Abstract
Purpose
Foundation years or internships are an important period for junior doctors to apply their knowledge and gain clinical competency. Experiences gained during the foundation years or internships are likely to inform newly qualified doctors’ opinions about how they want to continue their career. We aimed to understand how medical doctors’ internship experiences influence their career intention/decision.
Methods
We conducted qualitative evidence synthesis using meta-ethnography. We searched six electronic bibliographic databases for papers published between 2000–2020 and included papers exploring how foundation years or internship experiences shape doctors’ career intention/decisions, including in relation to migration, public/private/dual practice preference, rural/urban preference, and specialty choice. We used the GRADE-CERQual framework to rate confidence in review findings.
Results
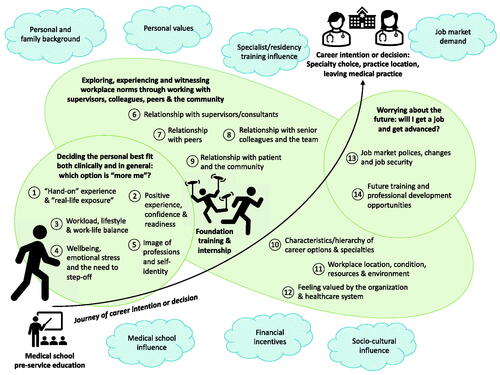
We examined 23 papers out of 6085 citations screened. We abstracted three high-level inter-related themes across 14 conceptual categories: (1) Deciding the personal best fit both clinically and in general (which option is ‘more me’?) through hands-on and real-life experiences (2) Exploring, experiencing and witnessing workplace norms; and (3) Worrying about the future in terms of job market policies, future training and professional development opportunities. Confidence in findings varied but was rated high in 8 conceptual categories.
Conclusions
Our meta-ethnographic review revealed a range of ways in which internship experience shapes medical doctors’ career intentions/decisions allowing us to produce a broad conceptual model of this phenomenon. The results highlight the importance of ensuring sufficient, positive and inspiring clinical exposure, improving workplace environment, relationship and culture, refraining from undermining specific specialities and communicating contractual and job market policies early on to young doctors, in order to attract doctors to less popular specialties or work locations where they are most needed. We propose our conceptual model should be further tested in new research across a range of contexts.
Introduction
The foundation years (FY) or internship is an important period where doctors in training transit from supervised student learning to professional employment, and rapidly assume clinical responsibility under supervision. From this perspective internship occurs after primary academic qualification and typically includes clinical rotations through key specialties in accredited hospital settings. In most countries this is a 1-year programme, though in the UK doctors undertake a 2-year foundation programme. In some countries like the US, the internship is merged with specialty residency training after medical school, and the first year of residency is typically called internship (Zhao et al. Citation2021). Despite the different terminology and different length and context, these junior doctors experience demanding working hours and a need for ongoing learning and assessment (Essa Citation2011; Sturman et al. Citation2017; Carlsson et al. Citation2022) – hereafter we refer to all these positions as internships.
Practice points
Medical regulators and educators, hospital administers, and policymakers should ensure positive and inspiring clinical exposure for interns and also sufficient exposure to different context-relevant career options including specialty rotations and work locations to account for varied preferences.
Sufficient resources like rest and catering facilities and a positive and supportive working environment should also be provided so that interns feel valued.
Changes in contractual, job market and training policies should be clearly communicated early to relieve doctors’ worries about their future.
Resources, guidance and training should be provided to senior healthcare professionals so they can ensure good mentoring practices, refrain from undermining specific specialities and learn how to best support junior doctors’ career decision-making processes.
Future studies should explore whether our conceptual model is appropriate across different countries and contexts, including for different modes of internship (e.g. in the US) and different career outcomes.
Internship years appear to be an important time in career decision making as this is closer to when most apply for specialty training programme or their first job (Scott et al. Citation2013). Experiences gained during the internship are likely to inform newly qualified doctors’ opinions about how they want to continue their career, including in which specialty, organization or even country (Scott et al. Citation2013). In the UK, the proportion of foundation doctors intending to pursue specialty training immediately after FY2 (the 2nd year of the foundation programme) declined from 71.3% in 2011 to 35.5% in 2019. Instead, many took up service roles in the NHS prior to committing to further training, or chose to take a break (GMC Citation2019). Aside from not being accepted by their preferred specialty or location, common reasons for doctors taking a break were the need to prevent or recover from burnout, uncertainty about career direction, feeling pressured to commit to a long training programme, and dissatisfaction with training environments(GMC Citation2019). Importantly, 11% of FY2 trainees expressed an intention to work outside of the UK temporarily or permanently, 7% intended to take a career break and 1% to leave medicine permanently (GMC Citation2019). Such delays or exits can have a negative impact on service delivery and workforce planning (Scanlan et al. Citation2019). These challenges are not unique to the UK (Cronin et al. Citation2019), and for low- and middle-income countries (LMICs) there are also substantial exits from public health systems and migration to high-income countries (Deressa and Azazh Citation2012; George and Reardon Citation2013; Herfs Citation2014; World Health Organization Citation2020).
Previous systematic reviews and evidence syntheses have summarised a broad list of factors that influence medical doctors’ career intentions and decision-making in relation to specialty choice (Puertas et al. Citation2013; Scott et al. Citation2013; Peel et al. Citation2018), retention in the public sector (El Koussa et al. Citation2016), in rural and under-developed areas (Mohammadiaghdam et al. Citation2020; World Health Organization Citation2021) and migration (Blacklock et al. Citation2014). While these reviews provide an overview of factors influencing career decisions across a range of contexts, there has been no in-depth investigation of how experiences during internship influence doctors’ ongoing career decisions. The closest is a review by Stagg et al. (Citation2012) which suggested that positive role models during clinical rotations could change students’ career choices towards rural practice and primary care, whereas negative influences such as surgical supervisors’ disrespect to colleagues and poor teaching could ‘turn off’ students from pursuing a surgical career (Stagg et al. Citation2012). Understanding the link between internship experience and ongoing career decisions is important for workforce planning, as this is a key time point to retain and direct the workforce where it is most needed. The internship period is also arguably amenable to change through action by health facilities, medical regulators, educators and policymakers.
