Abstract
This study examined whether time, treatment type, baseline individual differences, and treatment satisfaction affected the vaginal intercourse trajectories of women with Provoked Vestibulodynia (PVD) before and after psychological treatment. Women (N = 130) who received CBT or MBCT completed questionnaires prior to and 2-4 weeks, 6-, and 12-months following treatment. The odds of women engaging in vaginal penetration increased by 31% at each assessment. Baseline individual differences and treatment satisfaction predicted maintenance of or re-engagement in vaginal penetration at post-treatment. Findings suggest that women who refrain from vaginal intercourse after treatment differ from women who continue or resume this activity.
Introduction
Provoked vestibulodynia (PVD) is a distressing genito-pelvic pain condition characterized by burning pain elicited by contact to the vulvar vestibule, affecting at least 8% of women (Bornstein et al., Citation2016). PVD is associated with impairments in sexual function, and significant psychological and relational difficulties (Dargie, Gilron, & Pukall, Citation2017; Rosen, Santos-Iglesias, & Byers, Citation2017). Given that the primary symptom of PVD is pain during sexual activities involving pressure applied to the vulvar vestibule, the majority of studies evaluating interventions for PVD focus on two domains of outcome: intercourse pain intensity (primary) and sexual function (secondary) (Pukall et al., Citation2017). In this study, vaginal intercourse is defined broadly as any penetration of the vagina during sexual activity, regardless of the gender and anatomy of women’s sexual partners. Therefore, the terms vaginal penetration and vaginal intercourse will be used interchangeably.
Vaginal intercourse pain intensity is commonly assessed using a self-report numeric rating scale (NRS) ranging from 0 (no pain) to 10 (worst pain possible) (Dworkin et al., Citation2005; Pukall et al., Citation2017). Women who do not engage in vaginal intercourse before treatment are excluded from the analyses evaluating changes on this outcome measure. The Female Sexual Function Index (FSFI) (Rosen et al., Citation2000), a self-report questionnaire with solid psychometric properties and excellent discriminant validity, is the most widely used measure of sexual function in clinical trials for PVD (Masheb, Lozano-Blanco, Kohorn, Minkin, & Kerns, Citation2004; Pukall et al., Citation2017; Wiegel, Meston, & Rosen, Citation2005). However, FSFI scores for participants not engaging in vaginal penetration can be biased or entirely missing. This is because the scoring guidelines for the FSFI assign a zero score to anyone who has not been recently sexually active; unfortunately, this has the effect of falsely inflating dysfunction scores for sexually inactive respondents. This scoring practice has been criticized (Brotto, Citation2009; Gerstenberger et al., Citation2010; Meyer-Bahlburg & Dolezal, Citation2007). Further, women engaging in solely non-penetrative sexual activities rather than vaginal penetration receive a score of zero for the Pain subscale, also contributing to an overall lower FSFI total score and suggesting the presence of sexual dysfunction. In an attempt to limit the bias introduced by these scoring artifacts, some researchers exclude women not engaging in vaginal intercourse from analyses of the FSFI (Pukall et al., Citation2017). However, many PVD intervention studies do not explicitly state their data analysis procedures for this measure, or the number of women who may have been excluded due to lack of vaginal penetration. Overall, there is a paucity of research on women with PVD’s temporal patterns of engagement in vaginal penetration, despite reliance on this type of sexual activity for determining treatment efficacy.
Few studies report women’s vaginal intercourse trajectories with treatment for PVD, representing a significant gap in the literature. Findings from population-based studies indicating that >85% of women with vulvodynia reported vaginal intercourse in the past 6 months (Reed et al., Citation2012) may lead investigators to conclude that frequency of vaginal penetration is unaffected by PVD. However, data from intervention studies reveal that women seeking treatment for their PVD may differ from those in the general population, such that a sizeable minority appear to have stopped engaging in vaginal intercourse (Brotto, Basson, Smith, Driscoll, & Sadownik, Citation2015; Brotto et al., Citation2019; Lindström & Kvist, Citation2015; Smith, Sadownik, Dargie, Albert, & Brotto, Citation2019). For example, in a recent study of 316 women’s symptom trajectories after receiving multidisciplinary treatment for PVD, 25% of the sample did not attempt vaginal penetration in the 4 weeks before starting treatment (Smith et al., Citation2019). Similarly, a comparison of mindfulness-based cognitive therapy (MBCT) and cognitive behavioral therapy (CBT) for PVD in 130 women found that 51% of the sample reported no engagement in vaginal intercourse in the month before starting treatment (Brotto et al., Citation2019). Another intervention study examining efficacy of a four-session mindfulness-based group therapy for PVD found that the majority of their sample, 72% of the 85 participants, reported no vaginal penetration in the month prior to beginning the intervention (Brotto et al., Citation2019). In a study of desensitization therapy plus CBT, 27% reported no vaginal intercourse in the past year, and an additional 23% only engaged in this activity on 1-5 occasions during that time period (Lindström & Kvist, Citation2015). If women are unable to provide baseline scores for pain intensity and sexual function due to lack of vaginal penetration, they may be excluded from analyses of pain and sexual function at post-treatment, which directly impacts conclusions drawn about the efficacy of treatment.
A better understanding of the main goals of a particular treatment for PVD is key to predicting whether that treatment will impact resumption of vaginal penetration. CBT is a recommended first-line treatment for PVD and is a change oriented approach that directly targets avoidance behavior (Bornstein et al., Citation2016; Dunkley & Brotto, Citation2016). In contrast to CBT’s emphasis on change, mindfulness-based cognitive therapies are based on a foundation of acceptance and compassion (Dunkley & Brotto, Citation2016; Kabat-Zinn, Citation1982; Rosenbaum, Citation2013). MBCT does not use goal-oriented language when describing sexual activity and is therefore less likely to increase engagement in vaginal penetration relative to CBT (Dunkley & Brotto, Citation2016). Considering data from treatment studies showing that CBT increased vaginal intercourse frequency in women with lifelong vaginismus (ter Kuile et al., Citation2007), another genito-pelvic pain disorder, whereas MBCT had minimal impact on women with PVD’s reports of this activity (Brotto et al., Citation2015), CBT may be more likely than MBCT, overall, to lead to re-engagement in vaginal penetration.
We are not aware of studies investigating individual differences that may predict vaginal intercourse trajectories in women with PVD. We selected predictors of intercourse resumption based primarily on theory (fear-avoidance model of PVD), and available literature. The fear avoidance model (Lethem, Slade, Troup, & Bentley, Citation1983) and its expanded version (Vlaeyen & Linton, Citation2000) explains the psychological processes underpinning the transition from acute to chronic pain in patients with musculoskeletal disorders. This model posits that an initial pain experience generates catastrophic thoughts and pain-related fear, and these psychological phenomena lead to avoidance of pain-invoking activities. Avoidance strengthens fear and engenders hypervigilance of pain sensations, exacerbating the experience of pain, and a vicious cycle of chronic pain is born (Vlaeyen & Linton, Citation2000). Notably, this model was adapted for PVD (Bergeron, Rosen, & Morin, Citation2011) and states that a painful vaginal penetration experience can lead to catastrophic appraisals of pain and beliefs that vaginal intercourse is harmful. As a result, women avoid vaginal penetration to protect themselves from anticipated pain, and this avoidance increases negative affect, which intensifies the pain experience. Given the relevance of the fear-avoidance model of PVD for affected women’s engagement in vaginal penetration (or lack thereof), we used it alongside research findings to identify pretreatment predictors of vaginal intercourse trajectories.
