Abstract
This is a report of an unintended application of MR-HIFU therapy of uterine fibroids (UFs) in a woman in early pregnancy and should be treated as the first description of such an event.
A 37-year-old nullipara with confirmed UFs, who suffered from excessive uterine bleeding and dysmenorrhea, was qualified for MR-HIFU therapy to reduce UF-related symptoms. The procedure took place 2 months later. No complications occurred and the patient was discharged home in good overall condition. About 5 weeks after the procedure the patient was diagnosed with viable intrauterine pregnancy. Basing on early pregnancy ultrasound it was calculated that at the time of MR-HIFU procedure the patient was about 10 (+/− 3 days) days after the conception. Later, the pregnancy was uncomplicated and she gave birth to a healthy neonate. Physical examinations did not reveal any abnormalities in her child. Symptoms associated with UFs significantly decreased after the therapy and pregnancy.
Despite the fact that the pregnancy being subjected to MR-HIFU treatment had further uncomplicated course, the presented case indicates that counseling/management in women at reproductive age should be standardized to avoid unknown consequences of such unrecommended procedures for the fetus. According to current standards MR-HIFU procedures to treat UFs should never be performed without a negative pregnancy test.
Introduction
Uterine fibroids (UFs) are common, benign tumors originating from the myometrium [Citation1]. The growth and location are the main factors that determine if a tumor leads to symptoms which may include abnormal uterine bleeding, anemia, pelvic and abdominal pain, infertility and a variety of obstetric complications [Citation2].
For many years, surgery remained the method of choice in UF management [Citation2]. Nowadays, there is a trend to make the treatment less invasive and individually tailored to the patient's specific situation [Citation3,Citation4]. Women with symptomatic UFs who wish to conceive search for methods that preserve full ability to reproduce [Citation5]. One of the possible solutions to this problem is the use of ultrasound beam. Magnetic resonance-guided high-intensity focused ultrasound (MR-HIFU) is a quickly developing technology with a potential application in various clinical indications, including UFs [Citation6]. As for now this method is still not recommended for women wishing to preserve fertility, except for selected countries including the USA. However, this point of view is significantly changing by a growing quantity of available data [Citation7,Citation8].
At this point it should be strongly emphasized that we never perform a MR-HIFU procedure to treat UFs without a negative pregnancy test. A pregnancy is considered as an absolute contraindication to the procedure, and there are no data regarding the safety of MR-HIFU. We present an event associated with the application of MR-HIFU for the treatment of fibroids in a woman with undiagnosed early intrauterine pregnancy.
Case report
We present a case of a 37-year-old nullipara with confirmed UFs who suffered from excessive uterine bleeding and dysmenorrhea. The patient was admitted to our department for MR-HIFU therapy as she wanted to reduce the UF-related symptoms and eventually conceive in the future. The patient refused surgery and did not want to use any kind of available hormonal treatment.
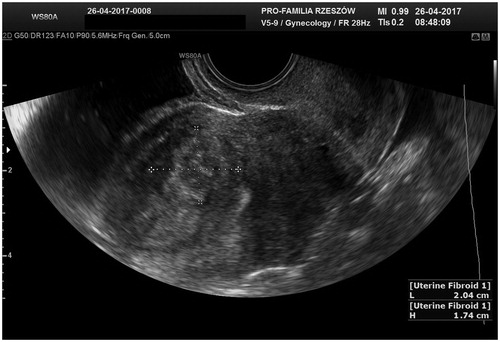
Transvaginal ultrasound scan and magnetic resonance imaging (MRI) (Philips Ingenia 3.0 T system, Philips, Amsterdam, Netherlands) performed during the hospitalization confirmed the presence of 2 UFs. The first one, about 21 × 20 × 17 mm in size (volume = 3.84 cm3), was a type 3 UF according to the FIGO classification [Citation9]. The tumor contacted the endometrium directly which could be the reason for clinical symptoms (). The second tumor coming out of the posterior wall had a diameter of about 10 mm and was a FIGO type 4 UF. The smaller tumor was considered as potentially asymptomatic [Citation9]. MRI signal intensity of both lesions corresponded to type I according to Funaki et al. (2007) [Citation10]. After counseling the patient was qualified for MR-HIFU procedure which was scheduled 2 months later.
Figure 1. Transvaginal ultrasound scan 2 months before MR-HIFU procedure. Uterine fibroid in the anterior wall in direct contact with the endometrium.
