Abstract
A permanent facial scar following external approach (transcutaneous) dacryocystorhinostomy is fortunately rare. Meticulous surgical technique is the key factor in avoiding a visible scar.
Simple measures to avoid a scar include use of local anaesthesia, location of the incision, maintaining a bloodless surgical field, using a skin flap technique and simple orbicularis and skin wound closure.
Although endonasal endoscopic dacryocystorhinostomy is gaining clinical acceptance and popularity, the external dacryocystorhinostomy is regarded as the gold standard in terms of surgical success, with a high patient satisfaction.
INTRODUCTION
Most oculoplastic surgeons do lacrimal surgery and although many have experience with dacryocystorhinostomy (DCR) via the endonasal endoscopic approach, there remains a prominent place for external-approach DCR and it is still considered the gold standard. It is the gold standard Citation1, Citation2. Of course, avoiding the cutaneous approach eliminates the risk of scarring, but there are occasions where an external approach may be preferable. For instance, for full access to the inside of the lacrimal sac to biopsy a suspected tumour or granulomatous lesion or to perform a retrograde canalicular intubation, and when there is displaced thick bone following trauma Citation3.
Measures to avoid a visible cutaneous scar in external DCR include infiltration with a local anaesthetic (bupivicaine and lignocaine plus epinephrine 1:400,000) to maintain a blood-free field, and meticulous surgical technique with a carefully placed skin incision and layered soft tissue surgery to avoid damage to the orbicularis Citation3, Citation4, Citation5, Citation6. Selective peroperative intravenous antibiotic helps reduce the risk of wound infection Citation7. Avoiding trauma, infection and inflammation all help to avoid a visible scar.
As an alternative to doing a standard external or endonasal endoscopic DCR, you can consider performing an “external” DCR via a retrocanalicular Citation8, conjunctival Citation9 or eyelid Citation10 approach. The retrocanalicular approach provides a novel “halfway” route but is probably best reserved for simple nasolacrimal duct obstruction with an enlarged sac to facilitate making the flaps.
There is tremendous pressure on lacrimal surgeons from their patients and referring physicians to do endonasal surgery; younger and middle-aged patients have heard of endonasal lacrimal surgery and wish to avoid a cutaneous scar, whilst older frail patients opt for the slightly less invasive and quicker endonasal technique Citation11. However, the incidence of a permanent cutaneous scar in external DCR is low and, in my practice, I recall only two bowed scars over the last 10 years that required z-plasty revision one year after surgery. In each patient there was an identifiable reason why the scar had formed, namely, incorrect placement of the incision in one patient and in the other, the “surgeon got lost”, damaged the orbicularis and used several subcutaneous 6/0 Vicryl sutures.
The paper by Caesar and McNab Citation12 in this issue of Orbit is one of the first attempts to quantify the problem of the DCR scar using a retrospective postal questionnaire. They reinforce the above perception by finding a very low rate of visible scar post-surgery.
Their paper sounds an accord with lacrimal surgeons. Does this mean that the need for endonasal surgery is diminished and we can all do external DCR with impunity?
WHAT IS ALL THE FUSS ABOUT?
The patient is a sensitive being and doesn't want a cut on the face, however well positioned and carefully sutured. It's associated with pain, is going to be visible for at least 1–3 weeks, maybe longer, and is going to have sutures (unless glue is used), which requires a visit to the nurse in the Lacrimal Clinic for removal. It is a visible incision that patients dislike, a temporary disfigurement, rather than the long-term risk of scar. Caesar and McNab Citation12 go a long way in their elegant study to reassure us that most external DCR surgery in careful hands does not cause a long-term problem.
When counselling patients pre-operatively we should warn them that with external DCR there is a visible incision for a few weeks, but that this does not equate with a long-term scar.
FIVE SIMPLE MEASURES TO AVOID A SCAR IN EXTERNAL DCR
1. Local Anaesthesia
Infiltrate a mixture of long- and short-acting local anaesthetics with epinephrine into the soft tissue on the side of the nose where the incision is planned, even if the surgery is under general anaesthesia. This helps provide a bloodless field and hence reduces the risk of tissue damage, especially to the orbicularis muscle. In addition, neurosurgical patties soaked with epineophrine 1 in 10,000 placed in the wound help reduce bleeding. The blood loss at external DCR should be minimal and barely enter the sucker tubing.
2. Incision Site and Shape
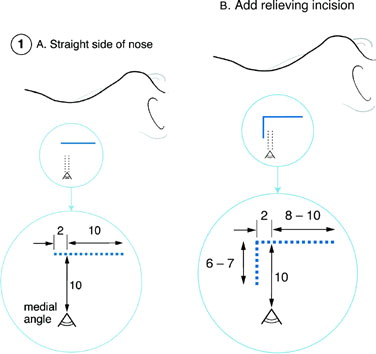
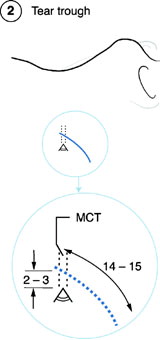
Choose the site and shape of the skin incision carefully. The most common incision is vertical, approximately 12 mm long, extending 2 mm above the level of the medial canthal tendon and placed 10 mm from the medial canthal angle. A neat trick in older lax skin that may rip is to do a planned superior relieving incision. There is also the lower curved tear-trough incision (see and ).
