Abstract
Objective
To compare the oncological outcomes between microwave ablation (MWA) and surgical resection (SR) in patients with ovarian cancer liver metastasis (OCLM).
Materials and methods
In this retrospective study, a total of 29 female patients (mean age, 47.8 ± 12.9 years; range, 21–65 years) diagnosed with forty-three OCLM nodules between September 2008 and July 2016 were included. All patients with ovarian cancer received chemotherapy and cytoreductive surgery (CRS). Fifteen patients with 22 nodules underwent MWA, and 14 patients with 21 nodules underwent SR. Overall survival (OS), local tumor recurrence-free survival (LTRS), and operation-related parameters were compared between the two groups. Multivariate analyses were performed on clinicopathological variables to identify factors affecting OS and LTRS.
Results
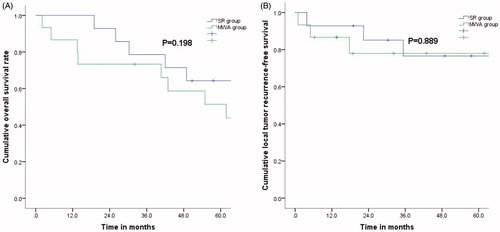
The median follow-up time was 70.2 months (range, 12.1–107.2 months). Fourteen patients died during this period. The 1-, 3-, and 5-year OS and LTRS rates after MWA were comparable to those after SR (p = .198 and p = .889, respectively). Compared with the SR group, the MWA group had a shorter surgical time (p < .001), less estimated blood loss (p < .001), shorter postoperative hospitalization (p < .001) and fewer costs (p = .015). The multivariate analysis showed that old age (p = .001) was a predictor of poor OS and that intrahepatic tumor size (p = .005) and intrahepatic tumor number (p = .001) were predictors of poor LTRS.
Conclusion
Percutaneous MWA had comparable oncologic outcomes with those of SR and could be a safe and effective treatment for OCLM.
Introduction
Ovarian cancer (OC) is the sixth most commonly occurring cancer among women globally and one of the prominent reasons for cancer-associated fatality [Citation1,Citation2]. Despite advancements in both diagnosis and treatments, including surgical resection (SR) and chemotherapy, the number of deaths continues to increase in a stepwise manner due to tumor progression and metastasis [Citation3]. Extraovarian metastasis through the intraperitoneal route of dissemination has been validated as the most typical pattern of extraovarian tumor spread. Moreover, OC can be transferred to distant organs (i.e., the liver, bone or lung) through blood circulation at the time of diagnosis [Citation4]. A great number of studies have demonstrated that liver metastasis (LM) originating from OC may be more prevalent than estimated, and metastasis is detected in nearly 1/2 of all patients at autopsy [Citation5]. In addition, the occurrence of ovarian cancer liver metastases (OCLM) results in a relatively poor prognosis, with a median survival time ranging from 3 to 12 months [Citation6]. Therefore, choosing an optimal treatment for LM is vitally important for patients with OC.
As a promising ablation modality, microwave ablation (MWA) has been frequently reported in terms of its therapeutic effectiveness [Citation7–10]. Compared with radiofrequency ablation (RFA), MWA is related to several speculative benefits, including a shorter operation time, a larger ablation volume, a higher intratumoral temperature, and less reliance on the electrical conductivities of tissues, showing comparable efficacy to hepatic resection. In recent years, image-guided thermal ablation has been utilized to treat several metastatic tumors [Citation11–13]. However, studies on OCLM that accept thermal ablation are rare. Liu et al. documented the technique effectiveness and survival outcomes of percutaneous RFA for OCLM in 11 patients, with 1-, 3-, and 5-year overall survival (OS) rates of 100%, 61% and 61%, respectively [Citation14].
SR can prolong survival for patients with OCLM, but its implementation is frequently limited by poor liver function and multiple tumor recurrence. Hepatic surgeons are responsible for assisting gynecologists in improving the prognosis of patients. Wang et al. reported that the OS time of patients with OCLM who received R0 laparoscopic liver resection (LR) was 50.1 months, which was significantly higher than that of patients who received non-R0 LR (20.0 months) when the primary OC received cytoreductive surgery (CRS) [Citation15].
