ABSTRACT
Purpose
The aim of this study was to investigate the results of all eviscerations and enucleations performed at the Department of Ophthalmology, Sahlgrenska University Hospital, during 2008–2019 and to compare them with previously collected data from 1999 to 2007.
Methods
This was a retrospective investigation using the medical records for all patients having had an evisceration or an enucleation at the Department of Ophthalmology, Sahlgrenska University Hospital, during the two defined periods of time. Main outcome measure was postoperative complications.
Results
During 1999–2007, 181 surgeries were performed, 100 with implants, and 28/100 exposed implants and 9/100 removed implants were recorded during follow-up. During 2008–2019, 250 operations were performed with 158 implants, and there were 3/158 exposed implants and 2/158 extruded implants. Two ruptures of the surgical wound without implant exposure were noted, and one implant was exchanged. The reduction of exposed implants between the two periods was statistically significant (p < .001, Chi-square test). In enucleations, the use of one kind of porous polyethylene implant in the recent study period replaced a multitude of implants in the earlier study period. In eviscerations, the major change between the two study periods was the introduction of the split sclera technique and smaller implant size.
Conclusion
The change in surgical technique between the two periods led to a significant reduction in implant-related complications.
Introduction
Eviscerations and enucleations are the two most common eye amputation techniques and have a long history.Citation1,Citation2 Despite their being well established, both techniques are still developing regarding indications, surgical method and material, and new studies are being published at a steady pace.Citation3–8 At the Department of Ophthalmology, Sahlgrenska University Hospital, data were previously collected and analysed on all eviscerations and enucleations carried out during 1999–2007 as a means of a clinical quality control. That earlier period was published regionally as a report in Swedish under the name “To recreate an eye, 9 years of experience of enucleations, eviscerations and secondary implants at the Department of Ophthalmology, Sahlgrenska University Hospital”.Citation9 Those data will be presented in the Results section of this article for comparison with the more recent data presented in this study. During the earlier period (1999–2007) the incidence of implant-related complications was relatively high, but in the years following (2008 and onwards) the clinical impression of the surgeons was of a significantly reduced incidence of complications. The present study was initiated to determine whether that clinical impression was true. Hopefully, the results of this investigation will be of interest to other surgeons who perform eye-amputating surgery and might help in the further development of surgical technique.
Methods
This was a retrospective study with data collected from the medical records of all the patients operated upon with an evisceration or an enucleation during 2008–2019. It was carried out at the Department of Ophthalmology, Sahlgrenska University Hospital, Sweden, with the permission from the Swedish Ethical Review Authority (2021–03837) and was conducted in agreement with the Declaration of Helsinki.
The already existing data from 1999 to 2007 were first controlled against medical records for type of surgery, surgeon, implant, implant size, implant-related complications and reoperations. Data were reliable except for missing information concerning implant type and size in 20% (not necessarily in the same patient). That material was used for comparison with the more recent study presented here and is referred to as the earlier period.
The variables registered in this study were age, gender, operated side, type of surgery, date of surgery, surgeon, indication for surgery, implant used, any scleral division in the evisceration procedures, size of implant, perioperative complications, postoperative complications, subsequent surgery and prosthesis use.
Surgical methods
Evisceration: A 360-degree peritomy of the conjunctiva was created. The globe was incised at the limbus and the cornea removed and the intraocular contents were taken out. Diathermy was applied to the central retinal artery and the vortex vessels. The internal scleral surface was cleaned with 99.5% alcohol and then rinsed with physiological saline solution. In 86% of the eviscerations with implants, the entire scleral shell was divided in two by a diagonal incision as described by Madottir and Sahlin.Citation10 For the other 14% two relaxing incisions were made from the scleral opening horizontally. In the eviscerations without an implant, the next step was suturing of the sclera with 5–0 polyglactin sutures (Vicryl®) and for the rest a suitable implant size was chosen. An implant was placed deep beneath the scleral shell, which was then sutured with 5–0 polyglactin sutures (Vicryl®). Before inserting the implant, it was soaked in gentamicin solution (18 mg/ml). The conjunctiva and Tenon’s capsule were closed with a running 8–0 polyglactin suture (Vicryl®). A suitably sized conformer (Ocular conformer®) was placed in the socket. All patients who received an implant were administered one dose of cefuroxime (1.5 grams) intravenously perioperatively.