In this review, we aimed to understand how this critical period of internship training shaped junior doctors’ career decision-making. The findings can inform medical regulators and educators, hospital administrators, and policymakers on factors to consider in strengthening internship training and career advice, especially when trying to attract junior doctors to less popular specialties and work locations.
Materials and methods
There are different methods for qualitative evidence synthesis. We chose meta-ethnography, a theory-generating, interpretive methodology for qualitative evidence synthesis as we hoped to develop conceptual understanding through a process of constant comparison of concepts and metaphors, rather than to simply aggregate findings (Noblit and Hare Citation1988; France et al. Citation2019). We followed the 7-stage meta-ethnography approach developed by Noblit and Hare for the synthesis process (Noblit and Hare Citation1988). The stage-by-stage documentation of our synthesis is provided in Supplementary Appendix 1.
Search strategy and screening
With assistance from a specialist medical librarian, we conducted a systematic search using MEDLINE, Embase, Global Health, PsycINFO, Science Citation Index Expanded and Social Sciences Citation Index to identify relevant articles. We combined terms and phrases related to foundation doctors, interns, junior doctors, career choices (such as general terms, specialty choices, migration, rural, public or private sector) and qualitative studies filters (Recherche qualitative [Biblio3S]). We included papers published between 2000 and 2020 in English, and for mixed-methods studies focused only on the qualitative components. The search strategy is provided in Supplementary Appendix 1.
We adopted a broad definition of ‘career intention and decisions’, including but not limited to migration, public/private/dual practice preference, rural/urban preference, and clinical specialty. To meet ‘foundation year or internship experience’ criteria for inclusion, papers had to focus on how doctors’ experience during foundation years or internship impacted their career intention and decisions. We defined internship as the period after primary medical qualification where doctors work in accredited positions in hospital settings to gain supervised experience, in line with another review (Zhao et al. Citation2021).
After de-duplication, two reviewers conducted two stages of independent screening (title and abstract, and full-text) and assessed selected papers for quality and relevance using two methods: (1) the Critical Appraisal Skills Programme (CASP) which includes 10 appraisal questions spanning recruitment strategy to ethical issues, and (2) the global categorization, described by Dixon-Woods et al. (Citation2007) (Malpass et al. Citation2009) which focuses on the ‘richness’ of the findings and their contribution to the synthesis. The global categorization includes four categories: ‘key paper’ (conceptually rich and could potentially make an important contribution to the synthesis), ‘satisfactory paper’, ‘irrelevant’ to the synthesis, and methodologically ‘fatally flawed’ (e.g., unclear study design and data source). ‘Irrelevant’ and ‘fatally flawed’ papers were excluded (Supplementary Appendix 2). We resolved disagreements on inclusion at all stages by discussion among the two reviewers.
Translation and synthesis
We first used NVivo software (version 1.4) to facilitate close reading and extraction and comparison of concepts from each selected paper. Contextual information of all included papers was first extracted and all papers were read thoroughly by the same two reviewers. For further extraction we extracted first-order constructs (participants’ common-sense interpretation in their own words) and second-order constructs (researchers’ interpretation based on first-order constructs), and used both to develop third-order constructs (reviewers’ interpretation of original authors’ interpretation (Schutz Citation2012; Toye et al. Citation2014), as there were studies that did not primarily focus on linking internship experience and career outcomes but had relevant quotations and data supporting that link.
To identify initial constructs, four key papers were selected based on their richness and career outcomes examined. These were examined independently to identify and extract concepts from each paper, and discussed by two reviewers. The remaining papers were extracted by one reviewer and checked by another. Concepts from all included papers were then clustered into relevant categories through constant discussion and comparison. We then went back to the primary papers, and translated and compared our newly developed conceptual categories across all papers to ensure that all relevant data were represented. This translation process was conducted in Microsoft Word, with workings presented in the translation table (Supplementary Appendix 3).
After completing the stages above, we organized the categories by higher-level themes to generate a visual conceptual model to illustrate how the internship experience influenced medical doctors’ career intention/decisions, i.e., our ‘line-of-argument’. We also applied the GRADE-CERQual framework, an approach to assess how much confidence to place in findings from qualitative evidence syntheses, to define our confidence at the category level (Lewin et al. Citation2018). The assessments were made by one reviewer and discussed with the other reviewer.
Results
Search results and article overview
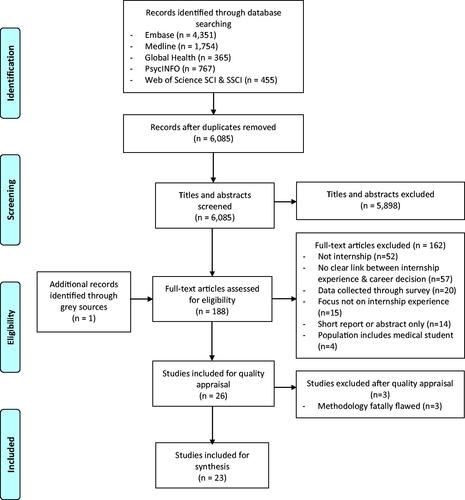
summarizes the results of the search process. Of 6085 citations identified after deduplication, 26 met inclusion criteria after the full-text review. Three further studies were excluded after quality appraisal, leaving 23 studies for the synthesis.
provides an overview of included studies. Most studies included were from high-income countries, including 12 papers from the UK, two from Australia, and one each from New Zealand, Germany, Ireland and the Netherlands. Only three studies were conducted in low- and middle-income countries (LMICs); India (Sreedaran and Hegde Citation2018), Sierra Leone (Woodward et al. Citation2018) and South Africa (Essa Citation2011). Fourteen papers examined career intentions (current interns considering future choices) and nine examined career decisions (doctors retrospectively reflect how they made current career choices). In terms of the career outcome examined, 14 studies examined specialty choices (specifically six general practice, three psychiatry, one surgery and others without a specific specialty focus), three examined practice location (including two rural practice and one migration), three investigated general career intention, two investigated why doctors are not going straight into specialty training (i.e., taking an F3 year in the UK) and one examined leaving specialty training midway (i.e., women leaving surgery training in Australia and New Zealand (Liang et al. Citation2019)).
