Abstract
Purpose
To evaluate endopelvic fascial swelling in patients with uterine fibroids after high-intensity focused ultrasound (HIFU) ablation on magnetic resonance imaging (MRI) and investigate the factors that influence endopelvic fascial swelling.
Methods
MRI and clinical data from 188 patients with uterine fibroids who were treated with HIFU were analyzed retrospectively. The patients were divided into a fascial swelling group and a non-swelling group, and the degree of swelling was graded. Fascial swelling was set as the dependent variable, and factors such as baseline characteristics and HIFU parameters, were set as the independent variables. The relationship between these variables and fascial swelling was analyzed by univariate and multivariate analyses. Correlations between the factors and the degree of fascial swelling were evaluated by Kruskal–Wallis test.
Results
The univariate analysis revealed that the fibroid location, distance from the fibroid to the sacrum, sonication time, treatment time, treatment intensity, therapeutic dose (TD), and energy efficiency (EEF) all affected the endopelvic fascial swelling (p < 0.05). Subsequently, multivariate analysis showed that the distance from the fibroid to the sacrum was significantly correlated with fascial swelling (p < 0.05). Moreover, TD and sonication time were significantly positively correlated with the degree of fascial swelling (p < 0.05). The incidence of sacrococcygeal pain was significantly correlated with fascial swelling (p < 0.05).
Conclusion
The distance from the fibroid to the sacrum was a protective factor for fascial swelling. TD and sonication time were significantly positively correlated with the degree of fascial swelling.
1. Introduction
Uterine fibroids are common benign tumors among women of reproductive age that impair their health and quality of life [Citation1]. The prevalence of uterine fibroids increases with age, and they may be present in over 70% of the premenopausal population [Citation2,Citation3]. Conventional treatment comprises laparoscopic or hysteroscopic myomectomy and hysterectomy. However, myomectomy is limited by the size and location of the fibroid, is associated with complications, such as uterine rupture, and has a high recurrence rate. Moreover, hysterectomy is not suitable for women who have a desire for future fertility. Therefore, the treatment of uterine fibroids has gradually progressed from conventional techniques to minimally invasive or noninvasive techniques to avoid complications, such as urinary incontinence, pelvic adhesions, and premature ovarian failure [Citation4–6]. The application of HIFU, which is a noninvasive modality, for the treatment of uterine fibroids is consistent with this trend. Moreover, MRI has been used as a routine imaging method after HIFU ablation for efficacy assessment.
The principle of HIFU is to bring a high-intensity ultrasound beam to a tight focus deep within the tissue, which raises the temperature of the target area rapidly to between 60 °C and 100 °C within 0.5–1.0 s, causing coagulative necrosis of the target [Citation7]. However, adjacent thermal damage may occur during HIFU ablation and can include lower abdominal pain, sacrococcygeal pain and lower limb paresthesia. According to previous studies, signals changes were observed on T2-weighted imaging (T2WI) of the abdominal wall and sacrum on postoperative MRI [Citation8,Citation9]. In clinical practice, endopelvic fascial swelling has often been observed on postoperative MRI, in which a high-intensity signal is exhibited on T2WI. Under normal circumstances, the endopelvic fascia appears with a stripe-like low-intensity signal on T2WI, which is difficult to observe. The pelvic plexus, which is formed by the hypogastric nerve, pelvic splanchnic nerve and sacral splanchnic nerve, converges at the bottom of the rectum and is covered by the endopelvic fascia [Citation10,Citation11]. Nerve damage in patients with uterine fibroids after HIFU ablation may be correlated with endopelvic fascial swelling.
Endopelvic fascial swelling is a serious issue needs to be addressed. However, no specific investigations have explored endopelvic fascial swelling during HIFU ablation of uterine fibroids. Therefore, the goal of the present study was to evaluate endopelvic fascial swelling on postoperative MRI and further investigate the factors that influence endopelvic fascial swelling. These results are likely to lead to improved pre-HIFU assessment procedures, better predictions of treatment risk factors and better postoperative care.