To our knowledge, no comparison of these two therapies for OCLM has been reported. Therefore, we investigated percutaneous MWA and SR for OCLM in terms of technical effectiveness, oncologic outcomes, and complications. The purpose of this study was to review the intermediate-term effectiveness of MWA versus SR in the management of OCLM and to identify prognostic factors associated with these two techniques.
Materials and methods
This retrospective study was performed according to the principles of the Declaration of Helsinki. The protocol was approved by the ethics committee of Sun Yat-sen University Cancer Center (Guangzhou, China). Because of the retrospective nature of this study, patient consent for inclusion was waived.
Patients
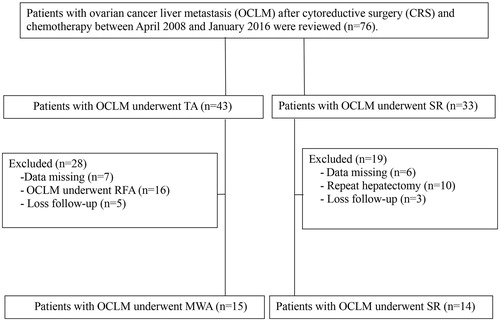
The medical records of all patients with OCLM after chemotherapy and CRS were reviewed between September 2008 and July 2016. Among them, 29 consecutive patients (mean age, 47.8 ± 12.9 years; range, 21–65 years) with forty-three OCLM nodules underwent either computed tomography (CT)-guided percutaneous MWA (n = 15) or SR (n = 14) and were included in this study according to the following criteria: (a) patients with a Child-Turcotte-Pugh (CTP) grade of A or B; (b) patients with an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or A; and (c) patients with up to five liver metastases, each <5 cm in diameter. The exclusion criteria were as follows: (a) severe clinical comorbidities such as heart, lung and renal diseases; (b) extreme coagulation conditions; (c) OCLM patients did not receive other treatments before SR or MWA; and (d) the follow-up time was <12 months. presents the patient enrollment procedure.
Figure 1. Flow diagram shows exclusion criteria in patients with ovarian cancer liver metastasis (OCLM).
OCLM was diagnosed based on a history of OC combined with typical imaging findings, that is, peritumoral enhancement in arterial-phase and hypoenhancing on dynamic images. For patients in the SR group, the OCLM diagnosis was established by postoperative histopathology. For patients in the MWA group, the OCLM diagnosis was confirmed by pathologic outcomes of needle biopsy samples. Explanations for selecting MWA over SR were as follows: (1) elevated risk for resection related to a difficult location or old age; (2) insufficient liver function; (3) refusal of general anesthesia; and (4) the patients were unwilling to undergo surgical treatment.
The following parameters were acquired from each patient: age, maximum tumor diameter, tumor number, tumor location, CTP grade, histologic type, previous treatments, and detection of LM. In addition, a laboratory examination (i.e., carbohydrate antigen [CA]-125, alanine transaminase [ALT], and aspartate transaminase [AST]) related to hepatic function was performed before and after the operation. The procedural or treatment variables acquired were as follows: operation time, projected blood loss, postoperative hospital stay, cost, date and site of metastasis, and date of and status at the last follow-up. The reasons for death were also recorded.
MWA procedure
A 64-slice spiral CT scanner (SOMATOM 64 Sensation, Siemens, Germany) was utilized to guide MWA puncture and acquire images. A KY2000 MWA system (Kangyou Medical Instruments, China) comprising two autonomous MW generators, two flexible coaxial cables plus two water-pumping machines was used. Before the MWA process, the patient was asked to be in a supine position, and a fine metal marker was placed on the body surface of the target tumor. Patients were placed under deep sedation for this procedure. An un-enhanced CT scan was acquired to confirm the puncture path and target lesion location. If the tumors were showed clearly, preoperative planning can be performed directly, while unclear tumors require intraoperative enhanced CT scans. Following local anesthesia with 1% lidocaine, an antenna was implanted percutaneously into the tumor and positioned at elected sites under CT assistance. For tumors <2.0 cm in size, only one antenna was introduced, whereas for larger tumors, multiple antennae were implanted. Two antennae were utilized concurrently throughout MWA to attain a greater ablation zone. For this procedure, we utilized 50 W for 10 min regularly. Moreover, the microwave needle tract was ablated throughout needle withdrawal.