Considering this theoretical model, treatment outcomes for women with PVD, especially the maintenance or resumption of vaginal intercourse, are likely influenced by the onset and intensity of one’s pain with penetration. Specifically, it is possible that a longer duration of PVD allows for the cycle of fear and avoidance to become more deeply rooted. In support of this notion, findings from recent studies suggest symptom onset at one’s first penetrative experience (i.e., lifelong PVD) and longer symptom duration may be associated with greater avoidance of vaginal penetration (Boerner & Rosen, Citation2015; Brotto et al., Citation2014; Lambert, Desrosiers, Chagnon, & Lepage, Citation2013; Reed, Haefner, & Cantor, Citation2003). The link between PVD subtype (lifelong versus acquired) and avoidance of vaginal penetration after receiving psychological treatment has yet to be explored, and the impact of treatment type (e.g., CBT vs. MBCT) on this relationship is unknown. Focusing on penetration pain intensity, based on the fear avoidance model we anticipate that more severe baseline pain will be associated with higher levels of fear and consequent avoidance. While we are not aware of any studies examining the direct relationship between pretreatment penetration pain and post-treatment engagement in vaginal intercourse for women with PVD, data from chronic pain populations lend support to this hypothesis, indicating that greater pain intensity is associated with less engagement in activities that give rise to pain sensations (Gutierrez et al., Citation2007; Rosemann, Kuehlein, Laux, & Szecsenyi, Citation2007; Tawashy, Eng, Lin, Tang, & Hung, Citation2009). Further, while both CBT and MBCT have proven effective in reducing women’s post-treatment penetration pain (Brotto et al., Citation2019), it is unknown whether the potential relationship between baseline pain severity and the occurrence of vaginal penetration differs according to treatment type (i.e., CBT vs. MBCT). Both CBT and MBCT aim to reduce penetration pain for women with PVD, although these interventions are theorized to achieve this endpoint via different mechanisms. While CBT challenges maladaptive pain-related cognitions and helps women build pain-relevant coping and self-management skills via behavioral intervention (Dunkley & Brotto, Citation2016), MBCT supports women to learn new ways of experiencing physical discomfort through nonjudgmental awareness and acceptance of physical sensations (Brotto et al., Citation2019). This study will examine the potentially different impact of those two treatments on the connection between baseline pain and engagement in vaginal penetration.
Considering psychological factors, the fear avoidance model adapted for PVD highlights pain catastrophizing as a potential contributor to avoidance of vaginal penetration, given that pain catastrophizing has been found to uniquely predict penetration pain intensity in women with PVD (Desrochers, Bergeron, Khalifé, Dupuis, & Jodoin, Citation2009). While studies examining chronic pain have found links between pain catastrophizing and avoidance of pain-invoking behaviors (e.g., Elfving, Andersson, & Grooten, Citation2007; Ruixie, Lynn, & Darnall, Citation2020), this construct has never been examined as a predictor of vaginal intercourse avoidance in women with PVD. Notably, CBT and MBCT employ different strategies to reduce levels of pain catastrophization. CBT relies on cognitive restructuring techniques to undermine maladaptive cognitions, and encourages women with PVD to actively disconfirm catastrophic thoughts about pain through vaginal dilation exercises (Dunkley & Brotto, Citation2016). Alternatively, MBCT supports women with PVD to develop mindful awareness (Schütze, Rees, Preece, & Schütze, Citation2010). A principal component of mindfulness is equanimity, which can be defined as an even-minded mental state toward all sensations, regardless of whether they are pleasant, unpleasant, or neutral (Desbordes et al., Citation2015). Thus, mindful awareness is theoretically incompatible with the relatively focused, selective attention that characterizes pain catastrophizing (Schütze et al., Citation2010; Sullivan, Lynch, & Clark, Citation2005). While both CBT and MBCT result in similar improvements in pain catastrophizing for women with PVD (Brotto et al., Citation2019), it is unknown whether the type of psychological treatment administered impacts associations between pretreatment pain catastrophizing and post-treatment avoidance of vaginal penetration.
While the fear-avoidance model posits that psychological reactions that attempt to manage or control pain via avoidance, such as pain catastrophizing, result in worsening of pain, acceptance of physical discomfort is a counterintuitive reaction that could prove adaptive (Boerner & Rosen, Citation2015). Specifically, chronic pain acceptance may impact willingness to engage in vaginal penetration, as greater acceptance of vulvovaginal pain has been linked with lower levels of sexual impairment in PVD (Boerner & Rosen, Citation2015). Considering that a key component of chronic pain acceptance is openness to experiencing pain sensations (Dewitte, Borg, & Lowenstein, Citation2018), it is possible that greater trait-level openness, a core facet of personality, may also be related to more engagement in vaginal intercourse in women with PVD, although to our knowledge this has never been explored. In contrast to CBT’s emphasis on change, primary goals of MBCT include fostering non-judgmental acceptance of the present moment, and adopting an open disposition to one’s experience, approaching all sensations with receptivity and curiosity (Dunkley & Brotto, Citation2016; van den Hurk et al., Citation2011). Importantly, researchers have found positive relationships between openness and facets of mindfulness (Baer, Smith, & Allen, Citation2004; Baer, Smith, Hopkins, Krietemeyer, & Toney, Citation2006; Brown & Ryan, Citation2003; van den Hurk et al., Citation2011). Considering the theoretical connections between mindfulness, chronic pain acceptance, and openness alongside the aforementioned empirical findings, it is possible that women with higher chronic pain acceptance and openness at baseline may have been more responsive to MBCT relative to CBT, and were more likely to continue to have or re-engage in vaginal penetration after treatment. Thus, we anticipate that predictive relationships between chronic pain acceptance and openness with post-treatment vaginal penetration will be stronger for women receiving MBCT vs. CBT.
With respect to other psychological factors related to components of the fear-avoidance model, anxiety has also been associated with preventative behaviors in studies of patients with chronic pain, including avoidance of pain-inducing activities (Lucchetti, Oliveira, Mercante, & Peres, Citation2012; Murphy, Lindsay, De, & Williams, Citation1997). In particular, anxiety has emerged as a possible predictor of whether vaginal intercourse might resume or not in PVD, such that women who were refraining from vaginal penetration prior to receiving multidisciplinary treatment self-reported higher levels of anxiety than women engaging in this activity (Desrochers, Bergeron, Landry, & Jodoin, Citation2008; ter Kuile & Weijenborg, Citation2006). We are not aware of any research showing that baseline levels of anxiety predict differential treatment outcomes for CBT vs. MBCT in individuals experiencing sexual dysfunction. Thus, we do not expect the relationship between pretreatment anxiety and post-treatment engagement in vaginal intercourse to be affected by the type of treatment received.
While identifying baseline predictors of treatment outcome (e.g. maintenance or resumption of vaginal intercourse) is essential to understanding who responds to treatment, and in what ways, treatment-related predictors of progress are of importance and are often overlooked. Within psychology research, treatment satisfaction has been theorized to play a crucial role in treatment compliance and completion, which may consequently impact clinical improvement (Cone, Citation2002). This idea is bolstered by empirical evidence, as a recent study found that levels of treatment satisfaction predicted post-treatment reductions in PTSD symptoms for combat veterans receiving a course of brief exposure-based psychotherapy (Gros, Gros, Acierno, Frueh, & Morland, Citation2013). Specifically, even when baseline predictors previously identified to predict post-treatment PTSD symptoms were investigated, including pretreatment PTSD symptoms, age, and ethnicity, treatment satisfaction remained a significant predictor of clinical improvement (Gros et al., Citation2013). In light of these findings, treatment satisfaction and other intervention-related predictors, such as perceptions of improvement during treatment, may be important for clinicians to monitor. Greater levels of treatment satisfaction and impressions of progress likely influence continuity of and engagement in treatment, potentially impacting treatment outcome.
This secondary data analysis was conducted to (1) Examine whether engagement in vaginal penetration was impacted by time (measured at 4 points) and the type of treatment women received (i.e., CBT or MBCT); (2) Establish individual vaginal penetration trajectories over the four assessment points (i.e., pretreatment, post-treatment, 6 months, and 12 months following psychological treatment for PVD); and (3) Investigate whether individual differences at pretreatment (i.e., duration of PVD symptoms, PVD subtype, penetration pain intensity, pain catastrophizing, chronic pain acceptance, openness, and anxiety) and treatment-related variables at 2-4 weeks post-treatment (i.e., treatment satisfaction and global impressions of change) predicted vaginal intercourse trajectories, and whether these relationships were impacted by treatment type (i.e., MBCT vs. CBT). This study will contribute to our understanding of the temporal patterns of vaginal penetration in women receiving treatment for PVD, with a focus on identifying individual patient differences that predict vaginal intercourse trajectories.
Materials and method
Participants
The data for this study were drawn from a clinical trial comparing Cognitive Behavioral Therapy (CBT) and Mindfulness Based Cognitive Therapy (MBCT) for PVD (Brotto et al., Citation2019). The sample consisted of 130 women with a physician-confirmed diagnosis of PVD seeking treatment. Participants were recruited from two tertiary care academic health centers that specialize in the treatment of PVD in a major metropolitan city.
Participants were required to meet the following inclusion criteria: (1) a diagnosis of PVD that was confirmed by a clinical history and a cotton-swab test conducted by a physician with expertise in sexual medicine; (2) a duration of PVD symptoms for at least 6 months; (3) able to attend 8 weekly treatment sessions; (4) were a minimum of 19 years of age and premenopausal; (5) able to read and write English fluently; (6) agreed not to start any new treatments for PVD for the duration of the study until 6 months following treatment completion. Women were not selected for participation if they met the following exclusion criteria: (1) experienced pelvic or vulvovaginal pain not related to intercourse or pressure to the vestibular area (e.g., generalized vulvodynia or deep pelvic pain); (2) a vulvar skin condition (e.g., lichen sclerosus); (3) significant symptoms of dissociation, as the tendency to dissociate would interfere with group MBCT. For information about recruitment numbers and about participants who dropped out at each follow-up time point, see the original publication (Brotto et al., Citation2019). Analyses revealed that women who dropped out of the study at the 6-month follow-up point did not differ from those who completed all follow-up assessments on characteristics listed in and , or on baseline variables of interest (Brotto et al., Citation2019).
