Abstract
Background
Doctors are increasingly expected to demonstrate medical leadership and management (MLM) skills. The Faculty of Medical Leadership and Management (FMLM) has published an indicative undergraduate curriculum to guide the development of MLM content at UK medical schools.
Method
Students from 30 medical schools were surveyed to determine their understanding of MLM teaching at their school. Timetables for 21 schools were searched for MLM-related keywords. Student-reported teaching and timetabled teaching were coded according to predefined themes. Aggregated demographic and postgraduate performance data were obtained through collaboration with the Medical Student Investigators Collaborative (msico.org).
Results
Whilst 88% of medical students see MLM teaching as relevant, only 18% believe it is well integrated into their curriculum. MLM content represented ∼2% of timetabled teaching in each 5-year undergraduate medical course. Most of this teaching was dedicated to teamwork, performance/reflection and communication skills. There was minimal association between how much of a topic students believed they were taught, and how much they were actually taught. We found no association between the volume of MLM teaching and performance in postgraduate examinations, trainee career destinations or fitness to practice referrals.
Conclusion
Our findings demonstrate limited and variable teaching of MLM content. Delivery was independent of broader teaching and assessment factors.
Keywords:
Introduction
A succession of high-profile enquiries into the safety and efficacy of patient care in the UK have highlighted the importance of robust clinical leadership amongst medical professionals (Royal Liverpool Childrens Inquiry Citation2001; Department of Health Citation2002; Francis Citation2013; Kennedy Citation2013; Kirkup Citation2015; Gosport Independent Panel Citation2018; O’Hara Citation2018). As a result, doctors are increasingly expected to demonstrate leadership capabilities (General Medical Council Citation2018). Furthermore, anecdotal evidence associates leadership and resilience as being intertwined in the modern NHS (Shipton et al. Citation2008; Fealy et al. Citation2015). Recently, there has been considerable interest around when, and how, management and leadership (MLM) training is delivered to doctors, resulting in the increased presence of MLM content in undergraduate curricula at UK medical schools. These attributes are now expected to be developed early and the General Medical Council (GMC), in their capacity as the professional regulator for doctors in the UK, has stated that graduates ‘must recognise the role of doctors in contributing to the management and leadership of the health service’ (General Medical Council Citation2018).
Practice points
Most medical students consider MLM to be relevant to them.
There is substantial variation in MLM teaching between undergraduate curricula.
There is a clear dichotomy between student perceptions of taught MLM content and actual timetabled teaching.
Whilst it has been shown previously by ourselves and others that medical courses in the UK vary substantially in taught content (Devine et al. Citation2020), teaching methods (McManus et al. Citation2020) and assessment volume (Devine et al. Citation2015), there has been very little high-resolution quantitative examination of MLM content in the curriculum. Jefferies et al. (Citation2016) found that 23 of 25 UK medical courses surveyed formally included MLM content within their curricula, however these findings were qualitative and did not elucidate the volume, content and format of this teaching. They did however identify that 88% of medical schools had intentions to increase the delivery of these areas within the next two years of the survey. Contextual barriers to curriculum delivery included a ‘lack of space,’ reluctance for staff to deliver MLM, faculty perceived lack of student interest, and a lack of valid MLM teaching sources and assessment methods.
A review of studies in 2011 (Abbas et al. Citation2011), mostly from the USA, found MLM education can be divided into five key domains: QI; managed care, use of resources, and costs; general leadership and management; role of the doctor; and patient safety. Students recognised the benefits of QI for improving patient care and were generally positive towards educational interventions in this area, however, there was dissatisfaction with managed care, use of resources, and costs. Students also displayed negative attitudes towards educational interventions around patient safety and felt there was a need for more interventions targeting gaining confidence in managing medical errors. With regards to students’ perceptions of MLM teaching, some small studies have been carried out in this area. UK medical students value the importance of MLM teaching (Stringfellow et al. Citation2015; Rouhani et al. Citation2018), and consider a wide range of leadership knowledge, skills, and qualities relevant to their practice, and feel that more is required from these areas in their curriculum (Butrous et al. Citation2012; Quince et al. Citation2014). These subjects include: structure of the NHS; economic factors affecting the NHS; team-working; decision-making and negotiating; and patient safety. Previously, students have reported that their preferred teaching methods for MLM are seminars, lectures, QI, experiential learning during clinical placements, but that it should be integrated into existing structured observation, reflection, and critical appraisal and analysis of mistakes (Quince et al. Citation2014; Stringfellow et al. Citation2015). They feel that MLM education must be relevant in the clinical context and that the greatest barrier to MLM in the curriculum is the attitudes of medical professionals, students, and society in general (Quince et al. Citation2014). In a small survey of final year UK medical students in 2016, over half of respondents rated the MLM teaching they had received during medical school as poor (Rouhani et al. Citation2018).
Whilst the integration of these elements may prove challenging for faculty, it is crucial that they are subject to the same level of quality assurance as other more traditional aspects of the curriculum. Standardisation of MLM domains has previously been explored through the publication of guidance documents, such as the Healthcare Leadership Model and the Medical Leadership Competency Framework (MLCF) ([FMLM] Faculty of Medical Leadership and Management Citation2013; NHS Leadership Academy and NHS Leadership Academy Citation2013). In recent years, the Faculty of Medical Leadership and Management (FMLM) has developed an indicative undergraduate curriculum ([FMLM] Faculty of Medical Leadership and Management Citation2018), mapped to the GMC’s competencies for newly qualified graduates, which describes suggested MLM learning and assessment opportunities.
