Abstract
Purpose
Ward rounds play a crucial role in the delivery of patient care in inpatient settings, but involve a complex mix of tasks, skills and challenges for junior doctors to negotiate. This study informs the development of high-quality training by identifying the activities that junior doctors perform, and those associated with stress during real-life ward rounds.
Materials and methods
All activities performed by FY1 doctors (n = 60) over 2 ward rounds were coded in real-time by a trained observer using the work observation method by activity timing (WOMBAT). Doctors’ heart rate was continuously recorded and non-metabolic peaks in heart rate used as a physiological indicator of stress.
Results
During ward rounds, FY1 doctors commonly engaged in indirect patient care, professional communication, documentation and observation. Very little time was spent on direct patient care (6%) or explicit supervision/education (0.01%). Heart rate data indicated that stress was highest during administrative tasks while interacting directly with patients while stepping out of rounds to complete personal tasks, when answering bleeps and while multi-tasking.
Conclusions
Training that specifically covers the activities involved, skills required, and challenges inherent in real-life ward rounds may better prepare FY doctors for this complex area of practice.
Introduction
Ward rounds – visits paid by hospital medical teams to each of the patients under their care to review the patient’s condition and plan next steps – play a crucial role in the delivery of high quality, safe inpatient care. However, ward rounds vary considerably in terms of organisation, efficiency, quality and patient experience (Royal College of Physicians Citation2012), and are complex and difficult to define (Walton et al. Citation2016). They may be particularly challenging for the most junior doctors, the group who typically experience the highest baseline levels of work-related stress (Bruce et al. Citation2009; Peisah et al. Citation2009).
Practice points
The main activities undertaken by junior doctors within ward rounds are indirect patient care, inter-professional communication and documentation.
Ward rounds involve many different tasks and require the ability to multi-task and deal with interruptions.
Ward rounds are highly variable from one to the next which may make them difficult to adequately simulate in training.
Junior doctors spend very little time during ward rounds receiving explicit supervision.
During ward rounds, administrative tasks, direct patient care, answering bleeps and multi-tasking appear to be the most stressful times.
Medical students and foundation doctors are not well prepared for their role in participating in or leading, ward rounds (Nikendei et al. Citation2008; Harvey et al. Citation2015; Pearce et al. Citation2019). Junior doctors receive little if any, formal training in how to effectively participate in (or lead) a ward round (Powell et al. Citation2015; Perversi et al. Citation2018; Pearce et al. Citation2019), and although medical students will attend many ward rounds as part of their undergraduate studies, these may offer little in the way of actual learning (Chaponda et al. Citation2009; Perversi et al. Citation2018).
If medical students and foundation doctors are to be trained to participate effectively in ward rounds, it is necessary to define the core tasks and skills involved. Both students and experts identify ‘non-technical skills’ (such as teamwork, communication and decision making) as key competencies required to conduct ward rounds (Harvey et al. Citation2015; Wolfel et al. Citation2016). These are in addition to the more technical tasks of diagnosis, prescribing, ordering investigations, patient education, discharge planning, etc. which are the core business of the ward round (Herring et al. Citation2011; RCP Citation2012). In addition, effective participation in ward rounds requires multi-tasking, the ability to think under pressure, and the ability to deal with frequent interruptions and distractions. During rounds doctors must also apply their medical knowledge in front of an audience (Nørgaard et al. Citation2004); answering questions, and engaging in face-to-face interactions with patients and relatives (Moss and McManus Citation1992; Carroll et al. Citation2008; Walton and Steinert Citation2010), introducing the possibility of being negatively judged by others if performance is suboptimal. Such factors are known to elicit stress (Dickerson and Kemeny Citation2004; Illing et al. Citation2013) which may in turn negatively impact performance and increase the incidence of errors (Thomas et al. Citation2015; Westbrook et al. Citation2018) during ward rounds.
In the most comprehensive study of the ward round period to date, Carroll et al. (Citation2008) used observations, in-depth interviewing and video filming to capture ward round practices in the intensive care setting. Upon reviewing the video footage, medical staff was surprised by the complex flow of information between junior and senior medical staff, how often discussions were interrupted and how multitasking in a fast-paced environment appeared to be daunting for junior staff.