SR procedure
Hepatic resection was performed by an open approach under general anesthesia. Surgeons with 19–27 years of experience in hepatectomy performed the surgeries. Intraoperative ultrasonography was used routinely to evaluate other possible tumors and the possibility of a negative resection margin. Anatomical resections in the form of segmentectomy and/or subsegmentectomy described by Makuuchi et al. were preferred in the surgeries [Citation16]. The resected specimens were histopathologically examined. According to the guidelines of the International Union Against Cancer (UICC), R0 and R1 resections were defined by the absence (tumor-free margin no <1 mm for all detected lesions) or presence (tumor-free margin of 0 mm) of microscopic tumor invasion of the resection margins [Citation17].
Follow-up
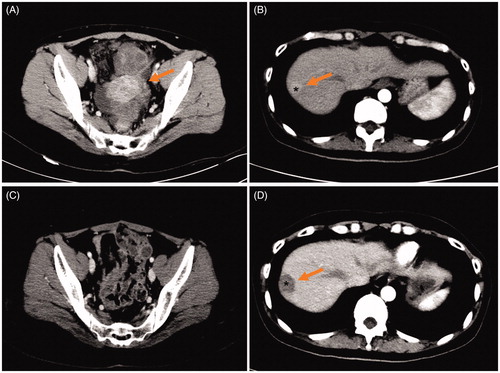
Follow-up was performed one and 3 months after treatment plus at 6-month intervals afterward. The following evaluations were performed: regular physical checkup, laboratory tests and ultrasound (US), CT, or magnetic resonance imaging (MRI). Intervals for CT/MRI were reduced when the levels of tumor markers were elevated following treatment. Technical success was described as the nonappearance of contrast enhancement on imaging in any region of the mass 1 month later. The patients in the SR and MWA groups who underwent preoperative and postoperative CT scans are presented in and , respectively. Local tumor recurrence-free survival (LTRS) was defined based on imaging findings of irregular nodular, scattered, or eccentric patterns of peripheral enhancement around the ablation zone in the MWA group and around the resected margin in the SR group. OS was defined as the date of the first session of MWA or SR to the date of death or the date of the last follow-up (survival or loss). A major complication was defined as an event that led to substantial morbidity and disability that increased the level of care or resulted in hospital admission. Follow-up was completed at the last visit or at the time of death or recurrence.
Figure 2. A 55-year-old woman with solitary ovarian cancer liver metastasis (OCLM). (A) Contrast-enhanced CT shows ovarian cancer (OC) lesions (arrow) located on left ovary in the arterial phase; (B) Contrast-enhanced CT shows OCLM lesion (*, arrow) located on S6 in liver; (C) Contrast-enhanced CT shows OC lesions removed by cytoreductive surgery (CRS) after 1 month (arrow); (D) Contrast-enhanced CT shows OCLM lesion (*, arrow) underwent surgical resection after 4 months.
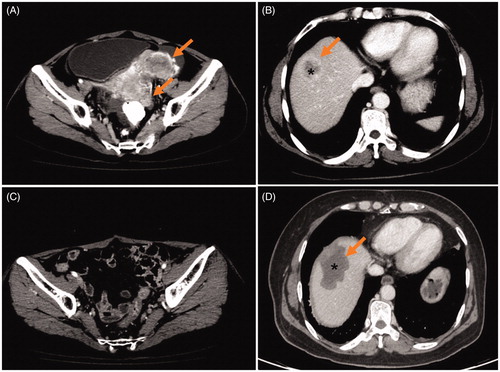
Figure 3. A 48-year-old woman with solitary ovarian cancer liver metastasis (OCLM). (A) Contrast-enhanced CT shows ovarian cancer (OC) lesions (arrow) located on ovary in the arterial phase; (B) Contrast-enhanced CT shows OCLM lesion (*, arrow) located on S7 in liver; (C) Contrast-enhanced CT shows OC lesions removed by cytoreductive surgery (CRS) after 3 months (arrow); (D) Contrast-enhanced CT shows OCLM lesion (*, arrow) underwent microwave ablation (MWA) after 2 months.
Statistical analysis
Data analysis was accomplished by means of SPSS 22.0 (USA). Student’s t-test was utilized to compare the data between the MWA and SR groups. The Wilcoxon signed-rank test (for continuous variables) and Pearson’s chi-squared test or Fisher’s exact test (for categorical variables) were implemented. The Kaplan–Meier method with the log-rank test was utilized to evaluate OS and LTRS. A Cox proportional hazards model was utilized to recognize the substantial impacts of several factors on LTRS or OS. p < .05 was considered statistically significant.