Despite continued efforts to integrate MLM training, there is a paucity of comprehensive quantitative data on MLM provision within undergraduate curricula. In this first iteration of the LUMENS study, we interrogate raw, whole-course timetables from 21 A100 medical courses in the UK in order to provide a quantitative baseline of conspicuous MLM training in the undergraduate curriculum. We describe the first quantitative comparison of MLM teaching duration, format and content at medical schools in the UK alongside findings from a national survey on student perceptions of MLM integration in their curricula. Finally, we consider the existence of a relationship between the volume of MLM teaching in the undergraduate curriculum and outcomes in key postgraduate metrics.
Materials and methods
In association with the Medical Student Investigators Collaborative (MSICo.org), we analysed whole-course timetables for the 2014–2015 academic year obtained under Freedom of Information (FoI) Act 2000 requests as part of the AToMS Study (Devine et al. Citation2020). At the time of the study there were 33 medical schools in the UK. In this paper, we have only described five-year (standard entry, A100) courses for undergraduates due to timetable availability. Graduate-only courses (Warwick and Swansea) were excluded. Of the 31 remaining schools, 6 were omitted for a variety of reasons (Supplementary material 1): Peninsula College of Medicine and Dentistry; University of St Andrews; Lancaster; Southampton; and Bristol. This left 25 medical schools with complete timetable data that were available for our analysis. Utilising the resources of the FMLM Medical Students Group (MSG), timetables acquired in the previous AToMS study were searched to identify MLM teaching provided in the timetabled curriculum according keywords corresponding to eight core themes (Supplementary Appendix C). These were: Communication, Finance and Resourcing, Safety and Whistleblowing, Performance and Reflection, Improvement and Audit, NHS Structure and ‘Other’ MLM Content. This was performed by coding teams at each medical school and recorded in a standard format (Supplementary Appendix B). At 5 schools (Aberdeen, Bristol, Keele, Leicester, and Sheffield), no students were available to perform timetable analysis and these schools were excluded. This left 21 schools in our final analysed dataset (Supplementary material 2).
In addition to our timetable analysis, we simultaneously distributed a survey to each of the 33 medical schools. Initial piloting on five medical students suggested the average time to completion was approximately 10 minutes. The survey was distributed by FMLM MSG members via social media and through school email channels. Students were able to access the survey for a total of 227 days throughout all semesters of the 2017–2018 academic year. In total, 644 responses were recorded, with 18 entries being discounted due to incomplete or repeat responses, leaving 626 valid responses from 30 schools (Supplementary material 3). Responses were received for every school for which we possessed timetables except for Edinburgh. Some schools (QUB, Birmingham, Swansea, Bristol, Keele, Oxford, Leicester, Manchester, Sheffield and Aberdeen) returned less than 10 respondents, and were excluded from specific sub-analyses.
Questions using a 5-point Likert-scale (where 1 indicated strongly disagree and 5 indicated strongly agree) were designed to probe: perceptions of the importance of MLM content in the undergraduate curriculum; awareness of the existence of the Medical Leadership Competency Framework (MLCF); perceptions of the importance of each domain addressed by the MLCF and desirable timing of MLM training in the undergraduate curriculum. The MLCF (Third Edition, 2010) was chosen for comparison as this framework had been in circulation for several years (First Edition, 2008), at the time of conducting LUMENS, and therefore felt most likely to be represented within undergraduate curricula. Separately, students were asked to rank the top three: most important topics; preferred teaching methods; and preferred assessment methods pertaining to MLM training. Additionally, free-text spaces were given to probe student perceptions on: what MLM topics were currently taught; the current format of MLM training; and how MLM is currently assessed in their respective curricula. Finally, free-text spaces invited students to describe the barriers they perceived as preventing the inclusion of MLM content in the undergraduate curriculum. A summary of all survey questions and wording is shown in Supplementary Appendix D. As an anonymous survey collecting no identifiable data from respondents, the survey was deemed to be exempt from the requirement to seek ethical approval by the UCL ethics committee.
For the purposes of determining the relationship between total volume of MLM training in the undergraduate curriculum, school demographic, postgraduate performance and fitness to practice (FtP), we utilised data published as part of the MedDifs study (McManus et al. Citation2020). We have preserved the authors original nomenclature, and a full explanation of the derivation of these metrics can be found in Table 1 of that paper (McManus et al. Citation2020).
Statistical analysis
Timetable coding was performed in Microsoft Excel using a pre-populated standardised coding spreadsheet with data validation to ensure uniformity of thematic coding between coders. Surveys were designed in Google Forms and linked to a Google Sheet prior to export to Microsoft Excel at the end of the survey period. Timetabled teaching activities were converted into hours and plotted according to theme using GraphPad Prism version 8.0 (GraphPad Software, San Diego, CA, USA). Likert-scale data were plotted as divergent stacked bars, superimposed with median score; and heatmaps of ‘Top 3’ questions were produced using Tableau Desktop Professional Edition version 2019.1 (Tableau Software, Seattle, WA, USA). Free-text answers were analysed thematically using NVivo Mac version 10.2.2.0 (QSR International, Melbourne, Australia) for the same themes probed during timetable coding. Correlations were calculated according to Pearson’s r using the rcorr function of the Hmisc v4.2.0 (Harrell Citation2019) package in R version 3.6.1(R Foundation Citation2019) and were plotted using the corrplot package version 0.84 (Wei Citation2019). Statistical significance is displayed according to the convention: *p ≤ 0.05; **p ≤ 0.01; ***p ≤ 0.001; ****p ≤ 0.0001.
