ABSTRACT
Purpose
The external dacryocystorhinostomy (Ex-DCR) is a reliable but surgically challenging procedure to overcome a nasolacrimal duct obstruction (NLDO). The aim of this study is to describe the outcomes of a modified technique of lacrimal sac opening and to compare it with the conventional Ex-DCR.
Methods
This comparative cohort study included adult patients undergoing Ex-DCR for primary acquired NLDO by or under supervision of one surgeon. Group 1 (conventional Ex-DCR including H-shaped incision, anastomosis of the anterior mucosal flap to nasal mucosal flap and resection of the posterior sac flap) was compared with Group 2 (modified Ex-DCR including excision of the medial lacrimal sac and anastomosis of remaining anterior sac flap to nasal mucosal flap). Outcome measures included the success rate (defined as complete symptom relief or patent irrigation after three months), reoperation rate, redo-free survival within five years, and occurrence of postoperative bleeding and postoperative infection.
Results
138 patients were included. The success rates were 94.7% (54/57 cases) for Group 1 and 96.3% (78/81) for Group 2 (p-value = 0.658). The redo-rate was 5.3% (3/75) in Group 1 and 2.5% (2/81) in Group 2 (p = 0.331). Two-year redo-free survival probability estimates were 89.8% for Group 1 and 96.3% for Group 2, respectively. No complications occurred in Group 2, whereas in Group 1, one patient (1.8%) suffered from postoperative bleeding and one (1.8%) from postoperative infection.
Conclusions
This study showed that our modified Ex-DCR technique is equally efficacious compared with the conventional Ex-DCR technique in adult patients with NLDO.
Introduction
External dacryocystorhinostomy (Ex-DCR) is the gold standard procedure for treating obstructions beyond the common canalicular duct opening. This surgical technique involves the creation of an alternative route for drainage of tears in nasolacrimal duct obstruction (NLDO). Communication between the lacrimal sac and the nasal cavity is allowed by creating a bony ostium. In 1904 the Ex-DCR technique was first described and consisted of resection of the lacrimal sac mucosa, bone, and nasal mucosa through an external skin incision.Citation1 Since then, there has been little change in the external technique, except for the introduction of nasal and lacrimal mucosal flaps, to create an epithelium-lined fistula, and the introduction of silicone intubation.Citation2,Citation3
Ex-DCR has proven to be a reliable operation with reported success rates between 70% and 95%.Citation4 However, the conventional Ex-DCR is a challenging surgical procedure and requires substantial experience. In addition, the duration of this procedure varies and largely depends on the surgical technique as well as anatomical and vascular factors. Over the years, numerous modifications of this surgical technique have been introduced by several authors for a better surgical outcome and to reduce the operative time.Citation5
The success of Ex-DCR depends on a properly sized, located, patent and mucosa-lined anastomosis between the lacrimal sac and the nose.Citation6 Classically, this is achieved by creating a H-shaped incision in both the lacrimal sac and nasal mucosa, with an end-to-end anastomosis of the anterior and posterior mucosal flaps, the classic double flap Ex-DCR.
The alternative anterior flap Ex-DCR technique includes suturing of the anterior flaps and total excision of the posterior flaps. This technique has been associated with equal success rates as Ex-DCR surgery with anterior and posterior flap anastomosis.Citation5–7
Over the years, we have developed a modified technique of lacrimal sac handling during Ex-DCR: with a No 15 scalpel blade we transect the lacrimal sac across its length and excise the medial sac. The anterior lateral sac remnant then serves as a small anterior flap, which is connected to a U-shaped nasal mucosal flap (following lacrimal intubation).
The aims of this study are (1) to describe this not previously published modified technique of lacrimal sac opening and (2) to compare its overall success rates, reoperation (redo) rate, time to redo, and occurrence of postoperative bleeding and postoperative infection with the conventional lacrimal sac management in Ex-DCR.