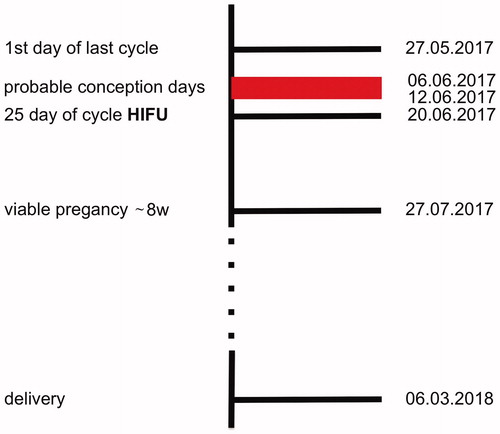
The patient was admitted to the hospital on the indicated day - it was the 25th day of the menstrual cycle. Her menstrual cycles were about the same length every month, occurring every 26–28 days. The patient performed standard urine pregnancy test according to the routine procedure – the test was undoubtedly negative, as a result of which MR-HIFU procedure was initiated. MR-HIFU Sonalleve (Philips, Amsterdam, Netherlands) device, which integrates an MRI scanner, was used. The duration of the whole procedure was about 120 min with the sonification time of 66 min. During MR-HIFU non-perfused volume (NPV) equaled 70%, the maximum power was 180 W and the temperature reached 62 degrees Celsius ( and Citation3). The procedure took place without any complications and the patient was discharged home in a good general condition with the recommendation of presenting for a follow-up visit in 3 months’ time. Due to the prolonging lack of menstrual period the patient came to an earlier check at the outpatient clinic in her place of residence. The physician confirmed the presence of a viable pregnancy (8/9 weeks of gestation - which corresponded to the gestational age from the last menstrual period). The data allowed to calculate that at the time of MR-HIFU procedure the patient was about 10 days after conception according to the first ultrasound, and between 8 and 12 days after conception basing on the date of the last menstruation, which would suggest that the pregnancy may have already nested within the uterine cavity.
Figure 2. The uterus and the uterine fibroid during MR-HIFU procedure. Thermometry guidance during the thermal ablation.
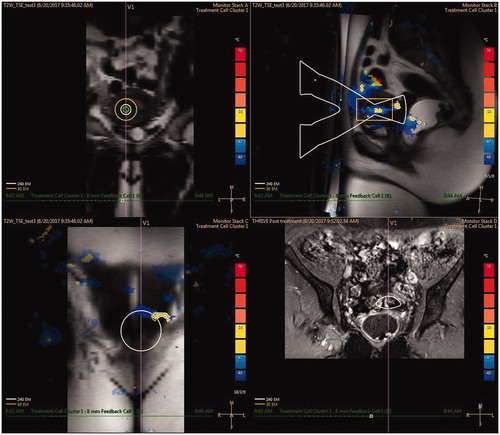
Figure 3. MRI scan of the lower abdomen and pelvis. (A) MR-HIFU qualification MRI scan. (B) MRI scan after the MR-HIFU procedure – visible tumor necrosis.
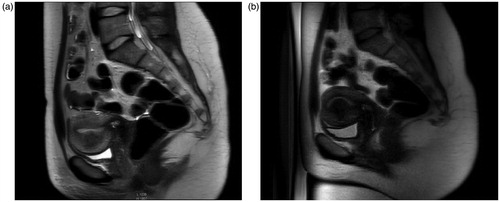
The later part of the pregnancy was uncomplicated, the fetus grew normally and the UF did not cause any symptoms (). The patient was initially scheduled for a vaginal delivery. However, due to a suspicion of macrosomia she was re-qualified for a cesarean section. The patient gave birth to a healthy neonate (4135 grams), the first and subsequent physical examinations did not reveal any abnormalities in the child, the UF was not removed during the surgery. Due to the lack of obstetric complications and the reduction of UF-related symptoms, the patient was not subjected to further treatment. The case report timeline is available in .
Discussion
According to the extensive research through the available databases this is the first described case of a woman with UFs who underwent MR-HIFU procedure after conception and gave birth to a healthy neonate.
MR-HIFU method is focused on optimal clinical efficacy, quick recovery and high-grade safety [Citation11]. Side effects are uncommon in patients who decided to choose this therapy [Citation12]. According to available data the majority of women in whom MR-HIFU was performed reported a significant reduction in UF‐related clinical symptoms and no need of re-intervention [Citation7,Citation12]. Even with those highly successful results MR-HIFU still does not find its place in general UF treatment guidelines and is not recommended for women wishing to conceive [Citation13], probably due to the lack of extensive high quality data about the safety of the procedure for further pregnancy. However, in recent years the trend to strictly prohibit this form of treatment has been slowing down. Some authors stated that such a form of therapy should not be treated as a contraindication to future pregnancies [Citation7]. A recent systematic review revealed that pregnancies after this form of treatment had low complication rates and the major negative effect was first trimester bleeding. However, further studies should be performed to obtain additional data [Citation14]. Very recent studies demonstrated that pregnancies after MR-HIFU treatment have favorable outcomes and no strictly related symptoms occur in the perinatal period [Citation8,Citation15]. Vaginal delivery after this kind of therapy appears to be safe as well [Citation8].
