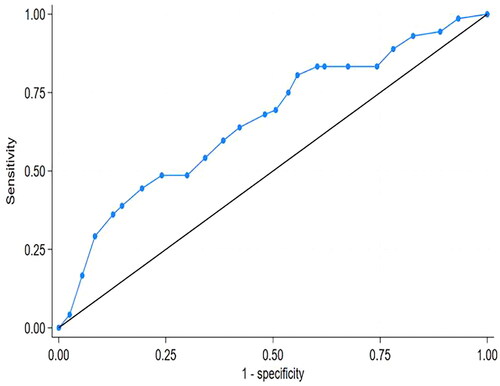
Table 2. Univariable and multivariable logistic regression for prediction of recurrent acute appendicitis.
Discussion
In this retrospective study, including both uncomplicated and complicated acute appendicitis, the recurrence of 20.6% was consistent with previous reports [Citation1,Citation5,Citation16,Citation18]. The present study provided a large cohort of adult patients with radiologically confirmed acute appendicitis and a median follow-up time that exceeds most prior studies. An appendix diameter of >10 mm and abscess formation were independently associated with recurrent appendicitis, while the presence of appendicolith, comorbidity and CRP-value were not significant predictors.
SUS hospital serves a population of approximately 750,000 inhabitants. At our institution, patients with radiologically confirmed complicated acute appendicitis are individually evaluated and may be treated conservatively. Our general approach to patients with uncomplicated acute appendicitis is laparoscopic appendectomy. The most likely reason for the high number of patients with conservatively treated uncomplicated acute appendicitis in this study is spontaneous recovery while awaiting surgery.
Characteristics that increase the risk of recurrence are not fully understood, and in current evidence-based literature, there is a wide spectrum of identified risk factors for recurrent acute appendicitis. Our results confirm previous findings that have identified abscess formation and a distended external appendix diameter on CT as significant risk factors [Citation21,Citation25,Citation26], although, the findings by Steiner et al. were described in a paediatric cohort. On the other hand, a recent retrospective study investigating multiple clinical and radiologic variables in adult patients during the COVID19 pandemic showed no significant association between recurrence and abscess formation or appendix diameter [Citation20]. However, as most prior studies, the cohort consisted of only 48 patients and a short follow-up time. Likewise, other studies have reported that type of appendicitis, abscess formation or percutaneous abscess drainage have no influence on the recurrence of acute appendicitis [Citation19,Citation20,Citation22,Citation27].
The presence of appendicolith in patients with acute appendicitis has allegedly been associated with high recurrence risk, which was not the case in this study. Our results are in line with some studies [Citation19,Citation20], but inconsistent with others [Citation22,Citation23,Citation28]. A large randomized trial by Flum et al. found increased recurrence risk in patients with appendicolith, but the study was limited by a follow-up time of 90 days, and selection bias with only 30% of eligible patients included in the final cohort. Conversely, Cuneyt et al. reported that recurrence was negatively associated with the presence of appendicolith, however, the radiologic finding of appendicolith was only detected in 17 patients [Citation4].
The discrepancy in study results may be explained by the substantial difference in cohort size, varying follow-up time, as well as the challenge of differentiating between recurrent acute appendicitis and persistent appendicitis. Moreover, studies focusing mainly on clinical parameters have also included conservatively treated patients without radiologic verification. Additional factors such as abscess size, the internal appendix diameter in relation to an appendicolith and the number of appendicoliths may affect the recurrence risk. Adjusting for these factors during analysis requires a large cohort of patients with appendicolith or abscess which should be considered in future studies.
Findings in this study based on radiologic parameters may be difficult to apply given acute appendicitis is often a clinical diagnosis in Sweden, primarily in young patients with typical symptoms. In cases with diagnostic uncertainty, US, if available, is used as the first-line modality. A CT scan is the most sensitive and specific diagnostic examination of acute appendicitis, with the disadvantage of exposure to ionizing radiation [Citation29]. This may still benefit patients above 40 years of age, since multiple studies [Citation12,Citation30] have demonstrated high rates (11–20%) of underlying appendiceal malignancy in patients with complicated acute appendicitis.
Limitations of this study include its retrospective and single centre study design, the loss of potential readmissions to facilities outside the region and the large difference in the number of patients with and without recurrence. Furthermore, the review of diagnostic images was delegated to multiple physicians, however, complex cases were reevaluated by a professor in radiology. Missing values were mainly restricted to BMI, appendicolith and external appendix diameter. Since these values were missing at random, statistical methods, such as multiple imputation, were not implemented in the analysis.
Conclusion
This study suggests abscess formation and appendix distension of >10 mm to be potential risk factors for recurrent acute appendicitis after initial successful conservative treatment. Identifying patients with a higher risk of recurrent appendicitis would rationalize the decision to perform appendectomy, instead of NOM.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15(1):27. doi: 10.1186/s13017-020-00306-3.
- Addiss DG, Shaffer N, Fowler BS, et al. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132(5):910–925. doi: 10.1093/oxfordjournals.aje.a115734.
- Yang Z, Sun F, Ai S, et al. Meta-analysis of studies comparing conservative treatment with antibiotics and appendectomy for acute appendicitis in the adult. BMC Surg. 2019;19(1):110. doi: 10.1186/s12893-019-0578-5.
- Kırkıl C, Yiğit MV, Aygen E. Long-term results of nonoperative treatment for uncomplicated acute appendicitis. Turk J Gastroenterol. 2014;25(4):393–397. doi: 10.5152/tjg.2014.7192.
- Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ. 2012;344(1):e2156–e2156. doi: 10.1136/bmj.e2156.
- McCutcheon BA, Chang DC, Marcus LP, et al. Long-term outcomes of patients with nonsurgically managed uncomplicated appendicitis. J Am Coll Surg. 2014;218(5):905–913. doi: 10.1016/j.jamcollsurg.2014.01.003.
