Abstract
Purpose
To compare results in patients treated with additional radiofrequency ablation (RFA) after clinical evaluation or vital volume (Va) increase.
Methods
Forty patients with 42 benign thyroid nodules who underwent additional RFA were evaluated in this retrospective study. According to the different indication for additional RFA, 18 patients were divided into Vv increase group (V group) and 22 into clinical evaluation group (C group). Patients were followed up at 1, 3, 6, 12 months and every 12 months thereafter by conventional ultrasound (US), contrast-enhancement ultrasound (CEUS) and clinical evaluation. Volume, volume reduction rate (VRR), symptom score and cosmetic score were evaluated before treatment and each ablation.
Results
After the first RFA, there were no statistically differences between two groups in volume, VRR, cosmetic and symptom scores. Compared with the first RFA, volume of all the patients after additional RFA decreased significantly (p < 0.001). In additional RFA, during a mean follow-up time of 10.15 ± 9.17 months, volume in V group was significantly smaller than in C group (2.84 ± 5.43 ml Vs 7.39 ± 13.01 ml, p = 0.046). VRR in V group was significantly larger than in C group (90.18 ± 12.74% Vs 75.66 ± 26.47%, p = 0.007) with significant improvement of cosmetic and symptom scores (p = 0.047; p = 0.030). No complications occurred after each session ablation.
Conclusion
Vv increase was a more reliable indicator for additional RFA than clinical evaluation. Additional RFA performed after Vv increase was more effective with respect to volume reduction and improvement of clinical outcomes. Therefore, Vv increase should be set as an indication for additional RFA.
Introduction
Thyroid nodules are common in the general population, occurring in 20–70% of individuals [Citation1]. Most asymptomatic thyroid nodules are benign and only need observation, but about 20% of nodules grow over time with compressive symptoms or cosmetic problems [Citation2,Citation3]. Although surgery is the standard treatment for thyroid nodules, some patients refuse surgery because of the invasiveness of the procedure, risk of complications and scar formation. Moreover, surgery may involve partial or total thyroidectomy, thus generating a risk for postoperative hypothyroidism and the need for thyroid hormone supplementation [Citation1,Citation4]. As such, minimally invasive thermal ablation techniques, such as radiofrequency ablation (RFA), have been introduced and have yielded some good results.
RFA and other thermal ablation techniques, such as microwave ablation, laser ablation, and high-intensity focused ultrasound (HIFU) ablation, have been recommended as safe and effective treatment modalities for benign thyroid nodules [Citation4–7]. Several studies have reported a significant decrease in nodule volume with improvement of clinical concerns after ablation [Citation8–11]. A meta-analysis also showed that the volume reduction rate (VRR) at 6, 12 and 24 months after RFA was 68%, 75% and 87%, respectively [Citation12]. However, a single-session ablation for some large nodules or nodules located to crucial structures may be inadequate [Citation13–20]. Because it is technically difficult to completely ablated all the nodule margin from a single-session, additional ablation could be required to achieve sustainable volume reduction. In most studies, the need for additional ablation was usually determined based on clinical evaluation of specific factors, including nodule regrowth, incompletely relieved symptoms, or unsatisfactory volume reduction (e.g., VRR < 50%) [Citation5]. Recently, Sim et al. [Citation17] proposed a method of monitoring the nodule volume after RFA by dividing it into the total volume (Vt), ablated volume (Va) and vital volume (Vv). They found that Vv increase tended to precede regrowth and thus making it an indication for additional ablation. However, to our best knowledge, there is no consensus about the appropriate indication for additional ablation. Moreover, little is known about the clinical outcomes of additional RFA performed according to different indications.
Therefore, the purpose of this study was to compare the outcomes of additional RFA between patients who underwent the treatment according to clinical evaluation and according to Vv increase.
Materials and methods
The Institutional Review Board of our institution approved this retrospective study (Approval number: S2019-211-01). Written information consent was obtained from all the patients prior to RFA and Contrast-enhancement ultrasound (CEUS).