2. Materials and methods
2.1. Patients and enrollment
A total of 134 patients with uterine fibroids who received HIFU treatment at the First Affiliated Hospital of Chongqing Medical University from January 2017 to August 2018 were included in this study, which was approved by the Institutional Review Board of Chongqing Medical University. Written informed consent was provided by all patients before treatment. The inclusion and exclusion criteria for HIFU therapy are listed in . The baseline characteristics and treatment parameters were collected for all patients. The baseline characteristics included age, the maximal diameter of the fibroid, the volume of the fibroid, the uterine position (anteverted, mid-position or retroverted), the fibroid type (intramural, subserosal, submucosal or transmural), the distance from the fibroid to the sacrum, the location (anterior, lateral or posterior wall), T2WI characteristics (hypointense, isointense, heterogeneous or markedly homogeneous hyperintense) of the fibroid and the degree of enhancement (slight, intermediate or progressive). The treatment parameters included sonication power, sonication time, treatment time, treatment intensity, therapeutic dose (TD), energy-efficiency factor (EEF), negative predictive value (NPV), and NPV ratio.
Table 1. Inclusion and exclusion criteria.
2.2. HIFU ablation
The treatment was performed with an US-guided HIFU tumor therapeutic system (Model-JC Focused Ultrasound Tumor Therapeutic System, Chongqing Haifu Medical Technology Co, Ltd., Chongqing, China). The transducer was 20 cm in diameter and had an operating frequency of 0.8 MHz, a power range of 0–400 W and a focal length of 15 cm; the dimensions of the focal region were 1.5 × 1.5 × 10 mm. The integrated transducer was controlled by a computer and was fixed in a sac filled with degassed water and could be moved smoothly in six directions. During treatment, an adjustable degassed water balloon was placed between the transducer and the skin anterior to the treated area to push away the bowel in the acoustic pathway.
The patient was placed in a prone position on the HIFU bed with the abdominal wall in contact with the degassed water in the tank, and the water temperature was set below 15 °C. In addition, a degassed water balloon was placed between the transducer and the anterior abdominal wall. HIFU was performed under intravenous sedation using fentanyl and midazolam hydrochloride. During the whole course of therapy, real-time ultrasonography was used to conform the location of the target area and the adjacent tissue. The patient remained conscious and was able to report any discomfort or pain during the treatment procedure, which was recorded. The sonication power was adjusted according to feedback from the patient and grayscale changes on the ultrasonographic image. When all signs of blood flow disappeared or a grayscale change in the target tissue was observed on color Doppler ultrasound, treatment was terminated. The sonication power, sonication time, treatment time, treatment intensity (s/hour), TD, EEF (mm3/s, ablated fibroid volume per second), NPV and NPV ratio were recorded.
According to the classification system of the Society of Interventional Radiology (SIR) [Citation12], the severity of complications, including lower abdominal pain, sacrococcygeal pain, lower limb paresthesia, and vaginal discharge, was recorded. The severity of complications was evaluated as follows: (1) class A: no therapy, no consequence; (2) class B: nominal therapy or no consequence, including overnight admission for observation only; (3) class C: therapy and minor hospitalization (<48 h) required; (4) class D: major therapy required, including an unplanned increase in the level of care or prolonged hospitalization (>48 h); (5) class E: permanent adverse sequelae; and (6) class F: death.
2.3. MRI evaluation
MRI was performed on a GE 3.0T MRI system (General Electric Company, Chicago, IL, USA). Standard T1-weighted imaging (T1WI) (repetition time/echo time (TR/TE), 600/10 ms; slice thickness, 6 mm; matrix size, 180 × 384 mm; NEX, 1), T2WI (TR/TE, 3280/105 ms; slice thickness, 6 mm; matrix size, 256 × 288 mm; NEX, 2), and enhanced-weighted imaging (TR/TE, 3.9/1.8; TI, 5.0 ms; slice thickness, 2 mm; matrix size, 256 × 288 mm; slab 50 cm) were performed prior to and 1–2 days after HIFU ablation.
The images were reviewed by two experienced radiologists. If there was a discrepancy, the chief doctor of the department evaluated the findings, and the chief’s decision was considered final. The volume of each fibroid was measured in three dimensions, longitudinal (d1), anteroposterior (d2) and transverse (d3), using the formula V = 0.5233 × d1 × d2 × d3 [Citation13]. The three dimensions of the nonperfused area were measured in the contrast-enhanced MR images, and the observation indices were calculated based on the treatment parameters, including the total energy (J, the energy required to treat the entire fibroid), EEF (J/cm3, the energy required to ablate the fibroid per unit volume), the treatment intensity (s/mm3, the sonication time required to ablate the fibroid per unit volume), and the NPV ratio (the ratio of NPV-to-fibroid volume). In all, 188 patients were divided into a fascial swelling group and a non-swelling group, and the severity of fascial swelling was evaluated. Endopelvic fascial swelling occurring in only one region was scored as degree 1, while fascial swelling occurring in two regions was scored as degree 2. Endopelvic fascial swelling occurring in four or more than regions was scored as degree 4.
