Abstract
Introduction: Radiological imaging often underestimates the extent of low volume peritoneal disease. The benefit of laparoscopy in assessing peritoneal metastases from colorectal and gastric cancer is accepted, but is inconclusive for appendiceal malignancy. We report our experience of diagnostic (DL) and therapeutic laparoscopy (TL) in patients with appendiceal tumours to determine indications and role in assessment and management.
Methods: A retrospective review of a National Peritoneal Malignancy Centre’s prospectively maintained database was performed. All patients with appendiceal neoplasms who underwent DL or TL between September 2011 and January 2016 were included. The indications and outcomes of the laparoscopy, complications and interval to laparotomy were evaluated.
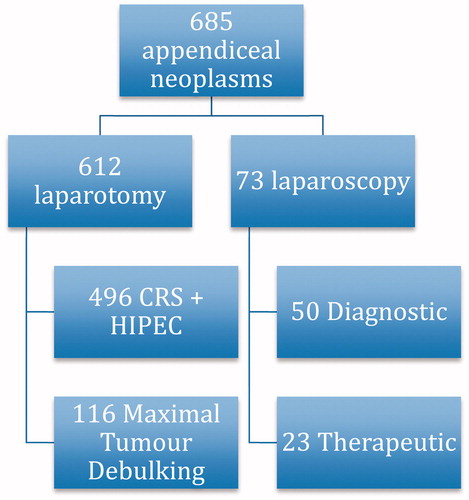
Results: Six hundred and eighty-five patients underwent surgery for appendiceal neoplasms during the study period, of which 73 (10.6%) underwent laparoscopy (50 DL, 23 TL). The main indications for DL were to clarify imaging and stage patients with high-risk histology. Indications for TL were an abnormal appendix without gross pseudomyxoma peritonei (PMP) or with low volume PMP, and concerns for fertility in the presence of PMP. DL resulted in 16 patients (32%) avoiding laparotomy because of extensive disease or no tumour found. Overall, 28 patients were assessed to have resectable disease and at laparotomy, 25/28 had complete cytoreduction with three patients unresectable. In the TL group, appendicectomy and peritoneal lavage was achieved in all four women with fertility concerns, allowing them to conceive thereafter. There were no complications.
Conclusions: Patients with high-risk appendiceal neoplasm may benefit from DL, and potentially avoid unnecessary laparotomy. TL is useful in patients with low volume PMP and may aid fertility in selected patients.
Introduction
Epithelial appendiceal tumours comprise a range of pathological and clinical entities, extending from benign adenomas to malignant nonmucinous adenocarcinomas with localised or extensive disease. Mucinous neoplasms are intermediate in this broad spectrum, and when ruptured, commonly result in a clinical syndrome known as pseudomyxoma peritonei (PMP) [Citation1]. The condition classically presents as a diffuse seeding of the peritoneal surfaces, omentum and ovaries with profuse intra-peritoneal mucin. Patients with advanced PMP present with variable symptoms including most commonly increasing abdominal distention, early satiety, respiratory distress and symptoms of intestinal obstruction.
Cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) is the standard of care for patients with PMP and can achieve overall survival (OS) outcomes of up to 84% at 5 years [Citation2,Citation3]. The strategy of CRS and HIPEC encompasses surgical removal of all macroscopic disease by parietal peritoneal resection and removal of involved viscera [Citation4], combined with intraperitoneal perfusion of hyperthermic chemotherapy (heated to 43 °C) aiming to eradicate the microscopic disease.
Even when complete cytoreduction is not possible, symptomatic patients with PMP from low-grade appendiceal tumours can derive significant benefit, and survival advantage, when major tumour debulking is achieved [Citation5].
Radiological imaging, such as computed tomography (CT), magnetic resonance imaging (MRI) and positron emission tomography-CT scans help to detect systemic metastases and to estimate the extent of peritoneal disease but are known to underestimate and under-stage small volume disease [Citation6–8]. The unresectable disease may, therefore, be detected intra-operatively. This is generally due to the extensive and widespread involvement of the small bowel serosa and mesentery, as peritoneal lesions in other sites are usually resectable. Thus, for instance, total colectomy and even gastrectomy may be necessary and can result in long-term survival and cure but enough small bowel needs to be preserved.