Table 1. Characteristics of included studies.
Most studies were assessed as good quality against the CASP checklist, however, most lacked a description of the relationship between researchers and participants (Q6). We also rated the papers based on their relevance as described by Dixon-Woods et al. (Citation2005): Twelve papers were rated as key papers and 11 as satisfactory.
We identified 14 categories of how internship experience influence doctors’ career intention/decision, further summarized into three high-level themes. Descriptions are provided below and in .
Table 2. CERQual summary of qualitative findings.
Theme 1: finding which career option is ‘more me’
The papers suggested that interns appraise the potential personal fit between their clinical interests and lifestyle, and to find the ‘more me’ option among different specialties, different roles and positions, and different organizations.
The importance of hand-on experiences, real-life exposure (category 1) and positive experiences (category 2)
The papers drew attention to how the experience of employment gave interns real-life exposure of what it means to be a doctor (with significantly more clinical responsibility as compared with medical students, e.g., prescribing, communicating with patients and families). This appeared to enable them to realize what ‘fits’ with their personality (Scanlan et al. Citation2018; Woodward et al. Citation2018), what they enjoy doing (Williams and Cantillon Citation2000; Querido et al. Citation2018; Sreedaran and Hegde Citation2018; Woodward et al. Citation2018), and what is ‘more me’ (Woodward et al. Citation2018), which influences career decision making (Essa Citation2011).
Importantly there were cases where interns felt poorly prepared for the tasks they encountered e.g., ‘not feeling confident managing very unwell people’ and describing it as anxiety-inducing (Brodribb et al. Citation2016; Spooner et al. Citation2017), or not feeling adequately prepared to enter specialty training (Smith et al. Citation2018). Some studies also suggested that interns realized their responsibilities were quite different from experiences as a student forcing some to reconsider their career choices (Appleton et al. Citation2017; Harris et al. Citation2020).
I hated my job [psychiatry] but I loved it as a student… I just found it really depressing as a doctor whereas as a student I found all the stories really interesting. [GP0P18-(Spooner et al. Citation2017)]
Positive experiences in managing patients, making decisions regarding their care, and seeing positive results helped boost interns’ confidence and sense of readiness (Ludwig et al. Citation2018; Scanlan et al. Citation2018) and inspired some to develop skills in areas they felt inadequately prepared for by medical school (Appleton et al. Citation2017). In some cases, interns could also rebuild their previously damaged confidence with a supportive team and positive experiences (Parker et al. Citation2014; Spooner et al. Citation2017), as an example of positive experience:
It’s a decision that I don’t think I would’ve made. Actually thinking back to making that decision, knowing how confident I was that I enjoyed anaesthetics; it still felt like a big thing to click that button and apply for that job. I most definitely wouldn’t have done that if I hadn’t had that experience in anaesthetics. [Story 2 Steven-(Scanlan et al. Citation2018)]
Considering work-life balance (category 3) and wellbeing (category 4)
Internship exposes individuals to the workloads and working hours of different rotations. The ability to control working hours was a considerable influence on their career decision. Most studies reported having a manageable work-life balance and specialties that fit with lifestyle aspirations as having considerable influence on career decisions, which also had a gender aspect to it, e.g., having children and raising a family (Williams and Cantillon Citation2000; Merrett et al. Citation2017; Querido et al. Citation2018; Scanlan et al. Citation2018; Sreedaran and Hegde Citation2018; Woodward et al. Citation2018). Interns seeking a good work-life balance and the flexibility to pursue interests outside of work seemed to be drawn to specialties that had more regular working hours (Beattie et al. Citation2017; Ludwig et al. Citation2018; Sreedaran and Hegde Citation2018) and some interns stayed away from specialties they loved and had a passion for because the demands of work conflicted with their personal desire to achieve a proper work-life balance (Spooner et al. Citation2017). Internship experience in rural areas was attractive to some interns because of the rural lifestyle, perceived lower stress and greater ability to maintain work-life balance (Cuesta-Briand et al. Citation2020). As an example for work life balance:
I would love to do gastroenterology, but… I just know I wouldn’t have a good work-life balance. Work-life balance is really important to me, I’d probably say more so than what I want to do in my career… if I’m not enjoying myself out of work, it’s just not worth it for me. [GP0P10-(Spooner et al. Citation2017)]
Linked to the working hours and work-life balance were exhausting and stressful rotations. Some were described as being a treadmill with no breaks contributing to burnout and impacting wellbeing (Scanlan et al. Citation2018). Others (e.g., general practice) were described as being lonely with no support and team spirit (Merrett et al. Citation2017). Psychiatry was seen as emotionally draining, with some interns casting doubts on whether they saw themselves working in that field in the future (Beattie et al. Citation2017).
When you’re with a patient and in particular a depressed patient…you feel emotionally drained at the end of it so I don’t know if I could cope with doing that all day for the rest of my life. [Participant 10-(Beattie et al. Citation2017)]
The role of self-identity (category 5)
Although only reported in a few papers, interns also reflected on whether their proposed career, as well as its status and public image, fitted with their self-identity and whether they would be considered a ‘proper doctor’ by choosing these specialties. For instance, they were concerned about being deskilled by choosing to pursue psychiatry because of not dealing with physical health problems (Appleton et al. Citation2017). General practice was perceived to attract less respect and a negative public image because of lack of awareness of what GPs do (Alberti et al. Citation2017; Spooner et al. Citation2017). On the other hand, specialties such as surgery were considered to be of a higher status and power (Olsson et al. Citation2019).
I don’t care what my friends and family think, it’s the wider population. … I had the girl doing my nails one day. She said, ‘Oh, what kind of doctor are you going to be?’ I said, ‘I’m going to be a GP’. And she said, ‘Oh, do you have to go to medical school for that?’ And I just thought, … there’s just that a bit less respect, isn’t there, than, ‘Oh yes, I’m a brain surgeon. [GP1P16-(Spooner et al. Citation2017)]
Theme 2: exploring, experiencing, and witnessing workplace and organizational norms
Through working with people including their direct supervisors/consultants, peers, senior colleagues including medical and nursing staff as well as with the local community, interns got to explore, experience, and witness workplace and organizational norms of medical facilities. This also helped them decide on which specialty, organization and work locations are preferable.