3. Bloodless Field
This is essential, see measures 1 and 4.
4. Skin Flap Approach to the Lacrimal Fossa
Create a skin flap and work between the skin and orbicularis to protect the angular vein from damage. Divide the pretarsal and preseptal fibres of the orbicularis to gain access to the anterior lacrimal crest. This stepped incision is self-sealing with no deep sutures required. In addition, neurosurgical patties soaked with epinephrine 1 in 10,000 placed in the wound help reduce bleeding. The blood loss at external DCR should be minimal and barely enter the sucker tubing.
5. Wound Closure
Avoid using any sutures at all in the orbicularis. If the skin flap stepped incision is used, the orbicularis is merely gently repositioned at the end of surgery and the skin closed with 6.0 monofilament or absorbable suture. These sutures are removed 5–10 days after surgery.
CONCLUSION
These five tips are a brief description of techniques to avoid a scar. External DCR has a fantastic anatomical and functional success rate but does take a little longer than the endonasal route Citation11. Endonasal techniques do not quite reach the level of success of external DCR yet, but are getting closer with powered tools—mechanical endonasal DCR Citation13, Citation14. Do not abandon the proven external DCR yet, enjoy the endonasal route and strive to maintain the external approach as well, without a scar.
REFERENCES
- Tarbet K J, Custer P L. External dacryocystorhinostomy. Surgical success, patient satisfaction and economic cost. Ophthalmology 1995; 102: 1065–1070, [PUBMED], [INFOTRIEVE], [CSA]
- Kashkouli M B, Parvaresh M, Modarreszadeh M, et al. Factors affecting the success of dacryocystorhinostomy. Orbit 2003; 22: 247–255, [PUBMED], [INFOTRIEVE], [CSA], [CROSSREF]
- Olver J M. Chapter 5: Adult lacrimal surgery. Colour Atlas of Lacrimal Surgery 1st ed. Butterworth-Heinemann, Oxford 2002; 91–144
- Harris G J, Sakol P J, Beatty R L. Relaxed skin tension line incision for dacryocystorhinostomy. Am J Ophthalmol 1989; 108: 742–743, [PUBMED], [INFOTRIEVE]
- Dortzbach R, Woog J J. Small-incision techniques in ophthalmic plastic surgery. Ophthalmic Surg 1990; 21: 615–622, [PUBMED], [INFOTRIEVE]
- Caesar R H, McNab A A. External dacryocystorhinostomy and local anaesthesia: techniques to measure minimised blood loss. Ophthalmic Plast Reconstr Surg 2004; 20: 57–59, [CSA], [CROSSREF]
- Yazici B, Meyer D R. Selective antibiotic use to prevent postoperative wound infection after external dacryocystorhinostomy. Ophthalmic Plast Reconstr Surg 2002; 18: 331–334, [CSA], [CROSSREF]
- Adenis J -P, Robert P -Y. Retrocanalicular approach to the medial orbit for dacryocystorhinostomy. Graefe's Arch Clin Exp Ophthalmol 2003; 241: 725–729, [CSA], [CROSSREF]
- Liu D. Conjunctival incision for primary conjunctivodacryocystorhinostomy with Jones tube. Am J Ophthalmol 2000; 129: 244–245, [PUBMED], [INFOTRIEVE], [CSA], [CROSSREF]
- Putterman A M. Eyelid incision approach to dacryocystorhinostomy facilitated with a mechanical retraction system. Am J Ophthalmol 1994; 118: 672–674, [PUBMED], [INFOTRIEVE], [CSA]
- Malhotra R, Wright M, Olver J M. A consideration of the time taken to do dacryocystorhinostomy (DCR) surgery. Eye 2003; 17: 691–696, [PUBMED], [INFOTRIEVE], [CROSSREF]
- Caesar R H, Fernando G, Scott K, McNab A A. Scarring in external dacryocystorhinostomy: Fact or Fiction?. Orbit 2005; 24: 83–86
- Moore W M, Bentley C R, Olver J M. Functional and anatomic results after two types of endoscopic endonasal dacryocystorhinostomy: surgical and holmium laser. Ophthalmology 2002; 109: 1575–1582, [PUBMED], [INFOTRIEVE], [CSA], [CROSSREF]
- Tsirbas A, Davis G, Wormald P J. Mechanical endonasal dacryocystorhinostomy versus external dacryocystorhinostomy. Ophthalmic Plast Reconstr Surg 2004; 20: 50–56, [CSA], [CROSSREF]