The presented case shows that despite the use of a strong ultrasound beam on already existing pregnancy, there were no adverse outcomes. In our opinion, the use of MR-HIFU in case of an already confirmed pregnancy is and will be absolutely contraindicated, and this case should be treated as an unexpected and unrecommended event. Our case showed that urine pregnancy test was insufficient to qualify the patient for the procedure during late secretory phase. Therefore, we suggest to perform an additional blood test to exclude pregnancy in such cases (e.g. urine with subsequent blood test at a different stage of the cycle). However, the majority of UF patients have abnormal uterine bleeding so it might be difficult to tell when the normal cycle occurs. Guidelines for the safe performance of the procedure in women at reproductive age should be developed. Furthermore, detailed counseling should be conducted including the recommendation to refrain from sexual intercourses without contraception if surgery is planned in the luteal phase. If effective contraception cannot be obtained, another solution may be the use of MR-HIFU only during the first phase of the cycle. Our case shows that the ultrasound used in MR-HIFU is focused strictly on the structure being treated, probably without large damage the adjacent fragile tissues (the endometrium, early pregnancy). Despite the uncomplicated pregnancy after the event, this case report does not provide a prognostic value for other similar events, and further efforts should be focused on avoiding the risk for the fetus.
Conclusion
In the presented case, the result of pregnancy being subjected to MR-HIFU treatment was favorable.
MR-HIFU procedure to treat UFs should never be performed without a negative pregnancy test. However, more detailed guidelines for a safe use of MR-HIFU and additional tests in women at reproductive age are necessary, e.g. blood pregnancy test about 1 week before the procedure and urine pregnancy test or the second blood test on the day of the treatment. A written statement of sexual abstinence over the whole period of the procedure should be considered as necessary.
In our opinion MR-HIFU offers an attractive alternative to traditional methods of UF treatment.
Acknowledgement
This patient took a part in a study on MR-HIFU use to treat uterine fibroids which had the Local Bioethics Committee Approval and informed written consent was obtained from the participant.
This study followed the principles of the Declaration of Helsinki.
The occurrence of this case has been mentioned during the presentation about experiences with uterine fibroid MR-HIFU therapy in Poland. 4th European Focused Ultrasound Charitable Society (EUFUS) Symposium – Leipzig, October 26–27, 2017.
Disclosure statement
All authors declare no conflict of interest.
Data availability statement
The data used to support the findings of this study are available from the corresponding author upon request.
Additional information
Funding
References
- Stewart EA, Cookson CL, Gandolfo RA, et al. Epidemiology of uterine fibroids: a systematic review. BJOG. 2017;124(10):1501–1512.
- Stewart EA, Laughlin-Tommaso SK, Catherino WH, et al. Uterine fibroids. Nat Rev Dis Primers. 2016;2:16043.
- O'Sullivan M, Overton C. Tailor management to the patient with fibroids. Practitioner. 2017;261(1802):19–22.
- Czuczwar P, Stepniak A, Milart P, et al. Comparison of the influence of three fibroid treatment options: supracervical hysterectomy, ulipristal acetate and uterine artery embolization on ovarian reserve - an observational study. J Ovarian Res. 2018;11(1):45.
- Carranza-Mamane B, Havelock J, Hemmings R, et al. The management of uterine fibroids in women with otherwise unexplained infertility. J Obstet Gynaecol Can. 2015;37(3):277–285.
- Schlesinger D, Benedict S, Diederich C, et al. MR-guided focused ultrasound surgery, present and future. Med Phys. 2013;40(8):080901.
- Fischer K, McDannold NJ, Tempany CM, et al. Potential of minimally invasive procedures in the treatment of uterine fibroids: a focus on magnetic resonance-guided focused ultrasound therapy. Int J Womens Health. 2015;7:901–912.
- Liu X, Xue L, Wang Y, et al. Vaginal delivery outcomes of pregnancies following ultrasound-guided high-intensity focused ultrasound ablation treatment for uterine fibroids. Int J Hyperthermia. 2018;35(1):510–517.
- Munro MG, Critchley HO, Broder MS, Disorders FWGoM, et al. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynaecol Obstet. 2011;113(1):3–13.
- Funaki K, Fukunishi H, Funaki T, et al. Magnetic resonance-guided focused ultrasound surgery for uterine fibroids: relationship between the therapeutic effects and signal intensity of preexisting T2-weighted magnetic resonance images. Am J Obstet Gynecol. 2007;196(2):184 e1–6.
- Ji Y, Hu K, Zhang Y, et al. High-intensity focused ultrasound (HIFU) treatment for uterine fibroids: a meta-analysis. Arch Gynecol Obstet. 2017;296(6):1181–1188.
- Chen J, Chen W, Zhang L, et al. Safety of ultrasound-guided ultrasound ablation for uterine fibroids and adenomyosis: a review of 9988 cases. Ultrason Sonochem. 2015;27:671–676.
- Kroncke T, David M. Magnetic resonance guided focused ultrasound for fibroid treatment-results of the second radiological gynecological expert meeting. Rofo. 2015;187(6):480–482.
- Clark NA, Mumford SL, Segars JH. Reproductive impact of MRI-guided focused ultrasound surgery for fibroids: a systematic review of the evidence. Curr Opin Obstet Gynecol. 2014;26(3):151–161.
- Zou M, Chen L, Wu C, et al. Pregnancy outcomes in patients with uterine fibroids treated with ultrasound-guided high-intensity focused ultrasound. BJOG. 2017;124(Suppl 3):30–35.