Patients
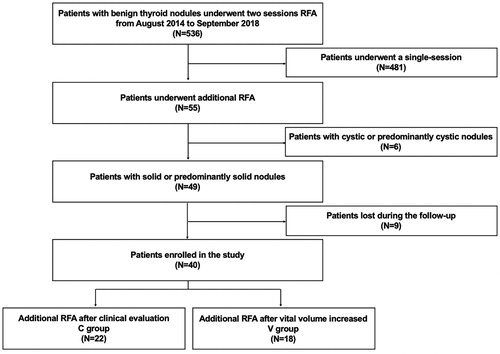
We evaluated patients with benign thyroid nodules who underwent RFA in our institution between August 2014 and September 2018. The inclusion criteria were: (1) confirmation of benign nodule status on two separate fine-needle aspiration (FNA) or core-needle biopsy (CNB) before each RFA; (2) no suspicious malignant features on US examination, including marked hypoechoic, ill-defined margins, taller-than-wide shape or microcalcifications; (3) solid (≤10% of fluid component) or predominantly solid nodules (11–50% of fluid component) [Citation21]; (4) report of cosmetic and/or symptomatic problems or concern of nodules growing rapidly; (5) serum thyroid hormone and thyrotropin levels within normal ranges; (6) refusal or ineligibility for surgery; (7) undergoing additional RFA. Of the 536 patients identified, 55 underwent additional RFA. After excluding those with cystic (>90% of fluid component)/predominantly cystic nodules (51–90% of fluid component)(N = 6) or those lost to follow-up (N = 9), 40 patients (35 females, 5 males, mean age 42.28 ± 11.95 years, range 18–74 years) with 42 benign thyroid nodules were evaluated in this study. The flowchart of patient enrollment is present in .
The need for additional RFA was decided based on (1) clinical evaluation that showed at least one of the following: nodule regrowth, incompletely relieved symptoms, or VRR < 50% or (2) Vv increase. The patients were divided into two groups according to the indication for additional RFA as the V group (i.e., patients who underwent additional RFA after Vv increase, N = 18 patients with 18 nodules) and the C group (i.e., patients who underwent additional RFA according to clinical evaluation findings, N = 22 patients with 24 nodules). Among the patients in the C group, 4 patients had concurrent nodule regrowth and Vv increase. The other 20 patients underwent additional RFA because they refused to wait until Vv increased. The trends in Vv increase in the C group before additional ablation were as follows: 4 patients had concurrent nodule regrowth and Vv increase; 2 patients had an enlarged Vv but <50%; and 18 patients had decreased Vv during the follow-up.
Pre-ablation assessment
Before treatment, each nodule underwent conventional US to evaluate the size, location, component, margin, shape, echogenicity, calcification and vascularity. The volume of thyroid nodules was calculated with the equations: V = πabc/6 (V is the volume, while a is the largest diameter, b and c are the other two perpendicular diameters). Nodule vascularity was scored as follows [Citation5]: grade 1, no vascularity; grade 2, peripheral vascularity; grade 3, intranodular vascularity < 50%; grade 4, intranodular vascularity > 50%. Symptom score was self-measured by patients using a 10-cm visual analogue scale (grade 0–10) [Citation5]. The cosmetic score was assessed by a physician (1, no palpable mass; 2, no cosmetic problem but palpable mass; 3, a cosmetic problem on swallowing only; and 4, a readily detected cosmetic problem) [Citation5].
CEUS was used to evaluate the ablated area of the nodule immediately after RFA and in the follow-up. Sulfur hexafluoride (SonoVueR, Bracco. International, Milan, Italy) was used as ultrasound contrast agent. CEUS was performed after bolus injection of SonoVue (2.4 ml), followed by a 5 ml of normal saline flush.