Results
Patient and tumor characteristics
The patient and tumor characteristics are shown in . The mean patient age was 43.2 ± 11.7 years (range, 21–60 years) in the SR group and 50.5 ± 13.2 years (range, 38–65 years) in the MWA group. This result shows that patients in the MWA group were older than those in the SR group (p = .044). The International Federation of Obstetrics and Gynecology (IFOG) stage at the initial diagnosis in the SR group was stage II in four patients, stage III in six patients, and stage IV in the remaining four patients, all of which had coexistent stable extrahepatic metastasis, including celiac metastasis in one patient, pulmonary metastasis in two patients, and peripancreatic metastasis in one patient. The IFOG stage at the initial diagnosis in the MWA group was stage II in four patients, stage III in seven patients, and stage IV in the remaining four patients, all of which had coexistent stable extrahepatic metastasis, including celiac metastasis in two patients and pulmonary metastasis in two patients. These results were comparable between the two groups (p = .572). In the SR group, the mean OCLM size was 3.2 ± 1.2 cm (range, 1.5–5.0 cm). In the MWA group, the mean OCLM size was 3.0 ± 1.4 cm (range, 0.8–5.0 cm). These results were comparable between the two groups (p = .212). In the SR group, solitary OCLM lesions were detected in 9 of 14 patients, whereas multiple OCLM lesions were detected in the remaining 5 patients. In the MWA group, solitary OCLM lesions were detected in 10 of 15 patients, whereas multiple OCLM lesions were detected in the remaining 5 patients. These results were comparable between the two groups (p = .796). In the SR group, papillary serous cystadenocarcinoma was detected in 6 patients, mucus papillary cystadenocarcinoma in 5 patients, endometrioid adenocarcinoma, clear cell adenocarcinoma and germinoma in the remaining patients. In the MWA group, papillary serous cystadenocarcinoma was detected in nine patients, mucus papillary cystadenocarcinoma in five patients, and clear cell adenocarcinoma in one patient. These results were comparable between the two groups (p = .217). In the SR group, CTP grade A was detected in 12 of 14 patients, whereas CTP grade B was detected in the remaining two patients. In the MWA group, CTP grade A was detected in 14 of 15 patients, whereas CTP grade B was detected in the remaining one patient. These results were comparable between the two groups (p = .464). In the SR group, synchronous OCLM was detected in two patients, and metachronous OCLM was detected in 12 patients, with a mean of 52.7 ± 32.1 months and a range of 17.6–88.2. In the MWA group, synchronous OCLM was detected in two patients, and metachronous OCLM was detected in 13 patients, with a mean of 61.8 ± 40.7 months and a range of 21.2–94.3 months. These results were comparable between the two groups (p = .941).
Table 1. Characteristics of patients with OCLM.
Treatment parameters and postoperative outcomes
The treatment parameters and postoperative outcomes are summarized in . Fourteen patients with 21 tumors in the SR group received a total of 24 sessions. Eighteen tumors were successfully treated in one session, and three tumors were successfully treated in two sessions. Fifteen patients with 22 tumors in the MWA group received a total of 24 sessions. Twenty-one tumors were successfully treated in one session, and one tumor was successfully treated in two sessions. The surgical time and hospitalization in the SR group were significantly longer than those in the MWA group (p < .001 and p < .001, respectively). There was more estimated blood loss and costs in the SR group than in the MWA group (p < .001 and p = .015, respectively). One patient in the SR group needed a blood transfusion treatment of 200–400 mL. Transfusion was not necessary in patients in the MWA group.
Table 2. Comparation of treatment parameters and postoperative outcomes between MWA and SR group.
Tumor markers
As a tumor marker of OC, CA-125 results were assessed pre-CRS, post-CRS, preoperation, and postoperation in all patients (). The mean values at four different time points were 923.52 ± 456.25, 17.52 ± 7.62, 18.23 ± 8.23, and 12.11 ± 5.82 U/mL in the SR group, and the mean values at four different time points were 776.15 ± 528.32, 16.92 ± 3.27, 18.11 ± 6.28, and 14.82 ± 4.19 U/mL in the MWA group.