To date, however, no studies have systematically recorded all of the activities that junior doctors perform during ward rounds, or attempted to quantify the levels of stress that different activities and experiences elicit. If simulations or other methods are to be used to train junior doctors in the skills required, and challenges inherent, inward rounds, it is important to build up a detailed picture of how ward rounds work in real life and to determine the elements that less experienced doctors find the most stressful. The present study does this by coding all activities performed by junior doctors’ during ward rounds in real-time using the well-established WOMBAT observational tool (Westbrook et al. Citation2012). This tool characterises all clinical and related activities into twelve categories (direct care, indirect care, medication, etc.) and records who was involved. Once identified, activities and experiences (such as multi-tasking; working with others, etc.) are then linked to real-time changes in stress. As it is not possible to assess stress directly during a ward round by, for example, frequently interrupting activities to obtain self-report ratings, heart rate was used as a proxy measure. Heart rate is commonly elevated when stressed (Zanstra et al. Citation2010) but is, of course, primarily determined by metabolic demand. To detect non-metabolic (i.e. stress-related) changes in heart rate, physical activity was measured continuously and allowed for statistical.
The present study aims to answer two research questions;
What are the main characteristics of ward rounds for foundation (FY1) doctors (in terms of activities performed, activity duration, people involved, need for multitasking and frequency of interruptions)?
Are differences in these observed ward round characteristics associated with potentially stress related increases in heart rate?
Methods and materials
Design
A real-time, within-person observational study where junior doctors had their activities coded and their heart rate continuously recorded during two separate ward rounds.
Participants and recruitment
Sixty doctors (of 72 approached) from two foundation year 1 (FY1) training cohorts (2014/15 and 2015/16) took part in the study (mean age = 25.15 years, SD = 2.3, two-thirds female). They were selected at random from a subset of 6 medical (n = 30) and 5 surgical (n = 30) inpatient wards in a large hospital. FY1 doctors taking medication known to alter heart rate were not eligible to participate. Data collection was arranged for weekdays only, as ward rounds are a less regular feature out of standard hours. Of the doctors who participated, three could only be observed on one of the two planned ward rounds, resulting in data on 117 of a possible 120 ward rounds.
Permissions and ethical approval
NHS research ethics approval was obtained for this study (REC reference 14/NS/0074).
Measures
Ward round observation
Each participant was observed during two separate ward rounds. All activities performed during the observed ward rounds were recorded by a trained observer using an Android tablet version (2.1) of the Work Observation Method By Activity Timing (WOMBAT), a comprehensive tool for observationally classifying clinical work (Westbrook et al. Citation2012). WOMBAT allows observers to classify work activity into one of twelve categories (see for definitions) and to indicate the people involved (Patient, Nurse, Doctor, Pharmacist, Relative, Allied Health Professional, Other, No-one), the location of the activity and the equipment/materials involved. Observers continuously log data and on entry, each primary task is time-stamped and linked to the other information recorded, along with whether the individual was interrupted (recorded by the observer) or multitasking (automatically detected).
Table 1. WOMBAT categories and definitions.
The reliability of observations was established in a separate study using a sample of 9 FY1 doctors from the same teaching hospital and wards as reported above but who were not involved in the main study. An experienced observer followed an established protocol (see Westbrook and Ampt Citation2009) to train a second observer to use the WOMBAT tool, after which sessions were independently double coded without interaction between observers. Following Westbrook, the level of agreement on time spent in each category was calculated. Inter-observer agreement was excellent for the number of times a coding category was selected within a session (r = 0.93) and for the proportion of time-coded as the same task (r = 0.95). Crucially, judges agreed on when the observed activities occurred. For this analysis, a specialist computer program (OASTES, Observer Agreement for Simulated Timed Event Sequences) that deals with the reliability of long streams of timed and event-coded data (Bakeman et al. Citation2009) was used to calculate how long each possible state co-occurred during a session. A tolerance-defined Kappa (TKtol) was produced, which tallied agreement between the two observers if selected categories matched within a 5 s window. This TKtol was 0.63, indicating satisfactory agreement between judges.
Physiological recording
Heart rate and activity level were measured continuously throughout ward rounds using small, chest-mounted Actiheart monitors (CamNtech) which demonstrate good validity and reliability (Brage et al. Citation2005). Non-metabolic increases in heart rate (i.e. those unrelated to physical activity) provide a physiological indicator of stress (Zanstra et al. Citation2010; Brouwer et al. Citation2018) so the present study used peak heart rate after adjustment for physical activity to detect periods of stress.