Ablation procedure
All RFA procedures were performed by an experienced US physician with more than 20-year experience in thyroid US and interventional US (Y.K.L). A bipolar RFA generator (CelonLabPOWER, Olympus Surgical Technologies Europe, Hamburg, Germany) and an 18-gauge bipolar RF electrodes with 0.9 cm active tip were used (CelonProSurge micro 100-T09, Olympus Surgical Technologies Europe, Hamburg, Germany) in this study.
Patients lay on an operating table in the supine position with the neck extended. Local anesthesia with 1% lidocaine was administered. If the distance between the tumor and critical cervical structures (trachea, cervical artery, jugular vein, esophagus and recurrent laryngeal nerve) was less than 5 mm, hydrodissection technique was used. RFA was performed using the trans-isthmic approach and moving-shot technique. The RFA power was 3 W. If a transient hyperechoic zone did not form at the electrode tip within 5–10 s, the radiofrequency power was increased to 5–9 W. CEUS was performed immediately after the RFA procedure to evaluate the ablation area. If any enhancement existed, a complementary ablation could be performed. Complications during and after the procedure were evaluated according to the clinical signs and symptoms [Citation21].
Post-ablation assessment
After the first RFA, the treated nodule was divided into 3 parts, which was Vt, Va and Vv [Citation15]. Vt was the total volume, which was measured and calculated by conventional US. Va was defined as the volume of ablated area which usually located in the central zone. It was measured and calculated by CEUS, which presented as a non-enhancement area within the treated nodule during the arterial phase and venous phase on CEUS. Vv was defined as the incompletely treated vital volume. It was calculated by the following equation: Vv = Vt − Va [Citation15]. Residual vital volume (RVR) was the ratio of residual vital volume to the total volume at last follow-up of the first RFA and the equation was as follows: RVR = Vv/Vt × 100%.
After ablation, patients were followed up at 13,612 months and every 12 months thereafter by conventional US, CEUS and clinical evaluation. VRR, cosmetic and symptom scores were evaluated during the follow-up period. The volume reduction was calculated as follows: VRR = ([initial volume − final volume] × 100%)/initial volume. Therapeutic success was defined as a > 50% volume reduction at last follow-up point [Citation21]. Regrowth was defined as an increase in total volume 50% over the previously recorded smallest volume [Citation21] and Vv increased was defined as a more than 50% increase compared to the previously reported smallest vital volume [Citation15].
Additional RFA
The procedure of additional RFA and follow-up strategy were the same as the the first RFA. After additional RFA, patients were followed up at 13,612 months and every 12 months thereafter. VRR of additional RFA (also calculated based on the initial volume), cosmetic and symptom scores were evaluated during the follow-up period. We also calculated VRR achieved only with the additional RFA (VRR2nd), which was defined as follows: VRR2nd = ([volume before additional RFA − final volume] × 100%)/volume before additional RFA.
Statistical analysis
Statistical analysis was performed using the SPSS statistical software (IBM Corp., Armonk), version 25.0. Continuous data were expressed as mean ± SD (range). Wilcoxon signed rank tests were used for comparison of the variables of the patients (follow-up time, volume, VRR, RVR, ablation time, power, energy, symptom score and cosmetic score) before treatment and each RFA. The Mann–Whitney test was used for comparison of the variables between the two groups before treatment and each RFA. Chi-square or Fisher’s exact test was used to compare the qualitative data between the two groups. A difference with p < 0.05 was considered as statistically significant.
Results
Clinical characteristics
A total of 40 patients (35 females, 5 males, mean age 42.28 ± 11.95 years, range 18–74 years) with 42 nodules (mean volume 20.24 ± 19.20 ml, range 0.82–91.48 ml) were enrolled in this study. Clinical characteristics of patients in two groups before the first RFA are presented in . There were 22 patients with 24 nodules in C group and 18 patients with 18 nodules in V group. There were no statistically differences of the demographic data and nodule characteristics between the two groups, including the age, sex, mean diameter, initial volume, solidity, vascularity, cosmetic score and symptom score.
Table 1. Comparisons between the two groups before RFA.