Relationship with consultants (category 6), peers (category 7), senior colleagues and the team (category 8)
The findings demonstrated that consultants and supervisors had a considerable influence on career choice (Croghan and Baker Citation2020). Supervisors as role models moulded interns’ attitudes, making them feel valued and supported (Spooner et al. Citation2017; Scanlan et al. Citation2018) and inspiring interns to want to be like them (Parker et al. Citation2014; Alberti et al. Citation2017; Querido et al. Citation2018). Some consultants also lobbied interns towards their specialty (Olsson et al. Citation2019). In contrast, bullying from supervisors or lack of role models to look up to were reported to contribute to interns shying away from or pausing a career in those specialty areas or work locations (Smith et al. Citation2018; Liang et al. Citation2019).
Building relationships with peers and other team members also played a vital role in enriching interns’ experiences. Positive workplace relationships with other seniors including medical staff and nursing staff influenced career decisions, as they acted as a source of information on training and work opportunities (Cuesta-Briand et al. Citation2020). Interns also sought information from colleagues and from social events organised by specialty unions, career workshops and shadowing doctors to inform their career decision (Spooner et al. Citation2017; Querido et al. Citation2018; Sreedaran and Hegde Citation2018; Olsson et al. Citation2019; Cuesta-Briand et al. Citation2020). In some other cases, interns witnessed their specialty registrars being ‘broken’, or felt unwelcomed or unsupported by the team, or were blamed by seniors when things went wrong, and thus switched their career plans to a different specialty (Spooner et al. Citation2017; Scanlan et al. Citation2018). As an example of relationship challenges with nursing staff:
The nursing staff wouldn't listen to me. They would then go and get consultants and run everything I did past them. There are some strong characters in that department and it’s well known that that is the case. I just clashed with them and I find it quite condescending and made me feel like, that you weren’t a doctor, that you are more a medical student because everything you said had to be verified by a consultant. [P9-(Smith et al. Citation2018)]
Competition between peers put some interns off certain specialties, especially when it was felt to be unhealthy and constraining (Olsson et al. Citation2019).
‘At the surgical and orthopaedic departments where I’ve been, you need to be fairly assertive, even bullish, to somehow get the educational experience you need. You have to make sure you get into theatre, struggle, really, and hinder others in your way to becoming a specialist. And that was not something I had any desire to do. Being somewhere where there was a lot of competition, I wasn’t interested in that. At all’. [No. 5, internal medicine, woman-(Olsson et al. Citation2019)]
Relationship with the community (category 9)
Another key category emerged on relationship with the community. Through working with patients and the community, interns were able to develop close doctor-patient relationships and felt integrated into the community (Querido et al. Citation2018). These experiences made interns appreciate the psychosocial aspects of patient care (Appleton et al. Citation2017) and gave them a sense of helping the community and changed perceptions of where they would want to work (Brodribb et al. Citation2016; Ludwig et al. Citation2018).
Characteristics and hierarchy of career options and specialties (category 10)
Often in their interaction with consultants and other senior colleagues, interns would hear them commenting on other specialties, sometimes stating that some are inferior (Firth and Wass Citation2011; Merrett et al. Citation2017; Croghan and Baker Citation2020; Harris et al. Citation2020). The interns themselves also developed attitudes towards certain specialties interacting with perception of self-identity as discussed previously. For instance, when discussing their career interests with their senior clinicians, ‘just a GP’ or ‘too good for GP’ were often used to create the impression that general practice was inferior, unworthy, unexciting or a reserve option (Alberti et al. Citation2017; Spooner et al. Citation2017). Interns seeking to specialize in psychiatry also described being stigmatized.
There is always a stigma. In my medicine F2 post … I had just finished psychiatry and when I said that I wanted to do psychiatry my consultant said something like ‘then there is no point bothering with you then’ (Appleton et al. Citation2017)
Nonetheless, some interns perceived such comments as ‘banter’, and a natural consequence of consultants’ passion for their specialty.
‘I think there are certain specialties that get made fun of. It hasn’t really had any impact on my decision making. I think probably because they get made fun of, partly, because people are jealous. [FD24, anaesthetics-(Harris et al. Citation2020)]
Workplace resources, environment (category 11) and feeling valued by the organization and healthcare system (category 12)
Interns were drawn to workplace environments with sufficient resources, that were supportive and seen to have high morale. Poor rest facilities, limited access to catering facilities and limited parking contributed to feelings of being unappreciated. This was compounded by the pressures from workloads, to cover rota gaps and from working in poorly resourced facilities (Rizan et al. Citation2019; Hollis et al. Citation2020). In some cases interns felt undervalued and disengaged leading to frustrations with the whole system (Scanlan et al. Citation2018). They described being viewed as ‘ward mules’ used for ‘service provision’ (Rizan et al. Citation2019) or the ‘cheapest option’ to fill rota holes and therefore felt only valued for the heavy workload they carry (Hollis et al. Citation2020).
…So the thought of having to do six, seven years to consultant, there’s no way. There’s literally no way I would do it. Management don’t know who I am, don’t know what I’m about. And if I raise a concern, I think they see that you’re a hassle, it’s a problem, as opposed to, you’re a valued team member that they think is worth being there. I don’t, yes, I don’t feel valued in that capacity. [Story 5 Clare-(Scanlan et al. Citation2018)]
Additionally in one study from South Africa, interns described frustrations with the public health sector, especially regarding management’s misappropriation of funds meant to provide essential resources and equipment in hospitals leading to frequent stockouts, thus ‘that’s why everybody is leaving’ (Essa Citation2011). This could be a specific issue for LMICs.
Theme 3: worry about the future
Aside from personal best fit and the norms of the current workplaces, interns also considered the future implication of their possible career choices, especially whether they would get a job and whether they would advance their career from a training and professional development perspective.
