Abstract
This study assessed the effect of different surface conditioning methods and ageing protocols on adhesion of resin cement to hybrid ceramic and polymeric CAD/CAM materials. CAD/CAM materials (n = 360, n = 30 per group), namely (a) Lithium disilicate (IPS e.max CAD-LIS), (b) Zirconia (IPS e.max ZirCAD-ZIR), (c) Polymer (Lava Ultimate-LAV), (d) Polymer infiltrated ceramic network (Enamic-ENA), (e) Polymer infiltrated ceramic (Experimental-1-CS1), (f) Polymer infiltrated ceramic (Experimental-2-CS2), (g) Lithium disilicate reinforced alumina (n!ce-NIC) were cut into slices (3 × 6 × 8 mm3) and conditioned: (a) Method 1: 5% hydrofluoric acid etching (H)+silane and (b) Method 2: Silica coating (CoJet (A)+silane). Group LIS was conditioned with only Method 1 and Group ZIR only with Method 2 (control). Resin cement (Variolink Esthetic II) was bonded onto the conditioned specimens and photopolymerized. One-half of the specimens was subjected to ageing (thermocycling 5–55°, 5000 cycles) and the other half was stored in distilled water (37 °C, 24 h). The resin-substrate interface was loaded under shear forces in a Universal Testing Machine (1 mm/min). Data (MPa) were analyzed using two-way ANOVA and Tukey`s tests (α = 0.05). Substrate type, conditioning method and ageing had a significant effect on adhesion values (p < .05). In aged conditions, ENA-H, ENA-A, LAV-H, LAV-A, CS2-A (15 ± 4 – 11.6 ± 5) showed no significant difference (p > .05), with the CS2-A (15 ± 4) showing the least reduction (5.5%) compared to all other groups (5.8–62.6%). CS1-A (100%) followed by ENA-H, ENA-A (93%), CS2-A (80%) presented the highest incidence of cohesive failures after ageing.
Introduction
The advances in the field of ceramics and resin composite materials in restorative dentistry significantly decreased the use of metals in dentistry. This is also in part due to increased implementation of Computer Aided Design/Computer Aided Manufacturing (CAD/CAM) technologies in dentistry. Besides optical expectations, with recent CAD/CAM materials, the lost tooth substances could be restored with materials having similar physical properties compared to that of the dentin and enamel. While ceramics have superior optical properties, they are known to be stiffer and more brittle, which leads to chipping of the veneering ceramics and excessive tooth wear of the antagonistic teeth. On the other hand, although resin composite materials demonstrate low mechanical properties and poor wear resistance, their fabrication is considerably easier and cheaper compared to ceramic materials [Citation1].
The introduction of multiphase materials aims to unify the best mechanical characteristics of resin composites and ceramics. Contemporary CAD/CAM materials are typically based on glassy matrix ceramics (lithium disilicate), polycrystalline ceramics (zirconia), highly filled polymers or sometimes classified as resin nano ceramic (RNC) [Citation2], polymer infiltrated ceramic network (PICN) [Citation3,Citation4] or hybrid ceramics that are usually a mixture of lithium disilicate, alumina and zirconia or aluminium-enriched feldspar-ceramic fused by a polymeric material.