Results
Undergraduate perceptions of MLM training
Medical students recognise the importance of medical leadership and management
Respondents (n = 626 students from n = 30 schools) were asked to rank their sentiment towards questions pertaining to undergraduate MLM training on a 5-point Likert-scale. Firstly, students were asked about the importance of MLM in the undergraduate curriculum (). This revealed that students largely believe MLM training to be relevant to their education (median Likert-score = 4.0; agreement = 87.5%). Furthermore, students felt strongly that MLM skills are important for life as a junior doctor (median Likert-score = 5.0); agreement = 88.3%). Despite this, when asked if medical leadership was taught well in their curriculum, only 17.8% of students agreed (median Likert-score = 2.0).
Figure 1. Perceived importance of undergraduate medical leadership and management training by medical students. 626 medical students from 30 medical schools rated their level of agreement on a 5-point Likert-scale to questions on the following themes: (A) the importance of medical leadership and management in the curriculum; (B) the integration of Medical Leadership Competency Framework themes in their curriculum; and (C) the optimal placement of MLM content in their curriculum. Responses were plotted on a centred Likert-chart, with stacked, divergent bars indicating the percentage sentiment (agree-disagree) and the median Likert-scale response superimposed in white.
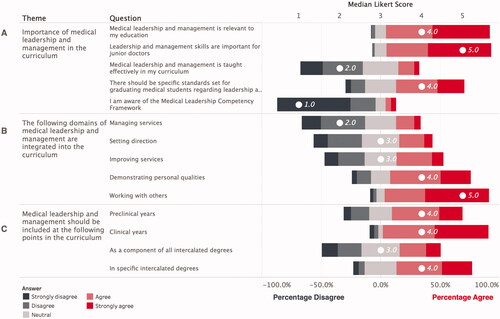
The medical leadership competency framework is poorly recognised by medical students
When asked if their ought to be standards set for graduating medical students regarding MLM, students largely agreed (median Likert-score = 4.0, agreement = 57.5%). When asked if they had heard of the Medical Leadership Competency Framework (MLCF), only 8.9% of students agreed (median Likert-score = 1.0). Together these findings suggest that whilst students value and recognise the importance of MLM training in the undergraduate curriculum, they largely feel it is not taught well.
The domains of the medical leadership competency framework are differentially integrated into the undergraduate curriculum
Having identified that students do not believe MLM is taught well in their curricula, and are only fleetingly aware of the MLCF, it was next interesting to examine how well the different domains of the MLCF are perceived to be integrated into the curriculum (). Students did not agree that ‘managing services’ (median Likert-score = 2.0; agreement = 20.6%), ‘setting direction’ (median Likert-score = 3.0; agreement = 27.8%) or ‘improving services’ (median Likert-score = 3.0; agreement = 39.5%) were well integrated. Students largely agreed that ‘demonstrating personal qualities’ (median Likert-score = 4.0; agreement = 67.5%) and ‘working with others’ (median Likert-score = 5.0; agreement = 87.6%) were well integrated. These findings suggest that certain domains of the MLCF, particularly those focussed on organisational leadership and service management are perceived to be lacking in the undergraduate curriculum.
Students value MLM training integrated at all stages of their undergraduate course and during specific intercalated degrees
In recent years there has been considerable consideration of the optimal time at which to integrate MLM content into undergraduate curricula. Next, we asked students when they felt MLM content would be most appropriately integrated into the MLM course (). Unsurprisingly, given the perceived value and relevance of MLM to students, respondents agreed to integration at most curricular timepoints polled: preclinical years (median Likert-score = 4.0; agreement = 59.2%); clinical years (median Likert-score = 4.0, agreement = 88.5%); and as a component of specific intercalated degrees (median Likert-score = 4.0; agreement = 63.5%). Students did not support the integration of MLM into all intercalate degrees (median Likert-score = 3.0; agreement = 34.7%). These findings may support the increased role of dedicated MLM-oriented intercalated degrees which are, at the time of writing, a growing offering at UK medical schools.
Students value teaching on teamwork, communication and whistleblowing
Next, students were asked to identify the three MLM topics which they would most value being taught about (). The most popular teaching topics ranked in the ‘top 3′ by students were effective communication (ranked ‘top 3′ by 50% of respondents); team working (42% of respondents); and patient safety/whistleblowing (38% of respondents).
Figure 2. Medical student preferences for MLM training topics, teaching and assessment methods. Heatmaps showing top three preferences for (A) MLM topics deemed most important for medical students; (B) teaching methods most suited to delivering MLM content; and (C) methods that most appropriately assess MLM teaching. Data indicative of the responses of 626 medical students from 30 medical schools. Response options provided to the respondents are displayed. Responses were weighted for each school based on the number of responses and transformed into a preference scale ranging from 0 to 1, with 0 indicating that no students ranked the answer in their ‘top 3’, and a score of 1 indicating that all students ranked the answer in their ‘top 3’. Heatmaps were then sorted according to the most popular preference.