Efficacy
For all the patients, the mean follow-up time of first RFA and of additional RFA was 7.90 ± 5.94 months and 10.15 ± 9.17 months, respectively. The baseline volume was 20.24 ± 19.20 ml and significantly decreased to 8.72 ± 11.52 ml after the first RFA and 5.44 ± 10.60 ml after additional RFA (all p < 0.001). The VRR was 62.28 ± 23.72% after the first RFA and 81.89 ± 22.65% after additional RFA (p < 0.001).The therapeutic success rate was 76.19%(32/42) after the first RFA and 92.86%(39/42) after additional RFA (p = 0.035). The mean cosmetic score was 3.26 ± 0.89 at baseline, and significantly decreased to 2.14 ± 0.81 after the first RFA and 1.36 ± 0.69 after additional RFA (all p < 0.001). The mean symptom score was 4.29 ± 1.60 at baseline, and significantly decreased to 2.36 ± 1.39 after the first RFA and 0.88 ± 1.29 after additional RFA (all p < 0.001). No regrowth nodules were found. Ablation time and energy in the first RFA was significantly larger than in additional RFA (p = 0.002; p < 0.001). The comparisons of all the patients between the first RFA and additional RFA are presented in .
Table 2. Comparisons of the first and additional RFA between the two groups.
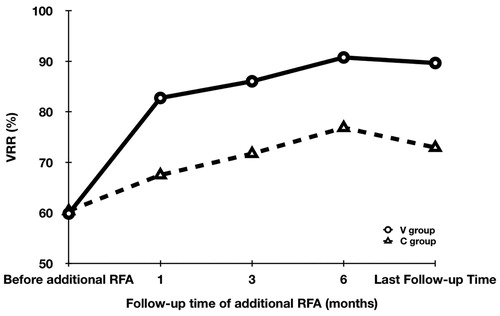
In the first RFA, the follow-up time was significantly longer in the V group than in the C group (9.00 ± 4.65 months vs 7.08 ± 6.73 months, p = 0.022). RVR was also significantly larger (86.11 ± 17.33% vs 63.43 ± 26.20%, p = 0.001). However, there were no statistically differences between the two groups for the volume, VRR, therapeutic success rate, ablation time, power, energy, cosmetic score and symptom score after the first RFA (all p > 0.05). In additional RFA, the volume was significantly smaller in the V group than in the C group (2.84 ± 5.43 ml vs 7.39 ± 13.01 ml, p = 0.046). The changes of VRR after additional RFA in two groups are presented in and . At first 3 months after additional RFA, VRRs in V group were larger than in C group, but the difference was not significant (p = 0.102; p = 0.102). However, at 6 months, VRR was significantly larger in the V group than in the C group (91.38 ± 17.78% vs 79.71 ± 25.87%, p = 0.006) and this remained at the last follow-up (90.18 ± 12.74% vs 75.66 ± 26.47%, p = 0.007). Moreover, VRR2nd in the V group during the follow-up time were all significantly larger than that in the C group (all p < 0.02). Both the cosmetic score [1.11 ± 0.32 vs 1.54 ± 0.83, p = 0.047)] and symptom score (0.39 ± 0.70 vs 1.25 ± 1.51, p = 0.030) were significantly smaller in the V group than in the C group. Representative cases of the two groups are shown in and . There were no significant differences in therapeutic success rate, ablation time, power, and energy between the two groups (all p > 0.05). No regrowth nodules were also found. Therapeutic success was achieved in all the patients in the V group. Meanwhile, three patients further underwent three ablation sessions because of unsatisfactory volume reduction in the C group. In these 3 patients, the initial volume was 43.56 ml, 60.20 ml and 29.91 ml before treatment, respectively. After the first RFA, the volume was 25.79 ml, 58.61 ml and 21.04 ml, respectively. At the last follow-up of second RFA, the volume was 24.74 ml, 57.69 ml and 28.2 ml, respectively. At the last follow-up after the third RFA, the volume was 19.79 ml, 29.67 ml and 14.63 ml, respectively. The VRR of the third RFA calculated based on the initial volume was 54.57%, 50.71%, and 51.09%.