Several studies have investigated the mechanical properties of recent CAD/CAM materials reporting higher modulus of elasticity compared to conventional dental ceramics, lower resistance to wear and thereby being less abrasive to the opposite dentition [Citation5,Citation6]. However, for the longevity of reconstructions and in particular the minimal invasive ones made of hybrid CAD/CAM materials not only the physical properties but also the adhesion of the resin cements to these restorative materials as well as to the tooth structures are of significant importance [Citation7,Citation8]. Adhesive cementation increases the retention and the fracture resistance of such restorative materials enhances the marginal adaptation and prevents micro-leakage at the restoration margins. Regarding traditional ceramic and resin composite materials, the literature provides reliable and well-established adhesion protocols [Citation9]. Since glassy matrix ceramics (i.e. feldspath, lithium disilicate) are acid-sensitive, they are recommended to be etched with 5 to 9.6% hydrofluoric acid (H) gel. The resulting selective solubility of the silicate phase yields to surface degradation and eventually a topographic relief that favours micro-mechanical retention. Furthermore, the application of a silane coupling agent on the etched ceramic surface increases the chemical bonding between the ceramic and the resin cement [Citation10–12]. This process promotes the cement hydrophilicity on the given ceramic surface [Citation13,Citation14] enhancing the contact with resin cement. In addition, the bifunctional silane coupling agents couple the silica oxides of the ceramics to the organic matrix of the resin cement by means of siloxane bonds [Citation15,Citation16]. As regards to resin composite materials, surface conditioning with air-borne particle abrasion with aluminum-oxide (Al2O3) particles has been recommended as the most effective method to roughen the surface reliably [Citation17]. Independent of the indirect resin composite-type particle size of about 50 µm, appears to be sufficient to create a sufficiently rough surface [Citation18–25]. In addition, previous studies reported even improved adhesion to resin composites through tribochemical silica coating (CoJet or Rocatec system, 3 M ESPE, St. Paul, MN, USA) that provides physicochemical surface conditioning (air-abrasion followed by silanization) often resulting in cohesive failure in the substrate [Citation19,Citation21–23,Citation25,Citation26].
Unlike ceramic and resin composite materials, there is a lack of information regarding the best possible and durable adhesion protocol to be employed in on hybrid materials [Citation27]. Since some hybrid ceramic materials contain no polymer network but a variety of glassy matrix or polycrystalline ceramic particles, others are based on a mixture of feldspathic ceramic infiltrated with the polymer. In fact, both phases require and benefit from different types of surface conditioning. Yet, application of multiple conditioning methods may yield to cross-contamination of the surface by each method. On the other hand, while some manufacturers suggest only either HF acid etching, others advice only air-abrasion claiming that one conditioning method would deliver sufficient adhesion. However, in fact, both the organic and inorganic compounds of the hybrid materials need to be conditioned accordingly where the HF etching is known to be more effective on the organic part and air-abrasion on the inorganic one. This discrepancy between manufacturers` instructions yields to confusion among clinicians as regards to cementation protocols.
The objectives of this study were, therefore, to evaluate the effect of two different surface conditioning methods on adhesion of resin cement to different CAD/CAM materials with and without ageing and investigate on the failure types after debonding. The hypotheses tested were that type of surface conditioning method would not show significant effect on adhesion and that ageing would decrease adhesion significantly.
Materials and methods
The brands, types, manufacturers and chemical compositions of the materials used in this study are listed in . Distribution of experimental groups based on the CAD/CAM materials, conditioning methods and ageing procedure are presented in .
Figure 1. Experimental sequence and allocation of groups depending on the material type and surface conditioning.
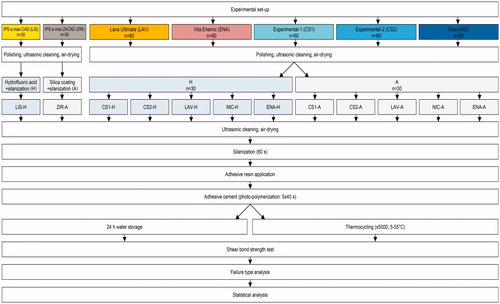
Table 1. The brands, chemical compositions, manufacturers, and batch numbers of the main materials used in this study.
Specimen preparation
Blocks of seven different CAD/CAM materials (n = 360, n = 30 per group), namely (a) Lithium disilicate (IPS e.max CAD-LIS, Ivoclar Vivadent, Schaan, Liechtenstein), (b) Zirconia (IPS e.max ZirCAD-ZIR), Ivoclar Vivadent), (c) polymer (Lava Ultimate-LAV, 3 M ESPE, Minnesota, USA), (d) Polymer infiltrated ceramic network (Enamic-ENA, VITA Zahnfabrik, Bad Säckingen, Germany), (e) Polymer infiltrated ceramic (Experimental-1-CS1, GC, Tokyo, Japan), (f) Polymer infiltrated ceramic (Experimental-2-CS2, GC), (g) Lithium disilicate reinforced alumina (n!ce-NIC, Institut Straumann AG, Basel, Switzerland) were cut into slices (3 × 6 × 8 mm3) using a precision cutting machine (Struers Accutom-50, Struers A/S, Ballerup, Denmark).