There is increasing awareness of the role of selective laparoscopy in pre-operative assessment of peritoneal malignancy. Most series confirm a definite role in gastric and colorectal peritoneal malignancy [Citation9,Citation10] but have generally concluded that laparoscopy has a limited role in appendiceal malignancy, particularly in mucinous tumours where many patients benefit form CRS or debulking and extensive disease precludes laparoscopy [Citation5].
Our approach has been a liberal use of laparoscopy in patients with colorectal peritoneal metastases who are all considered for staging laparoscopy if feasible, but a more selective use in patients with appendiceal tumours. Our aim has been to avoid over treatment for either minimal or no disease or major futile surgery for extensive disease resulting in an “open and close”. The impact of an abandoned CRS-HIPEC procedure is two-fold, patients are devastated at the loss of hope of long-term survival, and secondly, from a logistical viewpoint, an abandoned procedure is a huge waste of hospital resources as an operating will have been resourced for a potentially long operation taking on average 10 h.
For these reasons, we report our experience with laparoscopy in selected cases with appendiceal tumours, to determine the indications and role of laparoscopy in this setting.
Methods
A retrospective review of the Basingstoke Peritoneal Malignancy Institute’s prospectively maintained database was performed. All patients with appendiceal neoplasms who underwent laparoscopy between September 2011 and January 2016 were included. Patients were categorised into two groups, diagnostic laparoscopy (DL) or therapeutic laparoscopy (TL) depending on the main indication for the procedure. The proportion of complete cytoreduction in patients assessed at DL to be amenable for CRS-HIPEC was calculated. For patients who underwent TL, the indications and outcome were recorded. In addition, procedure-related complications and the interval to laparotomy were documented. The proportion of patients excluded from CRS-HIPEC based on laparoscopic findings was also calculated.
Laparoscopic evaluation
Laparoscopic access was based on surgeon’s preference and was performed via Hasson’s technique in the periumbilical region, or at Palmer’s point. In all cases, previous surgical scars were avoided, and midline port positioning, if feasible, was preferred to allow resection of the scar in the event that the patient subsequently proceeded to laparotomy and CRS-HIPEC. A thorough and systematic evaluation of the entire peritoneal cavity was performed, with additional ports placed to aid with selective adhesiolysis, perform biopsies and perform resections as judged necessary by the surgeon. Additional ports were also preferentially placed in the midline. Assessment of the peritoneal cavity and the likelihood of achieving a complete cytoreduction were recorded. Areas of the peritoneal cavity which were not well visualised were documented.
Results
Indications
Between September 2011 and January 2016, 685 patients underwent surgery for appendiceal neoplasms in our institution. Overall 612 patients went straight to laparotomy and 496 patients (72.4%) underwent complete CRS-HIPEC, 116 patients (17%) underwent maximal tumour debulking and the remaining 73 patients (10.6%) underwent laparoscopy, of which 50 were diagnostic, and 23 were therapeutic (. The median follow-up for this study was 23.9 months (3.1–58.5 months).
The most common indications for DL were to clarify imaging findings (42%), staging peritoneal involvement for high-risk histology (28%) and to obtain a histological diagnosis (14%). Nine patients had more than one indication for DL.
TL was performed because of an abnormal appendix in the absence of gross PMP (on imaging) in 15 patients (65%), an abnormal appendix with low volume PMP in four patients (17%) and in four patients (17%), low-grade PMP with minimal peritoneal disease was seen on imaging, but laparoscopy was performed to assess the extent of disease, as the patients’ were contemplating pregnancy, and did not agree to upfront surgery which, may involve bilateral oophorectomy. Patient demographics are outlined in and indications for laparoscopy in .
Table 1. Patient demographics.
Table 2. The indications for diagnostic and therapeutic laparoscopy.
Outcomes
Visualisation during diagnostic laparoscopy
In the DL group, 38 patients (76%) underwent a successful laparoscopy with good visualisation, while 12 patients (24%) had poor views obtained. Poor views were mostly of the small bowel, pelvis and left upper quadrant (spleen and stomach) ().