Table 3. Serum CA-125 levels for all the patients at multiple time points.
Changes in hepatic function
The changes in hepatic function are presented in . Before treatment, the AST, ALT, serum albumin, and total bilirubin levels were comparable between the SR and MWA groups (p = .419, p = .324, p = .782, and p = .485, respectively). After treatment, the AST, serum albumin, and total bilirubin levels were comparable between the SR and MWA groups (p = .225, p = .143, and p = .615, respectively). The ALT level was higher in the SR group than in the MWA group (p = .032).
Table 4. Preoperative and postoperative liver function between MWA group and SR group.
Midterm oncologic outcomes
The median follow-up period was 75.0 months (range, 19.0–107.2 months) in the SR group and 66.3 months (range, 12.1–92.5 months) in the MWA group. The mortality rate was 35.7% (five of 14 patients) in the SR group; the causes of death for all patients were OC or LM progression. Four of the patients had comorbid diseases, including hypertension in two patients and diabetes in two patients. Nine patients (60.0%; nine of 15 patients) in the MWA group died, and the cause of death was local OCLM or systemic progression. On the basis of follow-up imaging, a 100% technique success rate was achieved in both groups (SR: 24 of 24 treatments; MWA: 24 of 24 treatments). Four local tumor progression (LTP) lesions (28.6%; four of 14 patients) were detected after SR treatment, and three LTP lesions (20.0%; three of 15 patients) were detected after MWA treatment. The 1-, 3-, and 5-year OS rates in the SR and MWA groups were 100%, 78.6%, and 64.3% and 86.7%, 73.3%, and 51.3%, respectively (), showing no significant difference (p = 0.198). The 1-, 3-, and 5-year LTRS rates in the SR and MWA groups were 92.9%, 76.6%, and 76.6% and 86.7%, 78.0%, and 78.0%, respectively (), showing no significant difference (p = .889).
Complications
Reported deaths were not associated with any treatment. Three main complications (21.4%; three of 14 patients) transpired in the SR group after 24 surgical procedures, comprising two patients who had peritoneal effusion and one patient who had a biliary fistula. Peritoneal effusion results from hepatic decompensation. The reason for the occurrence of a biliary fistula is excessive mechanical injury secondary to surgical instruments, which may cause damage to the major bile ducts. These three patients received effective symptomatic treatment and recovered after one week. None of the major complications occurred in the MWA group after 24 sessions. The overall complication rates for both groups approached significance but were not significantly different (p = .058).
Multivariate analyses for OS and LTRS
The multivariate analysis () showed that the factor that significantly affected OS was age (p = .012; HR: 3.321, 95% CI: 1.494–6.727). The multivariate analysis () also showed that the factors that significantly affected LTRS were intrahepatic tumor size (p = .007; HR: 2.600, 95% CI: 1.102–5.282) and intrahepatic tumor number (p = .002; HR: 0.600, 95% CI: 0.494–0.727).
Table 5. Multivariate analysis of prognostic factors with OS.
Table 6. Multivariate analysis of prognostic factors with LTP.
Discussion
Three-quarters of patients with OC are in the advanced stage at the preliminary diagnosis. Among them, >20% are in stage IV due to insidious tumor advancement [Citation18]. OCLM is regarded as an extremely advanced disease stage, occurring due to poorly controlled principal disease that is generally transported from the initial sites. The liver is the most common organ of distant metastasis of OC, even though its occurrence is extremely low. CRS is well accepted as a first-line treatment in primary OC; however, the clinical importance of the assertive debulking operation for OCLM is still one of the most discussed topics in the field of gynecology [Citation17,Citation19]. Most studies have described that MWA is a safe and efficient treatment for several types of liver metastases, such as colorectal cancer liver metastases, and has received much attention as an alternative method in patients with a poor physical condition and who are inoperable. In general, OCLM is a manifestation of the terminal stage of cancer, which is difficult to control and treat. For younger women with good hepatic function, SR should be an ideal treatment modality for LM. For patients with a poor physical condition, MWA seems to be a more convenient and effective treatment modality for LM.