Table 1. Sociodemographic information for the overall sample (N = 130), and for women who reported vaginal penetration 4 weeks prior to pretreatment (n = 64) and women who did not (n = 66).
Table 2. PVD related, psychological, and personality characteristics for the overall sample (N = 130), and for women who reported vaginal penetration 4 weeks prior to pretreatment (n = 64) and women who did not (n = 66).
Procedure
After providing written consent, and one week prior to beginning treatment all women completed a battery of questionnaires online, which were administered and stored in SurveyMonkey. Each participant was emailed an individualized link to the questionnaires, and the study coordinator sent reminder emails and/or telephone calls up to 3 times for any woman who did not complete these baseline items. In addition, women completed questionnaire batteries at post-treatment (i.e., 2-4 weeks after treatment), 6 months, and 12 months following treatment completion via the same method.
The original study was approved by the Clinical Research Ethics Board at the University of British Columbia, #H12-02358, as well as the Vancouver Coastal Health Hospital Research Ethics Board, and all participants provided written consent. This project was registered with clinicaltrials.gov, NCT01704456.
Treatments
Both treatments were 8 weeks in length and consisted of weekly 2.25 hr long sessions. Clinicians facilitated only one type of group (i.e., CBT or MBCT) and had specialized training in group therapy and experience in the diagnosis and treatment of PVD. Facilitators for the MBCT arm had received further mindfulness training.
Both treatment groups included psychoeducation about the effects of PVD on women’s sexual lives (e.g., desire, motivation, and function) as well as information on communication-skills training to assist women to speak to current or future sexual partners about their PVD symptoms. Facilitators invited women to temporarily stop engaging in sexual activities that they found painful, and instructions about a gradual re-introduction of vaginal penetration were given in parallel in both treatment arms. Additionally, the CBT intervention incorporated behavioral skills training (e.g., progressive relaxation, vaginal inserts, or challenging avoidance behavior) and cognitive techniques (e.g., cognitive restructuring), and was adapted from Bergeron and associates’ 10-session group CBT for PVD (Bergeron, Khalifé, Dupuis, & McDuff, Citation2016; Bergeron, Rosen, & Corsini-Munt, Citation2018; Bergeron et al., Citation2001).
The MBCT intervention was developed over five years by experts in sexual medicine and meditation, and involved guided mindfulness exercises including the body scan, mindfulness of breath, and a loving self-compassion practice (Basson et al., Citation2012). Women in this treatment arm also completed meditations in-session that involved either mindfully observing pain elsewhere in their body or eliciting low-intensity, non-genital pain sensations by holding their arm in the air for this purpose. For home practice, women were invited to provoke vestibular pain by touching the vaginal opening with their fingers while mindfully observing these sensations. Every session involved a 1-hour guided mindfulness practice followed by an inquiry on the practice. A central focus of the MBCT treatment was to further develop women’s metacognitive awareness (i.e., noticing thoughts and acknowledging their existence without judgment).
Measures
Demographics and PVD characteristics
At baseline participants provided demographic data including age, ethnicity, and education. Additionally, women responded to questions about aspects of their sexual and relationship history (e.g., sexual orientation, relationship status, and relationship duration). Participants also answered questions pertaining to their PVD (e.g., duration, subtype: lifelong or acquired PVD).
Pain Intensity
At the pretreatment assessment, women were asked to use a numeric rating scale (NRS) ranging from 0 (no pain) to 10 (worst pain imaginable) to indicate the intensity of their 1) usual provoked pain symptoms; 2) worst provoked pain symptoms; 3) pain symptoms during vaginal penetration in the previous 4 weeks. Participants who did not engage in vaginal penetration during the previous 4 weeks selected N/A (did not attempt vaginal penetration). This last pain rating was repeated at each data collection point.
Psychological function/personality
Pain catastrophizing
The Pain Catastrophizing Scale (Sullivan, Bishop, & Pivik, Citation1995; PCS) was used to assess a variety of pain-related thoughts and feelings. Women used a scale ranging from 0 (not at all) to 4 (all the time) to indicate how frequently they had a specific thought or feeling when they experienced vestibular pain. The PCS consists of three subscales: (1) rumination: inability to stop focusing on the pain; (2) magnification: fear of the pain worsening; (3) helplessness: feeling a lack of control over the pain. Total scores range from 0 to 52, with higher scores indicating greater catastrophizing. This measure demonstrated excellent internal consistency (α = 0.94 in our sample) and convergent validity with measures of perceptions of pain severity (r = .51) and pain interference (r = .57) (Osman et al., Citation2000).
Chronic pain acceptance
The Chronic Pain Acceptance Questionnaire (McCracken, Carson, Eccleston, & Keefe, Citation2004; CPAQ) was used to measure acceptance of vulvovaginal pain and is made up of 2 subscales. The Activity Engagement subscale consists of 11 items that assess the degree to which one continues to take part in life activities despite the presence of pain. The Pain Willingness subscale includes 9 items that measure the degree to which one is open to experiencing pain sensations rather than avoiding or controlling them. Women used a numeric rating scale ranging from 0 (never true) to 6 (always true) to rate the applicability of the 20 statements to their experience. Total scores were used in this study and range from 0 - 120, with higher scores suggesting greater pain acceptance overall. The CPAQ demonstrated strong internal consistency (α = 0.86 in our sample), and the Activity Engagement and Pain Willingness subscales show adequate discriminant validity with pain intensity and physical disability (Reneman, Dijkstra, Geertzen, & Dijkstra, Citation2010).
Personality
The Ten-Item Personality Inventory (Gosling, Rentfrow, & Swann, Citation2003; TIPI) was administered and although it assesses openness, conscientiousness, extraversion, agreeableness, and emotional stability, we only analyzed openness in this study. Women were asked to respond to 10 statements, 2 for each of the aforementioned dimensions of personality, using a Likert scale ranging from 1 (disagree strongly) to 7 (agree strongly). Split half reliabilities for each of the five dimensions were assessed by Spearman-Brown coefficients, given that each dimension was measured by only two items. The Spearman-Brown coefficients for each dimension in the current sample were: 0.36 for openness, 0.62 for extraversion, 0.19 for agreeableness, 0.60 for conscientiousness, and 0.59 for emotional stability. The scale has adequate test-retest reliability (r = 0.72) and strong convergent validity with the Big Five Inventory (rs for individual traits = 0.65 - 0.87) (Benet-Martínez & John, Citation1998; John & Srivastava, Citation1999).
Anxiety
The Anxiety Sensitivity Index (Taylor et al., Citation2007; ASI-3) was used to measure participants’ concerns related to the possible negative consequences of anxiety symptoms. Women responded to 18 items using a 5-point Likert scale ranging from 0 (very little) to 4 (very much). Total scores ranged from 0 to 72, with higher scores indicating greater levels of anxiety sensitivity. The ASI-3 demonstrated excellent internal consistency in the current sample (α = 0.94). The scale exhibits strong convergent validity with the panic subscale of the Inventory of Depression and Anxiety Symptoms (Watson et al., Citation2007; r =.50-.54), which assesses anxious arousal.
Global impression of change and treatment satisfaction
The Patient Global Impression of Change questionnaire assessed the degree that women’s penetration pain and overall quality of sexual life changed after treatment. Women were asked to complete 2 separate items to rate the degree of improvement in 1) penetration pain on a 6-point scale ranging from 1 (complete recovery – no more pain) to 6 (deterioration); and 2) overall quality of sexual life on a 6-point scale ranging from 1 (great improvement) to 6 (deterioration). These items were not combined, yielding separate scores for improvements in penetration pain and sex life quality. Women reported their global satisfaction with treatment using a 11-point scale ranging from 0 (completely dissatisfied) to 10 (completely satisfied). The aforementioned items were drawn from a similar measure employed in an RCT that assessed group CBT for women with PVD (Bergeron et al., Citation2001).