Methods
Study design
In this retrospective comparative cohort study, patients aged 18 years or older undergoing Ex-DCR for primary NLDO between January 2001 and December 2015 at The Rotterdam Eye Hospital were included. Patients suffered from complaints of epiphora and had a negative Jones 2 test. If patients had surgical treatment for bilateral obstructions, only the first operated eye was submitted to analysis. Patients were excluded in case of a history of a proximal (e.g. canalicular) and/or distal lacrimal intervention (including 3-snip, balloon catheter dilatation, silicone intubation and previous external/endonasal DCR), proximal lacrimal obstruction (discovered through probing or during surgery), history of an acute dacryocystitis, granulomatous disease, ipsilateral lacrimal trauma or tumour.
This study was conducted in accordance with the principles of the Declaration of Helsinki (October, 2008), the guideline for Good Clinical Practice (CPMP/ICH/135/95) and the Medical Research Involving Human Subjects Act (WMO; 2006). The protocol proposal (register number 2016–26) was approved by the local Research Committee.
Surgical techniques
All patients were operated by, or operated under the direct supervision of, one surgeon (DP). Mid 2006, the surgeon adapted his surgical technique of opening the lacrimal sac from the conventional H-shaped incision with posterior lacrimal mucosal flap excision (Group 1, January 2001 – July 2006) to the modified medial lacrimal sac excision (Group 2, August 2006 – December 2015).
All procedures were performed under general anaesthesia in day care. After anaesthetic induction, xylometazoline impregnated nose packing was inserted. The patient was positioned in reverse Trendelenburg position.
A vertical, straight 10–12 mm line on the lateral nose bridge, at the level of or just medially from the angular vein. After a subcutaneous injection of 1–2 cc lidocaine-adrenaline 1:200,000, the marked line was incised with a surgical scalpel with a 15 mm blade. The medial canthal ligament was reached through blunt dissection of the orbicularis oculi muscle fibers. The periosteum along the anterior lacrimal crest was incised and reflected anteriorly using a Rollet Rugine. Any bleeding from small branches of the infraorbital artery running through the fine groove of the frontal process of the maxilla, known as the sutura notha, was addressed with cautery. If needed, the medial ligament was partially cut to create surgical space. The lacrimal sac was displaced laterally with a Freer periosteal elevator, later replaced by a suction device, hereby creating space for the introduction of a Citelli bone punch.
After removing the nose packing, a hole was forced in the thin bone at the junction of the lacrimal bone with the frontal process of maxilla, in the centre or posterior part of the lacrimal fossa. The bony rhinostomy was enlarged using a Citelli bone punch and Kerrison bone punches, until the bone of the lacrimal fossa, and part of the anterior lacrimal crest was removed. Then, an anteriorly based U-shaped nasal mucosa flap was created using a scalpel with a 15 mm blade.
After the dilatation of the superior and inferior punctum, the canalicular ducts were probed.
In Group 1 (conventional Ex-DCR), a conventional H-shaped lacrimal sac incision was performed. The posterior lacrimal flap was excised and after the insertion of a bi- or monocanalicular stent, the anterior lacrimal flap was connected with the U-shaped nasal mucosa flap using two Vicryl® (Polyglactin 910) 6.0 sutures.
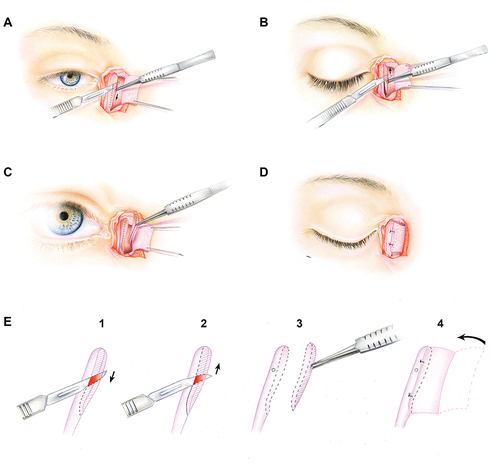
In Group 2 (modified Ex-DCR), at first, the medial wall of the lacrimal sac was tented with a Bowman’s Lacrimal Probe. Then, the excision (decapitation) of the medial lacrimal sac was performed with a through and through vertical cut using a scalpel with a 15 mm blade in a sagittal plane medially of the common canalicular duct (). After insertion of a bi- or monocanalicular stent, the remaining part of the anterior lacrimal sac wall was similarly connected to the U-shaped nasal mucosa flap using two Vicryl® (Polyglactin 910) 6.0 sutures (). A summary of this modified medial lacrimal sac incision and excision is shown in .
