?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Low back pain (LBP) is the most common injury in golfers of all abilities. The primary aim of this review was to improve understanding of human golf swing biomechanics associated with LBP. A systematic review using the PRISMA guidelines was performed. Nine studies satisfying inclusion criteria and dually reporting golf swing biomechanics and LBP were identified. Human golf swing biomechanics potentially associated with LBP include: reduced lumbar flexion velocity; reduced transition phase length; reduced lumbar torsional load; earlier onset of erector spinae contraction; increased lumbar lateral flexion velocity; reduced or greater erector spinae activity; and earlier onset of external oblique contraction. These potential associations were undermined by a very limited and conflicting quality of evidence, study designs which introduced a severe potential for bias and a lack of prospective study design. There is no conclusive evidence to support the commonly held belief that LBP is associated with “poor” golf swing technique. The potential associations identified should be further investigated by prospective studies of robust design, recruiting participants of both sexes and dexterities. Once firm associations have been identified, further research is required to establish how this knowledge can be best integrated into injury prevention and rehabilitation.
KEY POINTS
LBP has the highest incidence of any injury in elite, sub-elite and recreational golfers, causing a significant burden of injury worldwide.
There is very limited and conflicting evidence that some human biomechanical factors in the golf swing may be associated with LBP.
Prospective studies investigating the full movement pattern are required in order to improve understanding of the potential relationship between the biomechanics of the golf swing and LBP.
KEYWORDS:
1. Introduction
LBP represents a spectrum of disorders encompassing bony, musculotendinous, ligamentous and joint-related injuries, in addition to non-specific pain of no clear aetiology (Knezevic et al., Citation2021). The repeated application of mechanical stress has been associated with LBP, and demonstrable structural tissue changes have been reported in people with LBP, including degeneration of the lumbar facet joints, intervertebral disc degeneration, fascial contusion, localised tissue exudate accumulation and atrophy of the lumbar musculature (Goubert et al., Citation2016; Mohd Isa et al., Citation2022; Song et al., Citation2023).
The golf swing is a synchronous series of complex asymmetric movements. It can be generally described in four distinct phases: setup, the backswing, the downswing and the follow-through (Bourgain et al., Citation2022). During setup, the golfer establishes proper posture, balance and alignment, with the lumbar spine stationary in flexion. The backswing begins with the first movement of the clubhead away from the ball, moving the lumbar spine into rotation towards the trail side (Hume et al., Citation2005). The downswing is marked by a distal to proximal sequence generating movement of the clubhead towards the golf ball; the lumbar spine rapidly rotates through neutral into rotation towards the lead side and moves into lateral flexion towards the trail side (Cole & Grimshaw, Citation2016). This exposes the lumbar spine to significant compressive, rotational and shearing forces (Edwards et al., Citation2020). The follow-through spans impact through to completion of the golf swing, with the lumbar spine exposed to further force post-impact as the golfer decelerates (Edwards et al., Citation2020).
LBP accounts for approximately 25% of all injuries in golfers (Cole & Grimshaw, Citation2016; Gosheger et al., Citation2003; McCarroll et al., Citation1990; A. J. McHardy et al., Citation2007; M. F. Smith & Hillman, Citation2012), establishing it as the injury with the highest incidence amongst the 60–80 million golfers worldwide (The Royal and Ancient, Citation2015; Sports Marketing Surveys, Citation2021). The prevalence of LBP ranges from 12% to 27% in recreational golfers, rising to 40–58% in elite golfers (Batt, Citation1992; Burdorf et al., Citation1996; Gulgin & Armstrong, Citation2008; J. A. Smith et al., Citation2018). This equates to a potential global burden of LBP in golfers of up to 21.6 million people. Knowledge of the prevention and management of LBP would support a reduction in the burden of injury to which golf may contribute, and inform the rehabilitation of injured golfers.
Golf provides health enhancing physical activity, is associated with increased longevity, can have positive effects on stress and anxiety, and provides risk reduction for many common preventable conditions, amongst other reported health benefits (Belanger et al., Citation2013; Cabri et al., Citation2009; Ekeland et al., Citation2005; Gao et al., Citation2011; Murase et al., Citation1989; A. D. Murray et al., Citation2017; Palank & Hargreaves Jr, Citation1990; Parkkari et al., Citation2000; Quirk et al., Citation2020). Continued participation in golf is possible into later life, thereby providing benefits from physical activity through golf beyond the timeframe possible in many other sports (A. D. Murray et al., Citation2017). Improved understanding of the associations between LBP and golf may facilitate continued participation, maximising the health benefits golf provides.
Injury has further implications for professional athletes. Time spent side-lined by injury translates to lost income, underperformance and missed accolades. For those on the peripheries, injury may pose a threat to their status as a professional altogether. The availability of headline golfers is a major driver of revenue, interest and the success of individual tour events (Chung et al., Citation2013). Effective prevention of LBP would increase the availability of elite golfers for competition. This is central to the interests of the individual athlete, governing bodies and the golf industry as a whole.
Successful golf injury risk reduction strategies demand a thorough understanding of the risk factors associated with injury. Several explanations for the disproportionate prevalence of LBP in golfers have been proposed, including anthropometric risk factors (Burns et al., Citation2016; Evans et al., Citation2005; Vad et al., Citation2004), excessive repetition of the swing (McCarroll & Gioe, Citation1982; A. McHardy et al., Citation2007), failure to adequately warm-up (Fradkin et al., Citation2007; Gosheger et al., Citation2003) and biomechanics of the golf swing (Edwards et al., Citation2020; J. A. Smith et al., Citation2018). There is no consensus on which factors are most associated with an increased risk of LBP, nor consideration of which factors could be most readily modified.
In this review, we aimed to improve the understanding of biomechanical factors of the golf swing that are associated with LBP. This review will focus on human biomechanical parameters of the golf swing. Other kinetic variables describing the golf club during the swing will not be considered, as these are generated as a consequence of human biomechanics, and are therefore removed from the somatic movements potentially associated with increased risk of LBP by at least a degree. Swing biomechanics may be the modifiable risk with the greatest impact on LBP prevention, due to the significant lumbar compressive, rotational and shearing forces generated during the golf swing (Edwards et al., Citation2020). Identification of potentially modifiable risk factors, such as golf swing biomechanics, provides targets for prevention and rehabilitation of LBP in golfers.
2. Methods
A literature review was conducted according to the PRISMA statement for reporting systematic reviews. The checklist is shown in Online Supplementary Material 1 (Page et al., Citation2021).
2.1. Eligibility criteria
All primary research reporting analysis of the human biomechanics of the golf swing and the presence of LBP was included for further analysis. The term “lower-back” was not defined and synonyms such as lumbar, lower spine or sacral were accepted. Any method of pain reporting and quantification was accepted. All domains of biomechanical measurement were considered including kinetic, kinematic and electromyographical techniques. Only English language publications were included.
Any study that did not investigate pain and motion was excluded. Demographic characteristics of trial populations, including age, golfing ability, significant past medical history and concurrent morbidity, were not used as a basis for exclusion. No exclusions were made according to experimental methodology. No restrictions were placed on publication date or study design. No as-yet unpublished data were considered.
2.2. Information sources
Electronic databases searched were Medline (1966–present), Web of Science Core Collection (1970–present), Cochrane Central Register of Controlled Trials (1900–present), Scopus (1960–present) and Embase (1966–present). The search platforms selected were PubMed, Web of Science, Cochrane Library, Scopus and Embase, for each database, respectively. The literature search was completed on 6 February 2021 and updated on 7 April 2022 and on 6 June 2023, according to the guidance laid out by W. Bramer and Bain (Citation2017) and W. M. Bramer et al. (Citation2016). Reference lists of included studies were scanned for relevant studies.
2.3. Search strategy
After initial scoping searches and discussion between the authors, the following index terms were selected: golf* AND (back OR lumbar OR spine). The terms used were broad to maximise inclusivity. No adaptation of terms or format was required between search platforms.
2.4. Selection process
Following completion of the literature search, MW and SM independently conducted an eligibility assessment according to the pre-determined criteria by use of title and abstract screening, using the Rayyan reference screening software (Ouzzani et al., Citation2016). Disagreements were discussed, and in the event a consensus could not be reached the study proceeded to full-text analysis. Studies selected for full-text analysis were sourced. Where full-text versions could not be sourced, studies were excluded. All included studies were analysed by both MW and SM.