Overview of analyses
Sample size
This is a secondary data analysis so no power based sample calculation was performed. The study was fully powered to test the original hypotheses and the details of the power analysis are described in the original publication (Brotto et al., Citation2019). Intention to treat analysis (ITT), a conservative method that retains sample size while maintaining the comparability of randomized groups (Newell, Citation1992), was used for the analysis of vaginal penetration rate changes (n = 130). The analysis of predictors of different individual vaginal penetration trajectories used only the participants with data from at least 2 time points. Due to attrition at each follow-up assessment, a sample of n = 116 was used for those analyses. Women who were not included in those analyses due to missing data did not differ from women who were included on characteristics listed in and , or any of the baseline variables of interest.
Analysis of the effects of time and treatment group on vaginal penetration rates
Generalized Linear Mixed Models (GLMM) were used to examine the effects of time and treatment group on changes in the proportion of women with PVD engaging in vaginal penetration over four time points (pretreatment, post-treatment, 6 months-, and 12 months-follow-up). Specifically, we ran a GLMM model using time as a continuous predictor and treatment group (i.e., CBT vs. MBCT) as a nominal predictor, examining the interaction between these two factors on the proportion of women reporting vaginal penetration. Random intercept was included in the model.
Analysis of predictors of vaginal penetration trajectories
There were four trajectory groups which we defined as follows: (1) No Vaginal Penetration – no vaginal penetration at any time point; (2) Continuous Vaginal Penetration – vaginal penetration at every time point; (3) Resumed Vaginal Penetration – women who re-engaged in vaginal penetration at one of the post-treatment assessment points; and (4) Stopped Vaginal Penetration – women who stopped vaginal penetration at one of the post-treatment assessment points (and did not re-engage at later points). Multinomial logistic regression analyses were performed to evaluate seven baseline and three treatment-related predictors of the aforementioned vaginal penetration trajectory group membership. Multinomial logistic regression evaluates the degree to which independent variables predict membership to one or more groups relative to a reference group. Baseline predictors included duration of PVD symptoms, PVD subtype (i.e., lifelong or acquired), and baseline penetration pain intensity, pain catastrophizing, chronic pain acceptance, openness, and anxiety. Treatment-related predictors included global treatment satisfaction at post-treatment, impression of improvement in overall quality of sexual life and impression of change in penetration pain. All models included age as a control variable and an interaction between treatment and the focal predictor. We did not have any specific hypotheses for interactions between treatment modality and treatment-related predictors but examined them for the sake of completeness. In all models, the No Vaginal Penetration group served as a reference group except for the improvement in penetration pain predictor for which that group had no data therefore the Stopped Vaginal Penetration group served as the reference group.
Results
Sample characteristics
Of the 130 women who participated, 64 (49%) reported engaging in vaginal intercourse in the 4 weeks prior to their pretreatment assessment. For the 51% of women who did not have vaginal intercourse in the previous 4 weeks, 29 (45%) said that they expected vaginal penetration to be too painful, 14 (22%) were advised by a clinician not to have vaginal penetration, 12 (18%) reported that they did not have a sexual partner, and 10 (15%) disclosed other reasons. Group comparisons revealed that women who reported engaging in vaginal intercourse at baseline were younger, t(128) = 2.21, p = .029, reported lower penetration pain intensity, t(128) = 2.37, p = .019, and greater openness, t(127) = −2.07, p = .041. There were no other significant differences on sociodemographic (), PVD-related, psychological, or personality characteristics () between these groups.
Effects of time and treatment group on vaginal intercourse rates
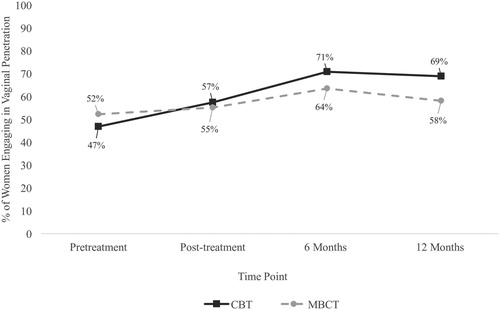
We conducted generalized linear mixed models using binomial regression and a logit function to examine the effects of time and treatment group (i.e., CBT vs. MBCT) on the proportion of women engaging in vaginal penetration to determine a) whether women were more likely to have vaginal penetration at post-treatment time points, and b) whether engagement in sexual activity was affected by treatment group. We found a main effect of time, F(1,427) = 7.44, p = .007 with OR = 1.31, 95% CI [1.08, 1.59], p = .007, indicating that on average a woman’s odds of having vaginal penetration increased by a factor of 1.31 (i.e., 31%) with each subsequent time point (time was modeled as continuous). The descriptive statistics show that approximately half of our sample (49%) reported vaginal penetration at pretreatment, and this proportion increased to 56% at post-treatment, 67% at 6 months-, and stabilized at 64% at 12 months-follow-up. Of note, these percentages represent the proportion of women who indicated that they had engaged in vaginal penetration during the 4 weeks prior to the time point indicated. There was no main effect of treatment group, F(1,425) = 0.76, p = .384, and no time by treatment group interaction, F(1,425) = 1.58, p = .209, indicating that a similar proportion of women reported engagement in vaginal intercourse in both the CBT and MBCT arms (see ).
Vaginal penetration trajectories
For the 116 women analyzed, there were 18 (16%) in the No Vaginal Penetration group, 33 (28%) in the Continuous Vaginal Penetration group, 50 (43%) in the Resumed Vaginal Penetration group, and 15 (13%) in the Stopped Vaginal Penetration group.
Baseline predictors
All models controlled for age. Treatment group did not significantly interact with any predictors other than baseline chronic pain acceptance; therefore, the statistics for that interaction are described below while the details of all the main effects are reported in . Chronic pain acceptance interacted with treatment group to predict greater likelihood of membership to the Resumed Vaginal Penetration group compared to the No Vaginal Penetration group (b = −.12, SE = .04, p = .007). To probe the interaction, simple effects were computed separately for MBCT and CBT groups. MBCT receiving women were more likely to resume vaginal penetration if their chronic pain acceptance at pretreatment was higher (b = .07, SE = .03, OR = 1.07, p = .011) whereas the opposite was found for CBT participating women. Those with lower pretreatment pain acceptance were more likely to resume vaginal penetration (b = −.08, SE = .05, OR = 0.92, p = .070), however, this effect only reached marginal significance.
Table 3. Effects of baseline and treatment-related predictors on membership to the Continuous, Resumed, and Stopped Vaginal Penetration groups relative to the No Vaginal Penetration group expressed as betas, odds ratios and 95% confidence intervals, adjusted for age.
Across the groups, baseline penetration pain intensity, pain catastrophizing, chronic pain acceptance, and openness were significant predictors of vaginal intercourse trajectories (). Specifically, lower penetration pain intensity and pain catastrophizing, and higher chronic pain acceptance and openness predicted greater likelihood of being in the Continuous Vaginal Penetration group relative to the No Vaginal Penetration group. No other baseline variables were found to predict membership to the Continuous Vaginal Penetration group. Lower pain catastrophizing emerged as a significant predictor of membership to the Resumed Vaginal Penetration group although this main effect is qualified by the interaction described above. None of our predictors (i.e., PVD symptom duration, PVD subtype, baseline penetration pain intensity, pain catastrophizing, chronic pain acceptance, openness, or anxiety) predicted membership to the Stopped Vaginal Penetration group relative to the No Vaginal Penetration group.
Treatment-related predictors
Treatment group did not significantly interact with any of the treatment-related predictors. When controlling for age, both global impression of treatment satisfaction and change for overall quality of sexual life at post-treatment were significant predictors of vaginal intercourse trajectories (). Specifically, greater treatment satisfaction predicted greater likelihood of membership to the Resumed Vaginal Penetration group relative to the No Vaginal Penetration group, but was not a significant predictor of membership to the Continuous or Stopped Vaginal Penetration groups. Additionally, perceptions of greater treatment-related improvement for one’s sexual life predicted membership to both the Continuous Vaginal Penetration and Resumed Vaginal Penetration groups relative to the No Vaginal Penetration group but was not a significant predictor of membership in Stopped Vaginal Penetration group. Finally, global impressions of treatment-related change for penetration pain did not emerge as a significant predictor of vaginal intercourse trajectories.
Discussion
Summary of findings
This study examined the impact of psychological treatment on vaginal penetration in women with PVD up to 12-months post-treatment. We examined whether PVD-related, psychological, and personality characteristics at pretreatment and treatment-related variables at post-treatment predicted these vaginal intercourse trajectories, whether these relationships were impacted by treatment group, and if women continued to have penetration, resumed it, or stopped it.