The optimal treatment for LM after CRS for OC has not been established. The European Association for the Study of the Liver guidelines suggest that SR or thermal ablation might be used to treat LM [Citation20]. MWA might permit a greater ablation zone and higher intratumoral temperatures compared to RFA. Several studies have also reported encouraging results of thermal ablation for OCLM in local tumor control as well as long-term survival [Citation21,Citation22]. We examined the OS and LTRS outcomes for 29 consecutive patients who received SR or MWA. Assessment of the clinical effectiveness and oncologic outcomes between MWA and traditional SR was also accomplished. Under the circumstance of similar hepatic function, compared to SR, MWA had a similar OS rate in patients with OCLM. Technical efficiency and local tumor control were two imperative factors to accomplish outcomes analogous to those after SR. Moreover, the SR group showed favorable OS. MWA treatment resulted in a higher incidence of death; however, 60.0% (9 of 15 patients) of patients died from old age, which may be a leading cause of an unfavorable prognosis.
In our study, patients who underwent MWA had a significantly higher mean age than those who underwent SR. Shorter surgical and hospitalization times, lower costs, less estimated blood loss, and no blood transfusion after MWA were advantageous for reducing perioperative morbidity and complications. Major complications in the MWA group were fewer than those in the SR group, although this difference was not statistically significant. The MWA group had similar preoperative ALT and AST levels but lower immediately postoperative ALT levels compared with the SR group. A large amount of evidence supports the concept that the risk of LTP and OS after MWA or SR are driven by unmodifiable patient- and tumor-related factors [Citation23–27]. The size and number of LM lesions may increase the difficulty of operation and fail to enlarge the safety margin, resulting in poor tumor control. Additionally, old age has always been one of the most important factors influencing patient survival, as confirmed in previous studies [Citation27–29].
The limitation of this study is its retrospective design with a relatively small patient series. First, a limited sample size might have reduced the statistical power in the comparative analysis so that some associations were not detected. Second, the success of MWA was assessed by radiographic findings versus a pathologic margin-free status. Therefore, despite the intermediate follow-up reported, it might take longer to use radiographic techniques to detect MWA failures. Third, the prognosis of patients with OCLM most likely relies upon primary disease progression in the liver and distant metastasis, which are difficult to compare between MWA and SR. Moreover, a comparison of LTRS after both techniques seems to be more understandable by readers. A prospective trial that compares standard procedures with MWA is needed to validate the role of this developing modality in the clinical field.
In conclusion, MWA and SR provided comparable results in terms of technical effectiveness, oncologic outcomes, and complications. The present results suggest and encourage that MWA could be a safe and feasibly effective option in the management of OCLM.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Loizzi V, Rossi C, Cormio G, et al. Clinical features of hepatic metastasis in patients with ovarian cancer. Int J Gynecol Cancer. 2005;15(1):26–31.
- Tempany CM, Zou KH, Silverman SG, et al. Staging of advanced ovarian cancer: comparison of imaging modalities–report from the Radiological Diagnostic Oncology Group. Radiology. 2000;215(3):761–767.
- Fischer OJ, Marguerie M, Brotto LA. Sexual function, quality of life, and experiences of women with ovarian cancer: a mixed-methods study. Sex Med. 2019;7(4):530–539.
- Cormio G, Rossi C, Cazzolla A, et al. Distant metastases in ovarian carcinoma. Int J Gynecol Cancer. 2003;13(2):125–129.
- Rose PG, Piver MS, Tsukada Y, et al. Metastatic patterns in histologic variants of ovarian cancer. An autopsy study. Cancer. 1989;64(7):1508–1513.
- Aletti GD, Podratz KC, Cliby WA, et al. Stage IV ovarian cancer: disease site-specific rationale for postoperative treatment. Gynecol Oncol. 2009;112(1):22–27.
- Liang P, Yu J, Yu XL, et al. Percutaneous cooled-tip microwave ablation under ultrasound guidance for primary liver cancer: a multicentre analysis of 1363 treatment-naive lesions in 1007 patients in China. Gut. 2012;61(7):1100–1101.
- Bhardwaj N, Strickland AD, Ahmad F, et al. Microwave ablation for unresectable hepatic tumours: clinical results using a novel microwave probe and generator. Eur J Surg Oncol. 2010;36(3):264–268.
- Yu J, Yu XL, Han ZY, et al. Percutaneous cooled-probe microwave versus radiofrequency ablation in early-stage hepatocellular carcinoma: a phase III randomised controlled trial. Gut. 2017;66(6):1172–1173.