Table 3. Outcomes of diagnostic laparoscopy.
Assessment during diagnostic laparoscopy
Thirty-one patients were assessed to have resectable PMP and 28 patients went on to have a laparotomy. Of these 28 patients, three were found to be unresectable intra-operatively and underwent maximum tumour debulking. The remaining 25 patients had complete CRS and HIPEC. Two of the 31 patients are currently awaiting laparotomy at the time of writing, and one patient developed pulmonary metastases before planned laparotomy. The median time from laparoscopy to laparotomy was 28 d (0–103 d).
Three patients had no tumour detected at laparoscopy, and one patient was found to have acellular mucin on histology. These four patients did not proceed to a laparotomy. One of the four patients subsequently presented with right hydronephrosis secondary to peritoneal disease and was considered to have been under-staged at DL.
Twelve patients were assessed to have the inoperable disease at DL and did not proceed to laparotomy. The indications for DL in these 12 were high-risk histology in six patients, to clarify CT findings in four and post-chemotherapy assessment in two. These patients were referred for palliative chemotherapy or best supportive care.
DL was equivocal in two patients, as it was not possible to commit to an assessment of resectability based on the laparoscopic views obtained. One of the patients went on to undergo complete CRS and HIPEC, while the other patient developed liver metastases and was not a candidate for CRS-HIPEC.
The findings of the last DL were not available for review. The outcomes of the DL are summarised in .
Therapeutic laparoscopy
The indications for TL included an abnormal appendix at cross-sectional imaging and fertility issues. Overall, 15/19 patients with an abnormal appendix on imaging underwent laparoscopic appendicectomy. Of the remaining four patients, one patient had a concurrent appendicectomy and oophorectomy as the ovaries were grossly abnormal. Two patients were converted to an open appendicectomy because of poor visualisation, and one patient converted to an open right hemicolectomy as the caecum was involved in the appendix tumour. The histological findings are summarised in .
Table 4. Histology of resection specimens for patients who underwent TL.
The four patients with fertility issues and low-grade PMP were diagnosed while undergoing investigations for infertility. During the laparoscopy, all four patients’ ovaries were encased with mucin, and three patients underwent laparoscopic appendicectomy and peritoneal lavage, with one patient converted to an open appendicectomy and peritoneal lavage because of adhesions. Peritoneal lavage included washing and aspiration with up to 2 l of warm saline and meticulous cleaning of the ovaries in all four patients. Histology revealed a low-grade appendiceal mucinous neoplasm with low-grade mucinous carcinoma peritonei in two patients and a low-grade appendiceal mucinous neoplasm with acellular mucin in the remaining two patients. All four patients have proceeded on to have children since the TL, and are to date, disease-free on follow-up.
Complications
There were no procedure-related complications amongst the 73 cases. To our knowledge, none of the patients have developed port site metastases. The median length of stay was 1 d (1–10 d) for the whole group.
Discussion
There is an increasing awareness of the role of CRS and HIPEC in the management of patients with PMP of appendiceal origin. Patients’, in whom complete cytoreduction can be achieved, benefit most from the procedure. CRS and HIPEC, however, has associated morbidity and mortality [Citation8,Citation11] and accurate staging in those with minimal or equivocal findings on radiology may avoid major surgery allowing a wait and watch approach. Furthermore, in low-grade disease, symptomatic patients derive benefit with prolonged survival with major tumour debulking [Citation5] but this is not necessarily the case with high-grade more aggressive appendiceal tumours where if there is widespread small bowel involvement, palliative chemotherapy may be a better option. DL evaluation provides a low-risk option for selected patients with appendiceal tumours with the goal of avoiding unnecessary laparotomy.
It is evident that not all patients with appendiceal neoplasms will benefit from a laparoscopic procedure. This study evaluated the role of laparoscopy in selected patients with appendiceal tumours, in a high-volume peritoneal malignancy unit primarily focussed on the treatment of PMP. Laparoscopy was performed in 10% of cases over the course of 4 years, 50 patients underwent DL and 23 patients underwent TL. DL was useful in patients with high-risk histology, CT findings suggestive of extensive disease and post chemotherapy assessment, avoiding unnecessary surgery in 12 of 50 patients (24%) with extensive disease on DL and one patient (2%) with acellular mucin on histological examination. A further 6% (3/50) of patients were found to have no disease during DL and did not undergo a laparotomy.