Figure 3. The conventional US and CEUS images of a 41-year-old male in the V group during each ablation (A) A solid nodule located in the right thyroid before treatment with an initial volume of 6.07 ml. (B) At 1 month after the first RFA, the total volume was 2.61 ml and VRR was 57.00%. CEUS showed residual vital tissues located in the peripherally area (arrow). The vital volume was 2.09 ml. (C) At 3 months after the first RFA, the total volume was 1.21 ml and VRR was 80.07%. CEUS showed the vital volume 1.12 ml. (D) At 6 months after the first RFA, the total volume enlarged to 1.79 ml and VRR was 70.51%. Vital volume increase was found in CEUS, which was 1.78 ml. Additional RFA was performed. (E) At 3 months after additional RFA, the total volume was 0.67 ml and VRR was 88.96%. (F) At 6 months after additional RFA, the total volume decreased to 0.11 ml and VRR was 98.19%.
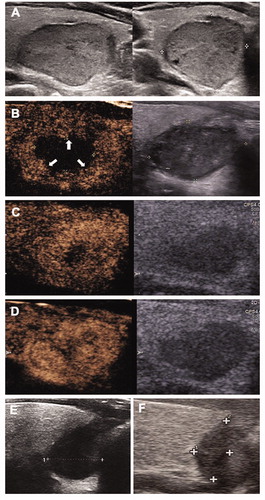
Figure 4. The conventional US and CEUS images of an 18-year-old female in the C group during each ablation (A) A solid nodule located in the right thyroid before treatment with an initial volume of 8.44 ml. (B) At 1 month after the first RFA, the total volume was 3.36 ml and VRR was 60.19%. CEUS showed residual vital tissues located in the peripherally area (arrow). The vital volume was 1.68 ml. (C) At 6 months after the first RFA, the total volume was 1.52 ml and VRR was 81.99%. CEUS showed the vital volume was 1.24 ml. Additional RFA was performed. (D) At 6 months after additional RFA, the total volume decreased to 0.85 ml and VRR was 89.95%.
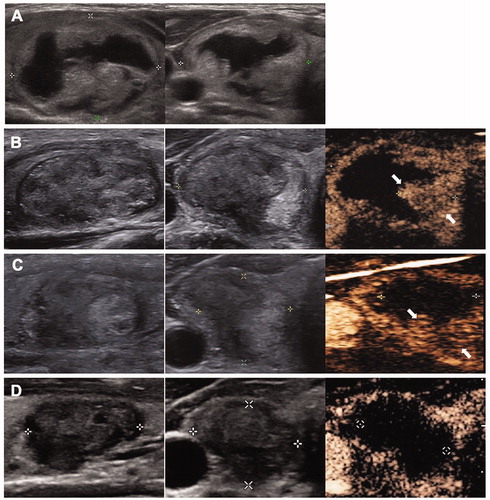
Table 3. Changes of VRRs and VRR2nd at each follow-up period after additional RFA.
Safety
All the patients were tolerable to the first and additional RFA procedures. No patients had complications during or after RFA. Side effects like pain and discomfort occurred in 4 patients at the first RFA (2 in V group and 2 in C group) and 5 patients at additional RFA (3 in V group and 2 in C group), respectively, which all resolved spontaneously within 3 days. There was no significantly differences in incidence of side effects between two groups in the first and additional RFA (p = 1.000; p = 0.810).
Discussion
There is no consensus about the appropriate indication for additional RFA in benign thyroid nodules. Our results showed that Vv increase was a more appropriate indication for additional RFA than clinical evaluation findings (i.e., nodule regrowth, incompletely relieved symptoms, or VRR <50%). Additional RFA was more effective with respect to volume reduction and improvement of symptom and cosmetic scores when performed according to Vv increase. No complications or sequelae occurred during and after each session ablation.