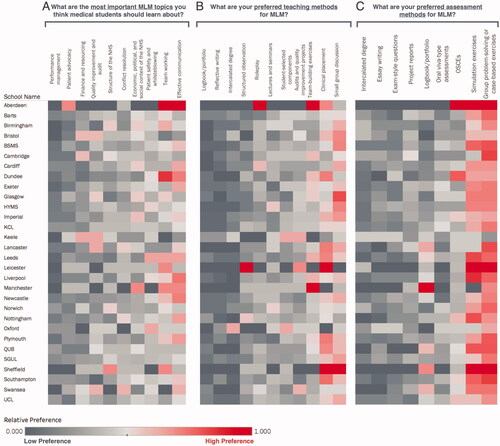
Students prefer to be taught MLM during clinical placements, small group discussions and team building exercises
Previous work has described a variety of teaching formats for MLM content in the undergraduate curriculum (Jefferies et al. Citation2016). The preferred formats by students responding to the LUMENS survey were small group discussion (ranked ‘top 3’ by 55% of students); clinical placement (52% of students), and team-building exercises (39% of students) – in order of preference.
Simulation, group problem solving, and case-based learning are the preferred assessment methods for MLM by medical students
Similarly to teaching format, student preferences for assessment of taught MLM content are yet to be elucidated. Here, we find that students prefer to be assessed during simulated leadership activities (ranked ‘top 3′ by 71% of students); group problem solving tasks (64% of students), and case-based learning (37% of students). These data suggest a strong appetite for simulation-based assessment.
Quantitative analysis of timetabled MLM teaching in undergraduate curricula
The duration and topics of MLM training varies substantially between medical schools
Timetabled MLM content was quantified at 21 of 26 schools with 5-year (A100) medical degrees for which complete timetables were available. We identified a mean of 96 hours (, n = 21, SD = 67, range = 5–248 hours) of MLM content across all medical schools. Keywords corresponding to 8 themes (Supplementary Appendix C) comprised of: Teamwork (, mean = 31, SD = 29, range = 0–110 hours); Communication (, mean = 26, SD = 20, range = 0–68 hours); performance management & reflection (PerformanceReflection) (, mean = 25, SD = 34, range = 1–133 hours); patient safety & whistleblowing (SafetyWhistleblowing) (, mean = 6, SD = 6, range = 0–22 hours); quality improvement & audit (ImprovementAudit) (, mean = 4, SD = 8, range = 0–31 hours); finance & resourcing (FinanceResourcing) (, mean = 2, SD = 2, range = 0–7 hours); NHS structure (StructureNHS) (, mean = 1, SD = 2, range = 0–5 hours); and Other (, mean = 3, SD = 3, range = 0–13 hours). Given that the mean total teaching identified by the AToMS study at a typical school was 3960 hours12, our findings demonstrate the relatively small contribution (∼2%) that MLM content contributes to the overall timetabled offering at UK medical schools.
Figure 3. The duration and content of undergraduate MLM teaching varies substantially between medical schools. Whole-course timetables for 21 A100 medical courses were interrogated for keywords corresponding to eight MLM themes (Teamwork; Performance and Reflection; Other; Finance and Resourcing; Communication; Quality Improvement & Audit; Patient Safety and Whistleblowing; and NHS Structure). Separately, free-text survey responses garnered student perceptions of which topics were taught during their undergraduate course (n = 626 students at 30 schools) and were analysed thematically according to the same eight themes using NVivo version 12.0. Graphs show: (A) the total duration of MLM training identified in the timetables of each 5-year medical degree, stacked by theme (n = 21 schools); (B) the percentage of students at each school identifying teaching matching each of the eight themes in free-responses to the question ‘What medical leadership and management topics are currently taught in your medical school (if any)?’ (n = 16 schools); and (C) a correlogram showing the Pearson r relationship between the volume of MLM teaching identified from the timetables at each school compared to the percentage of survey respondents identifying teaching matching the same themes in free-text survey responses (n = 16 comparisons). Grey ellipse indicates important relationships between actual and perceived teaching. *p ≤ 0.05; **p ≤ 0.01; ***p ≤ 0.001; ****p ≤ 0.0001.
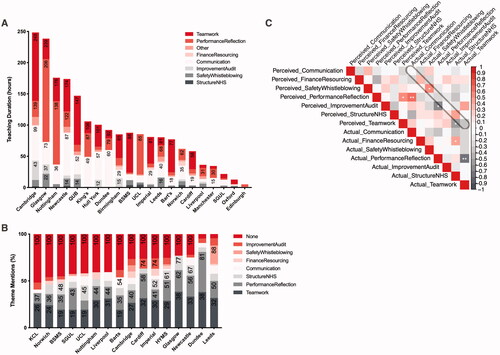
Students do not accurately perceive volume of timetabled MLM training
An important aspect of the LUMENS survey was to assess student free-text responses to the question: ‘What medical leadership and management topics are currently taught in your medical school (if any)?’ This enabled us to evaluate student recollection of taught MLM content and compare this to the true composition of MLM content on their course. Thematic analysis was performed on free-text responses from 626 student respondents. Responses were analysed and grouped into the same eight themes used for the timetable coding (vide supra) with the addition of one further category for students indicating that they received no MLM teaching. Themes identified in the responses are summarised for 16 schools (schools with fewer than 10 respondents and those not included in the timetable analysis are not shown) in . Each theme is represented as the proportion of total themes mentioned by respondents at that particular school. The dominant themes identified were the absence of MLM teaching in the curriculum (, mean = 32%, SD = 14%, range= 5–52%), teamwork (, mean = 28%, SD = 6%, range = 19–38%, and performance & reflection (, mean = 18%, SD = 8%, range = 10–43%).