Enucleation: A 360 degree peritomy of the conjunctiva was created. Blunt dissection was performed to free the conjunctiva from the globe and muscles, and the four rectus muscles were identified and cut after securing them with 6–0 polyglactin sutures (Vicryl®). The two oblique muscles were cut, and the globe was amputated and inspected. The surgical area was inspected and some diathermy was applied to the optic nerve stump if needed. Measurements were made to choose the right size of implant. A porous polyethylene implant with drilled channels (Medpor®) was placed deep in the orbit under the Tenon capsule. Before being inserted, the implant it was soaked in gentamicin solution (18 mg/ml). The rectusmuscles were sutured to the implant with 5–0 polyester (Surgidac®). Then, the straight muscles were sutured to each other with 6–0 polyglactin (Vicryl®) in front of the implant. The Tenon was closed in two layers with 6–0 polyglactin (Vicryl®) and then the conjunctiva with 7–0 polyglactin (Vicryl®). A suitably sized conformer (Ocular conformer®) was placed in the socket. In enucleations without an implant, the four rectus muscles were still fastened to each other. All patients who received an implant were administered one dose of cefuroxime (1.5 grams) intravenously perioperatively.
Statistical analysis
Statistical analyses were performed with SPSS version 25.0 (IBM, Armonk, NY, USA). Descriptive statistics, Chi-square test, Fisher's exact test and Student’s T-test for two independent samples were applied when relevant. All tests were two-sided and a p-value of <.05 was considered significant.
Results
During the earlier period (1999–2007), data were collected from all eviscerations and enucleations performed at the clinic with a focus on implants and implant-associated complications. Data from that material that was relevant to the present study are presented in . Among enucleations, three different types of implant material were used, namely, hydroxyapatite, aluminium oxide, and porous polyethylene. The muscles were attached to the porous polyethylene in several different fashions – sutured to a polyglactin mesh around the implant, sutured to autologous sclera covering the implant or sutured through drilled channels in the implant with either polyglactin or polyester sutures. In total, there were seven different implant techniques. In the eviscerations, two different variants of implants were used, namely, porous polyethylene and hydroxyapatite. Exposures occurred with both implants. Eight of the nine exposures were diagnosed in patients going through surgery during the first part of the earlier period. The results of eviscerations and enucleations together amounted to 28/100 (28%) exposed implants and 9/100 (9%) removed implants ().
Table 1. Eviscerations and enucleations during 1999–2007.
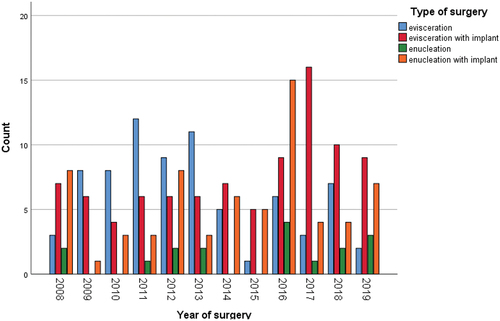
During the more recent period of 2008–2019, 250 operations were carried out. Data were collected at the end of 2021, which enabled a follow-up of at least 2 years (except for the patients operated on at the end of 2019). Data are shown in with eviscerations and enucleations presented separately. The number of surgeries over time is presented in . The number of different procedures varied greatly between years, and looking at , one gets the impression that the number of eviscerations without an implant has diminished over time. If the 12-year period is divided in two 6-year periods, the analysis shows that during the first period, eviscerations with an implant constituted 35/86 (41%) of all eviscerations. In the second period, the number of eviscerations with an implant was 56/80 (70%), and this difference was statistically significant (p < .001, Chi-square test).
Table 2. Demographic data, type of procedure, reason for surgery and surgical data, 2008–2019.
The indications for performing the procedures are also presented in . Infection was for the most part due to keratitis.
Out of 91 eviscerations with implants, 78 (86%) had the sclera divided into two parts as described by Masdottir and Sahlin in order to cover the implant optimally.Citation10
Any difference in mean implant size was analysed between the earlier and the recent period. There was no statistically significant difference in enucleations (p = .36, Student’s T-test). However, in eviscerations, the difference was statistically significant (p = .033, Student’s T-test) with larger implants in the earlier period.