Analyses
Ward round tasks were descriptively summarised using SPSS (version 24). Heart rate data were modelled using MLwiN (version 2.36), a multilevel analysis software. Unless otherwise stated, the multilevel data were analysed using a three-level multilevel model with observations nested within ward rounds (one or two), nested within participants. The intercept was always treated as a random effect at all levels. The regression slopes of dependent variables were treated as fixed. Ward round (first or second), observation counts (used to indicate time progression) and activity duration were controlled for in the analysis.
Results
What are the main characteristics of the ward round (WR)?
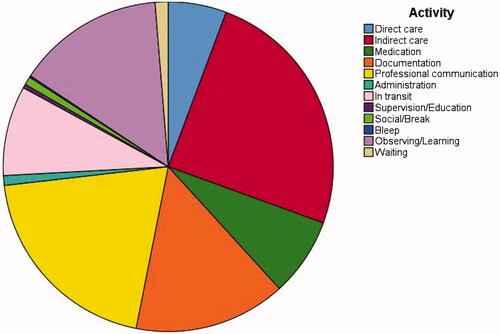
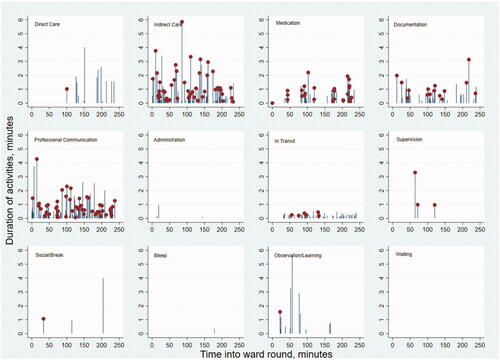
On average, ward rounds lasted over 100 min (M = 107 min, SD = 49 min) and ranged in length from 18 min to 4 h. FY1s spent less than 3 min (M = 2.6 min, SD = 3.3 min) ‘waiting’ or on ‘social/break’ (i.e. ‘off task’) during rounds. FY1s were multi-tasking (i.e. carrying out more than one task at a time) for close to 20% of each ward round on average (M = 21.5 min, SD = 15.2 min), with multitasking periods ranging from 0-70 min during a ward round. Similarly, the number of interruptions per ward round varied considerably (min 0, max 13), with an average of 3.1 interruptions per ward round (SD = 3.2). During a ward round, FY1s carried out on average 162 different activities, (range = 27–373). The busy and varied nature of at least some ward rounds is illustrated in . In this illustrative example, the FY1 carried out 373 different activities in a single ward round, most commonly involving indirect care and professional communication. Many of the activities involved multi-tasking and most were brief (average duration =0.77 min, SD 0.85). The longest period spent on a single task was 5.85 min of indirect care and during that time the FY1 also engaged in 2 min of professional communication.
Figure 1. Time spent on each activity across a ward round in one selected individual. Dots indicate multitasking (i.e. where multiple activities are being performed concurrently).
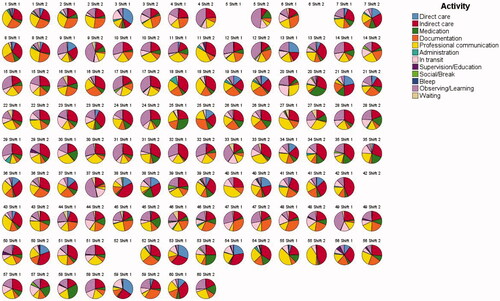
The average proportion of the ward round (WR) spent on different activities is depicted in . On average, around a quarter (25%) of FY1 doctors’ ward rounds were allocated to indirect patient care. Professional communication (i.e. any work-related discussion with another staff member other than medication-related discussion) made up 20% of activity, documentation 15% and observing/learning 15%. FY1 doctors spent 10% of the ward round in transit, i.e. moving between patients and tasks. Around 7–8% of the FY1s’ ward round was spent on medication tasks which mostly entailed discussing medication decisions with colleagues, reviewing drug documentation and prescribing. A small proportion of the FY1s’ ward round (6%) was dedicated to direct patient care, that is, any direct interaction between the study doctor and a patient. Finally, less than 4% of ward rounds were allocated to administration, supervision/education, social/break, answering bleep and waiting.
When individual ward round and doctor level data were examined, it was apparent that there was substantial variation in activities from one ward round to the next. displays two pie charts for each participating doctor, representing their activities on each of the two separate ward rounds studied. This figure illustrates the highly variable nature of this period of an FY1’s working day. Indeed the variation between ward rounds is greater than the variation between FY1 doctors.