Figure 1. A-E: The surgical steps of the modified external dacryocystorhinostomy technique. A-B, opening of the lacrimal sac by a vertical cut in the sagittal plane medially of the common canalicular duct. C, excision of the medial part of the lacrimal sac. D, the remaining part of the anterior lacrimal wall is similarly connected to the U-shaped nasal mucosa flap. E, summary of the steps used in the modified external DCR technique described in this paper.
In both groups, the deep orbicularis layer was finally closed with 2 fast-absorbing Vicryl® (Polyglactin 910) 6.0 sutures, and the skin was closed with intermittent Vicryl® or Prolene® (polypropylene) 6.0. The wound was covered with a double layer of Steri-Strips.
Postoperatively, corticosteroid eye ointment 0.5% was immediately administered. Corticosteroid-antibiotic eyedrops were applied 3 times daily during 2 weeks. The bi- or monocanalicular stent was left in situ for up to 3 months, after which it was removed on an outpatient basis. Whether a bi- or monocanalicular stent was used intraoperatively, depended on changes in personal preference and medical options during that time.
Patients were instructed to contact the hospital in case of persistent epiphora or other complaints after the initial follow-up period.
Data collection and outcomes
Patient files were reviewed and data regarding sex, age, laterality, use of silicone intubation stenting, postoperative complications and long-term outcomes were collected.
The primary outcome was the overall success rate at 3 months, defined as the postoperative resolution of symptoms or, if doubtful, postoperative patency of the lacrimal system on irrigation test (Jones 2 test).
Secondary outcomes included the need for a redo due to insufficient relief of symptoms, postoperative bleeding and infections. Postoperative bleeding was defined as a bleeding necessitating nasal packing or a reoperation. Postoperative infection was considered if necessitating systemic antibiotics.
Statistical analysis
Normally distributed continuous variables were described as mean (± standard deviation). Categorical variables were recorded as counts (percentages). The student’s t-test was applied for the comparison of continuous data whereas the Pearson Chi-square or Fisher Exact Tests were used for categorical data as appropriate.
Follow-up time started at the date of surgery and ended at the date of (1) redo or (2) death or (3) last follow-up (ie, date of last visit). Kaplan-Meier curves were plotted and redo-free survival probability estimates were obtained.Citation8 The log-rank test was used for univariable redo-free survival comparison.
Two-tailed p-values of <0.05 were considered as statistically significant. Statistical analysis was performed using SPSS version 25.0 (IBM Corp, Armonk, NY, USA), and figures were constructed using Graphpad Prism version 7.02 (GraphPad Software, Inc, San Diego, CA, USA).
Results
In total, 223 “eyes” of 192 patients were operated. After the exclusion of other or mixed levels of obstruction (proximal or both proximal and distal obstructions), missing operation data and secondly operated eyes, the study population consisted of 138 eyes in 138 patients. The baseline characteristics are displayed in . The conventional Ex-DCR (Group 1) and modified Ex-DCR (Group 2) groups did not differ significantly in terms of age, sex and laterality. Silicone intubation stenting was used more frequently in Group 2 as compared to Group 1 (87.7% versus 70.2%, p = 0.011) whereas bicanalicular stenting was performed more frequently in Group 1 (Group 1 100% versus Group 2 45.5%, p < 0.001), respectively.
Table 1. Baseline characteristics.
Primary outcome
Overall, Ex-DCR was considered successful in 132 patients (95.7%) at 3 months (). The overall success rates of Ex-DCR within three months were 94.7% (54/57 patients) in Group 1 and 96.3% (78/81 patients) in Group 2 (p = 0.658).