RFA and other thermal ablation techniques, such as microwave ablation, laser ablation, and HIFU ablation, have been considered as safe and effective alternative modalities to surgery for benign thyroid nodules [Citation4–7,Citation22,Citation23]. Therefore, their long-term efficacy has attracted research attention. Studies showed that 20.29–65.77% of nodules are treated with multiple sessions of ablation because of the large initial volume or unsatisfactory clinical outcomes [Citation13–16]. Moreover, some studies showed that 4.1–24.5% of the treated nodule occurred regrowth after 2 to 3 years and need additional ablation [Citation13,Citation17–20]. These results indicate that a single ablation may be inadequate to achieve long-term or sustained efficacy and additional ablation is required, particularly in nodules with initial large volumes [Citation5]. A meta-analysis compared ablation treatment strategies and found that two sessions of RFA were more effective than a single session [Citation24]. Dossing et al. [Citation25] also noted that three sessions of laser ablation achieved significantly greater volume reduction than one session treatment. Similar results were also found in this study. The VRR of additional RFA in two groups was 81.89 ± 22.65%, which was significantly larger than after the first RFA (62.56 ± 24.03%). Moreover, compared with the first RFA, the cosmetic and symptom scores were also significantly improved after additional RFA. Collectively, these results indicated that additional RFA could obtain it expected efficacy for patients who did not achieve satisfactory volume reduction from the first RFA.
Although the appropriate indication for additional ablation remains unclear [Citation26], it is usually considered based on clinical evaluation findings, including incomplete relieved symptom, unsatisfactory volume reduction, and nodule regrowth [Citation5]. However, Sim et al. [Citation17] recently suggested additional RFA should be considered when Vv increased was detected. In this study, during the additional RFA, the VRR was significantly larger in the V group than in the C group (90.18 ± 12.74% vs 75.66 ± 26.47%). Moreover, VRR2nd at each follow-up period was significantly larger in the V group than in the C group. Both the cosmetic and symptom scores were significantly smaller in the V group than in the C group, indicated that additional RFA is more effective when performed due to Vv increase than clinical evaluation. The differences of efficacy could be explained by RVR and the follow-up time of the first RFA. RVR after Vv increase was significantly larger than after clinical evaluation, indicating that the residual vital volume was markedly larger when Vv increased was observed. Meanwhile, after a longer follow-up time of the first RFA, the residual vital area gradually enlarged to a sufficient thickness to be treated [Citation26,Citation27]. Therefore, additional RFA could be applied to a larger residual area and achieve substantial incremental volume reduction. Moreover, we found that the volume and cosmetic and symptom scores were significantly decreased after first RFA, indicating that the first RFA could still improve certain nodule-related symptoms. In addition, volume, VRR, and cosmetic and symptom scores were similar between the two groups after the first RFA, showing that the symptoms did not worsen when patients waited until Vv increase was detected before undergoing additional RFA. Therefore, to maximize the efficacy of ablation, additional RFA should be considered after Vv increase.
Unlike the study by Sim et al. [Citation17] which only used conventional US for measurement and calculation, we performed CEUS to observe the Vv increase in this study. Because the margin of the ablated area was ill-defined and the presence of a color signal in the vital area was not constant, measurements via conventional US could be difficult and even incorrect, thus limiting its reliability for measuring the vital volume [Citation6,Citation28,Citation29]. CEUS is a contrast harmonic imaging technique that allows detection and characterization of focal lesions by assessing the micro-vascularization with second contras agent, thus overcoming the limitations of conventional US and enabling the display of parenchymal microvasculature [Citation29–31]. It has been recommended for monitoring the outcomes of ablation treatment and periprocedural assessment of treatment response after ablation for liver and thyroid lesions [Citation23,Citation31,Citation32]. In this study, the size and margin of necrotic area were successfully differentiated from the ablated nodule using CEUS, supporting its usefulness for the accurate calculation of the true vital volume and thus determining the appropriate indication for additional RFA.