The proportion of women engaging in vaginal penetration increased from 49% at baseline to 64% at 12 months post-treatment, with no effect of treatment type on women’s engagement in vaginal penetration, suggesting that CBT and MBCT were similarly effective at reducing avoidance of vaginal penetration and allowing women to resume penetrative sexual activity. Regarding vaginal intercourse trajectories, our results indicated that, as would be expected from the above finding of an increase in rates post-treatment, the largest group (43%) resumed vaginal penetration after receiving treatment. Approximately a quarter of our sample (28%) engaged in vaginal intercourse before and after treatment, reporting vaginal penetration at all time points. A total of 16% of women reported no engagement in vaginal penetration in the month prior to treatment onset, and did not resume vaginal intercourse at any time after treatment. Lastly, 13% of women were engaging in vaginal penetration at baseline and then stopped after treatment.
Concerning individual differences at pretreatment that predicted vaginal intercourse trajectories, consistent with our predictions, women who reported lower pain intensity, less pain catastrophizing, higher chronic pain acceptance, and greater openness were more likely to report engaging in vaginal penetration at all time points than to report no engagement in penetrative sex at all four times. Also consistent with our predictions, women who reported less pain catastrophizing were more likely to resume vaginal penetration post-treatment than to report no vaginal intercourse at any time point. Further, in line with our expectations, women with higher chronic pain acceptance who received MBCT were more likely to resume vaginal penetration following treatment, whereas the opposite relationship existed in the CBT group, although it did not reach statistical significance. Contrary to our hypotheses, PVD symptom duration, PVD subtype, baseline pain intensity, chronic pain acceptance, openness, and anxiety did not predict which women resumed vaginal penetration. Additionally, other than chronic pain acceptance, no other baseline or treatment-related predictors interacted with treatment modality to predict women’s vaginal intercourse trajectories.
Considering perceptions of treatment as predictors of vaginal intercourse trajectories, women who reported greater impressions of improvement in quality of sexual life at post-treatment were more likely to engage in vaginal penetration at all time points or to resume this activity at post-treatment or a follow-up time point than report no vaginal intercourse. Further, women who reported higher levels of global satisfaction with treatment were more likely to re-engage in vaginal penetration than to indicate no engagement in this activity. However, no treatment satisfaction measures predicted the women who stopped engaging in vaginal penetration. Of note, global impressions of change in penetration pain with treatment was not a significant predictor of women’s temporal patterns of vaginal intercourse, suggesting that resuming or maintaining vaginal penetration may be related to factors other than pain reduction.
No differential impact of treatment type
This study shed light on women with PVD’s temporal patterns of vaginal penetration before and after receiving treatment. Given that the largest vaginal intercourse trajectory group, 50 of 116 participants (43%), was comprised of women who re-engaged in vaginal intercourse post-treatment, we might conclude that CBT and MBCT are effective in reducing avoidance of vaginal penetration. This result complements the recent finding that both CBT and MBCT effectively improve symptoms of pain intensity, sexual dysfunction, and sex-related distress in women with PVD (Brotto et al., Citation2019).
Given that CBT directly targets avoidance of pain-related thoughts and experiences in order to reduce avoidant behavior, whereas MBCT fosters acceptance of these phenomena, the finding that both treatments similarly impacted women’s re-engagement in vaginal penetration was unexpected. In support of our results, a recent RCT comparing the efficacy of mindfulness-based stress reduction (MBSR) to CBT and usual care for patients with chronic lower back pain revealed that both MBSR and CBT resulted in greater improvement in functional limitation at 26 and 52 weeks relative to usual care. Importantly, these findings indicate that MBSR and CBT were similarly effective in reducing patients’ functional limitations (Cherkin et al., Citation2016). Although both CBT and MBCT had similar efficacy for most outcomes with PVD (Brotto et al., Citation2019), one of the few studies that examined mediators of therapeutic change found both shared and unique mechanisms underlying the improvements seen with MBCT vs CBT (Brotto, Bergeron, Zdaniuk, & Basson, Citation2020). Focusing on shared mechanisms, pain catastrophizing and pain acceptance willingness mediated improvements in pain and sexual distress in both MBCT and CBT (Brotto et al., Citation2020). Decreases in catastrophic penetration beliefs were also found to predict engagement in vaginal intercourse in a study that examined mediators of treatment outcome for women receiving treatment for vaginismus, a distinct but often co-occurring sexual concern (ter Kuile, Melles, Tuijnman-Raasveld, de Groot, & van Lankveld, Citation2015). Chronic pain acceptance, which encompasses pain willingness, has been linked to participation in pain-inducing activities (Boerner & Rosen, Citation2015; Brotto et al., Citation2020). Given these shared mediators for improvement of PVD symptoms following MBCT and CBT, and the present findings that the two treatments did not differ in predicting vaginal penetration resumption, we conclude that when the primary treatment goal is intercourse resumption, either treatment may be recommended. However, we acknowledge that this claim would be strengthened through the replication of our findings, highlighting the importance of including measures of vaginal intercourse re-engagement in future PVD treatment studies.
Who is most likely to engage in vaginal penetration?
Low levels of pain catastrophizing emerged as the sole baseline predictor (independent of treatment modality) of women’s re-engagement in vaginal intercourse at post-treatment in the current study. This finding is in line with the fear-avoidance model and its adapted version, which assert that individuals who catastrophize about their pain have a tendency to experience greater protective fear (Lethem et al., Citation1983; Vlaeyen & Linton, Citation2000). The model posits that the exacerbation of this fear can lead to avoidance of pain-inducing activities (Lethem et al., Citation1983; Vlaeyen & Linton, Citation2000), namely vaginal penetration for women with PVD. Further, pain catastrophizing has been found to uniquely predict variance in vaginal intercourse pain in women with PVD (Desrochers et al., Citation2009), indicating that this cognitive process may directly contribute to the aggravation of penetration pain. Considering these findings in tandem with those of a recent study that identified pain catastrophizing as a mediator of treatment efficacy after CBT and MBCT (Brotto et al., Citation2020), we can conclude that lower levels of pain catastrophizing meant less avoidance behavior, more engagement with the treatments delivered, and hence overall higher resumption of vaginal penetration.
Chronic pain acceptance also predicted which women re-engaged in vaginal penetration, but only when treatment group was taken into consideration. The finding that women with high chronic pain acceptance who received MBCT were more likely to resume vaginal intercourse than women with similar levels of chronic pain acceptance in the CBT group is not unexpected; however, this result constitutes a novel contribution to PVD literature. It is possible that women who were accepting of their pain sensations at the beginning of treatment were more likely to undertake meditation exercises that involved practicing mindful awareness of vulvovaginal pain that they provoked themselves, perhaps giving them confidence to employ mindfulness skills during other vaginal penetration experiences, resulting in less avoidance.
Higher chronic pain acceptance at pretreatment also predicted continuous engagement in rather than ceasing of vaginal intercourse, supporting the consensus in chronic pain research that higher pain acceptance predicts participation in activities that elicit pain (Gutierrez et al., Citation2007; Rosemann et al., Citation2007; Tawashy et al., Citation2009). These results are in agreement with findings from a cross-sectional study suggesting that women with PVD’s greater acceptance of their own vulvovaginal pain was associated with greater sexual functioning and satisfaction (Boerner & Rosen, Citation2015). Thus, it is possible that women with PVD who are more accepting of their pain may be motivated to pursue ongoing partnered penetrative sexual activity despite pain, shifting their focus to positive aspects of the sexual experience and likely the rewards of sexual activity (Boerner & Rosen, Citation2015). One interpretation of these findings is that women who are unable to accept their vulvovaginal pain may be at risk for ongoing disengagement of sexual activity despite treatment.
Two additional pretreatment variables predicted women who continued to have vaginal penetration throughout and after treatment; namely, pain intensity and openness. Not surprisingly, women who reported lower penetration pain intensity were more likely to have continuous vaginal penetration. Our results are consistent with observations from a separate study that women receiving CBT for PVD who had greater baseline penetration pain ratings were less likely to have vaginal penetration post-treatment than women with less severe pain at pretreatment (ter Kuile & Weijenborg, Citation2006). Another way of interpreting our findings is that higher baseline pain intensity would predict lack of engagement in vaginal penetration.
Our study was the first to evaluate trait-level openness as a predictor of engagement in vaginal penetration in women with PVD given that openness to experiencing pain sensations is a component of chronic pain acceptance (Dewitte et al., Citation2018). Women who scored higher on openness to experience were more likely to report vaginal intercourse at every time point than disengagement in this activity. Although previous studies have not investigated associations between openness and engagement in vaginal penetration, a recent meta-analysis revealed that openness was positively related to sexual satisfaction and desire, and negatively related to sexual dysfunction (Allen & Walter, Citation2018). It is possible that higher openness predicts ongoing engagement in vaginal intercourse because of its association with higher overall sexual functioning and satisfaction. In other words, women with more openness experience more sexual satisfaction leading them to seek out sexual activity. Given that the current study design did not allow us to evaluate directionality, it is also possible that openness leads to more engagement in sex, and then higher sexual satisfaction. Future studies should seek to evaluate the directionality of these relationships.