Table 2. Primary and secondary outcomes.
Secondary outcomes
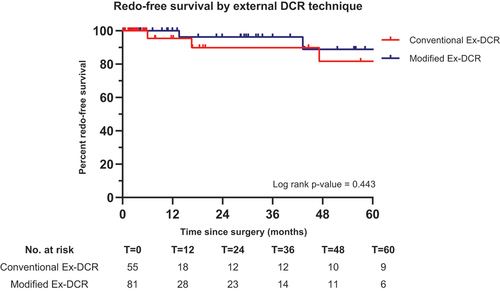
In 5 patients (3.6%) a redo Ex-DCR was performed. In Group 1, a redo Ex-DCR was performed in 5.3% (3/57) as compared with 2.5% (2/81) in Group 2 (p = 0.331). Redo-free survival was similar between both groups (log-rank p = 0.443). Estimated two-year redo-free survival probability estimates were 89.8% for Group 1 and 96.3% for Group 2, respectively. Estimated five-year redo-free survival probability estimates were 81.7% for Group 1 and 88.9% for Group 2, respectively ().
Figure 2. The Kaplan-Meier curves of the conventional and modified external dacryocystorhinostomy techniques.
Overall, a postoperative complication occurred in only 2 patients (1.5%). In Group 2 none of the patients suffered from postoperative bleeding or infection requiring systemic antibiotics. In Group 1, 1 patient (1.8%) developed a bleeding and 1 (1.8%) an infection, respectively. No statistically significant differences were observed in terms of complications ().
Discussion
This comparative cohort study compared the outcomes of a modified technique of lacrimal sac opening, the medial lacrimal sac excision (and anterior flap anastomosis), to the conventional Ex-DCR surgery including H-shaped incision (and anterior flap anastomosis). The Ex-DCR is a reliable − 95.7% success rate in the present series – but surgically challenging procedure to overcome an acquired NLDO. This showed that an Ex-DCR performed with a simple excision of the medial lacrimal sac is at least equally efficacious as the conventional Ex-DCR technique for treating acquired NLDO.
The present study shows that Ex-DCR is a successful technique to treat NLDO since 95.7% of patients had been treated successfully 3 months postoperatively. This percentage is on the high-end as others reported success rates of 90–95% in the literature.Citation4,Citation9 Moreover, there was no statistically significant difference in overall success rates between study groups, which showed that the modified technique is at least non-inferior to the standard DCR technique utilized in our clinic.
In addition, none of the patients undergoing the modified Ex-DCR developed a postoperative complication indicating that the procedure is generally safe in experienced hands.
The modified Ex-DCR techniques as presented in this paper, including excision of the medial lacrimal sac and anastomosis of remaining anterior sac flap to nasal mucosal flap, has several advantages over the conventional technique.
Lacrimal sac management is one of the most important and potentially troublesome steps in DCR surgery. Particularly complex is the fibrosed sac or a sac with altered anatomy, where an incision may cause iatrogenic damage to the common canaliculus associated with a poor outcome.Citation10,Citation11 With this modified technique a safer opening of the lacrimal sac is created. By using a Bowman’s lacrimal probe, the medial wall of the lacrimal sac is tented, showing the (altered) anatomy and thereby guiding the surgeon during this step of the procedure. This initiates a safer entrance of the lacrimal sac and by that less damage to the canalicular communis due to a better visibility during surgery.
In conventional H-opening of the lacrimal sac, the lacrimal surgeon often uses a hooked knife (e.g. phaco-knife) which enters the lacrimal sac from medial to lateral in the direction of the common canalicular outlet. This approach could lead to iatrogenic damage to the common canaliculus and – ultimately – canalicular stenosis. The modified technique, reported here, does not require an extra knife and avoids this type of injury as the plane of sac transection is parallel to the plane of the canalicular outlet in the lateral sac wall.
The modified technique can be performed with the same no 15 surgical blade as is used for the skin incision. In contrast to the additional angled or hooked (phacoemulsification) knife used in the conventional surgical technique, thereby reducing the costs.