The specimen surfaces were polished using silicon carbide papers in sequence of 600, 800 and 1200 grit (English Abrasives Ltd, London, United Kingdom) under water cooling and ultrasonically cleaned (Vitasonic, VITA Zahnfabrik) for 5 min in distilled water and dried. The specimens were then assigned to one of the following surface conditioning methods:
Surface conditioning methods
Method 1 (H): Material surfaces were etched with 5% hydrofluoric acid (H) (VITA Ceramic Etch, VITA Zahnfabrik) for 60 s, rinsed with air-water spray and dried. Then one coat of silane coupling agent was applied (Monobond Plus, Ivoclar Vivadent) with a clean micro brush and waited for its reaction for 60 s.
Method 2 (A): Material surfaces were air abraded using chairside silica coating system (CoJet System, 3 M ESPE) for 20 s from a distance of approximately 10 mm under a pressure of 2.5 bar.
Group LIS was conditioned with only Method 1 and Group ZIR only with Method 2 and acted as the control groups.
Before cementation, a thin layer of adhesive resin (Heliobond, Ivoclar Vivadent) was applied with a clean micro brush, the excess adhesive was removed with air and photo-polymerized for 20 s (XL 3000, 3 M ESPE; light output: 500 mW/cm2). Then, the translucent polyethylene mould (inner diameter: 3 mm; height: 5 mm) was fixed with a holder on the conditioned substrate in order to avoid its movement during filling with the cement. A new polyethylene mould was used for each specimen. Low viscous resin cement (Variolink Esthetic II, Ivoclar Vivadent) was mixed following the manufacturer’s instructions and injected into the mould from the top using a syringe (Centrix, DF, Rio de Janeiro, Brazil) onto the conditioned specimens. Excess resin material was hardly experienced due to perfect sealing of the moulds and the holder positioning mould on the substrate firmly and when then it was removed from the boarders of the polyethylene mould with a microbrush. The cement in the moulds were then photo-polymerized for 40 s from the top and four different sides of each specimen. Then, oxygen inhibiting gel (Oxyguard II, Kuraray Co. Ltd, Tokyo, Japan) was applied on the free surfaces for 1 min and washed and rinsed. The same operator who was previously calibrated for the study performed all the surface conditioning and cementation work.
One half of the specimens was subjected to ageing (thermocycling 5000 cycles, 5–55°, dwell time: 30 s) (Haake DC 10, Sigma-Aldrich, St. Louis in Missouri, USA) and the other half was stored in distilled water at 37 °C for 24 h [Citation28].
Macroshear test
Specimens were mounted in the specimen holder of the Universal Testing Machine (Zwick ROELL Z2.5 MA 18-1-3/7, Ulm, Germany) and the force was applied to the adhesive interface until failure occurred. The load was applied with a 50 kgf load cell to the substrate-adherend interface as close as possible to the surface of the substrate at a crosshead speed of 1 mm/min and the stress-strain curve was analyzed with the software program (TestXpert®, Zwick ROELL, Ulm, Germany).
Failure type evaluation
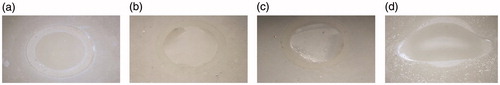
Failure sites were initially observed using an optical microscope (Zeiss MC 80 DX, Jena, Germany) at ×50 magnification. The failure types were classified as follows: Score 1 = Adhesive failure at the ceramic-cement interface with no cement remnants left on the substrate; Score 2 = <1/3 cement left adhered on the substrate; Score 3 = >1/3 cement left adhered on the substrate; Score 4 = Cohesive failure within the substrate.