In addition to baseline predictors, we evaluated treatment-related predictors of vaginal intercourse activity. Perceptions of improvements in overall quality of sexual life predicted both the continuation of and re-engagement in vaginal penetration after treatment, regardless of treatment type. For women who reported having vaginal intercourse at all time points, it is possible that treatment-related enhancement of their sexual relationship motivated them to continue engaging in vaginal penetration despite pain. For women who resumed vaginal intercourse at a time point following treatment, improvements in non-penetrative forms of sexual intimacy, such as sensual touch, kissing, or oral sex may have encouraged them to attempt vaginal intercourse. Higher levels of treatment satisfaction also predicted the resumption of vaginal penetration. Women who were satisfied with treatment, regardless of whether it was MBCT or CBT, and perceived an overall improvement in their sex life due to treatment were more likely to resume vaginal penetration. These findings point to the importance of global clinical significance of treatment beyond specific symptom improvement.
Who is most likely to not engage in vaginal penetration?
Notably, a sizeable minority of our sample (n = 18; 16%) did not engage in vaginal intercourse at post-treatment, and an additional 13% had stopped vaginal intercourse following treatment. None of our baseline pain-related, personality, or treatment satisfaction related variables could predict this group of women not engaged in vaginal penetration. From a study design perspective, this finding is notable given that most treatment studies use measures of improvement that rely on engagement in vaginal penetration (e.g., numeric rating scale, global measures of sexual functioning). Therefore, women who have disengaged from vaginal penetration will not be included in analyses, and thus, conclusions drawn are only generalizable to the women who resume vaginal intercourse. From a clinical implications perspective, our findings fall short in guiding the clinician as to which variables may predict which women do not engage in sexual activity. It is likely that a broader selection of predictors might have predicted this trajectory group given evidence that self-rated health, poor quality of life, depression, and loss of a partner are significant predictors of sexual activity in a large sample of women (Gass et al., Citation2011). It is worth noting that women with PVD may have had different goals for treatment, and for some, the lack of vaginal penetration might not have been experienced as distressing, especially if they experienced improvements in other domains.
Study implications
The value of this study is expressed in both its novel findings and the important questions it raises with respect to baseline and treatment-related characteristics that predict vaginal intercourse trajectories. Although we observed a significant increase in rates of vaginal penetration following both CBT and MBCT, and a large group of women resumed vaginal intercourse post-treatment, we know very little about baseline characteristics that predict this outcome. Put more simply, our analyses revealed a number of pretreatment variables that separated women with PVD who persisted with vaginal intercourse from those who consistently avoided this form of sexual activity. Our results identified lower baseline pain, lower pain catastrophizing, higher pain acceptance, and higher trait-level openness as predictors of penetrative sexual activity following treatment. Low pain catastrophizing, irrespective of treatment modality, was the only baseline predictor of re-engagement in vaginal penetration. Notably, for women in the MBCT group only, high pretreatment chronic pain acceptance was a predictor of vaginal intercourse resumption. Two treatment-related variables (i.e., greater satisfaction and higher ratings of change in quality of sexual life at post-treatment) predicted a transition from avoidance to the resumption of vaginal penetration. Thus, psychological treatment for PVD may support some women to re-engage in vaginal penetration regardless of their baseline characteristics, but the treatment specific mechanisms responsible for this change require further investigation. Additionally, if the goal of treatment is re-engagement in vaginal penetration, women with high chronic pain acceptance at baseline may benefit more from a MBCT rather than CBT approach. It is also worth mentioning that psychological predictors of vaginal penetration activity appear to be more useful than using PVD-related characteristics (e.g., PVD subtype, years since diagnosis) to estimate engagement in sexual activity.
Limitations
We asked about vaginal intercourse engagement as a dichotomous yes/no question and this limited our ability to examine vaginal intercourse frequency, a more nuanced snapshot of motivations and barriers to re-engaging in vaginal penetration. Further, non-penetrative sexual activities were not assessed, and whether CBT and MBCT differentially impact such activities warrants investigation. Also, given that approximately 15% of our sample were single it is possible that limited access to sexual partners could have contributed to a lack of engagement in vaginal intercourse for certain participants. Moreover, variables that were not assessed and have shown strong associations with sexual outcomes in PVD, such as body exposure anxiety, depressive symptoms, and relationship intimacy may have impacted engagement in vaginal intercourse and should be the focus of future research (Bois, Bergeron, Rosen, McDuff, & Grégoire, Citation2013; Maillé, Bergeron, & Lambert, Citation2015; Rosen, Muise, Bergeron, Impett, & Boudreau, Citation2015). Finally, although the study was fully powered to test the original hypotheses, we acknowledge that the secondary data analysis presented in this publication may have been underpowered. Thus, we interpret null findings with caution, and encourage researchers to include non-significant predictors of vaginal intercourse trajectories (e.g., baseline pain and anxiety) in future studies on this topic.
Conclusion
Our findings provide new data showing that MBCT and CBT lead to significantly increased rates of vaginal penetration, but that 29% of women either do not engage in penetration at any point or have stopped vaginal penetration. Given the sizeable nature of the latter group, researchers conducting treatment studies should consider measures of progress that do not rely on engagement in vaginal intercourse, and this may limit the utility of the FSFI for this population. Finally, there are a number of baseline predictors of avoidance of vaginal penetration; namely, higher baseline penetration pain intensity, greater pain catastrophizing, lower chronic pain acceptance, and lower openness to experience. For women with these characteristics, it would be especially important to identify outcomes that do not depend on penetrative sexual activity. Low pain catastrophizing at pretreatment is especially relevant to assess given that it predicted likelihood of re-engagement in vaginal intercourse. Clinicians should also determine women’s chronic pain acceptance at pretreatment, as women with greater pain acceptance may improve more with MBCT than CBT with respect to avoidance of vaginal penetration. Finally, there are treatment-related improvements in sex life quality associated with the maintenance and resumption of vaginal penetration. Future studies should seek to understand the experiences of women with PVD who have chosen not to engage in vaginal intercourse, in an attempt to develop treatments that will better meet their needs.
Additional information
Funding
References
- Allen, M. S., & Walter, E. E. (2018). Linking big five personality traits to sexuality and sexual health: A meta-analytic review. Psychological Bulletin, 144(10), 1081–1110. doi:10.1037/bul0000157
- Baer, R. A., Smith, G. T., & Allen, K. B. (2004). Assessment of mindfulness by self-report: The Kentucky inventory of mindfulness skills. Assessment, 11(3), 191–206. doi:10.1177/1073191104268029
- Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. doi:10.1177/1073191105283504
- Basson, R., Brotto, L. A., Carlson, M., Driscoll, M., Grabovac, A., & Smith, K. B. (2012). Moving on with our sexual lives despite painful penetration from Provoked Vestibulodynia and pelvic muscle tension: A mindfulness-based approach. [Unpublished treatment manual]. Department of Obstetrics & Gynaecology, University of British Columbia.
- Benet-Martínez, V., & John, O. P. (1998). Los Cinco Grandes across cultures and ethnic groups: Multitrait-multimethod analyses of the Big Five in Spanish and English. Journal of Personality and Social Psychology, 75(3), 729–750. doi:10.1037/00223514.75.3.729
- Bergeron, S., Binik, Y. M., Khalifé, S., Pagidas, K., Glazer, H. I., Meana, M., & Amsel, R. (2001). A randomized comparison of group cognitive–behavioral therapy, surface electromyographic biofeedback, and vestibulectomy in the treatment of dyspareunia resulting from vulvar vestibulitis. Pain, 91(3), 297–306. https://doi.org/10.1016/s0304-3959(00)00449-8
- Bergeron, S., Khalifé, S., Dupuis, M. J., & McDuff, P. (2016). A randomized clinical trial comparing group cognitive-behavioral therapy and a topical steroid for women with dyspareunia. Journal of Consulting and Clinical Psychology, 84(3), 259–268. doi:10.1037/ccp0000072
- Bergeron, S., Rosen, N. O., & Corsini-Munt, S. (2018). Treating the patient with genito-pelvic pain. In D. C. Turk & R. J. Gatchel (Eds.), Psychological approaches to pain management: A practitioner's handbook (p. 458–472). The Guilford Press.