Moreover, the conventional technique considering H-opening of the lacrimal sac and subsequent excision of the posterior-lateral lacrimal sac mucosa is (slightly) more time consuming; the modified Ex-DCR technique could therefore reduce the operating time.
Considering that the presented modified Ex-DCR technique includes fewer and less risky surgical steps, one might hypothesize that this technique is faster, safer and could be easier to learn than the conventional technique.
Furthermore, after excising the medial lacrimal sac, there is an extra opportunity for tissue analysis. Thus, a tissue biopsy for pathological analysis is readily available when needed.
Treatment failure and reclosure of the nasolacrimal bypass system is most often due to granulation tissue and obstructing intranasal adhesions. Another possibility is canalicular stenosis, possibly attributed to by iatrogenic trauma due to probing, stenting or lacrimal sac opening.Citation10,Citation11 A bony ostium that is too small also increases the chance of failure. To reduce the risk of recurrent disease, intraoperative stenting can be used as an adjunct to the surgical technique.
In literature, monocanalicular and bicanalicular intubation have similar success rates in congenital NLDO.Citation12 Unfortunately, there is no consensus whether monocanalicular or bicanalicular is the best option in primary acquired NLDO in adults.Citation13,Citation14
In our cohort, there was 1 case of postoperative bleeding and 1 case of postoperative infection, both after the conventional Ex-DCR. The complications had no negative effect on the primary outcome. These findings are consistent with the literature regarding complications after Ex-DCR, although the incidence rates of complications are uncertain due to the very low number of patients developing complications after Ex-DCR.Citation4
This comparative cohort study focussed solely on Ex-DCR and is therefore not suitable for comparison with endonasal DCR techniques. Currently, available data are inadequate to compare endonasal DCR to the gold standard Ex-DCR, but they suggest a wider range of success rates with endonasal DCR technique.Citation9 Still, the disadvantage of a possibly notable scar after Ex-DCR compared to the internal approach should be taken into account. However, previous research has shown that patient satisfaction with the Ex-DCR scar is very high (97%), with the majority considering the scar invisible.Citation15
The present study has several strengths and limitations. The major strength is the implementation and evaluation of a modified Ex-DCR technique in a relatively large cohort within one center by a single surgeon. By including only patients with distal acquired NLDO the cohort was more homogeneous since proximal obstructions have been reported as risk factors for functional failure after Ex-DCR.Citation16 A survival analysis was performed to assess the need for redo procedures over time.
The main limitation is the non-randomized study design. However, evaluating a novel surgical procedure in a randomized design before pilot studies is unfeasible. Therefore, a comparison with an historical cohort was performed. There are no assumptions that the risk of recurrence was higher in the earlier years. Due to the limited number of patients no other methods to adjust for confounding by indication were performed. Since the choice of procedure was dependent on the time period, there are no reasons to assume that patient factors influenced the decision process; no differences were seen in baseline characteristics. The decision whether to place a stent during surgery was based on the personal preference and experience of the surgeon. Furthermore, which type of stent (bi- or monocanalicular) was used depended on the pharmaceutical delivery options at that time. For this reason, the conventional Ex-DCR group had zero monocanalicular stents. This creates a potential risk of selection bias.
Due to the aim of a relatively large single-surgeon cohort, patients were included over a long time span. As a result, the hospital changed from paper records to electronic patient records, and therefore several details such as operative time could not be captured retrospectively. Lacrimal sac sizes were not captured intraoperatively. A prospective study could overcome these limitations. During the first 5 years few reoperations were needed, but a lot of loss to follow-up was observed. This could potentially be a possible selection bias, nevertheless patients were treated in a tertiary referral center and instructed to contact the hospital when persistent epiphora or other complaints after the initial follow-up period occurred.
Conclusion
The prerequisite for any modified DCR technique is to achieve a surgical success rate comparable to that of the reference standard. This study showed that our modified Ex-DCR technique is safe and at least equally efficacious compared with the conventional Ex-DCR technique in adult patients with acquired NLDO. We believe that our modified technique using a simplified opening of the lacrimal sac might be useful for lacrimal surgeons who aim to minimize the steps required for Ex-DCR and the number of required instruments.