To what extent do ward round tasks differ in their effects on heart rate?
Peak heart rate during each work task was calculated and compared to peak heart rate during ‘waiting’ (i.e. the period in which doctors are not engaged in any task) while controlling for the effects of physical activity. As shown in , peak heart rate was significantly higher (than waiting) during all active tasks except professional communication and highest during administration, direct care, and the rare instances of stepping out of a round to complete a personal task (social/break) or answering a bleep. However, all significant task-related changes observed in heart rate were relatively modest in size.
Table 2. Effect of work tasks on peak heart rate during the ward round, allowing for activity.
To what extent do multitasking and interruptions affect heart rate?
Differences in peak heart rate were computed between (i) periods when doctors were multitasking versus were not multitasking, and (ii) periods where doctors were carrying out activities as a result of being interrupted versus not. Peak heart rate was significantly higher on average (by 0.591 beats per minute; SE = 0.212, p < 0.01) when doctors were multitasking and this relationship did not significantly differ across different ward round tasks. In contrast, there was no significant relationship (–1.782bpm, SE = 0.956) between heart rate and being interrupted. Again, changes observed in heart rate were relatively modest in size.
Do interactions with other people during the ward round affect heart rate?
Peak heart rate when doctors were interacting with others was compared to heart rate when ‘no one’ else was involved in their activity. As shown in , peak heart rate was only higher than acting alone when dealing directly with patients. It was usually lower when working with other health professionals, particularly so for other doctors in training, nurses and allied health professionals.
Table 3. Effects of person interactions on peak heart rate, allowing for activity.
Discussion
The quality of ward rounds depends on a wide range of skills and the ability to deal effectively with challenges. If students are to be adequately prepared for effective participation in ward rounds, it is important to build up a clear picture of how ward rounds function in real life.
To our knowledge, this is the first study to systematically quantify all of the activities that junior doctors perform during ward rounds in real-time. On average, FY1 doctors spent most of each ward round on indirect patient care tasks (e.g. reviewing patient documents, ordering tests), professional communication (discussing the care of each patient with other healthcare professionals), documenting the round, and observing (typically watching more senior colleagues carry out tasks). Medication prescribing or reviewing took up a relatively small amount of time (8%) but FY1s were multi-tasking during half of such tasks which may have implications for safety as multi-tasking has been linked to prescribing errors (Westbrook et al. Citation2018). FY1s spent very little time (6%) on direct patient care during ward rounds and perhaps surprisingly, less than 0.01% of the ward round involved FY1s receiving active teaching (‘supervision/education’). On average, FY1s were multi-tasking around 20% of the time during ward rounds and were interrupted an average of three times per round, indicating that training in dealing with these specific challenges may be beneficial. When individual doctor-level data were examined, rounds were very variable, in line with previous studies (Stanley Citation1998; Chaponda et al. Citation2009; RCP Citation2012; Walton et al. Citation2016). This may make it more difficult to adequately prepare junior doctors, as the tasks and challenges they experience vary markedly from ward round to ward round.
Given the data reported on ward round variability and content, what should we concentrate on teaching? Knowledge of the purpose of a ward round and the ways in which it can be undertaken is important. This could be demonstrated by presenting the data we have obtained on what to expect, perhaps alongside video footage of a ward round. Developing proficiency in the non-technical skills highlighted is key, with actual hands-on patient interaction a much smaller part of the junior doctor role but nevertheless important. It is well recognised that learning these skills in medical school is essential (Kerins et al. Citation2020). Activities where students actively identify and critique the nontechnical skills used in real-life ward rounds are needed. Simulation is commonly used in medical education, and studies of ward round simulation have shown benefits in both subjective feelings of confidence (Harvey et al. Citation2015; Powell et al. Citation2015), and objective markers of performance (Pucher et al. Citation2014; Ford et al. Citation2017). Simulation can be also used to teach senior medical students to manage interruptions and distractions more effectively (Thomas et al. Citation2015) but it is recognised that current simulations may not adequately replicate the complexity of the actual workplace (Baker et al. Citation2017). Our data add to the literature and can be used to aid simulation design. A taxonomy of non-technical surgical ward round skills (WANTSS) has recently been produced describing specific desirable behaviours (Klaas et al. Citation2020) and is likely to be applicable in other disciplines. Other helpful approaches such as structured proformas and checklists are increasingly seen in quality improvement projects (Banfield et al. Citation2018; Mattinson and Cheeseman Citation2018) and maybe useful learning tools. Finally, formalised apprenticeship models (e.g. ‘student assistantships’, where final year students undertake the role of a foundation doctor as part of a ward attachment) provide an essential opportunity for students to gain practical experience of ward rounds as an active participant (Krautter et al. Citation2014; O’Connor Citation2019).