We next compared the proportion of each MLM theme perceived by students in free-text answers to the quantitative proportion of each MLM theme present in their respective school’s timetable (). The grey ellipse in indicated the ‘zone of agreement’ between the proportion of each theme identified in free-text responses and the proportion of each theme identified in quantitative interrogation of whole-course timetables. Excluding ‘Other’ (from the timetable analysis) and ‘none’ (from the free-text responses), we find that students only accurately perceive the proportion of taught safety and whistleblowing (SafetyWhistleblowing) content accurately (, Pearson r = 0.54, p = 0.03, n = 16 comparisons). Taken together, these findings suggest some degree of disconnect may exist between the degree to which students perceive they have been taught certain MLM topics, and the extent to which they actually have been in clearly timetabled curricular activities.
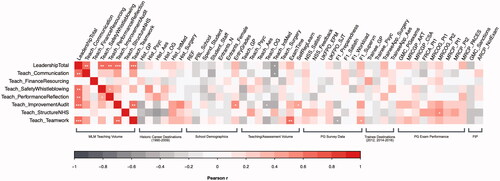
Associations between undergraduate MLM training and postgraduate outcomes for doctors
One important aspect relating to the development of MLM training in the undergraduate curriculum, is the extent to which such early training impacts future professional outcomes for doctors. Previous work has identified the benefits of MLM training in the postgraduate setting (Steinert et al. Citation2012; Frich et al. Citation2015; Hopkins et al. Citation2018). Using datasets available as part of the AToMS and MedDifs studies (Devine et al. Citation2020; McManus et al. Citation2020), we compared total MLM teaching and MLM teaching in each of the seven themes previously identified (‘Other’ excluded), with a range of demographic and postgraduate outcome data (). Total MLM teaching (LeadershipTotal) was not associated with metrics on FtP; MRCP + MRCGP performance; recent and historic career destinations; scoring in the National Student Survey and UKFPO FP survey; and was not associated with school demographic data. A moderate inverse correlation was found between the volume of internal medicine (TeachIntMed) training in the undergraduate curriculum and the volume of MLM training (, r = 0.52, p = 0.02, n = 20 comparisons). Broadly speaking, these results suggest minimal current impact of undergraduate MLM on postgraduate performance metrics. Importantly, these data also indicate that although MLM training volume varies substantially between medical schools, this variation is not likely attributed to school demographic factors such as entry grades (EntryGrades); cohort size (Entrants_N); spend per student (Spend_Student); staff-student ratio (Student_Staff); or student satisfaction rating (NSS_Satisfn). Furthermore, the volume of MLM training provision is not influenced by the total teaching (Teach_GP, Teach_Psyc, Teach_Aes, Teach_OG, Teach_IntMed, Teach_Surg) and assessment times (ExamTime), which might be indicative of overall curricular pressure within individual schools. Taken together, these findings present a reassuring picture of the potential outcomes of current MLM training provision and potential barriers to that provision.
Figure 4. There is no association between the amount of MLM content in the undergraduate curriculum and key postgraduate outcomes. The duration (total and themed) of MLM teaching was correlated with a range of measures including: historic career destinations (1990–2009); demographic data; volume of teaching and assessment; National Student Survey; UKFPO EPM, SJT and Foundation Trainee Survey; trainee destinations (2012, 2014–2016); postgraduate examination performance for MRCP and MRCGP; and fitness to practice (FtP) measures for graduates of each medical school (n = 20 comparisons). Correlogram shows the Pearson r relationships between each variable. *p ≤ 0.05; **p ≤ 0.01; ***p ≤ 0.001; ****p ≤ 0.0001.
Student-perceived barriers to integration of MLM training in the undergraduate curriculum
Current volume of MLM training in the undergraduate curriculum is not associated with overall curriculum time pressures (as measured by the AToMS study (Devine et al. Citation2020)). Despite this, it was interesting to examine the free-text responses of students when asked what barriers they perceive to the integration of MLM training in their curriculum. A word cloud showing the most frequently used words in these free text responses is shown in . Notably, although ‘more,’ ‘importance’ and ‘interest’ featured, the most prominent words were ‘time’ and ‘difficult.’ This suggested that students perceive time pressures influence the inclusion of training on MLM topics.
Figure 5. Barriers to the inclusion of MLM content in the undergraduate curriculum. (A) Free-text responses were invited to the question ‘What barriers are there to including medical leadership and management teaching in the curriculum?’ A word cloud identifies the most frequent words present in n = 626 responses. (B) A representative range of responses given by participants when invited to give a free-text response to the question ‘What medical leadership and management topics are currently taught in your medical school (if any)?’
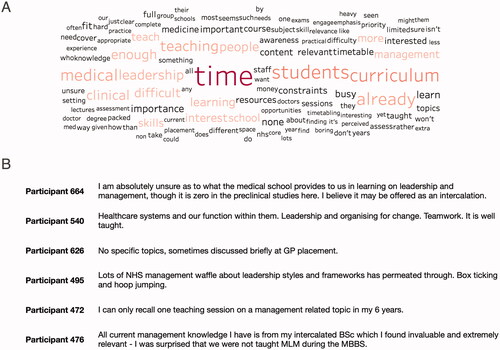
Though barriers clearly exist and integration is variable, students did speak positively as well as negatively about the topics and their experiences. Representative free-text responses to the question: ‘What medical leadership and management topics are currently taught in your medical school (if any)?’ are shown in .