- Simillis C, Symeonides P, Shorthouse AJ, et al. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon). Surgery. 2010;147(6):818–829. doi: 10.1016/j.surg.2009.11.013.
- Mentula P, Sammalkorpi H, Leppäniemi A. Laparoscopic surgery or conservative treatment for appendiceal abscess in adults? A randomized controlled trial. Ann Surg. 2015;266(6):e59–e242. doi: 10.1097/SLA.0000000000001495.
- Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA. 2015;313(23):2340–2348. doi: 10.1001/jama.2015.6154.
- Hansson J, Körner U, Khorram-Manesh A, et al. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 2009;96(5):473–481. doi: 10.1002/bjs.6482.
- Skendelas JP, Alemany VS, Au V, et al. Appendiceal adenocarcinoma found by surgery for acute appendicitis is associated with older age. BMC Surg. 2021;21(1):228. doi: 10.1186/s12893-021-01224-0.
- Mällinen J, Rautio T, Grönroos J, et al. Risk of appendiceal neoplasm in periappendicular abscess in patients treated with interval appendectomy vs follow-up with magnetic resonance imaging: 1-year outcomes of the peri-appendicitis acuta randomized clinical trial. JAMA Surg. 2019;154(3):200–207. doi: 10.1001/jamasurg.2018.4373.
- Bregendahl S, Nørgaard M, Laurberg S, et al. Risk of complications and 30-day mortality after laparoscopic and open appendectomy in a Danish region, 1998-2007; a population-based study of 18,426 patients. Pol Przegl Chir. 2013;85(7):395–400.
- Blomqvist PG, Andersson RE, Granath F, et al. Mortality after appendectomy in Sweden, 1987-1996. Ann Surg. 2001;233(4):455–460. doi: 10.1097/00000658-200104000-00001.
- Styrud J, Eriksson S, Segelman J, et al. Diagnostic accuracy in 2,351 patients undergoing appendicectomy for suspected acute appendicitis: a retrospective study 1986-1993. Dig Surg. 1999;16(1):39–44. doi: 10.1159/000018692.
- Sallinen V, Akl EA, You JJ, et al. Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br J Surg. 2016;103(6):656–667. doi: 10.1002/bjs.10147.
- Pogorelić Z, Beara V, Jukić M, et al. A new approach to laparoscopic appendectomy in children-clipless/sutureless harmonic scalpel laparoscopic appendectomy. Langenbecks Arch Surg. 2022;407(2):779–787. doi: 10.1007/s00423-021-02389-1.
- Podda M, Cillara N, Di Saverio S, et al. Antibiotics-first strategy for uncomplicated acute appendicitis in adults is associated with increased rates of peritonitis at surgery. A systematic review with meta-analysis of randomized controlled trials comparing appendectomy and non-operative management with antibiotics. Surgeon. 2017;15(5):303–314.
- Lien WC, Lee WC, Wang HP, et al. Male gender is a risk factor for recurrent appendicitis following nonoperative treatment. World J Surg. 2011;35(7):1636–1642. doi: 10.1007/s00268-011-1132-5.
- Richards CB, Pendower LK, Kotecha PD, et al. Identifying recurrence risk factors in CT-confirmed acute appendicitis in adults managed non-operatively during the COVID-19 pandemic. Cureus. 2022;14(9):e28794. doi: 10.7759/cureus.28794.
- Habeeb TAAM, Hussain A, Schlottmann F, et al. Recurrent appendicitis following successful drainage of appendicular abscess in adult without interval appendectomy during COVID-19. Prospective cohort study. Int J Surg. 2022;97:106200. doi: 10.1016/j.ijsu.2021.106200.
- Shindoh J, Niwa H, Kawai K, et al. Predictive factors for negative outcomes in initial non-operative management of suspected appendicitis. J Gastrointest Surg. 2010;14(2):309–314. doi: 10.1007/s11605-009-1094-1.
- Tsai HM, Shan YS, Lin PW, et al. Clinical analysis of the predictive factors for recurrent appendicitis after initial nonoperative treatment of perforated appendicitis. Am J Surg. 2006;192(3):311–316. doi: 10.1016/j.amjsurg.2005.08.037.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8.
- Steiner Z, Gilad Y, Gutermacher M, et al. Acute appendicitis in children: reexamining indications for conservative treatment – A large prospective analysis. J Pediatr Surg. 2022;57(10):373–379. doi: 10.1016/j.jpedsurg.2021.12.012.
- Liang T-J, Liu S-I, Tsai C-Y, et al. Analysis of recurrence management in patients who underwent nonsurgical treatment for acute appendicitis. Medicine. 2016;95(12):e3159. doi: 10.1097/MD.0000000000003159.
- Kaminski A, Liu IL, Applebaum H, et al. Routine interval appendectomy is not justified after initial nonoperative treatment of acute appendicitis. Arch Surg. 2005;140(9):897–901. doi: 10.1001/archsurg.140.9.897.
- Flum DR, Davidson GH, Monsell SE, et al. A randomized trial comparing antibiotics with appendectomy for appendicitis. N Engl J Med. 2020;383(20):1907–1919. doi: 10.1056/NEJMoa2014320.
- Shogilev DJ, Duus N, Odom SR, et al. Diagnosing appendicitis: evidence-based review of the diagnostic approach in 2014. West J Emerg Med. 2014;15(7):859–871. doi: 10.5811/westjem.2014.9.21568.
- Peltrini R, Cantoni V, Green R, et al. Risk of appendiceal neoplasm after interval appendectomy for complicated appendicitis: a systematic review and meta-analysis. Surgeon. 2021;19(6):e549–e58.