With respect to safety of additional ablation, we found no complications or sequela in each ablation. Moreover, there were no significant difference in the incidence of side effects between the first and additional RFA. A meta-analysis showed that the pooled proportion of overall and major complications after RFA was 2.38% and 1.35%, respectively [Citation33]. The low incidence of complications of RFA may be related to the experience of the physician, real-time US monitoring and ablated techniques such as moving-shot technique, trans-isthmic approach and hydrodissection technique recommended by guideline [Citation5].
This study had some limitations, including its retrospective design and relatively short follow-up period. Studies showed that nodule regrowth occurred 2 or 3 years after ablation [Citation13,Citation17–20]. Therefore, the long-term efficacy of additional RFA after different indications should be evaluated and compared in prospective studies. In addition, the sample size was small and did not allow for subgroup analysis according to the initial volume. Finally, the superiority of CEUS over conventional US for estimating Vv was not investigated in this stidu and needs further investigation.
In conclusion, Vv increase was a more reliable indicator for additional RFA than clinical evaluation. Additional RFA performed after Vv increase was more effective with respect to volume reduction and improvement of clinical outcomes. Therefore, Vv increase should be set as an indication for additional RFA.
Disclosure statement
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Additional information
Funding
References
- Gharib H, Papini E, Paschke R, et al. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules. J Endocrinol Invest. 2010;16:1–50.
- Durante C, Grani G, Lamartina L, et al. The diagnosis and management of thyroid nodules: a review. JAMA. 2018;319:914–924.
- Alexander EK, Hurwitz S, Heering JP, et al. Natural history of benign solid and cystic thyroid nodules. Ann Intern Med. 2003;138:315–318.
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26:1–133.
- Kim JH, Baek JH, Lim HK, et al.; Guideline Committee for the Korean Society of Thyroid Radiology (KSThR) and Korean Society of Radiology. 2017 Thyroid radiofrequency ablation guideline: Korean Society of Thyroid Radiology. Korean J Radiol. 2018;19:632–655.
- Papini E, Pacella CM, Solbiati LA, et al. Minimally-invasive treatments for benign thyroid nodules: a Delphi-based consensus statement from the Italian minimally-invasive treatments of the thyroid (MITT) group. Int J Hyperthermia. 2019;36:376–382.
- Dietrich CF, Müller T, Bojunga J, et al. Statement and recommendations on interventional ultrasound as a thyroid diagnostic and treatment procedure. Ultrasound Med Biol. 2018;44:14–36.
- Cesareo R, Pasqualini V, Simeoni C, et al. Prospective study of effectiveness of ultrasound-guided radiofrequency ablation versus control group in patients affected by benign thyroid nodules. J Clin Endocrinol Metab. 2015;100:460–466.
- Deandrea M, Garino F, Alberto M, et al. Radiofrequency ablation for benign thyroid nodules according to different ultrasound features: an Italian multicentre prospective study. Eur J Endocrinol. 2019;180:79–87.
- Cheng Z, Che Y, Yu S, et al. US-guided percutaneous radiofrequency versus microwave ablation for benign thyroid nodules: a prospective multicenter study. Sci Rep. 2017;7:9554.
- Lee GM, You JY, Kim HY, et al. Successful radiofrequency ablation strategies for benign thyroid nodules. Endocrine. 2019;64:316–321.
- Trimboli P, Castellana M, Sconfienza LM, et al. Efficacy of thermal ablation in benign non-functioning solid thyroid nodule: a systematic review and meta-analysis. Endocrine. 2020;67:35–43.
- Lim HK, Lee JH, Ha EJ, et al. Radiofrequency ablation of benign non-functioning thyroid nodules: 4-year follow-up results for 111 patients. Eur Radiol. 2013;23:1044–1049.
- Jeong WK, Baek JH, Rhim H, et al. Radiofrequency ablation of benign thyroid nodules: safety and imaging follow-up in 236 patients. Eur Radiol. 2008;18:1244–1250.