Discussion
Leadership and management training is of vital importance to the delivery of safe and effective healthcare. It has been shown to improve job satisfaction and personal wellbeing of those working in frontline medicine and increases the cost effectiveness of health services (Veronesi et al. Citation2015; Molero Jurado et al. Citation2018). As a result, the current zeitgeist in medical education is that MLM content ought to be delivered to undergraduate medical students ([FMLM] Faculty of Medical Leadership and Management Citation2013). The UK is well placed to evaluate the benefits of an early emphasis on MLM training, with a large number of publicly funded medical schools and an increasing number of standardised postgraduate assessments, surveys and other metrics. Such a wealth of data makes it possible to detect the benefits of such training. In this study, LUMENS 1.0, we sought to detect the baseline level of MLM training recorded on recent undergraduate timetables from a large number of UK medical schools. We then aimed to compare actual timetabled teaching with perceived teaching evaluated by means of a national survey of medical students. Finally, in collaboration with the Medical Student Investigators Collaborative (MSICo; msico.org), we drew on the robust datasets of the recent AToMS and MedDifs studies (Devine et al. Citation2020; McManus et al. Citation2020) to probe the impact of current MLM provision on postgraduate outcomes.
It did not surprise us to find that medical students had not heard of the Medical Leadership Competency Framework (MLCF). First published in 2008, the MLCF standardise domains of knowledge and skills for doctors involved in the planning, delivery and transformation of health services ([FMLM] Faculty of Medical Leadership and Management Citation2013). These domains were recently incorporated to guide an indicative undergraduate curriculum, published by the FMLM in 2018 ([FMLM] Faculty of Medical Leadership and Management Citation2018). Despite a lack of recognition of the MLCF, students did rank several of the domains from the MLCF as being integrated into their curricula. Our findings found that students did not agree that organisation and service leadership domains (improving and managing services and setting direction) were integrated into their curriculum. This represents an area of focus for those planning activities in undergraduate curricula. It may also reflect the somewhat ‘solid state’ nature of the other two domains: demonstrating personal qualities and working with others, which are arguably already well-entrenched into the fabric of medical curricula.
The central finding of this iteration of the LUMENS survey is that MLM training currently comprises an average of 96 hour or 2% of total undergraduate teaching time. Despite this, there is a huge range, with five schools reported as having fewer than 50 hours of timetabled MLM training. Given that 82% of the MLM components in our analysis were teamwork, performance/reflection and communication, this leaves only negligible time for training on patient safety, quality improvement, audit, NHS structure and whistleblowing. Given that 88% of students thought MLM was relevant to them, and yet only 18% considered it to be well taught, it is probable that students do not recognise teamwork, communication skills and reflection as MLM-related content. These neglected areas may therefore align with the three MLCF domains rated by students as being relatively under-integrated.
When asked via free-text response what MLM is taught in their course, the most popular responses did not typically coincide with the most frequently timetabled activity. Patient safety and whistleblowing teaching was the only exception to this. This suggests that despite a wealth of teaching on teamwork, reflection and communication skills, students do not recognise these as ‘leadership and management’ topics and instead recall taught content on patient safety and whistleblowing as being the most relevant answer to such a free-text question. This is interesting as it suggests some of the least taught topics are in fact the most memorable and most relevant to student ideas of what MLM education should be.
Though the benefits of MLM training have been established (Frich et al. Citation2015), there has only been a relatively recent impetus on medical schools to introduce clearly delineated MLM teaching programmes. Given this, we were not surprised to find an absence of association between MLM teaching and postgraduate outcomes, including performance in Royal College examinations; completion of ARCP; and GMC sanctions. The increasing establishment of MLM teaching programmes may influence these findings should LUMENS be repeated in future decades, once graduates have percolated up through to the latter stages of postgraduate training and beyond. As it stands today, there is no evidence to suggest undergraduate MLM teaching as delivered on courses developed for the 2014–2015 academic year influences the future performance of graduates.
Our data describe a ‘level playing field’ in terms of the school demographics, with no association between the current total volume of teaching and assessment and volume of MLM teaching provision. In contrast to students, who – in free-text responses – ranked time as being a prominent barrier to the inclusion of MLM teaching, it is certainly not the case that schools with the least teaching have had more ‘space’ to include MLM teaching, or vice-versa. It is also true that schools with higher spend per student, or higher staff-student ratios are no more inclined to include MLM teaching than those who spend less. Our results therefore suggest an absence of measurable barriers to the inclusion of more MLM teaching in the undergraduate curriculum.
However, it is important to recognise that since the LUMENS 1.0 study was undertaken significant developments in standardising MLM content within undergraduate curricula have taken place. The publication of an indicative undergraduate curricula ([FMLM] Faculty of Medical Leadership and Management Citation2018) linked directly to the GMC’s Outcomes for Graduates, development of an FMLM accreditation for UK Medical Schools, and roll-out of tailored Foundation Priority Programmes in Leadership ([UKFPO] The UK Foundation Programme Office Citation2022) are likely to raise understanding of MLM amongst current medical undergraduates. Future research should assess the impact of these measures.
In summary, we have identified substantial variation in the provisions of MLM teaching in the undergraduate curriculum. We report a clear dichotomy between student perceptions of taught MLM content and actual timetabled teaching. There is minimal association between the amount of timetabled MLM content in the curriculum today and performance at the postgraduate level. Despite this, there is a level playing-field for the development and integration of further such content in the undergraduate curriculum.