- Bergeron, S., Rosen, N.O., & Morin, M. (2011). Genital pain in women: Beyond interference with intercourse. Pain, 152, 1223–1225. doi:10.1016/j.pain.2011.01.035
- Boerner, K. E., & Rosen, N. O. (2015). Acceptance of vulvovaginal pain in women with provoked vestibulodynia and their partners: Associations with pain, psychological, and sexual adjustment. The Journal of Sexual Medicine, 12(6), 1450–1462. doi:10.1111/jsm.12889
- Bois, K., Bergeron, S., Rosen, N. O., McDuff, P., & Grégoire, C. (2013). Sexual and relationship intimacy among women with provoked vestibulodynia and their partners: Associations with sexual satisfaction, sexual function, and pain self-efficacy. The Journal of Sexual Medicine, 10(8), 2024–2035. doi:10.1111/jsm.12210
- Bornstein, J., Goldstein, A. T., Stockdale, C. K., Bergeron, S., Pukall, C., Zolnoun, D., … The International Pelvic Pain Society (IPPS). (2016). 2015 ISSVD, ISSWSH and IPPS consensus terminology and classification of persistent vulvar pain and vulvodynia. Obstetrics and Gynecology, 127(4), 745–751. doi:10.1097/AOG.0000000000001359
- Brotto L. A. (2009). Improving the Female Sexual Function Index [Letter to the Editor]. Journal of Sex & Marital Therapy, 35(2), 83–85. doi:10.1080/00926230802712327
- Brotto, L. A., Basson, R., Smith, K. B., Driscoll, M., & Sadownik, L. (2015). Mindfulness-based group therapy for women with provoked vestibulodynia. Mindfulness, 6(3), 417–432. doi:10.1007/s12671-013-0273-z
- Brotto, L. A., Bergeron, S., Zdaniuk, B., & Basson, R. (2020). Mindfulness and cognitive behavior therapy for provoked vestibulodynia: Mediators of treatment outcome and long-term effects. Journal of consulting and clinical psychology, 88(1), 48–64. doi:10.1037/ccp0000473
- Brotto, L. A., Bergeron, S., Zdaniuk, B., Driscoll, M., Grabovac, A., Sadownik, L. A., … Basson, R. (2019). A comparison of mindfulness-based cognitive therapy vs. cognitive behavioral therapy for the treatment of provoked vestibulodynia in a hospital clinic setting. The Journal of Sexual Medicine, 16(6), 909–923. doi:10.1016/j.jsxm.2019.04.002
- Brotto, L. A., Sadownik, L. A., Thomson, S., Dayan, M., Smith, K. B., Seal, B. N., … Zhang, A. (2014). A comparison of demographic and psychosexual characteristics of women with primary versus secondary provoked vestibulodynia. The Clinical Journal of Pain, 30(5), 428–435. doi:10.1097/AJP.0b013e31829ea118
- Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84, 822–848. doi:10.1037/0022-3514.84.4.822
- Cherkin, D. C., Sherman, K. J., Balderson, B. H., Cook, A. J., Anderson, M. L., Hawkes, R. J., … Turner, J. A. (2016). Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: A randomized clinical trial. Journal of the American Medical Association, 315 (12): 1240–1249. doi:10.1001/jama.2016.2323
- Cone, J. D. (2002). Evaluating outcomes: Empirical tools for effective practice. American Psychological Association.
- Dargie, E., Gilron, I., & Pukall, C. F. (2017). Provoked Vestibulodynia: A comparative examination of mental health, sleep, sexual functioning, and relationship adjustment. The Clinical Journal of Pain, 33(10), 870–876. doi:10.1097/AJP.0000000000000480
- Desbordes, G., Gard, T., Hoge, E. A., Hölzel, B. K., Kerr, C., Lazar, S. W., … Vago, D. R. (2015). Moving beyond mindfulness: Defining equanimity as an outcome measure in meditation and contemplative research. Mindfulness, 6(2), 356–372. doi:10.1007/s12671-013-0269-8
- Desrochers, G., Bergeron, S., Khalifé, S., Dupuis, M. J., & Jodoin, M. (2009). Fear avoidance and self-efficacy in relation to pain and sexual impairment in women with provoked vestibulodynia. The Clinical Journal of Pain, 25(6), 520–527. doi:10.1097/AJP.0b013e31819976e3
- Desrochers, G., Bergeron, S., Landry, T., & Jodoin, M. (2008). Do psychosexual factors play a role in the etiology of provoked vestibulodynia? A critical review. Journal of Sex & Marital Therapy, 34(3), 198–226. doi:10.1080/00926230701866083
- Dewitte, M., Borg, C., & Lowenstein, L. (2018). A psychosocial approach to female genital pain. Nature Reviews Urology, 15(1), 25–41. doi:10.1038/nrurol.2017.187
- Dunkley, C. R., & Brotto, L. A. (2016). Psychological treatments for provoked vestibulodynia: Integration of mindfulness-based and cognitive behavioral therapies. Journal of Clinical Psychology, 72(7), 637–650. doi:10.1002/jclp.22286
- Dworkin, R. H., Turk, D. C., Farrar, J. T., Haythornthwaite, J. A., Jensen, M. P., Katz, N. P., … IMMPACT. (2005). Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain, 113(1-2), 9–19. doi:10.1016/j.pain.2004.09.012
- Elfving, B., Andersson, T., & Grooten, W.J.A. (2007). Low levels of physical activity in back pain patients are associated with high levels of fear-avoidance beliefs and pain catastrophizing. Physiotherapy Research International, 12(1), 14–24. doi:10.1002/pri.355
- Gass, M. L., Cochrane, B. B., Larson, J. C., Manson, J. E., Barnabei, V. M., Brzyski, R. G., … Barad, D. H. (2011). Patterns and predictors of sexual activity among women in the Hormone Therapy trials of the Women's Health Initiative. Menopause (New York, N.Y.), 18(11), 1160–1171. doi:10.1097/gme.0b013e3182227ebd
- Gerstenberger, E. P., Rosen, R. C., Brewer, J. V., Meston, C. M., Brotto, L. A., Wiegel, M., & Sand, M. (2010). Sexual desire and the Female Sexual Function Index (FSFI): A sexual desire cutpoint for clinical interpretation of the FSFI in women with and without hypoactive sexual desire disorder. The Journal of Sexual Medicine, 7(9), 3096–3103. doi:10.1111/j.1743-6109.2010.01871.x
- Gosling, S. D., Rentfrow, P. J., & Swann, W. B., Jr. (2003). A very brief measure of the Big-Five personality domains. Journal of Research in Personality, 37(6), 504–528. doi:10.1016/S0092-6566(03)00046-1
- Gros, D.F., Gros, K.S., Acierno, R., Frueh, B., & Morland, L.A. (2013). Relation between treatment satisfaction and treatment outcome in veterans with posttraumatic stress disorder. Journal of Psychopathology and Behavioral Assessment, 35 (4), 522–530. doi:10.1007/s10862-013-9361-6
- Gutierrez, D. D., Thompson, L., Kemp, B., Mulroy, S. J., Physical Therapy Clinical Research Network, & Rehabilitation Research and Training Center on Aging-Related Changes in Impairment for Persons Living with Physical Disabilities (2007). The relationship of shoulder pain intensity to quality of life, physical activity, and community participation in persons with paraplegia. The Journal of Spinal Cord Medicine, 30(3), 251–255. doi:10.1080/10790268.2007.11753933
- John, O. P., & Srivastava, S. (1999). The Big Five Trait taxonomy: History, measurement, and theoretical perspectives. In L. A. Pervin & O. P. John (Eds.), Handbook of personality: Theory and research (p. 102–138). Guilford Press.
- Kabat-Zinn J. (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry, 4(1), 33–47. doi:10.1016/0163-8343(82)90026-3
- Lambert, B., Desrosiers, M., Chagnon, M., & Lepage, Y. (2013). Sexual behaviors in women with primary and secondary provoked vestibulodynia: A controlled study. Advances in Sexual Medicine, 03(03), 60–65. doi:10.4236/asm.2013.33010.