When the activities associated with stress were explored in the present study, peak heart rate was highest when FY1s were interacting directly with patients, undertaking administrative tasks related to the running of the ward round, or answering a bleep. Direct interactions with patients would reasonably be expected to produce stress, as social interactions carry with them the possibility of being negatively evaluated (‘social-evaluative threat’; Dickerson and Kemeny Citation2004). Direct patient care was also a relatively rare task for FY1 doctors (accounting for only 6% of ward round activity), so doctors will have had fewer opportunities to practice and build confidence. Interviews with FY1s (Bullock et al. Citation2013), suggest that many UK trainees want more experience of (and feedback on) direct patient care.
Administrative activities were also associated with elevations in heart rate, potentially reflecting the fact that such tasks were often completed under time pressure and with competing demands. These elevations in heart rate, of 2 or 3 beats per minute (compared to simply waiting) are substantial enough to suggest that some challenging or stressful psychological processes are involved in direct patient care and administration. It is also worth noting that more routine, frequent activities (such as indirect patient care or dealing with medication) are also associated with a heart rate increase.
Bleeps (while infrequent), were associated with elevations in peak heart rate, likely reflecting the urgent nature of being paged. Peak heart rate was also higher during the WOMBAT category ‘social/break’, but it is important to note that this is just a category label and that in the ward round context, these were not breaks per se. Rather, these were instances where FY1s either had to step out of rounds (e.g. for bathroom breaks) before returning to core tasks or where non-work discussions occurred, often while in transit between patients or wards. Both bleeps and social/break activities were rare during ward rounds (together comprising less than 0.01% of time spent on rounds) and so the heart rate elevations associated with these tasks may be less reliable.
Peak heart rate was significantly higher when FY1 doctors were multitasking, regardless of the type of task, perhaps suggesting that multitasking was stressful in its own right. However, the elevation in peak heart rate was not substantial and should be interpreted with caution. Multitasking is very common in medicine, being simultaneously detrimental to patient care, but a highly useful skill (Skaugset et al. Citation2016). Interestingly, there was no significant elevation in heart rate as a result of being interrupted, which is often listed alongside multitasking as a risk to patient safety. Interruptions were, however, infrequent, suggesting that ward rounds are relatively protected time compared to the rest of the working day.
Finally, heart rate was lower when working with other health professionals than when acting alone, most notably with other doctors in training, nurses and allied health professionals, indicating that support from other health professionals is beneficial. However, there was no strong evidence that it was particularly stressful to work with particular professionals or grades of staff.
As with all real-world studies, this study is not without limitations. The research presented relied on a single sample of doctors in their first postgraduate training year at a large UK teaching hospital, which may have implications for the generalisability of the findings. However, participants were selected at random and few of the doctors approached declined to participate so the effects of sampling bias were minimized as far as possible. In addition, heart rate is not a perfect correlate of psychological stress and will be affected by other factors, most notably physical activity. While metabolic changes in heart rate were controlled for by continuously recording and accounting for the effects of physical activity during analysis, some variation in heart rate will inevitably reflect non-stress processes. In future studies, it would be preferable to supplement such physiological measures with self-reports of perceived stress.
Conclusions
In conclusion, the present study provides in-depth information about both the content and experience of ward rounds for junior doctors. Ward rounds are complex and highly variable in nature. Junior doctors often have to multi-task during rounds and are interrupted relatively frequently. On average, junior doctors spend a lot of time during the ward round on indirect care and professional communication, but little time on direct patient care. Very little of junior doctors’ time during ward rounds (0.01%) is dedicated to receiving explicit teaching/supervision. Some activities produce heart rate changes indicative of increases in stress (administrative tasks, direct patient care, having to multitask and interacting with patients), and others appear to reduce stress (working with other medical staff during tasks). By knowing more about FY doctors’ experiences during ward rounds, it may be possible to better prepare trainees for common tasks and potential stressors and to make beneficial changes to both training and ward round practices.