2.4. Statistical analysis
Statistical analyses were performed using SPSS 24.0 (IBM, Chicago, IL). Normally distributed data are reported using the mean ± standard deviation; data with a skewed distributed are reported using the median and the interquartile range. Endopelvic fascial swelling was considered a dependent variable, and patient baseline characteristics and treatment parameters were considered covariates. The different influencing factors were subjected to univariate analysis. Age, the maximal diameter of the fibroid, the volume of the fibroid, and the distance from the fibroid to the sacrum were assessed by independent-samples t tests. Qualitative (uterine position, type of fibroid, location of the fibroid), T2WI and degree of enhancement data were assessed by the χ2 test. Treatment parameters (TD, EEF, NPV, treatment efficiency and NPV ratio) were assessed by independent-samples t tests or rank-sum tests. Significant independent variables were further evaluated by multivariate binary logistic regression analysis. Collinearity statistics were checked to determine the existence of multi collinearity (if two or more independent variables in a regression model are highly correlated, collinearity is accrued). The endopelvic fascia was divided into the fascia around the rectum and the four side walls of the pelvis, and the posterior fascia was the Waldeyer fascia. The degree of endopelvic fascial swelling was graded according to the extent of swelling. The correlation between the location of the fibroid, TD, sonication time and degree of endopelvic fascial swelling was assessed by the Kruskal–Wallis test. A p value below .05 was considered statistically significant.
3. Results
3.1. Baseline characteristics of the patients with uterine fibroids
A total of 188 females were successfully treated with only a single session, and they were divided into two groups: 128 patients with endopelvic fascial swelling (68.09%) and 60 patients without endopelvic fascial swelling (31.91%). In all, 57 patients and 42 patients were degree 1 and degree 2, respectively, while 29 patients were degree 3 or above.
The average age of the 188 patients was 40.5 ± 6.5 years (range, 23–53). The mean maximal diameter and volume of the fibroid were 5.75 ± 1.03 cm and 113.25 ± 68.14 cm3, respectively. Swelling of the endopelvic fascia was characterized by a low-intensity signal on T1WI, a high-intensity signal on T2WI and a high-intensity signal on enhanced imaging ( and ). The location of the fibroid and the distance from the fibroid to the sacrum were significantly associated with fascial swelling (p < 0.05), while the patients’ age, maximal fibroid diameter, fibroid volume, uterine location, type of subcutaneous fibroid, fat thickness, T2WI features, degree of enhancement were not significantly different between the two groups ().
Figure 1. Patient number 13, 36 years old. (A–C) MR images before HIFU treatment; (D–F) MR images after HIFU treatment. A sagittal T2-weighted image (A) demonstrates anterior wall fibroids (triangle) that are almost hypointense on T2-weighted scans; (C) is a diffusion-weighted image. Fascial swelling has a stripe-like high-intensity signal (long arrow).
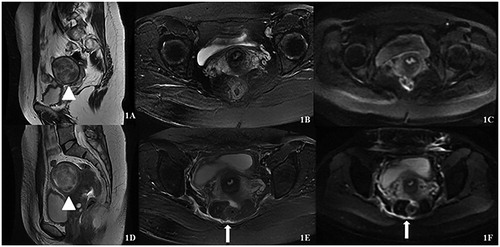
Figure 2. Patient number 125, 39 years old. (A–C) MR images before HIFU treatment; (D–F) MR images after HIFU treatment. A sagittal T2-weighted image (A) demonstrates anterior wall fibroids (triangle) that are almost hypointense on T2-weighted scans; (C) is a diffusion-weighted image. Fascial swelling has a stripe-like high-intensity signal (long arrow).
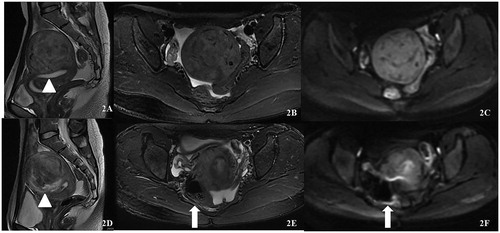
Table 2. Univariate analysis to evaluate the relationship between the endopelvic fascial swelling and the features of fibroids.