There were few perioperative complications of importance for the surgical outcome. In one evisceration, the surgeon described that the suture of the sclera over the implant was a bit tense. In one enucleation, one rectus muscle was lost and could not be sutured to the implant.
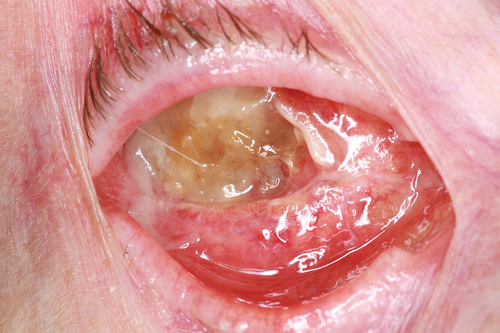
The main outcome of this study was postoperative complications, as presented in . A total of 132/166 (80%) of the eviscerations had no postoperative complication, and for the enucleations, the corresponding number was 70/84 (83%). There were seven implant/wound-related complications (3%) (), and they were operated on by seven different surgeons. Altogether, there were two spontaneous extrusions of the implant, three implant exposures and two ruptures of the surgical wound without implant exposure. These seven different complications resulted in one change of size of the implant and four sutures (one with the addition of a dermis-fat graft), while two of them had no additional surgery. It is difficult to see any specific pattern or common reason for these complications when looking in detail. Univariate analysis of these seven complications due to the size of implant or division of sclera in the evisceration group was not significant, but with such a small number of complications, statistical analysis is not meaningful. Three types of procedures, seven different surgeons, an age-span from 17 to 89 years, both sexes, and different indications for surgery are present in these seven histories. One extrusion could probably have been prevented because the surgeon in question (the author) wrote that the wound was a bit tense at primary surgery. One can assume that if a smaller implant had been used the extrusion could have been avoided. Three post-operative infections needed antibiotic treatment, and these were socket infections without implant infections. The only infection associated with an implant was the one presented as number 3 in . The results of implant-related complications in the two different study groups are presented in , and there was a statistically significant difference in exposures between the two reported periods (p < .001, Fisher's exact test). The most common post-operative problems were related to the eyelids (n = 12), and additional surgery needed after the initial procedures were for the most part directed at the eyelids (27/37, 73%) ().
Figure 3. Comparison of the numbers of implant-related complications and reoperations between the two study periods, n.
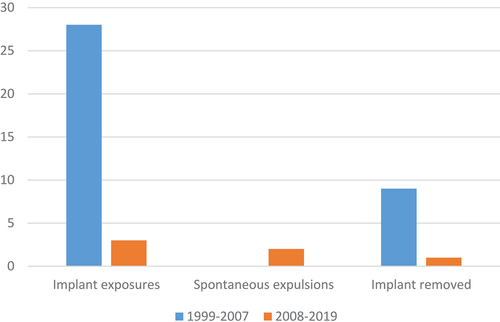
Table 3. Postoperative complications, 2008–2019 (one patient may have several complications).
Table 4. Implant/wound-related complications, 2008–2019, individual patients presented in consecutive order of appearance.
Table 5. Reoperations, 2008–2019.
Post-operative use of ocular prostheses is shown in . Thirteen of the 16 patients not wearing a prosthesis were operated on without an implant.
Table 6. Types of ocular prostheses used, 2008–2019.
Two surgeons were responsible for the majority of all the procedures during both the earlier and the recent period (53% during the earlier and 56% during the recent period). They were also the only ones who performed eye amputations during both periods. Seven surgeons were involved in procedures with implants in the earlier period and nine in the more recent period. The most productive surgeon carried out 60 implant operations during the earlier period followed by 69 during the recent period. This was followed by the other surgeon active during the whole period with 11 implant-surgeries during the earlier period and 33 during the recent period.