- Castle SM, Salas N, Leveillee RJ. Initial experience using microwave ablation therapy for renal tumor treatment: 18-month follow-up. Urology. 2011;77(4):792–797.
- Qi C, Yu XL, Liang P, et al. Ultrasound-guided microwave ablation for abdominal wall metastatic tumors: a preliminary study. WJG. 2012;18(23):3008–3014.
- Wei Z, Ye X, Yang X, et al. Efficacy and safety of microwave ablation in the treatment of patients with oligometastatic non-small-cell lung cancer: a retrospective study. Int J Hyperthermia. 2019;36(1):827–834.
- Maciolek KA, Abel EJ, Best SL, et al. Percutaneous microwave ablation for local control of metastatic renal cell carcinoma. Abdom Radiol. 2018;43(9):2446–2454.
- Liu B, Huang G, Jiang C, et al. Ultrasound-guided percutaneous radiofrequency ablation of liver metastasis from ovarian cancer: a single-center initial experience. Int J Gynecol Cancer. 2017;27(6):1261–1267.
- Wang M, Zhou J, Zhang L, et al. Surgical treatment of ovarian cancer liver metastasis. Hepatobiliary Surg Nutr. 2019;8(2):129–137.
- Makuuchi M, Hasegawa H, Yamazaki S. Ultrasonically guided subsegmentectomy. Surg Gynecol Obstet. 1985;161(4):346–350.
- Deraco M, Virzì S, Iusco DR, et al. Secondary cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for recurrent epithelial ovarian cancer: a multi-institutional study. BJOG. 2012;119(7):800–809.
- Nagtegaal ID, Odze RD, Klimstra D, The WHO Classification of Tumours Editorial Board, et al. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2019;76(2):182–188.
- Halkia E, Spiliotis J. The role of cytoreductive surgery and HIPEC in epithelial ovarian cancer. J Buon. 2015;20(Suppl. 1):S12–S28.
- Cornberg M, Tacke F, Karlsen TH. Clinical Practice Guidelines of the European Association for the study of the Liver - Advancing methodology but preserving practicability. J Hepatol. 2019;70(1):5–7.
- Bacalbasa N, Dima S, Brasoveanu V, et al. Liver resection for ovarian cancer liver metastases as part of cytoreductive surgery is safe and may bring survival benefit. World J Surg Onc. 2015;13(1):235.
- Gao W, Guo Z, Zhang X, et al. Percutaneous cryoablation of ovarian cancer metastasis to the liver: initial experience in 13 patients. Int J Gynecol Cancer. 2015;25(5):802–808.
- Liu F, Yu X, Liu Z, et al. Comparison of ultrasound-guided percutaneous microwave ablation and parathyroidectomy for primary hyperparathyroidism. Int J Hyperthermia. 2019;36(1):835–840.
- Tang X, Ding M, Lu B, et al. Outcomes of ultrasound-guided percutaneous microwave ablation versus surgical resection for symptomatic large hepatic hemangiomas. Int J Hyperthermia. 2019;36(1):632–639.
- Xu B, Zhou NM, Cao WT, et al. Comparative study on operative trauma between microwave ablation and surgical treatment for papillary thyroid microcarcinoma. World J Clin Cases. 2018;6(15):936–943.
- Xu C, Li L, Xu W, et al. Ultrasound-guided percutaneous microwave ablation versus surgical resection for recurrent intrahepatic cholangiocarcinoma: intermediate-term results. Int J Hyperthermia. 2019;36(1):351–358.
- de Lacerda GF, Howlader N, Mariotto AB. Differences in cancer survival with relative versus cause-specific approaches: an update using more accurate life tables. Cancer Epidemiol Biomarkers Prev. 2019;28(9):1544–1551.
- Salem ME, Yin J, Weinberg BA, et al. Clinicopathological differences and survival outcomes with first-line therapy in patients with left-sided colon cancer and rectal cancer: Pooled analysis of 2879 patients from AGITG (MAX), COIN, FOCUS2, OPUS, CRYSTAL and COIN-B trials in the ARCAD database. Eur J Cancer. 2018;103:205–213.
- Nicholas MN, Khoja L, Atenafu EG, et al. Prognostic factors for first-line therapy and overall survival of metastatic uveal melanoma: The Princess Margaret Cancer Centre experience. Melanoma Res. 2018;28(6):571–577.