3.2. Relationships between endopelvic fascial swelling and treatment parameters
The median average TD delivered was 354,796 J in the swelling group and 227,900 J in the non-swelling group. The sonication time, which represents the sum of the time required for all sonications used during the entire HIFU procedure, was 888 s in the swelling group and 584 s in the non-swelling group. shows that sonication time, treatment time, treatment intensity, TD and EEF were highly correlated with pelvic swelling (p < 0.05), while sonication power, NPV and the NPV ratio were not. Moreover, the maximal diameter of uterine fibroids, T2WI features and degree of enhancement were correlated with TD and EEF (p < 0.05). In addition, the statistical analysis results showed that the maximal diameter of fibroid, signal intensity on T2W1, degree of enhancement on T1WI all had significant relationship with TD (p < 0.05).
Table 3. Univariate analysis to evaluate the relationship between the endopelvic fascial swelling and ultrasound ablation parameters.
3.3. Correlations among fibroid characteristics, treatment parameters and endopelvic fascial swelling
Significant factors in the univariate analysis were further evaluated by multivariate binary logistic regression analysis. Spearman correlation analysis showed that the sonication time was collinear with TD, EEF, treatment time and treatment intensity. The treatment time was collinear with TD and EEF, so the sonication time, treatment time and treatment intensity were removed. Finally, the location of the fibroid, distance from the fibroid to the sacrum, TD and EEF were included in the collinear diagnosis. shows that the distance from the fibroid to the sacrum (p = 0.000, OR = 1.090, 95% CI = 1.054 to 1.127) was significantly associated with endopelvic fascial swelling.
Table 4. Multivariable binary logistic regression analysis to evaluate the correlation of fascial swelling with the significant factors of univariate analysis.
3.4. Correlation between the location of the fibroid and quantitative factors (TD, sonication time, EEF and the distance from the fibroid to the sacrum) and the degree of endopelvic fascial swelling
In the analysis performed in this study, showed that there were no significant correlations between the location of the fibroid and the degree of endopelvic fascial swelling. There were significant positive correlations between the TD, sonication time and degree of endopelvic fascial swelling (p < 0.05), whereas there were no significant correlations between the EEF and the distance from the fibroid to the sacrum and the degree of endopelvic fascial swelling in .
Table 5. Correlation between the location of the fibroid and the degree of endopelvic fascial swelling.
Table 6. Correlation among the quantitive factors (TD, sonication time, EEF and the distance from the fibroid to the sacrum) and the degree of endopelvic fascial swelling.
3.5. Adverse events
According to the international SIR criteria, the adverse event classifications are shown in . Adverse events were classified as class A or B; no class C, E or F events occurred in this study. The main adverse events were lower abdominal pain, sacrococcygeal pain, lower limb paresthesia and vaginal discharge. Among the class A events, the incidence rates of lower abdominal pain and sacrococcygeal pain were 46.1% and 38.3%, respectively, in the swelling group and 45.0% and 16.0%, respectively, in the non-swelling group. The incidence of sacrococcygeal pain in the swelling group was higher than that in the non-swelling group (p = 0.000). A total of 11 and 5 patients suffered from lower limb paresthesia, and 12 and 7 patients reported vaginal discharge in the swelling and non-swelling groups, respectively. Among the class B events, the incidence rates of lower abdominal pain and sacrococcygeal pain were 32.0% and 18.0%, respectively, in the swelling group and 18.0% and 11.7%, respectively, in the non-swelling group. Seven and 4 patients suffered from lower limb paresthesia, and 9 and 6 patients reported vaginal discharge in the swelling and non-swelling groups, respectively.
Table 7. Summary of postoperative adverse events.
4. Discussion
In the present study, all the operations in this study were performed by experienced operators in strict accordance with the standards, and all the treatments achieved satisfactory efficiency. The mean NPV ratio was 86.3 ± 47.4% immediately after the treatment, similar with previous studies [Citation8,Citation14]. Endopelvic fascial swelling was observed on postoperative MRI in 128 patients (68.09%) and exhibited well-defined low-intensity signals on T1WI and high-intensity signals on T2WI. In the univariate analysis, the location of the fibroid was correlated with endopelvic fascial swelling, consistent with a recent study [Citation15]. In the present study, more factors were observed by MRI, and factors that influence endopelvic fascial swelling were comprehensively analyzed.