Discussion
Our original hypothesis was confirmed, and there has been a considerable reduction in the complication rate for eye-amputating procedures between 1999–2007 and 2008–2019, at least regarding implant-related complications. Four changes in surgical technique over time were identified, and three of them may be important factors for this reduction. Regarding eviscerations, there were three major technical changes between the earlier and the later study periods. During the earlier period, hydroxyapatite and porous polyethylene implants were used but during the more recent study period, mainly silicone but also polyethylene implants were inserted. One other difference is that during the end of the earlier study period we started using the split sclera technique when implanting in eviscerations.Citation10 We believe that using the split sclera technique is the most important factor. The three implant-related complications in the evisceration group of the more recent period all happened with silicone implants. During 1999–2007, implant-related complications occurred both with porous polypropylene and hydroxyapatite. Hence, all three implant types are associated with complications in this study. We started using the split sclera technique at the end of the earlier period, and the patients with exposed implants were almost exclusively operated on during the first part of that period (all but one). That was before the introduction of the split sclera technique. Regarding the three implant-related complications after eviscerations in the recent study period, one occurred after surgery being done without splitting the sclera and could perhaps have been avoided if it had been split. In patient number 3 described in , the sclera was split but was somewhat tense during suture over the implant. With a smaller implant, it is likely that expulsion would not have occurred. There was also a significant difference in implant size between the two periods with the larger size in the earlier period. This is surprising since the split sclera technique enables a larger implant to be fitted in the orbit. Summarizing this, we judge the split sclera technique together with 18 mms mean implant size compared with 19 mms to be the most important factors.
In enucleations, the major difference between the earlier and later period was the implant. In the earlier period, we used a multitude of implants and suturing techniques for the muscles. From 2008, we have only used porous polyethylene with channels and polyester to attach the muscles to the implant. No other changes in surgical technique or perioperative care have been adopted.
The policy at the department is to choose evisceration whenever possible rather than enucleation. The author has worked at the department during the entire period reported in this article and has not noticed any major change in indications. The proportion of enucleations/eye amputations has not changed comparing the two periods (35% and 34%). Enucleation is reserved for malignant tumours and special cases not suitable for evisceration. An evisceration takes about half the time of an enucleation to perform and preserves the anatomy in the socket better, and eviscerations are associated with better post-operative motility and fewer complications.Citation11 The trend towards performing eviscerations, if possible, has also been described by Yousuf et al.Citation12 and Roelofs et al.Citation13 The frequency of inserting an implant at the time of surgery has increased comparing the two periods, from 48% to 69% in eviscerations and from 55% to 80% in enucleations. This probably reflects the improved results, which augments the courage of the surgeon to place an implant.
Complications after eye-amputating surgery are frequently reported,Citation5,Citation11 and exposures have been reported at a frequency of 0–76.5%.Citation4,–Citation8,–Citation11,–Citation14–16 Alwitry et al.Citation17 have published the results of eviscerations and enucleations and porous polyethylene implants. Their surgical technique seems to be very similar to ours, but still they have 6% exposures after enucleations and 54% exposures after eviscerations. Our seven wound-related complications (3%) were definitely in the lower range, which strongly indicates that our present surgical technique is worth considering.
Recently, three independent groups have published studies on risk factors for implant-related complications. Gupta et al.Citation18 presented a case–control study analysed with logistic regression, but no significant risk factor for implant exposure was identified in that material. Kim et al.Citation3 found that orbital cellulitis was the only risk factor for extrusion after evisceration with orbital implant. Habib et al.Citation4 found smoking and immunomodulatory therapy to be associated with implant exposure. It was not possible to include those inherent factors of patients in the present study, but considering the very low incidence of complications in our study, they would probably not have changed the results if included.
A limitation of this article is the retrospective design, and the fact that the surgeons did not actively follow patients. However, we had access to the ophthalmological medical records for the entire geographical area of Western Sweden, and the patients were checked for possible contacts elsewhere. In addition, it is very unlikely that a complication from surgery performed at our department would have been dealt with at another clinic if the patient was still living in Western Sweden. The competence is at our department and the patient would have been referred there. All patients with a prosthesis see an oculist at least every other year and would have been referred to our department if any complications had appeared. In summary, I believe that the number of complications accounted for in this article is very close to the true number of complications.
In conclusion, it is possible to achieve a very low rate of implant-related complications with the right choice of implant and surgical technique. The most probable reasons for improved results in eviscerations were the split sclera technique and a smaller implant. In enucleations, the technique of suturing the straight eye muscles to drilled channels in a porous polyethylene implant with polyester sutures improved the outcome.