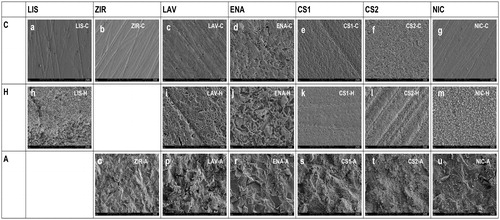
In order to evaluate the qualitative alterations on the substrate surfaces, from each group three additional specimens were prepared (polished-unconditioned, H and A conditioned). After ultrasonic cleaning, they were evaluated under the scanning electron microscopy (SEM). The specimens were coated with gold and palladium sputter and placed in high vacuum. Qualitative examination was performed under a magnification of ×5000, at 5 kV (Zeiss Supra V50, Carl Zeiss, Oberkochen, Germany).
Statistical analysis
Statistical analysis was performed using statistical software R [Citation29] including the package ggplot2 (R Foundation for Statistical Computing, Vienna, Austria) [Citation29]. A sample size of 15 in each group was calculated to have more than 80% power to detect a difference in means of 4 MPa. This assumes that the mean ± standard deviation ranges between 1 and 4 using a two-group Satterthwaite t-test with a 0.05 two-sided significance level. Kolmogorov-Smirnov and Shapiro–Wilk tests were used to test the normal distribution of the data. The means of each group were analyzed using a two-way analysis of variance (2-way ANOVA) and Tukey`s post hoc tests with the shear bond strength (MPa) as the dependent variable and substrate types (7 levels: LIS, ZIR, CS1, CS2, LAV, NIC, ENA), conditioning method (2 levels: H vs A) and ageing (2 levels: dry versus thermocycling) as the independent factors. P values <.05 were considered to be statistically significant in all tests.
Results
Type of substrate, conditioning method and ageing had significant effect on adhesion values (p < .05) ( and ).
Table 2. Results of 2-way ANOVA and Tukey`s post hoc tests.
Table 3. P values indicating significant differences between the mean shear bond strength of the resin cement to the substrate types (MPa) in dry and aged conditions. For groups abbreviations see .
In dry conditions, regardless of conditioning method ENA-H (18.4 ± 3.9), ENA-A (19 ± 4) and CS2-H (15.3 ± 4.2) and CS2-A (15.9 ± 3.3) showed no significant difference (p > .05) (, ). NIC-H (18.3 ± 3.1) was also not significantly different compared to these groups (p > .05). In aged conditions, ENA-H, ENA-A, LAV-H, LAV-A, CS2-A (15 ± 4 – 11.6 ± 5) showed no significant difference (p > .05), with the CS2-A (15 ± 4) showing the least reduction (5.5%) compared to all other groups (5.8–62.6%) in adhesion after ageing.
Figure 2. Boxplot of mean shear bond strength results (MPa). The box displays the data distribution between the first three quartiles. The horizontal line within the box represents the median values. Each point stands for a specimen measurement. For group descriptions see .
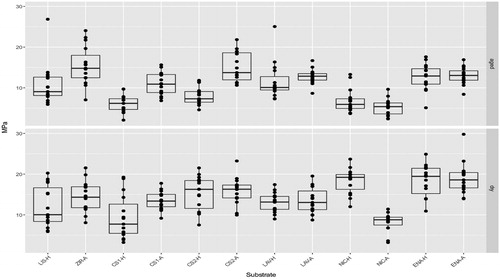
Table 4. The mean shear bond strength and standard deviations of the resin cement to the CAD/CAM materials (MPa ± standard deviations) after two surface conditioning methods.
While in dry conditions, exclusively cohesive failures were observed in CS1-A, ENA-H and ENA-A, and after ageing, CS1-A (100%) followed by ENA-H, ENA-A (93%), CS2-A (80%) presented the highest incidence of cohesive failures ().
Figure 3. Representative digital microscopy photos of the failure types after debonding (a) Score 1 = Adhesive failure at the ceramic-cement interface with no cement remnants left on the substrate, (b) Score 2 = ≤1/3 cement left adhered on the substrate, (c) Score 3 = ≥1/3 cement left adhered on the substrate, (d) Score 4 = Cohesive failure within the substrate.