Acknowledgment
We thank Jessica Leenen for her artistic contributions.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Additional information
Funding
References
- Toti A. Nuovo metodo conservatoire di cura radicale delle suppurazioni croniche del sacco lacrimale (dacriocistorinostomia). Clin Mod Pisa. 1904;10:385–387.
- Dupuy-Dutemps B. Procede plastique de dacryocystorhinostomie et ses resultants. Annales d’Ocullstique. 1921;158:241–261.
- Jones LT, Wobig JL. Surgery of the Eyelids and Lacrimal System. Birmingham, Alabama, USA: Aesculapius Publishing Company; 1976.
- Jawaheer L, MacEwen CJ, Anijeet D. Endonasal versus external dacryocystorhinostomy for nasolacrimal duct obstruction. Cochrane Database Syst Rev. 2017;2017(2). Art. No.: CD007097. doi:10.1002/14651858.CD007097.pub3.
- Sharma HR, Sharma AK, Sharma R. Modified external dacryocystorhinostomy in primary acquired nasolacrimal duct obstruction. J Clin Diagn Res. 2015 Oct;9(10):NC01–05. doi:10.7860/JCDR/2015/15940.6624.
- Bukhari AA. Meta-analysis of the effect of posterior mucosal flap anastomosis in primary external dacryocystorhinostomy. Clin Ophthalmol. 2013;7:2281–2285. doi:10.2147/OPTH.S55508.
- Kacaniku G, Begolli I. External dacryocystorhinostomy with and without suturing the posterior mucosal flaps. Med Arch. 2014;68(1):54–56. doi:10.5455/medarh.2014.68.54-56.
- Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481.
- Sobel RK, Aakalu VK, Wladis EJ, Bilyk JR, Yen MT, Mawn LA. A comparison of endonasal dacryocystorhinostomy and external dacryocystorhinostomy: a report by the American academy of ophthalmology. Ophthalmology. 2019;126(11):1580–1585. doi:10.1016/j.ophtha.2019.06.009.
- Green R, Gohil R, Ross P. Mucosal and lacrimal flaps for endonasal dacryocystorhinostomy: a systematic review. Clin Otolaryngol. 2017;42(3):514–520. doi:10.1111/coa.12754.
- Lin GC, Brook CD, Hatton MP, Metson R. Causes of dacryocystorhinostomy failure: external versus endoscopic approach. Am J Rhinol Allergy. 2017;31(3):181–185. doi:10.2500/ajra.2017.31.4425.
- Lin AE, Chang YC, Lin MY, Tam KW, Shen YD. Comparison of treatment for congenital nasolacrimal duct obstruction: a systematic review and meta-analysis. Can J Ophthalmol. 2016;51(1):34–40. doi:10.1016/j.jcjo.2015.10.002.
- Kashkouli MB, Kempster RC, Galloway GD, Beigi B. Monocanalicular versus bicanalicular silicone intubation for nasolacrimal duct stenosis in adults. Ophthalmic Plast Reconstr Surg. 2005;21(2):142–147. doi:10.1097/01.IOP.0000155524.04390.7B.
- Saleh GM, Tossounis CM, Litwin AS, Gauba V, Samaras K, McLean CJ. Monocanalicular versus bicanalicular intubation in external dacryocystorhinostomy for primary acquired nasolacrimal duct obstruction. Orbit. 2009;28(2–3):110–114. doi:10.1080/01676830802656711.
- Caesar RH, Fernando G, Scott K, McNab AA. Scarring in external dacryocystorhinostomy: fact or fiction? Orbit. 2005;24(2):83–86. doi:10.1080/01676830590926567.
- Lee MJ, Khwarg SI, Kim IH, Choi JH, Choi YJ, Kim N. Surgical outcomes of external dacryocystorhinostomy and risk factors for functional failure: a 10-year experience. Eye (Lond). 2017;31(5):691–697. doi:10.1038/eye.2016.308.