Acknowledgements
A part of this article was presented as a poster at ESOPRS 2021 (digital meeting). The author has had a minor commission for SantenPharma AB.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Additional information
Funding
References
- Beard CH. Enucleation. In: Ophthalmic Surgery. Philadelphia, USA: Blakiston’s Son & Co; 1910:457–477.
- Mules PH. Evisceration of the eye and its relation to the bacterial theory of the origin of sympathetic disease. Trans Ophthalmol Soc UK. 1885;5200.
- Kim JM, Sung JY, Lim HB, Choi EJ, Lee SB. Risk factors for orbital implant extrusion after evisceration. J Clin Med. 2021;10(15). doi:10.3390/jmc10153329.
- Habib LA, North VS, Freitag SK, Yoon MK, Lefebvre DR, Grace Lee N. Medical comorbidities and orbital implant exposure. Acta Ophthalmol. 2021;100(3):e813–e819. doi:10.1111/aos.14973.
- Gauthier AC, Oduyale OK, Fliotsos MJ, et al. Clinical characteristics and outcomes in patients undergoing primary or secondary enucleation or evisceration after ocular trauma. Clin Ophthalmol. 2020;14:3499–3506. doi:10.2147/OPTH.S273760.
- Al-Farsi HA, Sabt BI, Al-Mujaini AS. Orbital implant exposure following enucleation or evisceration. Oman J Ophthalmol. 2017;10(2):87–90. doi:10.4103/ojo.OJO_156_2016.
- Chiu SJ, Tan JHY, Currie ZI. To implant or not to implant: emergency orbital eviscerations with primary orbital implants. Eye (Lond). 2021;35(11):3077–3086. doi:10.1038/s41433-020-01382-0.
- Sobti MM, Shams F, Jawaheer L, Cauchi P, Chadha V. Unwrapped hydroxyapatite orbital implants: our experience in 347 cases. Eye (Lond). 2020;34(4):675–682. doi:10.1038/s41433-019-0571-3.
- Bohman E. Att återskapa ett öga: nio års erfarenhet av enukleationer, eviscerationer och sekundära implantationer vid ögonkliniken SU/Mölndal. Skövde: Västra Götalandsregionen; 2009.
- Masdottir S, Sahlin S. Patient satisfaction and results after evisceration with a split-sclera technique. Orbit. 2007;26(4):241–247. doi:10.1080/01676830600985916.
- Nakra T, Simon GJ, Douglas RS, Schwarcz RM, McCann JD, Goldberg RA. Comparing outcomes of enucleation and evisceration. Ophthalmology. 2006;113(12):2270–2275. doi:10.1016/j.ophtha.2006.06.021.
- Yousuf SJ, Jones LS, Kidwell ED Jr. Enucleation and evisceration: 20 years of experience. Orbit. 2012;31(4):211–215. doi:10.3109/01676830.2011.639477.
- Roelofs KA, Aghazadeh H, Cheema M, Weis E, Badilla J. Enucleation and evisceration: an analysis of indications, histopathological findings, and surgical trends over 23 years at a tertiary care hospital in western Canada. Can J Ophthalmol. 2019;54(1):106–110. doi:10.1016/j.jcjo.2018.02.026.
- Lin CW, Liao SL. Long-Term complications of different porous orbital implants: a 21-year review. Br J Ophthalmol. 2017;101(5):681–685. doi:10.1136/bjophthalmol-2016-308932.
- Ranno S, Serafino M, Nucci P. Four petal evisceration versus standard technique: a retrospective study. Eur J Ophthalmol. 2021;31(4):2156–2159. doi:10.1177/1120672120950160.
- Kord Valeshabad A, Naseripour M, Asghari R, et al. Enucleation and evisceration: indications, complications and clinicopathological correlations. Int J Ophthalmol. 2014;7(4):677–680. doi:10.3980/j.issn.2222-3959.2014.04.17.
- Alwitry A, West S, King J, Foss AJ, Abercrombie LC. Long-Term follow-up of porous polyethylene spherical implants after enucleation and evisceration. Ophthalmic Plast Reconstr Surg. 2007;23(1):11–15. doi:10.1097/01.iop.0000249429.02757.6b.
- Gupta R, Hari P, Khurana B, Kiran A. Risk factors for orbital implant exposure after evisceration: a case control study of 93 patients. Indian J Ophthalmol. 2019;67(7):1148–1151. doi:10.4103/ijo.IJO_1813_18.