SEM microphotographs of the substrate surfaces (×5000) at baseline (control-C) indicated the rougher surfaces with porosities with ENA followed by CS2, LAV and CS1 compared to other materials. After hydrofluoric acid etching (H), ENA material showed again distinct etched pattern followed by LAV and LIS demonstrating dissolved areas of the matrix. After silica-coating (A) however, the substrate surfaces showed evident roughened surfaces with the impact of sand particles offsetting the variations in microtexture observed at baseline ().
Figure 4. SEM microphotographs of the substrate surfaces (×5000) at baseline (control-C) (a–g) Note the ENA material showing rougher surface with porosities followed by CS2, LAV and CS1 compared to other materials, after hydrofluoric acid etching (H). (h–m) Note again that ENA material followed by LAV and LIS presenting etched patterns with dissolved areas of the matrix, after silica-coating (A) (o–u) Note the coverage of the substrate surfaces with sand particles offsetting the variations in microtexture observed at baseline.
Discussion
CAD/CAM materials of hybrid nature, be it polymeric or ceramic, differ greatly in their composition where surface conditioning method dictates the adhesion of resin cement to such materials. This study was undertaken in order to evaluate the effect of two different commonly applied surface conditioning methods, namely hydrofluoric acid etching (H) and silica coating followed by silanization (A) on the adhesion of resin cement to various CAD/CAM materials with and without ageing. Based on the results of this study, since the surface conditioning method type significantly affected the results, the first hypothesis could be rejected. On the other hand, ageing decreased the bond strength results significantly, yielding to acceptance of the second hypothesis.
In order to measure the bond strength values between an adherent and a substrate, a number of test methods could be employed. Overall, adhesion-related studies in dentistry, require bonded surface areas ranging from 3 mm2 to 1 mm2 in macro- and micro-test methods, respectively [Citation30,Citation31]. Due to the reduced bonded area and more homogeneous distribution of stresses, micro-test methods tend to show significantly higher bond strength results than the macro-test methods which could eventually affect the ranking of materials being tested in one study [Citation31,Citation32]. In this study, macroshear test method was chosen considering the polymeric and ceramic phases present in one material such as in the case of ENA. The larger bonded surface area would involve the adhesion of the resin both to the polymeric and the ceramic component of the material. Similarly, in the case of LAV, for instance, the polymeric network contains a high amount of inorganic fillers and adhesion of the resin cement to both phases was expected to differ on one substrate. Information derived from macroshear tests was expected to tackle the problem of adhesion aspects to multiphase materials as by definition they cover a larger bonded surface area.
In this study, for highly filled polymer (LAV), polymer infiltrated ceramic network (ENA), polymer infiltrated ceramic (CS1 and CS2) and lithium disilicate reinforced alumina (NIC), surface conditioning with chairside silica coating followed by silanization, resulted in similar or even better bond results compared to H conditioning method. In fact, H is a well-established method, for dissolving the silica phase of the glassy matrix ceramics but polycrystalline ceramics show better bond strength after surface roughening by air particle abrasion and silanization [Citation9]. Yet, among the materials LAV, ENA, CS1 and CS2 presenting both organic and inorganic phases did not benefit from H application only. Although SEM images showed distinct solubility of the inorganic phase after H application, surface conditioning with A provided similar or better adhesion results, especially after ageing conditions. It could be anticipated that the coating encompassing alumina and silica particles allowed for more durable siloxane bonds on the coating when compared to their adhesion to inorganic phase after H only. Furthermore, the voids created after H application were most likely more prone to water penetration and thereby, more hydrolytic degradation after thermocycling [Citation33]. The percentage decrease of adhesion with CS1-H (35.5) CS2-H (47.4), LAV-H (10.6), ENA-H (31.7) clearly supports this assumption. In a previous study [Citation34] where microshear test was employed, H method applied on LAV, ENA, CS did not improve adhesion of resin cement compared to non-conditioned groups after 5000 cycles of thermocycling. In that study, ENA (8.7) showed significantly higher bond strength values compared to CS (7.6) and LAV (7.2). Yet, the difference was only within the range of 1 to 1.5 MPa. Although no conditioning was