Glossary
WOMBAT: Work Observation Method By Activity Timing
Supplemental Material
Download MS Word (145.6 KB)Acknowledgements
The authors would like to thank participating FY1 doctors and the senior staff who made this study possible.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
Notes on contributors
Cheryl L. Bell
Cheryl L. Bell, PhD, Health Psychology, Institute of Applied Health Sciences, University of Aberdeen.
Julia L. Allan
Julia L. Allan, PhD, Health Psychology, Institute of Applied Health Sciences, University of Aberdeen.
Sarah Ross
Sarah Ross, MBChB, NHS Tayside/School of Medicine, University of Dundee.
Daniel J. H. Powell
Daniel J.H. Powell, PhD, Health Psychology, Institute of Applied Health Sciences, University of Aberdeen. Rowett Institute, University of Aberdeen.
Derek W. Johnston
Derek W. Johnston, PhD, Health Psychology, Institute of Applied Health Sciences, University of Aberdeen. School of Psychology, University of Aberdeen.
References
- Bakeman R, Quera V, Gnisci A. 2009. Observer agreement for timed-event sequential data: a comparison of time-based and event-based algorithms. Behav Res Methods. 41(1):137–147.
- Baker BG, Bhalla A, Doleman B, Yarnold E, Simons S, Lund JN, Williams JP. 2017. Simulation fails to replicate stress in trainees performing a technical procedure in the clinical environment. Med Teach. 39(1):53–57.
- Banfield DA, Adamson C, Tomsett A, Povey J, Fordham T, Richards SK. 2018. ‘Take Ten’ improving the surgical post-take ward round: a quality improvement project . BMJ Open Qual. 7(1):e000045.
- Brage S, Brage N, Franks P, Ekelund U, Wareham N. 2005. Reliability and validity of the combined heart rate and movement sensor Actiheart. Eur J Clin Nutr. 59(4):561–570.
- Brouwer AM, van Dam E, van Erp JBF, Spangler DP, Brooks JR. 2018. Improving real-life estimates of emotion based on heart rate: a perspective on taking metabolic heart rate into account. Front Hum Neurosci. 12:284.
- Bruce L, Carlisle D, Smith D. 2009. National training surveys 2008–2009 key findings. [place unknown]: Postgraduate Medical Education and Training Board.
- Bullock A, Fox F, Barnes R, Doran N, Hardyman W, Moss D, Stacey M. 2013. Transitions in medicine: trainee doctor stress and support mechanisms. J Workplace Learning. 25(6):368–382.
- Carroll K, Iedema R, Kerridge R. 2008. Reshaping ICU ward round practices using video-reflexive ethnography. Qual Health Res. 18(3):380–390.
- Chaponda M, Borra M, Beeching NJ, Almond DS, Williams PS, Hammond MA, Price VA, Tarry L, Taegtmeyer M. 2009. The value of the post-take ward round: are new working patterns compromising junior doctor education? Clin Med. 9(4):323–326.
- Dickerson SS, Kemeny ME. 2004. Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychol Bull. 130(3):355–391.
- Ford H, Cleland J, Thomas I. 2017. Simulated ward round: reducing costs, not outcomes. Clin Teach. 14(1):49–54.
- Harvey R, Mellanby E, Dearden E, Medjoub K, Edgar S. 2015. Developing non-technical ward-round skills. Clin Teach. 12(5):336–340.
- Herring R, Desai T, Caldwell G. 2011. Quality and safety at the point of care: how long should a ward round take? Clin Med. 11(1):20–22.
- Illing JC, Morrow GM, Rothwell Nee Kergon CR, Burford BC, Baldauf BK, Davies CL, Peile EB, Spencer JA, Johnson N, Allen M, et al. 2013. Perceptions of UK medical graduates’ preparedness for practice: a multi-centre qualitative study reflecting the importance of learning on the job . BMC Med Educ. 13(1):34.
- Kerins J, Smith SE, Phillips EC, Clarke B, Hamilton AL, Tallentire VR. 2020. Exploring transformative learning when developing medical students’ non-technical skills. Med Educ. 54(3):264–274.
- Klaas S, Murray K, Maran N, Flin R, Paterson-Brown S. 2020. A ward-round non-technical skills for surgery (WANTSS) taxonomy. J Surg Ed. 77(2):369–379.
- Krautter M, Koehl-Hackert N, Nagelmann L, Jünger J, Norcini J, Tekian A, Nikendei C. 2014. Improving ward round skills. Med Teach. 36(9):783–788.
