Abstract
Background
We developed a novel balloon-based endobiliary radiofrequency ablation (RFA) system to overcome the limitations of conventional RFA in treating malignant biliary strictures. This study aimed to evaluate the histological effects of balloon-RFA in porcine bile ducts.
Methods
Balloon-RFA of intrahepatic bile ducts from freshly resected porcine livers was performed for 60 s at 50, 60 and 70 °C. The specimens were subsequently sectioned for histological analysis and the slides were digitally scanned. Pseudo-coloring was applied based on the intensity of the ablation effect, and the area and estimated volume of ablation were measured.
Results
All samples showed epithelial sloughing and coagulative necrosis, and the entire internal circumference of the bile duct was evenly ablated. Complete transmural necrosis and involvement beyond the wall were found in 0% of samples ablated at 50 °C, in 33% at 60 °C and 100% at 70 °C. The mean depth and estimated volume of the ablation areas were 1.29 mm and 353.84 mm3, 1.44 mm, and 505.54 mm3 and 1.81 mm and 702.52 mm3 at 50, 60 and 70 °C, respectively.
Conclusions
Balloon-RFA leads to sloughing of the mucosa and coagulative necrosis. Ablation depth and volume increased in proportion to target temperature.
Introduction
Endobiliary radiofrequency ablation (RFA) is a promising option for treatment of malignant biliary strictures [Citation1]. RFA can achieve local tumor control, resulting in improved biliary stent patency and a potential survival benefit. However, conventional endobiliary RFA has some limitations, including the small number of amenable lesions and an uneven ablation area [Citation2]. These may explain why the results of previous studies have been contradictory [Citation3–6].
To overcome these issues, we developed balloon-based endobiliary RFA (balloon-RFA) [Citation7]. Although balloon-RFA may be indicated for various strictures and can theoretically achieve consistent depth without excessive ablation, its effects on the tissue itself are not well-characterized. This study aimed to evaluate the histological effects of balloon-RFA in porcine bile ducts.
Methods
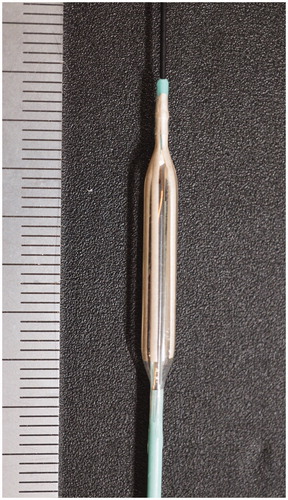
Balloon RFA catheter
A prototype balloon-RFA catheter (Japan Lifeline Co., Ltd., Tokyo, Japan) () and modified ARFA-GEN200 generator (Japan Lifeline Co., Ltd.) were used in this study. The catheter has a 3.5-mm diameter balloon at the tip, and eight stretchable electronic inks (20-mm long and 0.75-mm wide) are printed along the balloon’s length. A temperature sensor is equipped at the surface of the balloon, and cooling water can be perfused inside the balloon by an injection pump. The target temperature can be maintained automatically by adjusting the output power and cooling water perfusion, as well as monitoring the impedance during the procedure to ensure safety.
Experimental procedure
Freshly resected porcine livers were cut into blocks around the intrahepatic bile duct. The block was wrapped with gel and saline solution to keep the resistivity constant, and its interior temperature was kept at 37 °C. After RFA catheter insertion into the intrahepatic bile duct, ablation was performed at three different settings (50 °C for 60 s, 60 °C for 60 s and 70 °C for 60 s) for three times each. The output power was increased linearly from 5 W until the target temperature was reached and was continually adjusted to maintain this temperature. Each ablation setting was performed on a different specimen. The Institutional Animal Care and Use Committee of the Aichi Medical University approved this study.
Histologic analysis
After ablation, the intrahepatic bile duct was cut longitudinally to expose the mucosal surface using a pathology knife. The specimens were fixed in formalin, embedded in paraffin and sectioned for histological analysis. Hematoxylin and eosin, and NADH-tetrazolium reductase staining were performed. All slides were scanned by a digital scanner (NanoZoomer-XR; Hamamatsu Photonics K.K., Shizuoka, Japan) to create high-quality digital slides. All digital slides stained using hematoxylin and eosin staining were viewed and analyzed using Aperio ImageScope (Leica Biosystems, Nussloch, Germany). Slides that underwent NADH-tetrazolium reductase staining were analyzed by ImageJ software, and pseudo-coloring was applied based on the intensity of the ablation effects to recognize and determine the ablation area. The area and estimated volume of the ablation were subsequently measured.
Results
The experimental results are shown in . All samples showed epithelial sloughing and coagulative necrosis (), and the entire internal circumference of the bile duct was evenly ablated. Complete transmural necrosis was found in 0% (0/3) of samples ablated at 50 °C for 60 s, 33% (1/3) of those ablated at 60 °C, and 100% (3/3) of those ablated at 70 °C. The effects of RFA extended beyond the bile duct wall in 0% (0/3) of samples ablated at 50 °C for 60 s, 33% (1/3) of those ablated at 60 °C, and 100% (3/3) of those ablated at 70 °C.