practiced in our study, the findings of this previous study, partially confirm less effect obtained from H on multiphase materials since in some groups H and A presented no significant difference (LAV and ENA). In another study where micro tensile test was used, ENA after H method delivered high bond strength values (23.4) being not significantly different to that of A (15.7) [Citation35]. Similarly, LAV presented significantly higher bond strength with A (16.8) compared to H only (11.2) after 10.000 cycles of thermocycling. It has to be noted that the standard deviations in that study were higher than those observed in our study which could be attributed to the above-mentioned issues related to the test methods. Moreover, the pretest failures during cutting were not involved in that study [Citation35]. In this study, no pretest failures were experienced during thermocycling. Nevertheless, considering the hazardous compounds, present in H and concerns on clinical applications of such agents chairside [Citation36], the A conditioning method appears to offset the variations in substrate characteristics [Citation3,Citation33,Citation36–38]. In addition, moderate roughening with 30 µm silica particles apparently delivers better adhesion as supposed to 110 µm Al2O3 for conditioning organic and inorganic materials [Citation39,Citation40] where also the latter yields to more frequent adhesive failures [Citation41]. The manufacturer’s instructions of ENA suggests the use of 5% H etching prior to cementation whereas the instructions for LAV suggests the A method. However, based on the high degradation rate after H application on especially for CS1 and CS2, clinicians may consider using the A method only for these materials.
Bond strength results in adhesion studies should be also interpreted with failure types. Cohesive failures in the substrate indicate that bond strength of the adhesive system and the resin cement exceeds that of the cohesive strength of the substrate. In this study, after ageing, CS1-A (100%) followed by ENA-H, ENA-A (93%), CS2-A (80%) presented the highest incidence of cohesive failures, presenting more reliable adhesion results coupled with the bond strength results.
Among tested CAD/CAM materials, NIC was a lithium disilicate reinforced alumina where neither H nor A resulted in high bond strength values. Moreover, the hydrolytic degradation with this material was the highest especially after H compared to all tested materials. The manufacturer of this material suggests the use of H but clinicians should note the decrease in adhesion after this conditioning method in conjunction with this material.
One interesting finding of this study was the non-significant adhesion values between the non-aged and aged ZIR groups. Typically, hydrolytic degradation of methacrylate or phosphate monomer base adhesive resin has been evident in numerous previous studies [Citation42]. One reason for the stable bond to ZIR in this study could be attributed to the higher degree of polymerization of the tested resin cement where the photo-initiator has been changed from conventional camphorquinone to lucirin which certainly needs further investigation.
Reflecting the increase in digital applications and intention to produce tooth-like materials with organic and inorganic phases in dentistry, clinicians should consider the corresponding conditioning method prior to adhesive cementation. In this regard, the manufacturer’s instructions are not well- established for all materials and attempts are being made to avoid the use of H clinically or at the lab site [Citation37]. In this context, silica coating and silanization could be a more general option to condition CAD/CAM materials of organic or inorganic origin or a combination of them both, providing that hydrolytic degradation is still unavoidable with either H and A at varying rates which needs to be clinically confirmed.
Conclusions
From this study, the following could be concluded:
The adhesion of the tested resin cement to the CAD/CAM materials was influenced by the surface conditioning method type, ageing and the type of substrate.
For highly filled polymer (LAV), polymer infiltrated ceramic network (ENA), polymer infiltrated ceramic (CS1 and CS2) and lithium disilicate reinforced alumina (NIC), surface conditioning with chairside silica coating followed by silanization, resulted similar or better bond results compared to hydrofluoric etching and silanization.
After ageing, reduction in bond strength was observed in all cement-material combinations with the least for CS2 after silica coating and silanization. Ageing resulted in more hydrolytic degradation in hydrofluoric acid etched groups as opposed to silica coating and silanization.
After silica coating and silanization similar or higher incidence of cohesive failures were evident compared to hydrofluoric etching and silanization after ageing, except for NIC.