According to the univariate analysis, we found that the location of the fibroid showed a significant correlation with endopelvic fascial swelling and the distance from the fibroid to the sacrum was an independent protective factor in the multivariate analysis. Zhong et al. [Citation16] reported that compared with the lesions located in superficial regions, deeper lesions required more energy to achieve the same volume of necrotic tissue because of the absorption, reflection, and scattering of ultrasound waves in the acoustic pathway and can eventually induce ultrasonic energy attenuation with an increasing amount of tissue in front of the focus. The deeper the target tissue was, the more energy that was required to ablate the same volume of tissue in vitro with equal effects. The ultrasonic energy required to ablate the same unit volume of target tissue was positively correlated with the focus depth. A greater travel distance for HIFU beams from the transducer to the target lesion corresponded to a more complex ultrasound-tissue interaction, thereby increasing the risk of adverse effects. Fibroids in the posterior wall are close to the sacrum, which reflects ultrasound and deposits ultrasonic heat, causing obvious thermal injury. The incidence of endopelvic fascial swelling can be effectively reduced by ensuring a safe distance from the fibroid to the sacrum. Recent studies [Citation17,Citation18] reported that, during HIFU ablation, energy deposition in tissue is influenced by the cooling effect of blood flow due to ultrasonic heating, which can quickly remove heat and decrease local temperatures; thus, ultrasound energy is not easily deposited in progressive enhancement fibroids because there are more cells, less collagen fiber, and lower-density fibroids. Therefore, the blood supply of uterine fibroids is related to the degree of difficulty of HIFU ablation. Operators need to increase the temperature at the target area by increasing the TD and sonication time. In the present study, we found that TD was affected by the fibroid’s size, T2WI features and the degree of enhancement, which was consistent with previous studies [Citation19]. The more energy that is used to achieve the ablation, the more energy will be potentially deposited in the abdominal wall structures along the ablation pathway, and the greater the risk of thermal injury. However, the fibroid’s size, T2WI features and the degree of enhancement had no significant correlations with endopelvic fascial swelling. During HIFU ablation, the tissue in acoustic pathway, such as endopelvic fascia and bladder, also absorbs the sound energy to produce temperature rising effect. Ultrasound produces physical effects such as reflection and refraction at the interface of various biological tissues. The reflective interface may have energy deposition or the presence of ectopic small focal points, causing secondary focusing of the ultrasound to cause thermal damage to the tissue outside the target area, which is the major cause of endopelvic fascial swelling after HIFU treatment and the distance from the fibroid to the sacrum is the most influencing factors.
In the present study, endopelvic fascial swelling occurred around the uterus, sacrum, bladder and rectum, while the fascia in the anterior wall and the Waldeyer fascia were the predicted sites.When used to ablate deep fibroids, ultrasound beams can be absorbed and reflected by tissues in the acoustic pathway, bowel and sacrum, which can result in fascial swelling and damage to the sacrum nerves, leading to sacrococcygeal pain. The present study showed that sonication time not only was related to the occurrence of endopelvic fascial swelling but also determined the degree of fascial swelling, while TD was correlated with endopelvic fascial swelling. It is necessary for sonication time and TD to be combined in different methods to evaluate their synergistic effects [Citation9]. Yang et al. [Citation20] used HIFU combined with intratumoral ethanol to effectively reduce the TD output, increasing the overall ablation efficiency. Fascial swelling can be effectively reduced by detailed treatment protocols before performing and adjusting therapeutic parameters under the premise of ensuring the ablation effect during HIFU ablation.
According to the present results, the distance from the fibroid to the sacrum was only a protective factor and was related to the occurrence of fascial swelling; however, this distance was not correlated with the degree of fascial swelling. The safety margin or distance from the border of the fibroid to be treated in the sacrum should be taken into consideration [Citation21]. Therefore, a patient whose fibroids are close to the lumbosacral plexus or to the surface of another bone should be carefully evaluated before being deemed suitable for MRI-guided HIFU treatment.
Endopelvic fascial swelling was observed on postoperative MRI, and sacrococcygeal pain occurred during HIFU ablation. During follow-up, adverse events including sacrococcygeal pain and lower limb paresthesia were relieved within one week, and a gradual reduction was observed in fascial swelling, demonstrating that it can spontaneously recover. However, it is necessary to avoid fascial swelling, which is correlated with adverse effects, including sacrococcygeal pain. The limitations of this retrospective study are that this study is a single center analysis, and we enrolled a small sample size. The present study explored influencing factors of occurrence and the degree of endopelvic fascial swelling in patients with uterine fibroids, and the fascial swelling will be further quantified.
Conclusion
The present study has shown that postoperative MRI can be used to effectively observe and evaluate endopelvic fascial swelling. Based upon multivariable binary logistic regression, the results show that the distance from the fibroid to the sacrum was an important factor that predicted the presence of endopelvic fascial swelling during HIFU ablation and that there were significant positive correlations among TD, sonication time, and the degree of endopelvic fascial swelling.