Job market policies and changes (category 13)
Job market policies like wages and employment contracts, and interns’ perceptions about the future job market influenced their career choices. Interns described choosing specialties strategically based on existing workforce gaps or a growing need (e.g., ‘more employable’ (Woodward et al. Citation2018)), or on the contrary after witnessing senior doctors encounter a lack of job opportunities and being disillusioned (Croghan and Baker Citation2020). In some contexts (e.g., UK) changes in junior doctors' contracts also made alternative specialist training unattractive compared to General Practice because the latter has a shorter training period. Changes in employment contracts for junior doctors also made interns consider migrating to work in other countries where they would strike a good work-life balance with better working conditions (Smith et al. Citation2018). However, the influence of job market policies and changes may be limited as they are sometimes difficult to predict (Croghan and Baker Citation2020).
Future training and professional development opportunities (category 14)
Interns described an interest to pursue specializations where there was more 1:1 mentorship and training, as well as commitment from the seniors and the organization towards professional development, (Scanlan et al. Citation2018; Smith et al. Citation2018) instead of specializations where they perform mundane administrative tasks (Hollis et al. Citation2020). On some other occasions, interns with an interest to work in rural areas were frustrated by lack of training pathways and future development opportunities if they do not want to proceed with a GP pathway (Cuesta-Briand et al. Citation2020):
I actually find it very disappointing after working in rural areas and wanting to go back to those areas so badly, that unless you specifically want to be that rural GP, there’s firstly no pathway. And two, it’s not only not encouraged, it’s almost frowned upon. I find it amazing because the whole time I was in rural areas people talk about how much they’re trying to bring people rurally. When I look at it I kind of see a lot of closed doors. [I19; Male; FGY1-(Cuesta-Briand et al. Citation2020)]
Confidence in findings
Details of our GRADE-CERQual assessment are provided in and Supplementary Appendix 4. The assessment of confidence applies only to the 14 categories. We rated 8 categories of high confidence and 5 moderate confidence. The ‘image of professions and self-identify’ was rated very low confidence due to concerns about data adequacy and relevance.
Discussion
Our meta-ethnographic review summarized how experiences during internship appear to significantly influence medical doctors’ career intentions and decisions. We developed a conceptual model to illustrate the journey of career intention/decision making during this period (). Our synthesis highlights that improving internship experiences is a broad agenda. It especially spans ensuring sufficient and positive clinical exposure while maintaining work-life balance and wellbeing, improving workplace environments and culture, building a supportive relationship with consultants and other medical and nursing team members, and relieving worries about future job security and professional development following the internship period.
Figure 2. Line of argument. Note. The final phase of meta-ethnographic analysis is to develop a conceptual model or line of argument that is abstracted from, but more than the sum of, the themes. This figure illustrates our conceptual model which is the journey of career intention decision-making and how foundation years and internship influence such journeys. These junior doctors’ intentions may be shaped early during medical school training, this can be cemented or changed during the chaotic and stressful foundation year and internship training period, which is the focus of our synthesis. Foundation doctors and interns need to decide on the ‘more me’ option of possible career choices (category 1–5), draw on experience in the workplace and relationships with different groups of people (category 6–12), and also think about the future implications of career options (category 13–14). These categories are intertwined and overlapping. We also acknowledged many other factors including personal and family background and personal values may play a significant role in the career-decision making, and doctors could further change their mind during specialist training; moreover, the career decision is also influenced by the job market and employment terms and conditions. These factors extracted from previous reviews are represented (in ‘blue clouds’) outside of the main categories identified by this review, though it should be noted that this is by no means an exclusive list of factors that influence career intention or decision.
While our review focused only on qualitative studies, the impact of internship experience on career decisions is also evidenced by quantitative studies. A survey in Ireland suggested that negative experience as an intern, especially burnout and callousness, was significantly associated with doctors’ intention to leave the country permanently (Cronin et al. Citation2019). Another study in Australia that surveyed medical, nursing, pharmacy and allied health students also confirmed that students satisfied with their rural placement (16–20 weeks for medicine and allied health students and 2–8 weeks for nursing and pharmacy) were twice as likely to consider living and working in a regional, rural or remote location following graduation, after adjusting for other demographic covariates (Fatima et al. Citation2018).
Our findings also align with the wider literature on career decisions and identity work. The social cognitive career theory by Lent et al. (Citation1994) suggests the influence of personal, environmental and learning experiences and the interaction between these as well as contexts that shaped personal agency, formulation, pursuit and attainment of career goals and also performance (Lent et al. Citation1994; Lent and Brown Citation1996). Identity theories especially ‘possible selves’ (Markus and Nurius Citation1986) and ‘provisional selves’ (Ibarra Citation1999) further illustrate how the decisions are made between different career options. Interns observe role models (consultants, or other senior colleagues) to identify potential identities. They then experiment and try on different career options throughout different rotations to inform their career intentions and who they want or fear of becoming, i.e., ‘possible selves’ (Markus and Nurius Citation1986). The theory of ‘provisional selves’ further describes how these possible professional identities are formed, and the process may also include self-evaluation (internal self-congruence) and perceptions of external judgment from either peers, colleagues or society (Ibarra Citation1999). This is in line with our findings especially as interns figuring out their self-identity, relationship with other colleagues and seniors as well as absorbing comments from others on the characteristics and hierarchy of career options and specialties.
Our study has important implications for policy and practice. While internship trainings are context dependent, the following practices should be considered and tested to understand their impact on career planning. Medical regulators and training institutions should ensure interns have sufficient exposure to different career options including specialty rotations and work locations to account for varied preferences. The internship environment should also be regularly monitored to ensure adequate resources are available (Zhao et al. Citation2022). This exposure should allow interns to explore different potential career interests and whether they match their clinical and lifestyle expectations, e.g., incorporating rural clinical rotations may attract junior doctors into rural and remote area practice (World Health Organization Citation2021); arranging short specialty tasters or shadowing senior colleagues may interest junior doctors in specialties with recruitment difficulties (East Anglian Foundation Programme Citation2010). Changes in contractual, job market and future training policies should also be clearly communicated well in advance, by policy makers, regulators and training institutions, to clearly signal upcoming opportunities and alleviate stress about future job security.