- Guang Y, He W, Luo Y, et al. Patient satisfaction of radiofrequency ablation for symptomatic benign solid thyroid nodules: our experience for 2-year follow up. BMC Cancer. 2019;19:147.
- Jung SL, Baek JH, Lee JH, et al. Efficacy and safety of radiofrequency ablation for benign thyroid nodules: a prospective multicenter study. Korean J Radiol. 2018;19:167–174.
- Sim JS, Baek JH, Lee J, et al. Radiofrequency ablation of benign thyroid nodules: depicting early sign of regrowth by calculating vital volume. Int J Hyperthermia. 2017;33:905–910.
- Døssing H, Bennedbaek FN, Hegedüs L. Long-term outcome following interstitial laser photocoagulation of benign cold thyroid nodules. Eur J Endocrinol. 2011;165:123–128.
- Valcavi R, Riganti F, Bertani A, et al. Percutaneous laser ablation of cold benign thyroid nodules: a 3-year follow-up study in 122 patients. Thyroid. 2010;20:1253–1261.
- Wang B, Han Z-Y, Yu J, et al. Factors related to recurrence of the benign non-functioning thyroid nodules after percutaneous microwave ablation. Int J Hyperthermia. 2017;33:459–464.
- Mauri G, Pacella CM, Papini E, et al. Image-guided thyroid ablation: proposal for standardization of terminology and reporting criteria. Thyroid. 2019;29:611–618. [pubmedMismatch]
- Mauri G, Gennaro N, Lee MK, et al. Laser and radiofrequency ablations for benign and malignant thyroid tumors. Int J Hyperthermia. 2019;36:13–20.
- Mainini AP, Monaco C, Pescatori LC, et al. Image-guided thermal ablation of benign thyroid nodules. J Ultrasound. 2017;20:11–22.
- Ha EJ, Baek JH, Kim KW, et al. Comparative efficacy of radiofrequency and laser ablation for the treatment of benign thyroid nodules: systematic review including traditional pooling and Bayesian network meta-analysis. J Clin Endocrinol Metab. 2015;100:1903–1911.
- Dossing H, Bennedbaek FN, Hegedus L. Effect of ultrasound-guided interstitial laser photocoagulation on benign solitary solid cold thyroid nodules: one versus three treatments. Thyroid. 2006;16:763–768.
- Sim JS, Baek JH. Long-term outcomes following thermal ablation of benign thyroid nodules as an alternative to surgery: the importance of controlling regrowth. Endocrinol Metab. 2019;34:117–123.
- Cervelli R, Mazzeo S, De Napoli L, et al. Radiofrequency ablation in the treatment of benign thyroid nodules: an efficient and safe alternative to surgery. J Vasc Interv Radiol. 2017;28:1400–1408.
- Sim JS, Baek JH, Cho W. Initial ablation ratio: quantitative value predicting the therapeutic success of thyroid radiofrequency ablation. Thyroid. 2018;28:1443–1449.
- Albrecht T, EFSUMB Study Group, et al. Guidelines for the use of contrast agents in ultrasound. Ultraschall Med. 2004;25:249–256. Blomley M, Bolondi L,.
- Ma JJ, Ding H, Xu BH, et al. Diagnostic performances of various gray-scale, color Doppler, and contrast-enhanced ultrasonography findings in predicting malignant thyroid nodules. Thyroid. 2014;24:355–363.
- Claudon M, Dietrich CF, Choi BI, et al.; European Federation of Societies for Ultrasound. Guidelines and good clinical practice recommendations for Contrast Enhanced Ultrasound (CEUS) in the liver – update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultrasound Med Biol. 2013;39:187–210.
- Gharib H, Papini E, Garber JR, et al. American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi Medical Guidelines for Clinical Practice for the Diagnosis and Management of Thyroid Nodules – 2016 update. Endocr Pract. 2016;22:1–60.
- Chung SR, Suh CH, Baek JH, et al. Safety of radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: a systematic review and meta-analysis. Int J Hyperthermia. 2017;33:920–930.