Clinical relevance
Considering higher bond strength values and high incidence of cohesive failure types, overall, either polymeric or ceramic contemporary multiphase hybrid CAD/CAM materials could be conditioned with silica coating and silanization prior to adhesive cementation which could substitute the use of hydrofluoric etching and silanization.
Acknowledgements
The authors acknowledge Mr. A. Trottmann and Mrs. B. Sener, University of Zürich, Center for Dental and Oral Medicine, Zürich, Switzerland, for their assistance with the specimen preparation, and GC Tokyo, Japan, Ivoclar Vivadent, Schaan, Liechtenstein and Institut Straumann AG, Basel, Switzerland for generous provision of the materials.
Disclosure statement
The authors did not have any commercial interest in any of the materials used in this study.
References
- Ruse ND, Sadoun MJ. Resin-composite blocks for dental CAD/CAM applications. J Dent Res. 2014;93:1232–1234.
- Koller M, Arnetzl GV, Holly L, et al. Lava ultimate resin nano ceramic for CAD/ CAM: customization case study. Int J Comput Dent. 2012;15:159–164.
- Bähr N, Keul C, Edelhoff D, et al. Effect of different adhesives combined with two resin composite cements on shear bond strength to polymeric CAD/CAM materials. Dent Mater J. 2013;32:492–501.
- Coldea A, Swain MV, Thiel N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent Mater. 2013;29:419–426.
- Albero A, Pascual A, Camps I, et al. Comparative characterization of a novel cad-cam polymer-infiltrated-ceramic-network. J Clin Exp Dent. 2015;7:e495–e500.
- Awada A, Nathanson D. Mechanical properties of resin-ceramic CAD/CAM restorative materials. J Prosthet Dent. 2015;114:587–593.
- Hayashi M, Tsuchitani Y, Kawamura Y, et al. Eight-year clinical evaluation of fired ceramic inlays. Oper Dent. 2000;25:473–481.
- Fradeani M, Redemagni M. An 11-year clinical evaluation of leucite-reinforced glass-ceramic crowns: a retrospective study. Quint Int. 2002;33:503–510.
- Özcan M, Vallittu PK. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent Mater. 2003;19:725–731.
- Aida M, Hayakawa T, Mizukawa K. Adhesion of composite to porcelain with various surface conditions. J Prosthet Dent. 1995;73:464–470.
- Della Bona A, Shen C, Anusavice KJ. Work of adhesion of resin on treated lithia disilicate-based ceramic. Dent Mater. 2004;20:338–344.
- Özcan M, Barbosa SH, Melo RM. Effect of surface conditioning methods on the microtensile bond strength of resin composite to composite after aging conditions. Dent Mater. 2007;23:1276–1282.
- Lu R, Harcourt JK, Tyas MJ, et al. An investigation of the composite resin/porcelain interface. Aust Dent J. 1992;37:12–19.
- Phoenix RD, Shen C. Characterization of treated porcelain surfaces via dynamic contact angle analysis. Int J Prosthodont. 1995;8:187–194.
- Soderholm KJ, Shang SW. Molecular orientation of silane at the surface of colloidal silica. J Dent Res. 1993;72:1050–1054.
- Matinlinna J, Lassila LV, Özcan M, et al. An introduction to silanes and their clinical applications in dentistry. Int J Prosthodont. 2004;17:155–164.
- Özcan M, Koc-Dundar B. Composite-composite adhesion in dentistry: a systematic review and meta-analysis. J Adhes Sci Tech. 2014;21:2209–2229.
- Swift EJJ, Brodeur C, Cvitko E, et al. Treatment of composite surfaces for indirect bonding. Dent Mater. 1992;8:193–196.
- Imamura GM, Reinhardt JW, Boyer DB, et al. Enhancement of resin bonding to heat-cured composite resin. Oper Dent. 1996;21:249–256.
- Shortall AC, Baylis RL, Wilson HJ. Composite inlay/luting resin bond strength-surface treatment effects. J Dent. 1996;24:129–135.