Most studies did not report interns receiving formal advice from career advisors, but consultants and other senior colleagues seem key sources of information (Spooner et al. Citation2017; Smith et al. Citation2018; Sreedaran and Hegde Citation2018; Cuesta-Briand et al. Citation2020). Resources, guidance and training should be provided to senior healthcare professionals so they can ensure good mentoring practices, like having regular one-to-ones with trainees focusing not only on educational and academic progress but also on professional and personal growth (Stamm and Buddeberg-Fischer Citation2011; Han et al. Citation2014), refraining from undermining specific specialities and incorporating this into faculty development (NHS Health Education England and Medical Schools Council Citation2016; Alberti et al. Citation2017) and learning how to best support junior doctors’ career decision-making processes. Lastly, sufficient resources like rest and catering facilities and a positive and supportive working environment should also be provided so that interns feel valued, instead of just being made to feel like ‘cheap labour’. This could be as simple as asking consultants and colleagues to remember the names of their trainees (Cleland et al. Citation2018; Scanlan et al. Citation2018).
Several limitations should be considered for this review. To start with, as meta-ethnography is an interpretative approach to qualitative evidence synthesis, a different research team might provide a different interpretation of the data. In our case we re-interpreted some first-order constructs when the paper did not primarily focus on linking experience and career outcomes but where we found relevant data. While we did not contact the original teams and clarify such re-interpretations, the extraction and interpretation of concepts were led by one author and reviewed by another, and further shared and discussed within the whole research team for validation and feedback. Second, we had a very strict definition of internship experience during the screening process and excluded papers focusing on residency unless the papers explicitly stated that the focus was on the first year of residency which is commonly referred to as internship. This resulted in our not including any paper published from the US and other countries where the internship year is embedded in multi-year specialty residency programs, thus our findings might be less applicable to those settings. Third, we acknowledge that both internship and career preference are context-dependent and vary by the socio-cultural environment of the geographical locations in which they are situated and the health system structure. For example in some countries including the UK, the choice to enter the private sector is much more constrained especially for early career doctors as post-graduate training opportunities are limited to public sector, and also ‘rural’ practice in high-income countries could be quite different from many LMIC settings which may be more under-resourced and lacking basic infrastructure (Lehmann et al. Citation2008); Additionally much of our literature is from a small set of countries – for example, only three of our included papers are from LMICs which reflects the paucity of data from regions where the internship experience could be most stressful and from which many junior doctors choose to migrate after internship (Essa Citation2011; George and Reardon Citation2013). Future work is needed to investigate internship experience and career outcomes in different settings and additional factors linking internship experience and career intention/decision. Lastly, while our study focused on a broad list of career outcomes, we did not explicitly differentiate career intentions and career outcomes. Interns could choose a different specialty than their intention due to job market demand or training availability, and such decision-making is dynamic and could change even during specialty training. Our conceptual model () recognized such limitations and highlighted job market demand and other factors that influence career choices identified in previous systematic reviews. We recommend future studies explore whether our conceptual model is appropriate across different countries and contexts, including for different modes of internship (e.g., in the US) while extending research to other factors that might influence career outcomes such as personal values, medical school experiences and job market demands, and other career outcomes for example non-patient facing specialties, research and management.
Conclusion
Our meta-ethnographic review revealed a range of ways in which internship experience shapes medical doctors’ career intentions/decisions. Medical regulators and educators, hospital administrators, and policymakers need to take these into consideration to improve the training experience for these junior doctors generally, but also use to inform efforts to attract doctors to less popular specialties or work locations where they are most needed. We propose our conceptual model should be further tested in new research across different contexts.
Authors contributions
YZ and DM contributed equally to this manuscript. YZ and ME conceived of the analysis. YZ and DM contributed to study selection, screening and analysis. YZ and DM wrote the first draft of the manuscript. CB, DG, CN, SM and ME provided critical feedback on the synthesis and the first draft of the manuscript. All authors read and approved the final manuscript.
Glossary
Meta-ethnography: A theory-generating, interpretive methodology for qualitative evidence synthesis to develop conceptual understanding through a process of constant comparison of concepts and metaphors, rather than to simply aggregate findings.
Supplemental Material
Download Zip (393.9 KB)Acknowledgements
We thank Eli Harriss, the Knowledge Centre Manager at the Bodleian Health Care Libraries, University of Oxford for her support in literature search.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
Notes on contributors
Yingxi Zhao
Yingxi Zhao, MPH, is a PhD (DPhil) student at the Oxford Centre for Global Health Research. His doctoral project focuses on human resource for health in low- and middle-income countries with a specific focus on medical doctor interns.
Daniel Mbuthia
Daniel Mbuthia, MSc, previously worked as an Assistant Research Officer at the health systems and research ethics, KEMRI-Wellcome Trust Research Programme.
Claire Blacklock
Claire Blacklock, MBChB MRCP MRCGP DTM&H PGDip FHEA DFPH, is a PhD (DPhil) student at the Oxford Centre for Global Health Research. Her thesis project aims to understand the role of senior nurses in neonatal care delivery in Kenyan hospitals.
David Gathara
David Gathara, PhD, is an Assistant Professor of Health Systems at the London School of Hygiene and Tropical Medicine.
Catia Nicodemo
Catia Nicodemo, PhD, is a senior research fellow in health economics at Nuffield Department of Primary Health Sciences, University of Oxford.
Sassy Molyneux
Sassy Molyneux, PhD, is Professor in Global Health at the Oxford Centre for Global Health Research, and a senior researcher at the KEMRI-Wellcome Trust Research Programme in Kenya.
Mike English
Mike English, MBBChir, MD, FMedSci, is Professor of International Child Health at the Oxford Centre for Global Health Research. He is a UK trained paediatrician who has worked in Kenya for over 20 years supported by a series of Wellcome fellowships.
References
- Alberti H, Banner K, Collingwood H, Merritt K. 2017. ‘Just a GP’: a mixed method study of undermining of general practice as a career choice in the UK. BMJ Open. 7(11):e018520.
