Peritoneal carcinomatosis from gastrointestinal cancer, gynaecologic cancer, and peritoneal mesothelioma was accepted by physicians caring for cancer patients as a uniformly lethal condition. This has changed. As a result of three decades of laboratory and clinical investigation, peritoneal metastases (no longer referred to as carcinomatosis) can be prevented or can be cured. Knowledgeable application of treatment modalities currently available is essential to success. As peritoneal metastases studies expanded worldwide, an international forum for presentation and exchange of ideas was essential to facilitate progress. To this end, the Peritoneal Surface Oncology Group International (PSOGI) emerged sponsoring a biennial workshop to update the global efforts in peritoneal metastases. The expansion of research, education, and practice began in 1998 as a small meeting in Basingstoke, UK with approximately 20 participants. In contrast, on 17–19 November 2016 approximately 700 participants from 54 countries around the globe gathered in Washington, DC for two and a half days of a comprehensive update of strategies to control peritoneal metastases (). Twenty meet-the-professor breakfast seminars, six didactic lectures, five debates, five patient presentation sessions, comprehensive review of active protocols and international registries plus two satellite sessions took place. This special issue on cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) selected the best PSOGI 2016 presentations for this multi-authored monograph on peritoneal metastases.
Table 1. Peritoneal Surface Oncology Group International (PSOGI) 1998–2016.
This special issue of International Journal of Hyperthermia contains a wide variety of topics all focussed on expansion of our knowledge on peritoneal metastases. A survey of the clinical trials activity with CRS and HIPEC in colorectal cancer, ovarian cancer, and gastric cancer occurred. The efforts currently active in colorectal cancer include both trials to prevent peritoneal metastases from occurring at some time in the future in high-risk patients, and also trials to improve the eradication of established peritoneal metastases. In ovarian cancer, HIPEC is being tested in the management of both primary and recurrent ovarian cancer. In gastric cancer, HIPEC is being tested as well as neoadjuvant intraperitoneal and systemic chemotherapy (NIPS).
New sources of information concerning patient selection for CRS and HIPEC applications are the international registries. This strategy for accumulating data on large numbers of patients from many institutions worldwide may be especially valuable for rare diseases such as peritoneal mesothelioma and small bowel adenocarcinoma. Also, there are many rare diseases that fail curative treatment because of peritoneal metastases. The BIG RENAPE registry of rare diseases converts the anecdotal patient treated by CRS and HIPEC into a series of patients whereby the results of treatment can be critically evaluated and selection factors determined. The national registries work to standardise and optimise patient management and encourage a critical evaluation of outcomes.
A longstanding criticism of peritoneal metastases management has been the multiple different HIPEC regimens used at different institutions. Through a comprehensive review of pharmacology and a survey of results of treatment over two decades, a recommendation for standardised HIPEC for the many diseases with peritoneal metastases currently treated has been possible.
There is a great need in the efforts to continue to improve the results of treatment of peritoneal metastases to optimally select patients. There is no doubt that some patients have a high likelihood to develop peritoneal metastases. Identification of these patients and then initiating a properly timed CRS and HIPEC or HIPEC added to a primary colorectal surgery is now being investigated. Also important in selection is the radiologic identification of patients who, if treated by CRS and HIPEC, would be unlikely to profit. The description of concerning radiologic features that facilitates exclusion of patients with poor results of treatment is now possible and will improve as more data accumulates.
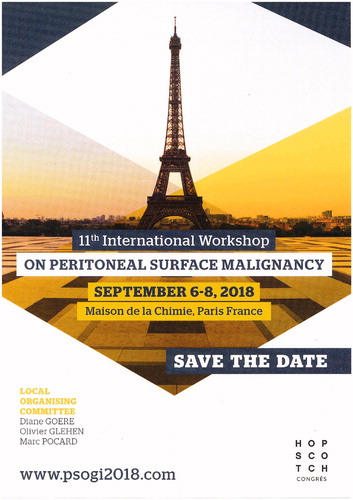
Finally, 10 take home messages were given to PSOGI 2016 delegates and readers of this special issue to stimulate further discussion. Hopefully, the challenges expressed within this special issue of current state of the art continue through to PSOGI 2018 in Paris ().
Figure 1. Peritoneal Surface Oncology Group International 2018 in Paris. (Figure from Sugarbaker PH. The seven best from PSOGI 2016. Ann Surg Oncol. 2017 Feb 6. doi: 10.1245/s10434–017-5793–7).
Paul H. SugarbakerCenter for Gastrointestinal Malignancies, MedStar Washington Hospital Center, Washington, DC, USA [email protected]© 2017 Informa UK Limited, trading as Taylor & Francis Group