- Mattinson AR, Cheeseman SJ. 2018. Development and implementation of a structured ward round in acute adult psychiatry. BMJ Open Qual. 7(3):e000035.
- Moss F, McManus I. 1992. The anxieties of new clinical students. Med Educ. 26(1):17–20.
- Nikendei C, Kraus B, Schrauth M, Briem S, Jünger J. 2008. Ward rounds: how prepared are future doctors? Med Teach. 30(1):88–91.
- Nørgaard K, Ringsted C, Dolmans D. 2004. Validation of a checklist to assess ward round performance in internal medicine. Med Educ. 38(7):700–707.
- O’Connor E. 2019. Cognitive apprenticeship in the ICU: ward round activities to enhance student learning. Med Teach. 41(1):116.
- Pearce J, Redman M, Gajebasia S, Dirksen R. 2019. Ward rounds: can an aide-memoire help new doctors? Clin Teach. 16(2):147–151.
- Peisah C, Latif E, Wilhelm K, Williams B. 2009. Secrets to psychological success: why older doctors might have lower psychological distress and burnout than younger doctors. Aging Ment Health. 13(2):300–307.
- Perversi P, Yearwood J, Bellucci E, Stranieri A, Warren J, Burstein F, May H, Wolff A. 2018. Exploring reasoning mechanisms in ward rounds: a critical realist multiple case study. BMC Health Serv Res. 18(1):643.
- Powell N, Bruce CG, Redfern O. 2015. Teaching a ‘good’ ward round. Clin Med . 15(2):135–138.
- Pucher PH, Aggarwal R, Singh P, Srisatkunam T, Twaij A, Darzi A. 2014. Ward simulation to improve surgical ward round performance: a randomized controlled trial of a simulation-based curriculum. Ann Surg. 260(2):236–243.
- Royal College of Physicians. 2012. Work and wellbeing in the NHS: why staff health matters to patient care. October, 2017. https://www.rcplondon.ac.uk/guidelines-policy/work-and-wellbeing-nhs-why-staff-health-matters-patient-care.
- Skaugset LM, Farrell S, Carney M, Wolff M, Santen SA, Perry M, Cico SJ. 2016. Can you multitask? Evidence and limitations of task switching and multitasking in emergency medicine. Ann Emerg Med. 68(2):189–195.
- Stanley P. 1998. Structuring ward rounds for learning: can opportunities be created? Med Educ. 32(3):239–243.
- Thomas I, Nicol L, Regan L, Cleland J, Maliepaard D, Clark L, Walker K, Duncan J. 2015. Driven to distraction: a prospective controlled study of simulated ward round experience to improve patient safety teaching for medical students. BMJ Qual Saf. 24(2):154–161.
- Walton JM, Steinert Y. 2010. Patterns of interaction during rounds: implications for work-based learning. Med Educ. 44(6):550–558.
- Walton V, Hogden A, Johnson J, Greenfield D. 2016. Ward rounds, participants, roles and perceptions: literature review. Int J Health Care Qual Assur. 29(4):364–379.
- Westbrook JI, Ampt A. 2009. Design, application and testing of the Work Observation Method by Activity Timing (WOMBAT) to measure clinicians’ patterns of work and communication. Int J Med Inf. 78:S25–S33.
- Westbrook JI, Creswick NJ, Duffield C, Li L, Dunsmuir WT. 2012. Changes in nurses’ work associated with computerised information systems: Opportunities for international comparative studies using the revised Work Observation Method By Activity Timing (WOMBAT). 11th International Congress on Nursing Informatics; Jun 23–27, 2012; Montreal, Canada: International Congress in Nursing Informatics (11th: 2012: Montreal, Quebec). p. 448.
- Westbrook JI, Raban MZ, Walter SR, Douglas H. 2018. Task errors by emergency physicians are associated with interruptions, multitasking, fatigue and working memory capacity: a prospective, direct observation study. BMJ Qual Saf. 27(8):655–663.
- Wölfel T, Beltermann E, Lottspeich C, Vietz E, Fischer MR, Schmidmaier R. 2016. Medical ward round competence in internal medicine–an interview study towards an interprofessional development of an Entrustable Professional Activity (EPA). BMC Med Educ. 16(1):1–10.
- Zanstra YJ, Johnston DW, Rasbash J. 2010. Appraisal predicts hemodynamic reactivity in a naturalistic stressor. Int J Psychophysiol. 77(1):35–42.