- Appleton A, Singh S, Eady N, Buszewicz M. 2017. Why did you choose psychiatry? A qualitative study of psychiatry trainees investigating the impact of psychiatry teaching at medical school on career choice. BMC Psychiatry. 17(1):276.
- Beattie S, Crampton PES, Schwarzlose C, Kumar N, Cornwall PL. 2017. Junior doctor psychiatry placements in hospital and community settings: a phenomenological study. BMJ Open. 7(9):e017584.
- Blacklock C, Ward AM, Heneghan C, Thompson M. 2014. Exploring the migration decisions of health workers and trainees from Africa: a meta-ethnographic synthesis. Soc Sci Med. 100:99–106.
- Brodribb W, Zadoroznyj M, Martin B. 2016. How do rural placements affect urban-based Australian junior doctors’ perceptions of working in a rural area? Aust Health Rev. 40(6):655–660.
- Carlsson Y, Nilsdotter A, Bergman S, Liljedahl M. 2022. Junior doctors’ experiences of the medical internship: a qualitative study. Int J Med Educ. 13:66–73.
- Cleland J, Roberts R, Kitto S, Strand P, Johnston P. 2018. Using paradox theory to understand responses to tensions between service and training in general surgery. Med Educ. 52(3):288–301.
- Croghan SM, Baker T. 2020. The great gamble? A mixed-methods study of factors influencing medical students in specialty choice. J R Coll Physicians Edinb. 50(4):422–430.
- Cronin F, Clarke N, Hendrick L, Conroy R, Brugha R. 2019. The impacts of training pathways and experiences during intern year on doctor emigration from Ireland. Hum Resour Health. 17(1):74.
- Cuesta-Briand B, Coleman M, Ledingham R, Moore S, Wright H, Oldham D, Playford D. 2020. Understanding the factors influencing junior doctors’ career decision-making to address rural workforce issues: testing a conceptual framework. IJERPH. 17(2):537.
- Deressa W, Azazh A. 2012. Attitudes of undergraduate medical students of Addis Ababa University towards medical practice and migration, Ethiopia. BMC Med Educ. 12(1):68.
- Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A. 2005. Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Policy. 10(1):45–53.
- Dixon-Woods M, Sutton A, Shaw R, Miller T, Smith J, Young B, Bonas S, Booth A, Jones D. 2007. Appraising qualitative research for inclusion in systematic reviews: a quantitative and qualitative comparison of three methods. J Health Serv Res Policy. 12(1):42–47.
- East Anglian Foundation Programme 2010. Guidance on the provision of specialty tasters for foundation doctors [Internet]. [place unknown]. https://heeoe.hee.nhs.uk/sites/default/files/guidance_on_specialty_tasters_for_foundation_trainees_final_feb_2012.pdf.
- El Koussa M, Atun R, Bowser D, Kruk ME. 2016. Factors influencing physicians’ choice of workplace: systematic review of drivers of attrition and policy interventions to address them. J Glob Health. 6(2):020403.
- Essa ZI. 2011. Post-medical interns’ reflections on medical internships in South African state training hospitals. [Thesis] [Internet]. [place unknown]; [accessed 2021 May 11]. http://wiredspace.wits.ac.za/handle/10539/9209.
- Fatima Y, Kazmi S, King S, Solomon S, Knight S. 2018. Positive placement experience and future rural practice intentions: findings from a repeated cross-sectional study. J Multidiscip Healthc. 11:645–652.
- Firth A, Wass V. 2011. The impact of general practice attachments on foundation doctors: achieving the goals of modernising medical careers. Educ Prim Care. 22(5):314–320.
- France EF, Cunningham M, Ring N, Uny I, Duncan EAS, Jepson RG, Maxwell M, Roberts RJ, Turley RL, Booth A, et al. 2019. Improving reporting of meta-ethnography: the eMERGe reporting guidance. BMC Med Res Methodol. 19(1):1–13.
- George G, Reardon C. 2013. Preparing for export? Medical and nursing student migration intentions post-qualification in South Africa. Afr J Prim Health Care Fam Med. 5(1):483.
- GMC. 2019. The state of medical education and practice in the UK 2019 [Internet]. [place unknown]. https://www.gmc-uk.org/-/media/documents/somep-2019–-full-report_pdf-81131156.pdf.
- Han E, Chung E, Oh S, Woo Y, Hitchcock M. 2014. Mentoring experience and its effects on medical interns. Singapore Med J. 55(11):593–597.
- Harris M, Wainwright D, Wainwright E. 2020. What influences young doctors in their decision-making about general practice as a possible career? A qualitative study. Educ Prim Care. 31(1):15–23.
- Herfs PGP. 2014. Aspects of medical migration with particular reference to the United Kingdom and the Netherlands. Hum Resour Health. 12(1):59.
- Hollis AC, Streeter J, Van Hamel C, Milburn L, Alberti H. 2020. The new cultural norm: reasons why UK foundation doctors are choosing not to go straight into speciality training. BMC Med Educ. 20(1):282.
- Ibarra H. 1999. Provisional selves: experimenting with image and identity in professional adaptation. Adm Sci Q. 44(4):764–791.
- Lehmann U, Dieleman M, Martineau T. 2008. Staffing remote rural areas in middle- and low-income countries: a literature review of attraction and retention. BMC Health Serv Res. 8(1):19.
- Lent R, Brown S, Hackett G. 1994. Toward a unifying social cognitive theory of career and academic interest, choice, and performance. J Vocat Behav. 45(1):79–122.
- Lent RW, Brown SD. 1996. Social cognitive approach to career development: an overview. Career Dev Q. 44(4):310–321.
- Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, Bohren MA, Tunçalp Ö, Colvin CJ, Garside R, et al. 2018. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci. 13(1):2.
- Liang R, Dornan T, Nestel D. 2019. Why do women leave surgical training? A qualitative and feminist study. The Lancet. 393(10171):541–549.
- Ludwig K, Machnitzke C, Kühlein T, Roos M. 2018. Barriers to practicing General Practice in rural areas – results of a qualitative pre-post-survey about medical students during their final clinical year. GMS J Med Educ. 35(4):Doc50.