Author contributions
KM designed and organised survey distribution, performed initial data analysis and wrote the manuscript. JG was involved in the overall design of the study, interpreted data and wrote the manuscript. CG, BA, SB, RB, RC, HD, AF, ZH, II, TK, AK, RK, EM, JM, EM, SP, DS, VT, SV were responsible for local survey distribution, coded raw timetable data and reviewed the manuscript for critical content. The FMLM student group members listed in Supplementary Appendix A were responsible for local survey distribution, performed data validity checks and reviewed the manuscript for critical content. OPD was involved in the overall design of the study, facilitated collaboration with the MSICo student group, performed data analysis, interpreted data, and wrote the manuscript.
Supplemental Material
Download PDF (287 KB)Acknowledgements
We thank Professor IC McManus and the MSICo student group (msico.org) for the provision of raw timetable data and postgraduate outcome data used in this study. We have received no funding in support of this work.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and swriting of the article.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Notes on contributors
Katherine Aldersley
Katherine Aldersley, BMBS, MSc Public Health, is an Internal Medicine Trainee in Manchester, North Sector.
Jonathan Gibb
Jonathan Gibb, MBChB (Hons), BSc Medicine (Hons), is a National Institute for Health and Care Research Academic Clinical Fellow in General Adult Psychiatry at the University of Bristol, UK.
Charlotte Grainger
Charlotte Grainger, MBChB, BMedSc (Hons), is currently Junior Clinical Fellow in Orthopaedics and Plastic Surgery at King’s College Hospital.
Bilal Abou-el-Ela-Bourquin
Bilal Abou-El-Ela-Bourquin, BSc, MB BChir, is associated with Foundation Programme (East of England), Ophthalmology Specialty Training (Thames Valley Deanery).
Shreya Badhrinarayanan
Shreya Badhrinarayanan, BM BS, FRSPH.
Ravina Bhanot
Ravina Bhanot, MBBS, BSc, is a GP Trainee (North East London Foundation Trust), DRCOG.
Ryan Clark
Ryan Clark, BSc, MBChB, is associated with Foundation Programme (Scotland Deanery).
Hannah Douglas
Hannah Douglas, MBChB, is a Foundation Year 2 Doctor (NHS Lothian).
Akiko Fukui
Akiko Fukui, MBBS, MSc, BSc, is a Foundation Year 1 Doctor.
Zac Hana
Zac Hana, MBBS, is a NHS Clinical Entrepreneur.
Inshal Imtiaz
Inshal Imtiaz, MBBS, is a Foundation Year 2 Doctor.
Tejinder Kalsi
Tejinder Kalsi, MPharm, MBBS, is a Foundation Year 1 Doctor.
Ahmed Kerwan
Ahmed Kerwan, MBBS, MSc Medical Anthropology.
Rajkumar Khera
Raj Khera, MBChB, BSc (Hons), is a 50:50 Clinical Teaching Fellow at University Hospitals of Coventry and Warwickshire NHS Trust.
Eloisa MacLachlan
Eloisa MacLachlan, MBChB, BSc Molecular Medicine, is a Post Foundation Fellow.
Jack McGrath
Jack McGrath, MBBCh, is a Foundation Year 2 Doctor (Cwm Taf Morgannwg University Health Board).
Ellen Meredith
Ellen Meredith, MBBS, Master of Public Health, is a Hospital Medical Officer (St Vincent’s Hospital Melbourne, Australia).
Sam Penrice
Sam Penrice, MBChB.
Dina Saleh
Dina Saleh, MBBS, BSc, is an Internal Medicine Trainee Year 2 Doctor (Imperial College Healthcare NHS Trust).
Vivek Tank
Vivek Tank, MBBS, BSc Sports and Exercise Medicine (Hons), Senior House Officer Doctor (University Hospitals of Leicester).
Sharvari Vadeyar
Sharvari Vadeyar, BMBS, BMedSci, is an Academic Foundation Year Two doctor at Heartlands Hospital finishing in August 2022.
FMLM Medical Student Group, student representatives from all UK medical schools aiming to engage medical students and promote clinical leadership through changes to the curriculum.
Oliver Patrick Devine
Oliver Patrick Devine, MBPhD, BMedSci, is a Academic Foundation Doctor (Guy’s and St Thomas’ Hospital, London) and is a past Chair of FMLM Medical Student Group.
References
- Abbas MR, Quince TA, Wood DF, Benson JA. 2011. Attitudes of medical students to medical leadership and management: a systematic review to inform curriculum development. BMC Med Educ. 11:93.
- Butrous E, Park C, Ward T, Yu C, Lemer C, Woolcock C, Bicknell CD, Warren OJ. 2012. Knowledge and opinions of undergraduate medical students on NHS structure, medical management and leadership: defining the structure of curriculum improvement. Int J Clin Leadersh. 17(3):131–138.
- Department of Health. 2002. Learning from Bristol: The Department of Health’s response to the report of the public inquiry into children's heart surgery at the Bristol Royal Infirmary 1984–1995. London: Department of Health.
- Devine OP, Harborne AC, McManus IC. 2015. Assessment at UK medical schools varies substantially in volume, type and intensity and correlates with postgraduate attainment. BMC Med Educ. 15:146.