It is well established that low-volume peritoneal disease is underestimated by non-invasive imaging techniques. In particular, low-volume small bowel disease is difficult to ascertain on CT scans [Citation12]. In this study, five patients who had limited progressive disease on CT scan underwent DL and were found to have more extensive disease than seen on CT. MRI is another imaging modality which is being evaluated, in an attempt to increase the detection of small bowel disease [Citation13], but outcomes have been variable [Citation14,Citation15]. In the study by Torkzak, MRI was found to be comparable to CT scan in detecting peritoneal disease when interpreted by an experienced radiologist, but inferior to CT when interpreted by a less experienced MRI radiologist [Citation14]. Low et al. found that delayed gadolinium-enhanced MRI was the most accurate of the MR techniques, with a sensitivity of 82–89%, and specificity of 87% [Citation15].
Small bowel involvement is generally the main reason precluding complete CRS in PMP, and within the spectrum of appendiceal neoplasm, some tumours exhibit a more aggressive behaviour and are more likely to involve the small bowel. These consist of adenocarcinoma ex-goblet cell, and high-grade mucinous carcinoma peritonei with signet ring cells [Citation1]. These patients, in our experience, may benefit from DL and 24% (12/50) of patients in our experience avoided an unnecessary laparotomy.
In many instances, patients with the metachronous peritoneal disease have undergone multiple abdominal operations before referral for consideration of CRS-HIPEC. One of the common reasons that laparoscopic evaluation prior to laparotomy is not utilised, is the fear of significant adhesions, which can result in difficulty gaining access to the peritoneal cavity, poor visualisation and inadvertent enterotomies. This is less common with PMP, as with increasing awareness and use of imaging, many patients have had no or minimal (laparoscopy or appendicectomy) surgery prior to referral, hence rendering these feared complications less likely. Our study supports this, as there were no procedure-related complications in this experience, and DL was successful in providing good visualisation in 76% of patients. The technique of avoiding previous laparotomy scars and placing ports in the midline where possible, also allows for excision of the scars in the event that the patient proceeds to CRS and HIPEC, reducing the risk of port-site tumour deposits.
Iversen et al. have evaluated routine laparoscopy in selection of patients for CRS-HIPEC in patients with colorectal, appendiceal, PMP and peritoneal mesothelioma, and found that the inclusion of laparoscopy to the evaluation of patients before CRS-HIPEC increased the completion of cytoreduction rate from 56% to 70%, but this difference was not statistically significant [Citation10]. They concluded that laparoscopy had no role in PMP patients with extensive masses at CT.
In another published experience, DL was incorporated into the management algorithm for patients with peritoneal metastases from 14 different primaries [Citation16]. Tabrizian et al. reported that DL excluded 31% of patients from upfront laparotomy. In the current study, focussed only on appendiceal tumours, DL excluded 32% (12 patients with extensive surgery, one patient with acellular mucin and three patients with no disease) of patients from an unnecessary laparotomy. However, there was a small (2%) risk of under-staging the disease with DL.
TL was indicated mostly for an abnormal appendix on imaging, without the presence of PMP, and was found to be extremely useful in the patients with low-grade PMP, with the minimal disease on imaging, trying for a pregnancy. In four patients who presented having investigations for infertility, laparocopy allowed for a low-risk, minimally invasive procedure to be carried out, to evaluate the peritoneum, perform an appendicectomy for definitive histology and peritoneal lavage to clear the mucin, which was encasing the ovaries and likely contributing to infertility. All four patients in our series went on to have successful pregnancies within a year. This highlights the role, which TL may have in the management of appendiceal tumours, and that TL should be considered when counselling female patients on fertility prior to surgery.
The study has some limitations. Whilst data collection was prospective, the data was retrospectively analysed. In addition, patients included in the study are a highly selected group (accounting for 10% of the total cohort with appendiceal tumours) and were chosen to undergo laparoscopy for specific indications. For this reason, the results are not applicable to all patients with appendiceal neoplasms. However, the findings of this report help to establish a selective role for DL in patients with appendiceal tumours, where laparoscopy has previously been stated to have a limited, or indeed no role and propose some indications where laparoscopy may be used therapeutically in selected patients.