Figure 2. The bile duct wall was injured thermally and the epithelium was sloughed off as a result of the treatment (a). Eosinophilic coagulative necrosis was observed at the bile duct wall and the surrounding tissue (b, c).
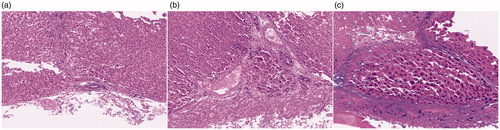
Table 1. Detailed histologic findings after balloon-based radiofrequency ablation.
Digital analysis of the pseudo-color-mapped samples showed that the length and depth of the ablation area were 18.03 and 1.29 mm, respectively, at 50 °C for 60 s setting. The dimensions of the ablation area were unclear in two samples. The mean length of the ablation area in samples ablated at 60 and 70 °C for 60 s were 20.18 and 21.47 mm, respectively, while the mean depth was 1.44 and 1.81 mm, respectively. The mean estimated volume of the total ablation area was 353.84, 505.54 and 702.52 mm3 in samples ablated for 60 s at 50, 60 and 70 °C, respectively.
Discussion
This study confirmed that the histological effects of balloon-RFA involve sloughing of the mucosal layer and coagulative necrosis. The ablation depth and area were found to be increased in proportion to the target temperature.
RFA can improve biliary stent patency by preventing tumor ingrowth, and may prolong survival in patients with pancreatobiliary cancer by achieving local tumor control [Citation1]. However, there is no consensus on its optimal usage and its usefulness is still debated. Conventional RFA catheters do not achieve effective ablation of strictures that are short, non-tight, or rough, due to insufficient contact with the tissue [Citation2]. Additionally, the point at which the electrodes are in contact with will inevitably experience pronounced and deep burns. This may be one of the reasons underlying the discrepancies between previous studies. Conversely, if appropriate ablation can be achieved, RFA would be effective for treating malignant biliary strictures.
Balloon-RFA can in theory allow for contact of the electrodes with the entire circumference of the bile duct wall. This study findings showed that the entire internal circumference of the bile duct was ablated, and the ablation area consistently showed a cylindrical pattern around the catheter. Additionally, the ablation area and volume were proportional to the target temperature. Therefore, with further research, it would be possible to determine the shape, range and volume to be ablated before the procedure. Assuming balloon-RFA application under endoscopic guidance, the ablation area may be set and controlled according to intraductal ultrasonography assessment. Additionally, balloon-RFA could also possibly be applied percutaneously.
The results of this study should be considered in the context of its limitations, which include its ex-vivo design using normal porcine bile ducts. Animal models of biliary strictures do not exist, limiting the assessment of the effect of balloon-RFA on the strictures. Furthermore, achieving a similar ablative effect in human tissues may require higher thermal energies. To definitively establish this innovative procedure, its efficacy needs to be confirmed in further analyses. In-vivo experiments are currently underway.
In conclusion, balloon-RFA has significant potential and may be a relevant option for treating malignant biliary strictures. This preclinical study should pave the way for evaluation of the efficacy of this procedure in future trials.
Ethical approval
The Institutional Animal Care and Use Committee of the Aichi Medical University approved this study.
Author contributions
Tadahisa Inoue: conception and design, data acquisition, analysis and interpretation and drafting and revising of the manuscript.
Masashi Yoneda: data interpretation and revising of the manuscript.
Acknowledgments
We thank Japan Lifeline Co., Ltd. for providing the balloon-based radiofrequency ablation system.
Disclosure statement
Tadahisa Inoue received honoraria from Japan Lifeline Co., Ltd. and Boston Scientific Japan. The other author discloses no financial relationships relevant to this publication.
Additional information
Funding
References
- Larghi A, Rimbaș M, Tringali A, et al. Endoscopic radiofrequency biliary ablation treatment: a comprehensive review. Dig Endosc. 2019;31(3):245–255.
- Inoue T, Ibusuki M, Kitano R, et al. Endobiliary radiofrequency ablation combined with bilateral metal stent placement for malignant hilar biliary obstruction. Endoscopy. 2020;52(07):595–599.
- Sharaiha RZ, Natov N, Glockenberg KS, et al. Comparison of metal stenting with radiofrequency ablation versus stenting alone for treating malignant biliary strictures: is there an added benefit? Dig Dis Sci. 2014;59(12):3099–3102.
- Kallis Y, Phillips N, Steel A, et al. Analysis of endoscopic radiofrequency ablation of biliary malignant strictures in pancreatic cancer suggests potential survival benefit. Dig Dis Sci. 2015;60(11):3449–3455.
- Yang J, Wang J, Zhou H, et al. Efficacy and safety of endoscopic radiofrequency ablation for unresectable extrahepatic cholangiocarcinoma: a randomized trial. Endoscopy. 2018;50(08):751–760.
- Teoh AY, Cheung SY, Chong C, et al. Endoscopic biliary radiofrequency ablation for malignant distal common bile duct strictures does not improve survival. A randomized controlled trial [abstract]. Gastrointest Endosc. 2018;87(6):AB104–AB105.
- Inoue T, Ito K, Yoneda M. Novel balloon catheter-based endobiliary radiofrequency ablation system: ex-vivo experimental study. Dig Endosc. 2020;32(6):974–978.