2.5. Data collection process
Nine papers meeting the criteria were analysed independently by MW and SM. Prior to data collection, a results table was devised to support systematic analysis of all relevant information. This table is provided in Online Supplementary Material 2. Results were compared between the two authors, and a consensus was met on any point of disagreement.
2.6. Data items
Information extracted from each of the selected studies comprised: demographic characteristics of the study population, including handedness and golfing ability; definition of pain required for inclusion in the LBP group; type of biomechanical technique and the outcomes measured; testing protocol; all relevant biomechanical outcome measures that were compared between LBP and control groups; and the limitations of each study. After beginning the extraction process, this was refined to include anatomical landmarks used in gathering kinematic and EMG data, due to observed variation in procedure between studies. Study design was determined using the National Institute for Health and Care Excellence (NICE) algorithm for classification of quantitative study designs (National Institute for Health and Care Excellence, Citation2012).
2.6.1. Elite and sub-elite golfers
The recently published International Consensus Statement by the International Golf Federation (IGF) (A. Murray et al., Citation2020) defines elite golfers as “professional players competing on tour or amateurs competing in international/national amateur championships”. The same publication defines sub-elite golfers as “PGA teaching professionals, amateurs competing in regional/county/state tournaments or with handicap ≤ 5”, and recreational golfers as those with a handicap greater than five. It is possible that these cohorts may be exposed to distinct risk factors from one another. Therefore, we compared potential differences in the biomechanical associations with LBP in recreational and elite and sub-elite golfers by grouping studies according to golfing ability.
2.7. Study risk of bias assessment
Risk of bias was assessed independently by MW and SM using the ROBINS-I tool for cohort-type studies (Sterne et al., Citation2016). This tool was selected following full-text screening, due to the inclusion of only prospective cohort and retrospective case-control studies in the review. ROBINS-I provides a structured assessment of the risk of bias in a single study across multiple domains, and gives a framework to determine the overall risk of bias. MW and SM assessed each of the nine studies included across these individual domains, and used the results of this assessment to assign an overall risk of bias to each study.
2.8. Effect measures
We calculated the standardised mean difference (SMD) Cohen’s D for each relevant outcome measure. As there are no alternative suggested thresholds for classification of Cohen’s D in relation to back pain impacting on the biomechanics of the golf swing, we utilised the general thresholds originally suggested (Cohen, Citation1988). Specifically, no effect (SMD ≤ 0.2), small effect (SMD 0.2–0.5), moderate effect (SMD 0.5–0.8) and large effect (SMD > 0.8) were used for descriptive purposes.
2.9. Synthesis methods
Prior to data extraction, we had planned to undertake a meta-analysis. However, due to the heterogeneity of the methodologies employed, outcome measures reported and participants included, it was not appropriate to pool findings from across studies in a meta-analysis. Alternatively, we have presented the main findings from the individual studies in an evidence gap map (White et al., Citation2020). This summarises the findings and allows us to demonstrate the level of evidence across the different outcome measures and methodologies.
2.10. Certainty assessment
The level of evidence provided by the studies was independently assessed by MW and SM, using the five criteria specified by GRADE (study limitations, consistency of effect, imprecision, indirectness and publication bias) (Guyatt et al., Citation2008). Level of evidence was then qualified according to the following definitions: strong evidence (multiple studies with a low risk of bias reporting homogenous outcomes); moderate evidence (multiple studies reporting homogenous outcomes, at least one of which has a low risk of bias); limited evidence (a single study with a low risk of bias, or multiple studies with a moderate risk of bias reporting homogenous outcomes); very limited evidence (a single study with a moderate risk of bias); and conflicting evidence (heterogenous outcomes reported between studies) (van Tulder et al., Citation2003).
3. Results
3.1. Study selection
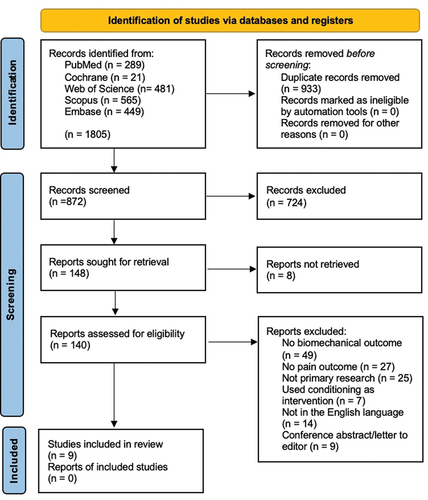
The initial search identified a total of 1805 studies (). Following the exclusion of duplicates, 872 studies progressed to manual screening by title and abstract. A total of 724 of these did not meet the criteria for inclusion.
In total, 140 papers were selected for full-text eligibility assessment. Nine were identified as satisfying the inclusion and exclusion criteria of this review. There were two occasions on which studies by the same group of researchers published within the same year were included in the review. They are referred to as (a) Cole and Grimshaw (Citation2008b) and Cole and Grimshaw (Citation2008a) and Quinn, Olivier, McKinon and Dafkin (Citation2022) and (b) Quinn, Olivier and McKinon (Citation2022) hereafter.
3.2. Study characteristics
Seven of the nine studies included in the review were case-control, comparing groups with pain to groups without, and dually reported pain and quantifiable biomechanical swing parameters as primary outcomes (Cole & Grimshaw, Citation2008a, Citation2008b, Citation2014; Horton et al., Citation2001; Lindsay & Horton, Citation2007; Sim et al., Citation2017; Tsai et al., Citation2010). The remaining two studies were prospective cohort studies, comparing baseline biomechanical swing parameters between golfers with and without LBP after a six-month follow-up period (Quinn, Olivier, & McKinon, Citation2022; Quinn, Olivier, McKinon, & Dafkin, Citation2022). Primary outcomes reported varied between studies ().
Table 1. Summary of study characteristics.
The number of swings and the methods by which swings were selected for analysis varied between studies. Only one study selected swings to be included for analysis using pre-determined quantitative criteria (Tsai et al., Citation2010), two included all trials performed (Quinn, Olivier, & McKinon, Citation2022; Quinn, Olivier, McKinon, & Dafkin, Citation2022) and the rest utilised qualitative feedback such as quality of strike or straightness of ball flight to determine trials for inclusion. One study declared they had used a power calculation for their sample size (Tsai et al., Citation2010), but did not state their primary outcome or null hypothesis. With multiple variables being assessed within each study, there is a high risk of false positives. Two of the studies addressed this concern through lowering the level of significance required (Cole & Grimshaw, Citation2008a, Citation2014), whilst another performed a Bonferroni correction (Tsai et al., Citation2010).
The authors used varying techniques to record and assess pain. Two studies recruited control participants only if they had never previously reported LBP (Lindsay & Horton, Citation2007; Tsai et al., Citation2010), three required control participants be free of LBP for the preceding 12 months (Cole & Grimshaw, Citation2008a, Citation2008b, Citation2014), and another for 6 months (Horton et al., Citation2001). A single study described control participants as “healthy”, without providing any further information (Sim et al., Citation2017). The two studies of prospective design required only that participants be free of LBP at the time of baseline assessment (Quinn, Olivier, & McKinon, Citation2022; Quinn, Olivier, McKinon, & Dafkin, Citation2022). This led to the inclusion of 12 participants who reported LBP in the preceding 6 months, with five golfers missing training or competition due to their pain, and 10 golfers who reported pain in the month before baseline assessment. Three studies used the Short-Form McGill Pain Questionnaire to quantify pain severity (Cole & Grimshaw, Citation2008a, Citation2008b, Citation2014), and another used the Oswestry Disability Questionnaire (Tsai et al., Citation2010). The remaining studies did not measure LBP severity, but reported its presence or absence (Horton et al., Citation2001; Lindsay & Horton, Citation2007; Quinn, Olivier, & McKinon, Citation2022; Quinn, Olivier, McKinon, & Dafkin, Citation2022; Sim et al., Citation2017). The duration of LBP was not reported by five studies (Cole & Grimshaw, Citation2008a, Citation2008b, Citation2014; Sim et al., Citation2017; Tsai et al., Citation2010). A single study defined the LBP group as those who experienced LBP associated with golf for at least 6 months prior to assessment (Horton et al., Citation2001), and another selected participants who “always” reported LBP associated with golf (Lindsay & Horton, Citation2007). The mean duration of LBP reported by participants in the prospective studies was 2–3weeks (Quinn, Olivier, & McKinon, Citation2022; Quinn, Olivier, McKinon, & Dafkin, Citation2022). The authors did not report whether pain was felt acutely whilst playing golf or on a chronic basis associated with golf participation.