- Malpass A, Shaw A, Sharp D, Walter F, Feder G, Ridd M, Kessler D. 2009. “Medication career” or “Moral career”? The two sides of managing antidepressants: a meta-ethnography of patients’ experience of antidepressants. Soc Sci Med. 68(1):154–168.
- Markus H, Nurius P. 1986. Possible selves. Am Psychol. 41(9):954–969.
- Merrett A, Jones D, Sein K, Green T, Macleod U. 2017. Attitudes of newly qualified doctors towards a career in general practice: a qualitative focus group study. Br J Gen Pract. 67(657):e253–e259.
- Mohammadiaghdam N, Doshmangir L, Babaie J, Khabiri R, Ponnet K. 2020. Determining factors in the retention of physicians in rural and underdeveloped areas: a systematic review. BMC Fam Pract. 21(1):1–23.
- NHS Health Education England, Medical Schools Council. 2016. By choice – not by chance: Supporting medical students towards future GP careers [Internet]. [place unknown]. https://www.medschools.ac.uk/media/2881/by-choice-not-by-chance.pdf.
- Noblit GW, Hare RD. 1988. Meta-ethnography: synthesizing qualitative studies. Newbury Park (CA): SAGE.
- Olsson C, Kalén S, Ponzer S. 2019. Sociological analysis of the medical field: using Bourdieu to understand the processes preceding medical doctors’ specialty choice and the influence of perceived status and other forms of symbolic capital on their choices. Adv Health Sci Educ Theory Pract. 24(3):443–457.
- Parker JE, Hudson B, Wilkinson TJ. 2014. Influences on final year medical students’ attitudes to general practice as a career. Qual Res. 6(1):8.
- Peel JK, Schlachta CM, Alkhamesi NA. 2018. A systematic review of the factors affecting choice of surgery as a career. Can J Surg. 61(1):58–67.
- Puertas EB, Arósquipa C, Gutiérrez D. 2013. Factors that influence a career choice in primary care among medical students from high-, middle-, and low-income countries: a systematic review. Rev Panam Salud Publica. 34(5):351–358.
- Querido S, van den Broek S, de Rond M, Wigersma L, ten Cate O. 2018. Factors affecting senior medical students’ career choice. Int J Med Educ. 9:332–339.
- Recherche qualitative [Biblio3S]. [accessed 2021 Nov 9]. https://extranet.santecom.qc.ca/wiki/!biblio3s/doku.php?id=concepts:recherche-qualitative.
- Rizan C, Montgomery J, Ramage C, Welch J, Dewhurst G. 2019. Why are UK junior doctors taking time out of training and what are their experiences? A qualitative study. J R Soc Med. 112(5):192–199.
- Scanlan GM, Cleland J, Stirling SA, Walker K, Johnston P. 2019. Does initial postgraduate career intention and social demographics predict perceived career behaviour? A national cross-sectional survey of UK postgraduate doctors. BMJ Open. 9(8):e026444.
- Scanlan GM, Cleland J, Walker K, Johnston P. 2018. Does perceived organisational support influence career intentions? The qualitative stories shared by UK early career doctors. BMJ Open. 8(6):e022833.
- Schutz A. 2012. Collected papers I. The problem of social reality. Springer Science & Business Media.
- Scott A, Joyce C, Cheng T, Wang W. 2013. Medical career path decision making: a rapid review. Ultimo (Australia): Sax Institute. https://www.saxinstitute.org.au/wp-content/uploads/REPORT_Medical-career-path.pdf.
- Smith SE, Tallentire VR, Pope LM, Laidlaw AH, Morrison J. 2018. Foundation Year 2 doctors’ reasons for leaving UK medicine: an in-depth analysis of decision-making using semistructured interviews. BMJ Open. 8(3):e019456.
- Spooner S, Pearson E, Gibson J, Checkland K. 2017. How do workplaces, working practices and colleagues affect UK doctors’ career decisions? A qualitative study of junior doctors’ career decision making in the UK. BMJ Open. 7(10):e018462.
- Sreedaran P, Hegde D. 2018. Reasons for pursuing psychiatry as a career: a qualitative study of future psychiatrists from India. Arch Ment Health. 19(1):30.
- Stagg P, Prideaux D, Greenhill J, Sweet L. 2012. Are medical students influenced by preceptors in making career choices, and if so how? A systematic review. Rural Remote Health. 12:1832.
- Stamm M, Buddeberg-Fischer B. 2011. The impact of mentoring during postgraduate training on doctors’ career success. Med Educ. 45(5):488–496.
- Sturman N, Tan Z, Turner J. 2017. “A steep learning curve”: junior doctor perspectives on the transition from medical student to the health-care workplace. BMC Med Educ. 17(1):92.
- Toye F, Seers K, Allcock N, Briggs M, Carr E, Barker K. 2014. Meta-ethnography 25 years on: challenges and insights for synthesising a large number of qualitative studies. BMC Med Res Methodol. 14(1):80.
- Williams C, Cantillon P. 2000. A surgical career? The views of junior women doctors. Med Educ. 34(8):602–607.
- Woodward A, Lake EG, Rajaraman N, Leather A. 2018. Specialist training aspirations of junior doctors in Sierra Leone: a qualitative follow-up study. BMC Med Educ. 18(1):199.
- World Health Organization. 2020. 10 year member state led review of the WHO Global Code of Practice on the International Recruitment of Health Personnel. [Internet]. https://apps.who.int/gb/ebwha/pdf_files/WHA73/A73_9-en.pdf.
- World Health Organization 2021. WHO guideline on health workforce development, attraction, recruitment and retention in rural and remote areas: web annexes. Geneva: WHO.
- Zhao Y, Musitia P, Boga M, Gathara D, Nicodemo C, English M. 2021. Tools for measuring medical internship experience: a scoping review. Hum Resour Health. 19(1):10.
- Zhao Y, Osano B, Were F, Kiarie H, Nicodemo C, Gathara D, English M. 2022. Characterising Kenyan hospitals’ suitability for medical officer internship training: a secondary data analysis of a cross-sectional study. BMJ Open. 12(5):e056426.