Conclusions
Selected patients with appendiceal tumours may benefit from diagnostic or TL with a low procedural-related risk of complications. Patients with high-risk appendiceal neoplasms may benefit from a DL by potentially avoiding a laparotomy, while TL is useful to clarify image-detected abnormalities, obtain histology from the appendix, and in our experience with four female patients with fertility concerns, allowed for appendicectomy and peritoneal lavage which may contribute to fertility.
Disclosure statement
All authors declare no conflict of interest or receive any funding for research.
References
- Carr N, Cecil TD, Mohamed F, et al. (2016). A consensus for classification and pathologic reporting of pseudomyxoma peritonei and associated appendiceal neoplasia: the results of the Peritoneal Surface Oncology Group International (PSOGI) modified Delphi process. Am J Surg Pathol 40:14–26.
- Smeenk RM, Verwaal VJ, Antonini N, Zoetmulder FA. (2007). Survival analysis of pseudomyxoma peritonei patients treated by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg 245:104–9.
- Moran B, Cecil T, Chandrakumaran K, et al. (2015). The results of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in 1200 patients with peritoneal malignancy. Colorectal Dis 17:772–8.
- Sugarbaker PH. (1995). Peritonectomy procedures. Ann Surg 221:29–42.
- Dayal S, Taflampas P, Riss S, et al. (2013). Complete cytoreduction for pseudomyxoma peritonei is optimal but maximal tumor debulking may be beneficial in patients in whom complete tumor removal cannot be achieved. Dis Colon Rectum 56:1366–72.
- Koh JL, Yan TD, Glenn D, Morris DL. (2009). Evaluation of preoperative computed tomography in estimating peritoneal cancer index in colorectal peritoneal carcinomatosis. Ann Surg Oncol 16:327–33.
- de Bree E, Koops W, Kroger R, et al. (2004). Peritoneal carcinomatosis from colorectal or appendiceal origin: correlation of preoperative CT with intraoperative findings and evaluation of interobserver agreement. J Surg Oncol 86:64–73.
- Jacquet P, Jelinek JS, Chang D, et al. (1995). Abdominal computed tomographic scan in the selection of patients with mucinous peritoneal carcinomatosis for cytoreductive surgery. J Am Coll Surg 181:530–8.
- Mirza A, Galloway S. (2016). Laparoscopy, computerised tomography and fluorodeoxyglucose positron emission tomography in the management of gastric and gastro-oesophageal junction cancers. Surg Endosc 30:2690–6.
- Iversen LH, Rasmussen PC, Laurberg S. (2013). Value of laparoscopy before cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis. Br J Surg 100:285–92.
- Chua TC, Yan TD, Saxena A, Morris DL. (2009). Should the treatment of peritoneal carcinomatosis by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy still be regarded as a highly morbid procedure? A systemic review of morbidity and mortality. Ann Surg 249:900–7.
- Coakley FV, Choi PH, Gougoutas CA, et al. (2002). Peritoneal metastases: detection with spiral CT in patients with ovarian cancer. Radiology 223:495–9.
- Low RN. (2016). Preoperative and surveillance MR imaging of patients undergoing cytoreductive surgery and heated intraperitoneal chemotherapy. J Gastrointest Oncol 7:58–71.
- Torkzad MR, Casta N, Bergman A, et al. (2015). Comparison between MRI and CT in prediction of peritoneal carcinomatosis index (PCI) in patients undergoing cytoreductive surgery in relation to the experience of the radiologist. J Surg Oncol 111:746–51.
- Low R, Barone RM, Gurney JM, Muller WD. (2008). Mucinous appendiceal neoplasms: preoperative MR staging and classification compared with surgical and histopathologic findings. Am J Roentgenol 190:656–65.
- Tabrizian P, Jayakrishnan TT, Zacharias A, et al. (2015). Incorporation of diagnostic laparoscopy in the management algorithm for patients with peritoneal metastases: a multi-institutional analysis. J Surg Oncol 111:1035–40.