It appears on two occasions that two studies were performed on the same cohort of participants, but the authors either did not specify whether this was the case or provide complete demographic details within the article (Cole & Grimshaw, Citation2008b, Citation2014; Quinn, Olivier, & McKinon, Citation2022; Quinn, Olivier, McKinon, & Dafkin, Citation2022). Studies exclusively analysed the swings of male golfers. Five studies included only right-handed golfers, two studies included two left-handed golfers, appearing to be the same individuals (Quinn, Olivier, & McKinon, Citation2022; Quinn, Olivier, McKinon, & Dafkin, Citation2022), and the remaining two not did not specify dexterity (Horton et al., Citation2001; Lindsay & Horton, Citation2007). Four studies recruited elite or sub-elite golfers (Horton et al., Citation2001; Lindsay & Horton, Citation2007; Quinn, Olivier, & McKinon, Citation2022; Quinn, Olivier, McKinon, & Dafkin, Citation2022), four recruited recreational golfers (Cole & Grimshaw, Citation2008a, Citation2008b, Citation2014; Tsai et al., Citation2010), and one recruited both (Sim et al., Citation2017). Demographic characteristics were comparable throughout. A summary is given in .
Table 2. Demographic characteristics (mean ± sd) of participants included in each study.
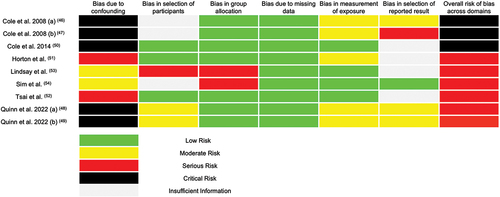
3.3. Risk of bias in studies
Risk of bias varied between studies (). The authors provided the data outlined in the methodology, regardless of result, with no overt missing data. Use of objective quantitative outcomes largely protected against bias during collection of data. In the majority of cases, groups were determined according to rigid pre-determined definitions that protected the research from allocation bias, but in two studies the cohort parameters were sufficiently vague to introduce a serious risk of bias during group allocation (Lindsay & Horton, Citation2007; Sim et al., Citation2017).
There were numerous methodological practices that introduced potential for bias. Three studies outlined recruitment protocols in sufficient detail to adequately confirm the validity of their respective cohorts (Cole & Grimshaw, Citation2008a, Citation2008b; Sim et al., Citation2017). The other six either provided insufficient information to facilitate accurate assessment of the bias encountered or employed techniques that risked introducing selection bias (Cole & Grimshaw, Citation2014; Horton et al., Citation2001; Lindsay & Horton, Citation2007; Tsai et al., Citation2010). There was a trend of moderate risk of bias during reporting of results, chiefly caused by a lack of pre-registered research protocols. Adherence to the outlined methodology was maintained, but there were cases where deviation could not be excluded. No study assessed for the potential presence of confounding variables, and in two prospective studies the presence of recent LBP was not a criterion for exclusion, leading to a potentially serious risk of bias (Quinn, Olivier, & McKinon, Citation2022; Quinn, Olivier, McKinon, & Dafkin, Citation2022).
The overall risk of bias for each paper included in the review was deemed to be at a minimum serious, and in some cases critical, according to the definitions provided by the ROBINS-I tool ().
3.4. Results of individual studies
A total of 73 outcomes were reported across the nine studies, with 61 being reported by only a single study. Of these, 10 outcomes were reported by two studies, and two outcomes were reported by three studies.
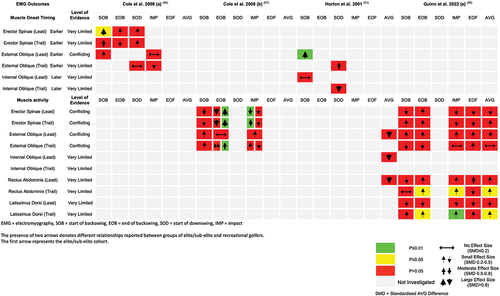
3.4.1. Kinematics
Of the nine studies analysed, five utilised kinematic analysis () (Cole & Grimshaw, Citation2014; Lindsay & Horton, Citation2007; Quinn, Olivier, & McKinon, Citation2022; Sim et al., Citation2017; Tsai et al., Citation2010). The techniques used by the authors were homogenous; all gathered data using 3D kinematics, with Lindsay et al. combining 3D kinematics and accelerometery (Lindsay & Horton, Citation2007). Three studies investigated somatic positioning and movement velocity of the lumbar spine, hip and trunk (Cole & Grimshaw, Citation2014; Lindsay & Horton, Citation2007; Tsai et al., Citation2010), with a further study additionally reporting positioning of the lower limbs, upper thorax and X-factor (Quinn, Olivier, & McKinon, Citation2022). X-factor is defined as the difference in shoulder and pelvic rotation at the point of transition between the backswing and downswing (McLean, Citation1992). The slight increase in shoulder to pelvic separation immediately after initiation of the downswing is known as X-factor stretch (CitationHow to Fix Golf Back Pain). A single study reported the length of the transition phase (Sim et al., Citation2017). It was rare for two studies to report the same kinematic measure. The majority of reported outcomes were not significantly different between the LBP and control group. Heterogeneity in the outcomes reported means those variables reported as being associated with LBP were not corroborated by other studies. The kinematic outcomes reported are displayed in the gap map in . It should be noted that (b) utilised two effect measures with different scales for effect size according to whether or not data was normally distributed, but did not state which variables were normally distributed (Quinn, Olivier, & McKinon, Citation2022). We therefore categorised these according to the general effect sizes (Cohen, Citation1988).
Figure 3. An evidence gap map summarising findings from the studies to use kinematic techniques. Some outcomes were condensed down to the specific plane of movement to allow for optimal visualisation in the manuscript. For a complete breakdown, please see Supplementary Material 3.

Lindsay and Horton (Citation2007) reported no significant difference in peak lumbar flexion, extension or rotation between elite golfers with and without LBP. Similarly, no baseline differences were found in lumbar flexion or extension in a prospective study of elite golfers (Quinn, Olivier, & McKinon, Citation2022). Peak lead-side lumbar lateral flexion was greater in elite golfers with LBP (Lindsay & Horton, Citation2007), a finding supported at the start of the backswing by a prospective study of elite golfers (Quinn, Olivier, & McKinon, Citation2022), although not in recreational golfers (Cole & Grimshaw, Citation2014). No significant differences were reported in the hip angle, trunk angle and crunch factor (Cole & Grimshaw, Citation2014) or the trunk extension (Tsai et al., Citation2010) of recreational golfers with and without LBP. Elite golfers who developed LBP displayed statistically significant baseline differences to peers who did not develop LBP. Golfers who developed LBP displayed: greater upper thoracic lateral flexion; greater lead knee abduction; reduced lead knee flexion; reduced lead ankle dorsiflexion; greater trail hip abduction; reduced lead knee adduction; increased lead ankle adduction; increased trail knee flexion; increased trail hip adduction; and reduced lead ankle eversion (Quinn, Olivier, & McKinon, Citation2022). Only two of these findings, reduced lead knee flexion and reduced lead ankle dorsiflexion, were replicated at more than one point of the swing.
Sim et al. (Citation2017) quantified the transition phase according to lead hand speed, X-factor stretch and relative instantaneous angles of the pelvis and thorax. When defined by relative angle and X-factor stretch, elite golfers with LBP displayed significantly shorter transition phases than their uninjured peers. No significant difference was reported when the transition phase was defined by lead hand speed.
Lindsay and Horton (Citation2007) reported no significant difference in lumbar extension velocity or lumbar rotational velocity between elite golfers with LBP and their uninjured peers. The latter finding was corroborated amongst recreational golfers by Tsai et al. (Citation2010). Elite golfers without LBP demonstrated greater peak lumbar flexion velocity, and those with LBP greater peak lateral flexion velocity (Lindsay & Horton, Citation2007). Cole and Grimshaw (Citation2014) were the only researchers to investigate the velocity of trunk motion, and reported no significant differences.