- Bouschlicher M, Cobb D, Vargas M. Effect of two abrasive systems on resin bonding to laboratory processed indirect resin composite restorations. J Esthet Restor Dent. 1999;11:185–196.
- Nilsson E, Alaeddin S, Karlsson S, et al. Factors affecting the shear bond strength of bonded composite inlays. Int J Prosthodont. 2000;11:52–58.
- Soares CJ, Giannini M, Oliveira MT, et al. Effect of surface treatments of laboratory-fabricated composites on the microtensile bond strenght to a luting resin cement. J Appl Oral Sci. 2004;12:319–326.
- D'Arcangelo C, Vanini L. Effect of three surface treatments on the adhesive properties of indirect composite restorations. J Adhes Dent. 2007;9:319–326.
- Ellakwa AE, Shortall AC, Burke FJ, et al. Effects of grit blasting and silanization on bond strengths of a resin luting cement to Belleglass HP indirect composite. Am J Dent. 2003;16:53–57.
- Yoshida K, Kamada K, Atsuta M. Effects of two silane coupling agents, a bonding agent, and thermal cycling on the bond strength of a CAD/CAM composite material cemented with two resin luting agents. J Prosthet Dent. 2001;85:184–189.
- Spitznagel FA, Horvath SD, Guess PC, et al. Resin bond to indirect composite and new ceramic/polymer materials: a review of the literature. J Esthet Restor Dent. 2014;26:382–393.
- International Organization for Standardization. Dentistry- polymer-based crown and bridge materials. Geneva: ISO; 1996. [ISO 10477].
- The R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2015. https://www.R-project.org/2015.
- Valandro LF, Özcan M, Amaral R, et al. Effect of testing methods on the bond strength of resin to zirconia-alumina ceramic: microtensile versus shear test. Dent Mater J. 2008;27:849–855.
- Bracher L, Özcan M. Adhesion of resin composite to enamel and dentin: a methodological assessment. J Adhes Sci Technol. 2018;32:258–271.
- Betamar N, Cardew G, van Noort R. Influence of specimen designs on the microtensile bond strength to dentin. J Adhes Dent. 2007;9:159–168. 32.
- Elsaka S. Bond strength of novel CAD/CAM restorative materials to self-adhesive resin cement: the effect of surface treatments. J Adhes Dent. 2014;16:531–540.
- Cekic-Nagas I, Ergun G, Egilmez F, et al. Micro-shear bond strength of different resin cements to ceramic/glass-polymer CAD-CAM block materials. J Prosthodont Res. 2016;60:265–273.
- Frankenberger R, Hartmann VE, Krech M, et al. Adhesive luting of new CAD/CAM materials. Int J Comput Dent. 2015;18:9–20.
- Özcan M, Allahbeickaraghi A, Dundar M. Possible hazardous effects of hydrofluoric acid and recommendations for treatment approach: a review. Clin Oral Invest. 2012;16:15–23.
- Marshall SJ, Bayne SC, Baier R, et al. A review of adhesion science. Dent Mater. 2010;26:e11–e16.
- Reymus M, Roos M, Eichberger M, et al. Bonding to new CAD/CAM resin composites: influence of air abrasion and conditioning agents as pretreatment strategy. Clin Oral Investig. 2018;[in Press]:[1–10].
- Valandro LF, Özcan M, Bottino MA, et al. Bond strength of a resin cement to high-alumina and zirconia-reinforced ceramic: the effect of surface conditioning. J Adhes Dent. 2006;8:175–181.
- Kim JE, Kim JH, Shim JS, et al. Effect of air-particle pressures on the surface topography and bond strengths of resin cement to the hybrid ceramics. Dent Mater J. 2017;36:454–460.
- Campos F, Almeida CS, Rippe MP, et al. Resin bonding to a hybrid ceramic: effects of surface treatments and aging. Oper Dent. 2016;41:171–178.
- Özcan M, Bernasconi M. Adhesion to zirconia used for dental restorations: a systematic review and meta-analysis. J Adhes Dent. 2015;17:7–26.