Disclosure statement
The authors have no conflicts of interest to declare. The authors alone are responsible for the content and writing of the paper.
Data availability statement
The data that support the findings of this study are available from the corresponding author Zhang upon reasonable request.
Additional information
Funding
References
- Juhasz-Boss I, Jungmann P, Radosa J, et al. Two novel classification systems for uterine fibroids and subsequent uterine reconstruction after myomectomy. Arch Gynecol Obstet. 2017;295:675–680.
- Day Baird D, Dunson DB, Hill MC, et al. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188:100–107.
- Elizabeth S. Clinical practice. Uterine fibroids. N Engl J Med. 2015;372:1646–1655.
- Marinova M, Rauch M, Schild H, Strunk HM. Novel non-invasive treatment with high-intensity focused ultrasound (HIFU). Ultraschall in Med. 2016;37:46–55.
- Melody T, Laura G, Callum P, et al. Nonresective treatments for uterine fibroids: a systematic review of uterine and fibroid volume reductions. Int J Hyperther. 2019;36:295–301.
- Peng S, Xiong Y, Li K, et al. Clinical utility of a microbubble-enhancing contrast (“SonoVue”) in treatment of uterine fibroids with high intensity focused ultrasound: a retrospective study. Eur J Radiol. 2012;81:3832–3838.
- Chen L, ter Haar G, Hill CR. Influence of ablated tissue on the formation of high-intensity focused ultrasound lesions. Ultrasound Med Biol. 1997;23:921–931.
- Yin N, Hu L, Xiao Z-B, et al. Factors influencing thermal injury to skin and abdominal wall structures in HIFU ablation of uterine fibroids. Int J Hyperther. 2018;34:1298–1303.
- Cun JP, Fan HJ, Zhao W, et al. Factors influencing MR changes associated with sacral injury after high-intensity focused ultrasound ablation of uterine fibroids. Int J Hyperther. 2019;36:21–28.
- Petros M, John ES. Surgical anatomy of the retroperitoneal spaces, part IV: retroperitoneal nerves. Am Surg. 2010;76:253–262.
- Dellon AL, Wright EJ, Manson PN. Chronic pelvic pain after laser prostatectomy: treatment by resection of the perineal branches of the pudendal nerve. J Reconstr Microsurg. 2014;30:547–550.
- Cardella JF, Kundu S, Miller DL, et al. Society of interventional radiology clinical practice guidelines. J VascInterv Radiol. 2009;20:5189–5191.
- Orsini LF, Salardi S, Pilu G, et al. Pelvic organs in premenarcheal girls: real-time ultrasonography. Radiology. 1984;153:113–116.
- Chen J, Li Y, Wang Z, et al. Evaluation of high-intensity focused ultrasound ablation for uterine fibroids: an IDEAL prospective exploration study. Bjog: Int J Obstet Gy. 2018;125:354–364.
- Zhang XH, Zhai SH, Dong GL, et al. MRI evaluating changes of pelvic fascia after high intensity focused ultrasound ablation of uterine fibroids. Chin J Med Imaging Technol. 2017;33:1540–1544.
- Liu ZQ, Gong C, Liu YC, et al. Establishment of a scoring system for predicting the difficulty level of high-intensity focused ultrasound ablation of uterine fibroids. Int J Hyperther. 2018;34:77–86.
- Peng S, Zhang L, Hu L, et al. Factors influencing the dosimetry focused ultrasound ablation of for high-intensity uterine fibroids. Medicine (Baltimore). 2015;94:e650.
- Kim YS, Lee JW, Choi CH, et al. Uterine fibroids: correlation of T2 signal intensity with semiquantitative perfusion MR parameters in patients screened for MR-guided high intensity focused ultrasound ablation. Radiology. 2016;278:925–935.
- Duc NM, Keserci B. Review of influential clinical factors in reducing the risk of unsuccessful MRI-guided HIFU treatment outcome of uterine fibroids. Diagn Interv Radiol. 2018;24:283–291.
- Yang Z, Zhang Y, Zhang R, et al. A case-control study of high-intensity focused ultrasound combined with sonographically guided intratumoral ethanol injection in the treatment of uterine fibroids. J Ultrasound Med. 2014;33:657–665.
- Liu YC, Zhang WY, He M, et al. Adverse effect analysis of high-intensity focused ultrasound in the treatment of benign uterine diseases. Int J Hyperther. 2018;35:56–61.