3.4.2. Electromyography
Four studies used electromyography (EMG) as a biomechanical measure (Cole & Grimshaw, Citation2008a, Citation2008b; Horton et al., Citation2001; Quinn, Olivier, McKinon, & Dafkin, Citation2022). The most commonly selected muscles were the major muscles of the lower back and abdomen. External oblique (EO) was analysed by all four studies, and erector spinae (ES) by three (Cole & Grimshaw, Citation2008b; Horton et al., Citation2001; Quinn, Olivier, McKinon, & Dafkin, Citation2022). Rectus abdominis (RA) was analysed by two studies (Horton et al., Citation2001; Quinn, Olivier, McKinon, & Dafkin, Citation2022), and internal oblique (IO) and latissimus dorsi (LD) by a single study (Horton et al., Citation2001). Researchers investigated either the timing of contraction onset relative to various phases of the swing, the relative activity of muscles at certain moments throughout the swing, or both. A summary of the findings is given in .
There was no significant difference in ES activity at the start of the backswing in recreational golfers with and without LBP (Cole & Grimshaw, Citation2008a). Recreational golfers with lower handicaps and LBP display greater activity of ES at the end of the backswing than peers without LBP (Cole & Grimshaw, Citation2008a). The converse relationship was demonstrated amongst a cohort of higher handicap recreational golfers; those with LBP generated greater ES activity at the end of the backswing than those without LBP (Cole & Grimshaw, Citation2008a). No differences in ES activity at impact were displayed in higher handicap recreational golfers, but lower handicap recreational golfers with LBP demonstrated reduced ES activity compared to uninjured counterparts (Cole & Grimshaw, Citation2008a). Earlier activation of lumbar ES at the start of the backswing was reported in recreational golfers with LBP, but no differences in onset timing were reported at the end of the backswing or start of the downswing (Cole & Grimshaw, Citation2008b). In a prospective study of elite golfers, no baseline statistically significant differences were found in ES activity throughout the swing (Quinn, Olivier, McKinon, & Dafkin, Citation2022).
Recreational golfers with LBP display no differences in EO activity compared to uninjured peers at the start of the backswing or at impact, but have greater EO activity at the end of the backswing (Cole & Grimshaw, Citation2008a). The average amplitude of EO activation throughout the swing was not significantly different between elite golfers with and without LBP (Horton et al., Citation2001), findings corroborated by a prospective study which found no baseline differences in EO activity between elite golfers who did and did not develop LBP at any point in the swing (Quinn, Olivier, McKinon, & Dafkin, Citation2022). Elite golfers with LBP display later onset of EO contraction at the start of the backswing (Horton et al., Citation2001), but this was not replicated amongst recreational golfers (Cole & Grimshaw, Citation2008b). Neither cohort displayed a significant difference in EO onset at the start of the downswing (Cole & Grimshaw, Citation2008b; Horton et al., Citation2001). There was no difference in EO onset at impact in groups of recreational golfers with and without LBP (Cole & Grimshaw, Citation2008b).
Elite golfers who developed LBP showed increased baseline activity of trail-side RA and LD at the end of the backswing, at impact, and the mean activity of both muscles was greater throughout the swing (Quinn, Olivier, McKinon, & Dafkin, Citation2022). No differences were reported in lead-side RA and LD activity (Quinn, Olivier, McKinon, & Dafkin, Citation2022) The mean amplitude of activity of RA and IO throughout the swing was not significantly different in elite golfers with and without LBP (Horton et al., Citation2001). Timing of IO contraction at the start of the backswing and start of the downswing amongst elite golfers with LBP was not significantly different to their uninjured peers (Horton et al., Citation2001).
3.4.3. Torsion
Two of the seven studies investigated the effect of lumbar torsion during the golf swing on LBP () (Sim et al., Citation2017; Tsai et al., Citation2010). The authors of both studies estimated torsion utilising ground reaction force plates, on which the participant stood during testing.
Figure 5. An evidence gap map summarising findings of studies to measure outcomes relating to lumbar torsion.
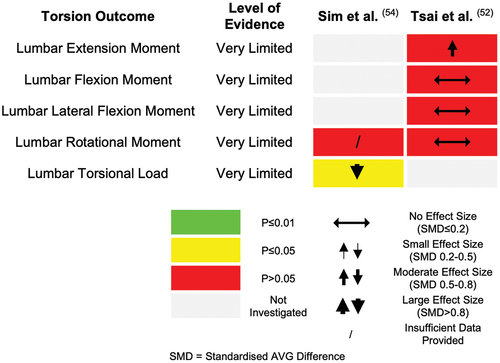
Tsai et al. (Citation2010) reported no significant differences in the lumbar torsion generated by injured or uninjured recreational golfers across all six recorded time points during the swing, from initiation of the backswing to impact. Sim et al. (Citation2017) sought to investigate different methodologies for quantification of the transition phase and tested three distinct sets of biomechanical parameters by which it could be defined. Regardless of the method utilised, uninjured elite golfers generated significantly greater torsion than their injured counterparts during the transition phase of the golf swing. They did not report a significant difference in the torsional load generated during the transition phase by recreational golfers with and without LBP, although amateur golfers produced less torsional load than the elite golfers.
3.4.4. Elite and sub-elite golfers vs recreational golfers
Only one study recruited both elite and recreational golfers (Sim et al., Citation2017). Elite golfers, with and without LBP, displayed longer transition phases and generated greater lumbar torsion during the transition phase than recreational counterparts.
A total of eight outcomes were reported by more than one study, where one study recruited elite or sub-elite golfers and the other recruited recreational golfers. Lindsay et al. (Lindsay & Horton, Citation2007) reported that elite and sub-elite golfers with LBP displayed greater peak lumbar lateral flexion and greater lumbar lateral flexion velocity than their uninjured peers, and Quinn et al. (Quinn, Olivier, & McKinon, Citation2022) found that that elite golfers who would develop LBP showed greater lumbar lateral flexion at the start of the backswing. In contrast, Cole and Grimshaw (Citation2014) reported no such differences in recreational golfers. Horton et al. (Horton et al., Citation2001) found no significant differences in mean EO activity in elite golfers with and without LBP. In contrast, recreational golfers with LBP showed greater EO activity at the end of the backswing than their uninjured counterparts (Cole & Grimshaw, Citation2008a). Cole and Grimshaw (Citation2008a) reported greater bilateral erector spinae activity at the end of the backswing and reduced bilateral ES activity at impact in recreational golfers with LBP. Additionally, they reported increased trail-side external oblique activity at the end of the backswing in the injured cohort. None of these findings were replicated in the baseline swing characteristics of elite golfers who would go on to develop LBP (Quinn, Olivier, McKinon, & Dafkin, Citation2022). Horton et al. (Citation2001) reported that elite golfers with LBP exhibited earlier initiation of EO contraction, in relation to the start of the backswing. This was not corroborated in recreational golfers, where no significant differences in EO onset were reported (Sim et al., Citation2017). Neither elite nor recreational golfers with LBP demonstrated significant differences in the activity of trail-side EO compared to their uninjured peers (Cole & Grimshaw, Citation2008a; Quinn, Olivier, McKinon, & Dafkin, Citation2022).
Both Tsai et al. (Citation2010) and Lindsay and Horton (Citation2007) reported no significant difference in peak lumbar spine rotational velocity between golfers with and without LBP, in a group of recreational and a mixed cohort of elite and sub-elite golfers, respectively. This was the only instance in which studies recruiting differing abilities of golfers reported a common finding. However, the lack of agreement across studies investigating different levels of golfing ability is potentially inflated due to the low number of studies incorporating comparable outcome measures.
3.5. Certainty of evidence
A total of 73 outcomes were reported by the studies analysed. Forty-nine of these did not demonstrate statistically significant differences between those with and without LBP. The evidence collected pertaining to these outcomes was subject to a severe risk of bias, and a lack of methodological and outcome homogeneity between studies. Therefore, the quality of evidence was assessed as being very limited.
Twenty-four of the 73 outcomes reported achieved the level of statistical significance. The level of evidence was of very limited quality, relating to 19 of these outcomes. This assessment was based on a severe risk of bias and each outcome being reported by only a single study. The remaining five significant outcomes were demonstrated by a conflicting level of evidence due to heterogeneity of results between studies. Quality of evidence assessments relating to the outcomes to achieve statistical significance are summarised in .