- Lethem, J., Slade, P. D., Troup, J. D., & Bentley, G. (1983). Outline of a Fear-Avoidance Model of exaggerated pain perception. Behaviour Research and Therapy, 21(4), 401–408. doi:10.1016/0005-7967(83)90009-8
- Lindström, S., & Kvist, L. J. (2015). Treatment of provoked vulvodynia in a Swedish cohort using desensitization exercises and cognitive behavioral therapy. BMC Women's Health, 15, 108. doi:10.1186/s12905-015-0265-3
- Lucchetti, G., Oliveira, A. B., Mercante, J. P. P., & Peres, M. F. P. (2012). Anxiety and fear-avoidance in musculoskeletal pain. Current Pain and Headache Report, 16, 399–406. doi:10.1007/s11916-012-0286-7
- Maillé, D. L., Bergeron, S., & Lambert, B. (2015). Body image in women with primary and secondary provoked vestibulodynia: A controlled study. The Journal of Sexual Medicine, 12(2), 505–515. doi:10.1111/jsm.12765
- Masheb, R. M., Lozano-Blanco, C., Kohorn, E. I., Minkin, M. J., & Kerns, R. D. (2004). Assessing sexual function and dyspareunia with the Female Sexual Function Index (FSFI) in women with vulvodynia. Journal of Sex & Marital Therapy, 30(5), 315–324. doi:10.1080/00926230490463264
- McCracken, L. M., Carson, J. W., Eccleston, C., & Keefe, F. J. (2004). Acceptance and change in the context of chronic pain. Pain, 109(1-2), 4–7. doi:10.1016/j.pain.2004.02.006
- Meyer-Bahlburg, H. F., & Dolezal, C. (2007). The Female Sexual Function Index: A methodological critique and suggestions for improvement. Journal of Sex & Marital Therapy, 33(3), 217–224. doi:10.1080/00926230701267852
- Murphy, D., Lindsay, S., De, C., & Williams, A.C.D.C. (1997). Chronic low back pain: Predictions of pain and relationship to anxiety and avoidance. Behaviour Research and Therapy, 35(3), 231–238. doi:10.1016/S0005-7967(96)00103-9
- Newell D. J. (1992). Intention-to-treat analysis: Implications for quantitative and qualitative research. International Journal of Epidemiology, 21(5), 837–841. doi:10.1093/ije/21.5.837
- Osman, A., Barrios, F. X., Gutierrez, P. M., Kopper, B. A., Merrifield, T., & Grittmann, L. (2000). The Pain Catastrophizing Scale: Further psychometric evaluation with adult samples. Journal of Behavioral Medicine, 23(4), 351–365. doi:10.1023/a:1005548801037
- Pukall C., Bergeron S., Brown C., Bachmann, G., Wesselmann, U., & Vulvodynia Collaborative Research Group. (2017). Recommendations for self-report outcome measures in vulvodynia clinical trials. The Clinical Journal of Pain, 33(8), 756–765. doi:10.1097/AJP.0000000000000453
- Reed, B. D., Haefner, H. K., & Cantor, L. (2003). Vulvar dysesthesia (vulvodynia): A follow-up study. The Journal of Reproductive Medicine, 48(6), 409–416. doi:10.1097/01.OGX.0000090196.75538.9E.
- Reed, B. D., Harlow, S. D., Sen, A., Legocki, L. J., Edwards, R. M., Arato, N., & Haefner, H. K. (2012). Prevalence and demographic characteristics of vulvodynia in a population-based sample. American Journal of Obstetrics and Gynecology, 206(2), 170.e1–170.e9. doi:10.1016/j.ajog.2011.08.012
- Reneman, M. F., Dijkstra, A., Geertzen, J. H., & Dijkstra, P. U. (2010 ). Psychometric properties of chronic pain acceptance questionnaires: A systematic review. European Journal of Pain (London, England), 14(5), 457–465. doi:10.1016/j.ejpain.2009.08.003
- Rosemann, T., Kuehlein, T., Laux, G., & Szecsenyi, J. (2007). Osteoarthritis of the knee and hip: A comparison of factors associated with physical activity. Clinical Rheumatology, 26(11), 1811–1817. https://doi.org/10.1007/s10067-007-0579-0
- Rosenbaum, T. Y. (2013). An integrated mindfulness-based approach to the treatment of women with sexual pain and anxiety: Promoting autonomy and mind/body connection. Sexual and Relationship Therapy, 28(1-2), 20–28. doi:10.1080/14681994.2013.764981
- Rosen, R., Brown, C., Heiman, J., Leiblum, S., Meston, C., Shabsigh, R., Ferguson, D., & D'Agostino, R., Jr (2000). The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. Journal of Sex & Marital Therapy, 26(2), 191–208. doi:10.1080/009262300278597
- Rosen, N. O., Muise, A., Bergeron, S., Impett, E. A., & Boudreau, G. K. (2015). Approach and avoidance sexual goals in couples with provoked vestibulodynia: Associations with sexual, relational, and psychological well-being. The Journal of Sexual Medicine, 12(8), 1781–1790. doi:10.1111/jsm.12948
- Rosen, N. O., Santos-Iglesias, P., & Byers, E. S. (2017). Understanding the sexual satisfaction of women with provoked vestibulodynia and their partners: Comparison with matched controls. Journal of Sex & Marital Therapy, 43(8), 747–759. doi:10.1080/0092623X.2016.1263705
- Ruixie, Z., Lynn, M., & Darnall, B. D. (2020). Daily pain catastrophizing predicts less physical activity and more sedentary behavior in older adults with osteoarthritis. Pain, 161 (11), 2603–2610. doi:10.1097/j.pain.0000000000001959
- Schütze, R., Rees, C., Preece, M., & Schütze M. (2010). Low mindfulness predicts pain catastrophizing in a fear-avoidance model of chronic pain. Pain, 148 (1), 120–127. doi:10.1016/j.pain.2009.10.030
- Smith, K. B., Sadownik, L. A., Dargie, E., Albert, A., & Brotto, L. A. (2019). Multidisciplinary treatment for provoked vestibulodynia: Treatment trajectories, predictors, and moderators of sexual distress and pain. The Clinical Journal of Pain, 35(4), 335–344. doi:10.1097/AJP.0000000000000682
- Sullivan, M. J. L., Bishop, S. R., & Pivik, J. (1995). The Pain Catastrophizing Scale: Development and validation. Psychological Assessment, 7(4), 524–532. doi:10.1037/1040-3590.7.4.524
- Sullivan, M. J., Lynch, M. E., & Clark, A. J. (2005). Dimensions of catastrophic thinking associated with pain experience and disability in patients with neuropathic pain conditions. Pain, 113(3), 310–315. doi:10.1016/j.pain.2004.11.003
- Tawashy, A. E., Eng, J. J., Lin, K. H., Tang, P. F., & Hung, C. (2009). Physical activity is related to lower levels of pain, fatigue and depression in individuals with spinal-cord injury: A correlational study. Spinal Cord, 47(4), 301–306. doi:10.1038/sc.2008.120
- Taylor, S., Zvolensky, M. J., Cox, B. J., Deacon, B., Heimberg, R. G., Ledley, D. R., … Cardenas, S. J. (2007). Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment, 19(2), 176–188. doi:10.1037/1040-3590.19.2.176
- ter Kuile, M. M., Melles, R. J., Tuijnman-Raasveld, C. C., de Groot, H. E., & van Lankveld, J. J. (2015). Therapist-aided exposure for women with lifelong vaginismus: Mediators of treatment outcome: A randomized waiting list control trial. The Journal of Sexual Medicine, 12(8), 1807–1819. doi:10.1111/jsm.12935
- ter Kuile, M. M., van Lankveld, J. J., de Groot, E., Melles, R., Neffs, J., & Zandbergen, M. (2007). Cognitive-behavioral therapy for women with lifelong vaginismus: Process and prognostic factors. Behaviour Research and Therapy, 45(2), 359–373. doi:10.1016/j.brat.2006.03.013
- ter Kuile, M. M., & Weijenborg, P. T. (2006). A cognitive-behavioral group program for women with Vulvar Vestibulitis Syndrome (VVS): Factors associated with treatment success. Journal of Sex & Marital Therapy, 32(3), 199–213. doi:10.1080/00926230600575306
- van den Hurk, P. A. M., Wingens, T., Giommi, F., Barendregt, H. P., Speckens, A. E. M., & van Schie, H. T. (2011). On the relationship between the practice of mindfulness meditation and personality – an exploratory analysis of the mediating role of mindfulness skills. Mindfulness, 2, 194–200. doi:10.1007/s12671-011-0060-7
- Vlaeyen, J. W., & Linton, S. J. (2000). Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain, 85(3), 317–332. doi:10.1016/s0304-3959(99)00242-0
- Watson, D., O'Hara, M. W., Simms, L. J., Kotov, R., Chmielewski, M., McDade-Montez, E. A., Gamez, W., & Stuart, S. (2007). Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS). Psychological Assessment, 19(3), 253–268. doi:10.1037/1040-3590.19.3.253
- Wiegel, M., Meston, C., & Rosen, R. (2005). The Female Sexual Function Index (FSFI): Cross-validation and development of clinical cutoff scores. Journal of Sex & Marital Therapy, 31(1), 1–20. doi:10.1080/00926230590475206