- Devine OP, Harborne AC, Layard Horsfall H, Joseph T, Marshall-Andon T, Samuels R, Kearsley JW, Abbas N, Baig H, Beecham J, et al. 2020. The analysis of teaching of medical schools (AToMS) survey: an analysis of 47,258 timetabled teaching events in 25 UK medical schools relating to timing, duration, teaching formats, teaching content, and problem-based learning. BMC Med. 18(1):126.
- [FMLM] Faculty of Medical Leadership and Management. 2013. Medical leadership competency framework. London: Faculty of Medical Leadership and Management.
- [FMLM] Faculty of Medical Leadership and Management. 2018. Medical leadership and management – an indicative undergraduate curriculum. London: Faculty of Medical Leadership and Management.
- Fealy GM, McNamara MS, Casey M, O'Connor T, Patton D, Doyle L, Quinlan C. 2015. Service impact of a national clinical leadership development programme: findings from a qualitative study. J Nurs Manag. 23(3):324–332.
- Francis R. 2013. Report of the Mid Staffordshire NHS Foundation trust public inquiry – executive summary. London: House of Commons.
- Frich JC, Brewster AL, Cherlin EJ, Bradley EH. 2015. Leadership development programs for physicians: a systematic review. J Gen Intern Med. 30(5):656–674.
- General Medical Council. 2018. Outcomes for graduates. London: General Medical Council.
- Gosport Independent Panel. 2018. Gosport War Memorial Hospital – the report of the Gosport Independent Panel. London: House of Commons.
- Harrell FE. 2019. HMISC package. R documentation; [accessed 2021 Oct 22]. https://www.rdocumentation.org/packages/Hmisc/versions/4.2-0.
- Hopkins J, Fassiotto M, Ku MC, Mammo D, Valantine H. 2018. Designing a physician leadership development program based on effective models of physician education. Health Care Manage Rev. 43(4):293–302.
- Jefferies R, Sheriff IHN, Matthews JH, Jagger O, Curtis S, Lees P, Spurgeon PC, Fountain DM, Oldman A, Habib A, et al. 2016. Leadership and management in UK medical school curricula. J Health Organ Manag. 30(7):1081–1104.
- Kennedy I. 2013. Review of the response of Heart of England NHS Foundation Trust to concerns about Mr Ian Paterson’s surgical practice; lessons to be learned; and recommendations. West Midlands: Solihull Hospital Kennedy Breast Care Review.
- Kirkup B. 2015. Morecambe Bay investigation: report. Lancashire: Morecambe Bay Investigation.
- McManus IC, Harborne AC, Layard Horsfall H, Joseph T, Smith DT, Marshall-Andon T, Samuels R, Kearsley JW, Abbas N, Baig H, et al. 2020. Exploring UK medical school differences: the MedDifs study of selection, teaching, student and F1 perceptions, postgraduate outcomes and fitness to practise. BMC Med. 18(1):136.
- Molero Jurado MDM, Pérez-Fuentes MDC, Gázquez Linares JJG, Simón Márquez MDM, Martos Martínez Á. 2018. Burnout risk and protection factors in certified nursing aides. IJERPH. 15(6):1116.
- NHS Leadership Academy NHS Leadership Academy. 2013. Healthcare leadership model, London. https://www.leadershipacademy.nhs.uk/resources/healthcare-leadership-model/.
- O’Hara J. 2018. Report of the inquiry into hyponatraemia related deaths. Northern Ireland: Department of Health.
- Shipton H, Armstrong C, West M, Dawson J. 2008. The impact of leadership and quality climate on hospital performance. Int J Qual Health Care. 20(6):439–445.
- Quince T, Abbas M, Murugesu S, Crawley F, Hyde S, Wood D, Benson J. 2014. Leadership and management in the undergraduate medical curriculum: a qualitative study of students' attitudes and opinions at one UK medical school. BMJ Open. 4(6):e005353.
- R Foundation. 2019. The R Project for Statistical Computing. R Foundation; [accessed 2021 Oct 22]. https://www.r-project.org/.
- Rouhani MJ, Burleigh EJ, Hobbis C, Dunford C, Osman NI, Gan C, Gibbons NB, Ahmed HU, Miah S. 2018. UK medical students’ perceptions, attitudes and interest towards medical leadership and clinical managers. AMEP. 9:119–124.
- Royal Liverpool Childrens Inquiry. 2001. The Royal Liverpool Children’s inquiry report. London: House of Commons. https://www.gov.uk/government/publications/the-royal-liverpool-childrens-inquiry-report.
- Steinert Y, Naismith L, Mann K. 2012. Faculty development initiatives designed to promote leadership in medical education. A BEME systematic review: BEME Guide No. 19. Med Teach. 34(6):483–503.
- Stringfellow T, Rohrer R, Loewenthal L, Gorrard-Smith C, Sheriff I, Armit K, Lees PD, Spurgeon PC. 2015. Defining the structure of undergraduate medical leadership and management teaching and assessment in the UK. Med Teach. 37(8):747–754.
- [UKFPO] The UK Foundation Programme Office. 2022. Foundation priority programmes. https://foundationprogramme.nhs.uk/programmes/2-year-foundation-programme/foundation-priority-programme/.
- Veronesi G, Kirkpatrick I, Altanlar A. 2015. Clinical leadership and the changing governance of public hospitals: implications for patient experience. Public Admin. 93(4):1031–1048.
- Wei T. 2019. Visualization of a correlation matrix [R package corrplot version 0.84]; [accessed 2021 Oct 22]. https://cran.r-project.org/web/packages/corrplot/index.html.