Table 3. Certainty of evidence supporting outcomes reported as statistically significant.
4. Discussion
In this review, we aimed to investigate all primary research reporting biomechanical analysis of the golf swing and the presence of LBP, in order to assess the evidence behind the hypothesis that biomechanics of the golf swing is associated with LBP. Several potential golf swing biomechanical associations with LBP were reported. The overall quality of evidence was very limited to conflicting, with a serious risk of bias due to confounding and participant selection in the included studies, as well as there being a limited number of studies. This research area would benefit from well-conducted prospective research, as the belief that biomechanical factors in the golf swing can contribute to LBP is widely held (Foley, Citation2021; Freedman, Citation2018; How to Fix Golf Back Pain Citation2021; James, Citation2019; Kamson, Citation2020; Roberts, Citation2019; Rose, Citation2014; Schuler, Citation2020), despite very limited primary research to support this.
To the authors’ knowledge, this is the first systematic review of golf swing biomechanical factors associated with LBP. Previous reviews have taken a narrative approach, describing the biomechanical patterns integral to the golf swing, the torsional loads experienced throughout the golf swing, possible mechanisms of injury and the epidemiology of injury in golf. These publications provide potential hypotheses for the disproportionate incidence of LBP in golfers, but do not critically analyse the evidence base.
Establishing risk factors for injury is an important step in decreasing injury risk. Potential risk factors have been identified in this review, and although they could be considered to guide primary and secondary prevention of LBP, caution should be taken until further evidence is developed. Importantly, golf swings are not homogenous, and players may have multiple contributory biomechanical factors.
4.1. Potential risk factors
Increased torsional load during the transition phase of a swing results in exaction of greater forces on the lumbar spine (Sim et al., Citation2017; Tsai et al., Citation2010). This may predispose structural changes, providing a potential mechanism of injury explaining the association between increased lumbar torsion and LBP. Similarly, a shorter transition phase means that these forces are acting over a shorter period, exposing the golfer to greater energy through lumbar spinal structures at a faster rate. When the repetitive nature of the golf swing throughout training/competition is considered, this increased stress may lead to pain. Alternatively, the shorter duration of the golf swing may be a result of LBP occurrence, reducing the time in the fully rotated position, but requiring a greater torsional load to be developed quicker in order to perform a successful swing. These hypotheses should be assessed in prospective research, through continuous monitoring of the golf swing in golfers.
Unilateral contraction of ES and EO causes ipsilateral lumbar lateral flexion (Rab et al., Citation1977). This mechanism of action and the positive association between magnitude of ES and EO contraction and LBP lend further support to the association between lumbar lateral flexion magnitude and velocity and LBP that was also reported, albeit with a conflicting level of evidence. Future research should report sidedness of muscle activation and the direction of lumbar lateral flexion to provide further insight into the potential relationship between these two factors.
Bilateral contraction of EO leads to lumbar flexion (Rab et al., Citation1977). It has been reported that there is a positive association between the magnitude of EO activity and LBP, but a negative association with lumbar flexion velocity and LBP. These contradictory findings indicate that increased EO activity may be unlikely to cause back pain via lumbar flexion, and an alternative explanation for the mechanism of injury should be sought. Focusing on single muscles when assessing activation profiles during the golf swing prevents us from understanding the full activation profile, as activation of other muscles may be altered to accommodate/affect differences observed in EO.
Overall, golfers with LBP tended to demonstrate a shorter duration of golf swing. This was seen through an increased velocity of torso rotation alongside some suggestion that increased activation of ES and EO at the end of the backswing, especially in non-elite golfers. The potential discrepancy between elite and non-elite golfers in variables associated with LBP suggests that any association between biomechanics of the golf swing and LBP is not only complex, but also potentially dependent on the golfer’s ability.
There is a lack of research into the mechanical load the lumbar spine is exposed to during the golf swing. Elite golfers have been reported to generate a peak lumbar load of approximately six times participant bodyweight (Lim et al., Citation2012), and a maximum load of 10 N/Kg during the transition phase (Sim et al., Citation2017). The same authors report that recreational golfers generate approximately 1.7N/Kg of load during the transition phase, significantly less than their elite counterparts (Sim et al., Citation2017). Isolated exposure to loads of this scale is unlikely to cause injury to normal anatomy, but repeated exposure could lead to damage of lumbar structures and subsequent LBP. Future research on the loads applied to the lumbar spine in the golf swing, ideally utilising modelling techniques to estimate the load applied at the tissue level, should be conducted to improve the understanding of the mechanisms by which LBP develops.
Biomechanics of the golf swing are not the only potential risk factor for LBP in golfers, and it would be optimal for future research to account for these. There are many other factors that have been suggested to be important for injuries in recreational (Cabri et al., Citation2009) and elite (Robinson et al., Citation2019) golfers. These include the volume of practice and competition, the surface balls are being hit from (for example, it is suggested wrist injuries may increase if balls are being hit from mats or firm ground instead of turf (Hawkes et al., Citation2013) and when modifications are made to the swing or equipment used. Psychosocial factors and their impact on musculoskeletal injury risk and rehabilitation, including LBP, are recognised in both athletes (Ardern et al., Citation2013; McCall et al., Citation2015) and the general population (Knezevic et al., Citation2021; Nicholas et al., Citation2011; Pincus et al., Citation2002; Vlaeyen et al., Citation2018). Golf-specific research on the impact of psychosocial factors is lacking and may aid the holistic understanding of injury risk in golfers. Other sports, including tennis and cycling, describe biomechanical factors as well as the volume and intensity of play to be potential contributors to injury. LBP is reported to be prevalent in elite athletes from other sports, including cross-country skiing, rowing and dancing (Farahbakhsh et al., Citation2018; Fett et al., Citation2017; Trompeter et al., Citation2017). Therefore, the prevalence of LBP in golf may be associated with prevalence of LBP in athletes in general, and may not be specific to mechanics of the golf swing itself.
4.2. Limitations
The greatest limitations of the research were inconsistency in the recording and reporting of biomechanical factors and pain, and the paucity of prospective studies. The eligible studies for this review were majority retrospective case-control studies, limiting the ability to determine whether the associations identified are causative of or resultant from LBP. Participants’ LBP may have been caused by golf or, noting the prevalence of LBP in the general population (Hoy et al., Citation2012), may have been due to other factors. The minority of studies that were of prospective design did not exclude participants who had experienced LBP that impaired their participation in golf in the month prior to baseline assessment, introducing severe risk of confounding bias and undermining the prospective study design (Quinn, Olivier, & McKinon, Citation2022; Quinn, Olivier, McKinon, & Dafkin, Citation2022).
The overall quality of study design was low. The number of swings included in the analysis was minimal, the greatest being only 10 swings per golfer, and the processes by which they were selected were inconsistent. By excluding a majority of the recorded swings, the researchers created an idealistic situation in which a golfer does not make a “bad” swing, a circumstance unrepresentative of golf, and in particular recreational golf. It is important to take into account the variability of the individual golfer’s swing, across multiple days, in future research, instead of relying on an average across a low number of swings within a single session. Researchers should pre-determine quantifiable criteria by which to identify representative swings to select for analysis, and seek to analyse a greater number of trials per participant. The reporting of pain was heterogenous and often qualitative. Future research should employ objective quantitative techniques that specify pain site, onset, character, duration and severity to more comprehensively report LBP and facilitate meaningful comparison.
A serious risk of bias due to poor statistical design and analysis was present across the included studies. The absence of a primary outcome to which they were powered may have led to type II errors. One study declared a power calculation, but it is not clear what this was powered to, and they did not state a primary outcome (Sterne et al., Citation2016). Therefore, it is not clear if those biomechanical factors in the golf swing not associated with LBP were truly not associated or whether the studies were insufficiently powered to demonstrate a difference between cohorts. To support future development of this, a consensus is needed as to what effect size would be clinically meaningful for the respective outcome. Furthermore, only four out of the nine studies accounted for the multiple statistical tests performed, and the positive associations identified may represent type I errors (Cole & Grimshaw, Citation2008a, Citation2008b, Citation2014; Tsai et al., Citation2010). With the large number of discrete variables that are able to be extracted from a movement like a golf swing, it is imperative that selection is not based on significance, but on prior hypotheses, ideally presented in pre-registered protocols (Pataky et al., Citation2016). A more ideal approach would be to analyse the golf swing as a continuous time-domain action, incorporating appropriate analyses (i.e., statistical parametric mapping or functional data analysis) (Warmenhoven et al., Citation2018).
The cohorts recruited were generally small, participants were universally male and, with the exception of two participants, right-handed. These demographics are unrepresentative of the global golfing population. This further limits the ability to reliably generalise the findings of this review to the majority of golfers.
The numerous biomechanical variables in the golf swing and the lack of knowledge regarding their impact on LBP make adequate control of confounding variables difficult to achieve. A greater body of research is required to achieve sufficient control for possible confounders, along with the consistent application of such protocols across future research.
There was variation in the specific outcomes measured and experimental technique. The authors employed terms inconsistently, with the phrases “top of the backswing” and “start of the downswing” used interchangeably across the literature. These terms are distinct from one another, and should not be confused as synonymic. The categorisation of golfers according to ability varied. The IGF International Consensus Statement definitions of elite, sub-elite and recreational golfers align closely with observed skill levels at which changed biomechanical swing traits are seen (Zheng et al., Citation2008). It is therefore likely that these distinct cohorts are exposed to different biomechanical risk factors for LBP, and future research should recruit and distinguish participants according to the IGF categories. This heterogeneity within the existing literature renders meaningful comparison between papers challenging.
Researchers used highly specialist equipment that is unavailable to the independent golfer. Outcomes were complex, requiring a degree of scientific expertise to interpret. Positive associations related to parameters that are unintuitive and challenging to consciously modify. These factors limit the usefulness of any positive findings to the golfer or sports medicine practitioner seeking to prevent LBP. Once biomechanical risk factors have been investigated with more certainty, development of novel approaches to monitoring these more cost-effectively and requiring less skill is needed.
4.3. Conclusion and implications
There was no conclusive evidence to support the hypothesis that LBP is associated with biomechanics of the golf swing. The overall quality of evidence was limited, with a serious risk of bias. The associations reported in this review should be further investigated by prospective studies incorporating sound experimental and statistical approaches, before attempts to replicate findings in the playing arena are made. Once firm associations have been established, it is then important for future research to consider how this knowledge can be best integrated into injury prevention and rehabilitation. Future research should recruit participants of both sexes and handedness, across all levels.
4.4. Registration and protocol
The review protocol was not pre-registered.
4.5. Support
The authors received no funding or external support at any stage of the review process.
4.6. Competing interests
SM and NDC have no conflicts of interest. DC and AM receive remuneration in clinical, research and development roles for the European Tour Group/DP World Tour. MW has an unpaid role at the European Tour Group. IRM is a consultant for Stryker.
4.7. Availability of data, code and other materials
A summary of the table used to supplement data extraction from individual studies is included in Online Supplementary Material 2.
4.8. Geolocation statement
This review was conducted solely in the cities of Edinburgh and London, United Kingdom.
Author’s contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Dr Matthew Watson and Dr Stuart Miller. The first draft of the manuscript was written by Dr Matthew Watson and all authors commented on the initial and all subsequent versions of the manuscript. All authors read and approved the final manuscript.
Electronic Supplementary Material 3.pdf
Download PDF (562.7 KB)Electronic Supplementary Material 1.pdf
Download PDF (468.2 KB)Electronic Supplementary Material 2.pdf
Download PDF (252.6 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online https://doi.org/10.1080/02640414.2024.2319443.
Additional information
Funding
References
- Ardern, C. L., Taylor, N. F., Feller, J. A., & Webster, K. E. (2013). A systematic review of the psychological factors associated with returning to sport following injury. British Journal of Sports Medicine, 47(17), 1120–6. https://doi.org/10.1136/bjsports-2012-091203
- Batt, M. E. (1992). A survey of golf injuries in amateur golfers. British Journal of Sports Medicine, 26(1), 63–65. https://doi.org/10.1136/bjsm.26.1.63
- Belanger, L. J., Plotnikoff, R. C., Clark, A. M., & Courneya, K. S. (2013). Prevalence, correlates, and psychosocial outcomes of sport participation in young adult cancer survivors. Psychology of Sport and Exercise, 14(2), 298–304. https://doi.org/10.1016/j.psychsport.2012.10.010
- Bourgain, M., Rouch, P., Rouillon, O., Thoreux, P., & Sauret, C. (2022). Golf swing biomechanics: A systematic review and methodological recommendations for kinematics. Sports, 10(6), 91. https://doi.org/10.3390/sports10060091
- Bramer, W., & Bain, P. (2017). Updating search strategies for systematic reviews using endnote. Journal of the Medical Library Association, 105(3), 285–9. https://doi.org/10.5195/jmla.2017.183
- Bramer, W. M., Giustini, D., de Jonge GB, Holland, L., Bekhuis, T., & de Jonge, G. B. (2016). De-duplication of database search results for systematic reviews in endnote. Journal of the Medical Library Association: JMLA, 104(3), 240–243. https://doi.org/10.3163/1536-5050.104.3.014
- Burdorf, A., Van Der Steenhoven, G. A., & Tromp-Klaren, E. G. M. (1996). A one-year prospective study on back pain among novice golfers. The American Journal of Sports Medicine, 24(5), 659–664. https://doi.org/10.1177/036354659602400516
- Burns, K., Pierson, M., Becker, J., Wu, W., & Nakajima, M. (2016). Relationship between hip strength, range of motion, and Low Back Pain in collegiate women’s golfers. Medicine and Science in Sports and Exercise, 48(5), 586–587. https://doi.org/10.1249/01.mss.0000486760.73376.5e
- Cabri, J., Sousa, J. P., Kots, M., & Barreiros, J. (2009). Golf-related injuries: A systematic review. European Journal of Sport Science, 9(6), 353–66. https://doi.org/10.1080/17461390903009141
- Chung, K. Y. C., Derdenger, T. P., & Srinivasan, K. (2013). Economic value of celebrity endorsements: Tiger Woods’ impact on sales of Nike golf balls. Marketing Science, 32(2), 271–93. https://doi.org/10.1287/mksc.1120.0760
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Elsevier.
- Cole, M. H., & Grimshaw, P. N. (2008a). Electromyography of the trunk and abdominal muscles in golfers with and without Low Back Pain. Journal of Science & Medicine in Sport / Sports Medicine Australia, 11(2), 174–81. https://doi.org/10.1016/j.jsams.2007.02.006
- Cole, M. H., & Grimshaw, P. N. (2008b). Trunk muscle onset and cessation in golfers with and without Low Back Pain. Journal of Biomechanics, 41(13), 2829–33. https://doi.org/10.1016/j.jbiomech.2008.07.004
- Cole, M. H., & Grimshaw, P. N. (2014). The crunch factor’s role in golf-related Low Back Pain. The Spine Journal, 14(5), 799–807. https://doi.org/10.1016/j.spinee.2013.09.019
- Cole, M. H., & Grimshaw, P. N. (2016). The biomechanics of the modern golf swing: Implications for lower back injuries. Sports Medicine, 46(3), 339–51. https://doi.org/10.1007/s40279-015-0429-1
- Edwards, N., Dickin, C., & Wang, H. (2020). Low Back Pain and golf: A review of biomechanical risk factors. Sports Medicine and Health Science, 2(1), 10–8. https://doi.org/10.1016/j.smhs.2020.03.002
- Ekeland, E., Heian, F., & Hagen, K. B. (2005). Can exercise improve self esteem in children and young people? A systematic review of randomised controlled trials. British Journal of Sports Medicine, 39(11), 792–8. https://doi.org/10.1136/bjsm.2004.017707
- Evans, K., Refshauge, K. M., Adams, R., & Alipr, I. L. (2005). Predictors of Low Back Pain in young elite golfers: A preliminary study. Physical Therapy in Sport, 6(3), 122–30. https://doi.org/10.1016/j.ptsp.2005.05.003
- Farahbakhsh, F., Rostami, M., Noormohammadpour, P., Zade, A. M., Hassanmirazaei, B., Jouibari, M. F., Kordi, R., & Kennedy, D. J. (2018). Prevalence of Low Back Pain among athletes: A systematic review. Journal of Back and Musculoskeletal Rehabilitation, 31(5), 901–916. https://doi.org/10.3233/BMR-170941
- Fett, D., Trompeter, K., Platen, P., & Smith, B. (2017). Back pain in elite sports: A cross-sectional study on 1114 athletes. Public Library of Science ONE, 12(6), e0180130. https://doi.org/10.1371/journal.pone.0180130
- Foley, S. (2020, March 3). 4 steps to save your back [webpage]. golfdigest.com: Golf digest. Retrieved June 4, 2021, from https://www.golfdigest.com/story/save-your-back-foley
- Fradkin, A. J., Cameron, P. A., & Gabbe, B. J. (2007). Is there an association between self-reported warm-up behaviour and golf related injury in female golfers? Journal of Science & Medicine in Sport / Sports Medicine Australia, 10(1), 66–71. https://doi.org/10.1016/j.jsams.2006.04.001
- Freedman, K. F. (2018, November 19). How to avoid back pain from your golf swing [webpage]. Rothman Orthopaedics; Retrieved June 4,2021, from https://rothmanortho.com/stories/blog/Back-Pain-From-Golf-Swing
- Gao, K. L., Hui-Chan, C. W., & Tsang, W. W. (2011). Golfers have better balance control and confidence than healthy controls. European Journal of Applied Physiology, 111(11), 2805–12. https://doi.org/10.1007/s00421-011-1910-7
- Gosheger, G., Liem, D., Ludwig, K., Greshake, O., & Winkelmann, W. (2003). Injuries and overuse syndromes in golf. The American Journal of Sports Medicine, 31(3), 438–443. https://doi.org/10.1177/03635465030310031901
- Goubert, D., Oosterwijck, J. V., Meeus, M., & Danneels, L. (2016). Structural changes of lumbar muscles in non-specific Low Back Pain: A systematic review. Pain Physician, 19(7), E985–e1000. https://doi.org/10.36076/ppj/2016.19.E985
- Gulgin, H. R., & Armstrong, C. W. (2008). Passive hip rotation range of motion in LPGA golfers. Clinical Kinesiology: Journal of the American Kinesiotherapy Association, 62(2), 9–15.
- Guyatt, G. H., Oxman, A. D., Vist, G. E., Kunz, R., Falck-Ytter, Y., Alonso-Coello, P., & Schünemann, H. J. (2008). GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ: British Medical Journal, 336(7650), 924–926. https://doi.org/10.1136/bmj.39489.470347.AD
- Hawkes, R., O’Connor, P., & Campbell, D. (2013). The prevalence, variety and impact of wrist problems in elite professional golfers on the European tour. British Journal of Sports Medicine, 47(17), 1075–9. https://doi.org/10.1136/bjsports-2012-091917
- Horton, J. F., Lindsay, D. M., & Macintosh, B. R. (2001). Abdominal muscle activation of elite male golfers with chronic Low Back Pain. Medicine and Science in Sports and Exercise, 33(10), 1647–54. https://doi.org/10.1097/00005768-200110000-00006
- How to Fix Golf Back Pain. (2021,June 3). [Webpage]. rotaryswing.com. Retrieved June 4, 2021, from https://rotaryswing.com/golf-instruction-videos/full-swing-basics/downswing/golf-back-pain-cure
- Hoy, D., Bain, C., Williams, G., March, L., Brooks, P., Blyth, F., Woolf, A., Vos, T., & Buchbinder, R. (2012). A systematic review of the global prevalence of Low Back Pain. Arthritis & Rheumatism, 64(6), 2028–2037. https://doi.org/10.1002/art.34347
- Hume, P. A., Keogh, J., & Reid, D. (2005). The role of biomechanics in maximising distance and accuracy of golf shots. Sports Medicine, 35(5), 429–49. https://doi.org/10.2165/00007256-200535050-00005
- James, J. (2019, April 9). Why do I have lower back pain after playing golf? [Webpage]. Golf Forever; RetrievedJune 4, 2021, from https://golfforever.com/lower-back-pain-after-golfing/
- Kamson, S. (2020, March 20). Tips for golfing with back pain [webpage]. Spine Institute Northwest; Retrieved June 4,2021, from https://www.spineinstitutenorthwest.com/tips-for-golfing-with-back-pain/
- Knezevic, N. N., Candido, K. D., Vlaeyen, J. W. S., Van Zundert, J., & Cohen, S. P. (2021). Low Back Pain. The Lancet, 398(10294), 78–92. https://doi.org/10.1016/S0140-6736(21)00733-9
- Lim, Y.-T., Chow, J. W., & Chae, W.-S. (2012). Lumbar spinal loads and muscle activity during a golf swing. Sports Biomechanics, 11(2), 197–211. https://doi.org/10.1080/14763141.2012.670662
- Lindsay, D., & Horton, J. (2007). Comparison of spine motion in elite golfers with and without Low Back Pain. Journal of Sports Sciences, 20(8), 599–605. https://doi.org/10.1080/026404102320183158
- McCall, A., Carling, C., Davison, M., Nedelec, M., Le Gall, F., Berthoin, S., & Dupont, G. (2015). Injury risk factors, screening tests and preventative strategies: A systematic review of the evidence that underpins the perceptions and practices of 44 football (soccer) teams from various premier leagues. British Journal of Sports Medicine, 49(9), 583–589. https://doi.org/10.1136/bjsports-2014-094104
- McCarroll, J. R., & Gioe, T. J. (1982). Professional golfers and the price they pay. The Physician and Sportsmedicine, 10(7), 64–70. https://doi.org/10.1080/00913847.1982.11947272
- McCarroll, J. R., Rettig, A. C., & Shelbourne, K. D. (1990). Injuries in the amateur golfer. The Physician and Sportsmedicine, 18(3), 122–6. https://doi.org/10.1080/00913847.1990.11709999
- McHardy, A., Pollard, H., & Luo, K. (2007). One-year follow-up study on golf injuries in Australian amateur golfers. The American Journal of Sports Medicine, 35(8), 1354–1360. https://doi.org/10.1177/0363546507300188
- McHardy, A. J., Pollard, H. P., & Luo, K. (2007). Golf-related lower back injuries: An epidemiological survey. Journal of Chiropractic Medicine, 6(1), 20–26. https://doi.org/10.1016/j.jcme.2007.02.010
- McLean, J. (1992). Widen the gap. Golf Magazine, 12, 49–53.
- Mohd Isa, I. L., Teoh, S. L., Mohd nor, N. H., & Mokhtar, S. A. (2022). Discogenic Low Back Pain: Anatomy, pathophysiology and treatments of intervertebral disc degeneration. International Journal of Molecular Sciences, 24(1), 208. https://doi.org/10.3390/ijms24010208
- Murase, Y., Kamei, S., & Hoshikawa, T. (1989). Heart rate and metabolic responses to participation in golf. The Journal of Sports Medicine and Physical Fitness, 29(3), 269–72.
- Murray, A. D., Daines, L., Archibald, D., Hawkes, R. A., Schiphorst, C., Kelly, P., Grant, L., & Mutrie, N. (2017). The relationships between golf and health: A scoping review. British Journal of Sports Medicine, 51(1), 12–19. https://doi.org/10.1136/bjsports-2016-096625
- Murray, A., Junge, A., Robinson, P. G., Bizzini, M., Bossert, A., Clarsen, B., Coughlan, D., Cunningham, C., Drobny, T., Gazzano, F., Gill, L., Hawkes, R., Hospel, T., Neal, R., Lavelle, J., Scanlon, A., Schamash, P., Thomas, B., … Wotherspoon, M. (2020). International consensus statement: Methods for recording and reporting of epidemiological data on injuries and illnesses in golf. British Journal of Sports Medicine, 54(19), 1136–1141. https://doi.org/10.1136/bjsports-2020-102380
- National Institute for Health and Care Excellence. Appendix E Algorithm for classifying quantitative (experimental and observational) study designs methods for the development of NICE public health guidance (3rd edition) (2012) [ Available from: https://www.nice.org.uk/process/pmg4/chapter/appendix-e-algorithm-for-classifying-quantitative-experimental-and-observational-study-designs
- Nicholas, M. K., Linton, S. J., Watson, P. J., & Main, C. J. (2011). Early identification and management of psychological risk factors (“yellow flags”) in patients with Low Back Pain: A reappraisal. Physical Therapy, 91(5), 737–53. https://doi.org/10.2522/ptj.20100224
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan-a web and mobile app for systematic reviews. Systematic Review, 5(1), 210. https://doi.org/10.1186/s13643-016-0384-4
- Page, M. J., Moher, D., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., … Whiting, P. (2021). PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ: British Medical Journal, 372, n160. https://doi.org/10.1136/bmj.n160
- Palank, E. A., & Hargreaves Jr, E.H. (1990). The benefits of walking the golf course. The Physician and Sportsmedicine, 18(10), 77–80. https://doi.org/10.1080/00913847.1990.11710155
- Parkkari, J., Natri, A., Kannus, P., Mänttäri, A., Laukkanen, R., Haapasalo, H., Nenonen, A., Pasanen, M., Oja, P., & Vuori, I. (2000). A controlled trial of the health benefits of regular walking on a golf course. The American Journal of Medicine, 109(2), 102–108. https://doi.org/10.1016/S0002-9343(00)00455-1
- Pataky, T., Vanrenterghem, J., & Robinson, M. (2016). The probability of false positives in zero-dimensional analyses of one-dimensional kinematic, force and EMG trajectories. Journal of Biomechanics, 49(9), 1468–1476. https://doi.org/10.1016/j.jbiomech.2016.03.032
- Pincus, T., Burton, A. K., Vogel, S., & Field, A. P. (2002). A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of Low Back Pain. Spine, 27(5), E109–20. (Phila Pa 1976). https://doi.org/10.1097/00007632-200203010-00017
- Quinn, S. L., Olivier, B., & McKinon, W. (2022). Lower quadrant swing biomechanics identifies golfers with increased risk of Low Back Pain: A prospective longitudinal cohort study. Journal of Sport Rehabilitation, 31(8), 1041–51. https://doi.org/10.1123/jsr.2021-0191
- Quinn, S. L., Olivier, B., McKinon, W., & Dafkin, C. (2022). Increased trunk muscle recruitment during the golf swing is linked to developing lower back pain: A prospective longitudinal cohort study. Journal of Electromyography and Kinesiology, 64, 102663. https://doi.org/10.1016/j.jelekin.2022.102663
- Quirk, H., Hock, E., Harrop, D., Crank, H., Peckham, E., Traviss-Turner, G., Machaczek, K., Stubbs, B., Horspool, M., Weich, S., & Copeland, R. (2020). Understanding the experience of initiating community-based group physical activity by people with serious mental illness: A systematic review using a meta-ethnographic approach. European Psychiatry: The Journal of the Association of European Psychiatrists, 63(1), e95. https://doi.org/10.1192/j.eurpsy.2020.93
- Rab, G. T., Chao, E. Y., & Stauffer, R. N. (1977). Muscle force analysis of the lumbar spine. The Orthopedic Clinics of North America, 8(1), 193–9. https://doi.org/10.1016/S0030-5898(20)30945-7
- Roberts, M. (2019,February 5). ‘X-factor’ golf swing linked to back pain. [Webpage]. BBC; Retrieved June 4,2021, from https://www.bbc.co.uk/news/health-47114990
- Robinson, P. G., Murray, I. R., Duckworth, A. D., Hawkes, R., Glover, D., Tilley, N. R., Hillman, R., Oliver, C. W., & Murray, A. D. (2019). Systematic review of musculoskeletal injuries in professional golfers. British Journal of Sports Medicine, 53(1), 13–18. https://doi.org/10.1136/bjsports-2018-099572
- Rose, G. (2014,September 19). The golfer’s guide to lower back pain – part 1. [Webpage]. mytpi.com: TPI Nevada; Retrieved June4,2021, from https://www.mytpi.com/articles/health/the_golfer’s_guide_to_lower_back_pain_part_1
- The Royal and Ancient. Golf around the world. (2015).
- Schuler, T. (2020,September 18). 5 easy tips to prevent back pain due to golfing [webpage]. Virginia Spine Institute; Retrieved June 4,2021, from https://www.spinemd.com/5-easy-tips-to-prevent-back-pain-from-golfing/
- Sim, T., Choi, A., Lee, S., & Mun, J. H. (2017). How to quantify the transition phase during golf swing performance: Torsional load affects low back complaints during the transition phase. Journal of Sports Sciences, 35(20), 2051–9. https://doi.org/10.1080/02640414.2016.1255345
- Smith, J. A., Hawkins, A., Grant-Beuttler, M., Beuttler, R., & Lee, S.-P. (2018). Risk factors associated with Low Back Pain in golfers: A systematic review and meta-analysis. Sports Health, 10(6), 538–546. https://doi.org/10.1177/1941738118795425
- Smith, M. F., & Hillman, R. (2012). A retrospective service audit of a mobile physiotherapy unit on the PGA European golf tour. Physical Therapy in Sport, 13(1), 41–4. https://doi.org/10.1016/j.ptsp.2010.09.001
- Song, M. X., Yang, H., Yang, H. Q., Li, S. S., Qin, J., & Xiao, Q. (2023). MR imaging radiomics analysis based on lumbar soft tissue to evaluate lumbar fascia changes in patients with Low Back Pain. Academic Radiology, 30(11), 2450–2457. https://doi.org/10.1016/j.acra.2023.02.038
- Sports Marketing Surveys. The R&A: Strategy core figures. (2021).
- Sterne, J. A., Hernán, M. A., Reeves, B. C., Savović, J., Berkman, N. D., Viswanathan, M., Henry, D., Altman, D. G., Ansari, M. T., Boutron, I., Carpenter, J. R., Chan, A.-W., Churchill, R., Deeks, J. J., Hróbjartsson, A., Kirkham, J., Jüni, P., Loke, Y. K., … Whiting, P. F. (2016). ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ: British Medical Journal, 355, i4919. https://doi.org/10.1136/bmj.i4919
- Trompeter, K., Fett, D., & Platen, P. (2017). Prevalence of back pain in sports: A systematic review of the literature. Sports Medicine, 47(6), 1183–1207. (Auckland, NZ). https://doi.org/10.1007/s40279-016-0645-3
- Tsai, Y. S., Sell, T. C., Smoliga, J. M., Myers, J. B., Learman, K. E., & Lephart, S. M. (2010). A comparison of physical characteristics and swing mechanics between golfers with and without a history of Low Back Pain. Journal of Orthopaedic and Sports Physical Therapy, 40(7), 430–8. https://doi.org/10.2519/jospt.2010.3152
- Vad, V. B., Bhat, A. L., Basrai, D., Gebeh, A., Aspergren, D. D., & Andrews, J. R. (2004). Low Back Pain in professional golfers: The role of associated hip and low back range-of-motion deficits. The American Journal of Sports Medicine, 32(2), 494–7. https://doi.org/10.1177/0363546503261729
- van Tulder, M., Furlan, A., Bombardier, C., & Bouter, L. (2003). Updated method guidelines for systematic reviews in the Cochrane collaboration back review group. Spine, 28(12), 1290–1299. (Phila Pa 1976). https://doi.org/10.1097/01.BRS.0000065484.95996.AF
- Vlaeyen, J. W. S., Maher, C. G., Wiech, K., Van Zundert, J., Meloto, C. B., Diatchenko, L., Battié, M. C., Goossens, M., Koes, B., & Linton, S. J. (2018). Low Back Pain. Nature Reviews Disease Primers, 4(1), 52. https://doi.org/10.1038/s41572-018-0052-1
- Warmenhoven, J., Harrison, A., Robinson, M. A., Vanrenterghem, J., Bargary, N., Smith, R., Cobley, S., Draper, C., Donnelly, C., & Pataky, T. (2018). A force profile analysis comparison between functional data analysis, statistical parametric mapping and statistical non-parametric mapping in on-water single sculling. Journal of Science & Medicine in Sport / Sports Medicine Australia, 21(10), 1100–1105. https://doi.org/10.1016/j.jsams.2018.03.009
- White, H., Albers, B., Gaarder, M., Kornør, H., Littell, J., Marshall, Z., Mathew, C., Pigott, T., Snilstveit, B., Waddington, H., & Welch, V. (2020). Guidance for producing a Campbell evidence and gap map. Campbell Systematic Reviews, 16(4), e1125. https://doi.org/10.1002/cl2.1125
- Zheng, N., Barrentine, S. W., Fleisig, G. S., & Andrews, J. R. (2008). Kinematic analysis of swing in pro and amateur golfers. International Journal of Sports Medicine, 29(6), 487–93. https://doi.org/10.1055/s-2007-989229