Abstract
Purpose
The aim of this study was to retrospectively compare and analyze pregnancy outcomes of patients with uterine fibroids after high intensity focused ultrasound (HIFU) ablation and laparoscopic myomectomy (LM).
Materials and methods
The study group consisted of 346 patients with uterine fibroids who wished to conceive, in which 152 patients received HIFU ablation treatment (HIFU group) and 194 patients received LM treatment (LM group). The parents’ baseline characters were recorded and the pregnancy outcomes were evaluated in a median follow-up time of 42 months (range: 16 ∼ 81) after the treatment, and the differences of the two groups were compared.
Results
Patients with uterine fibroids in HIFU group had a significant shorter pregnancy interval than that in LM group (10 months VS. 13 months, p < .05). No significant differences were observed in pregnancy rate, miscarriage rate, live birth rate, natural pregnancy rate, cesarean section rate, and perinatal complications rate between the HIFU group and the LM group (p > .05). When stratified by age, infertility history, fibroid types, fibroid numbers, and fibroid sizes, there was no statistically significant difference in pregnancy rate between the HIFU group and the LM group (p > .05).
Conclusions
Based on the results from this study, both HIFU and LM can be safely used to treat patients who wish to conceive. The pregnancy outcomes of post-HIFU are similar to that of post-LM.
Introduction
Uterine fibroids (uterine myomas, leiomyomas) are the most common genital tract benign tumors in women of childbearing age. The prevalence increases with aging, with an estimated rate varying from 50% to 77% among women [Citation1]. Previous studies have indicated that uterine fibroids account for 10% of infertility cases globally, and also account for 20–30% of miscarriages [Citation2]. Thus, uterine fibroids have a clearly adverse effect on women's reproductive status and outcomes, mainly by impeding transportation and implantation of embryos, blood supply and local hormonal level changes [Citation3]. Moreover, uterine fibroids also increase the risk of pregnancy complications, such as abnormal fetal position, premature rupture of membranes, premature delivery, postpartum hemorrhage and so on [Citation2]. Therefore, an increasing number of gynecologists are looking for different ways to increase pregnancy rate and improve pregnancy outcomes of patients with uterine fibroids.
Currently, the traditional treatment of choice for patients with uterine fibroids who wish to conceive is myomectomy [Citation4]. The advantages of laparoscopic myomectomy (LM) in comparison to abdominal myomectomy include less severe complications and faster recovery rate [Citation5]. However, LM will cause damage to the uterine smooth muscle; thus, patients are often suggested to conceive 1–2 years after surgery. In addition, uterine rupture during pregnancy may occur in patients with uterine fibroids [Citation6]. Therefore, it is necessary to develop and evaluate alternatives to surgical procedures especially when fertility preservation is the goal.
High intensity focused ultrasound (HIFU) is a novel noninvasive tumor ablative technique. Over the last two decades, HIFU has been widely used in practice to treat uterine fibroids. As a noninvasive treatment technique, HIFU is performed under the guidance of ultrasound or magnetic resonance imaging, so the fibroids can be selectively ablated without damaging adjacent structures [Citation7]. A few retrospective studies [Citation2,Citation8] have also shown that the pregnancy is safe after HIFU. However, there are few comparative studies on pregnancy outcomes between HIFU and LM.
Therefore, the main aim of this study was to compare the pregnancy outcomes of patients with uterine fibroids treated by HIFU or LM.
Materials and methods
Ethical considerations
The ethics committee of the Third Xiangya Hospital approved this study. All patients signed an informed consent form before HIFU or LM treatment.
Patients
This cohort study included 346 patients who received HIFU or LM at the Third Xiangya Hospital of Central South University between January 2013 and June 2018.
The inclusion criteria were as follows: (1) uterine fibroids diagnosed by contrast-enhanced MRI or postoperative pathology; (2) women of childbearing age who wish to become pregnant; (3) the size of uterine fibroids: 3 ∼ 12cm in diameter; (4) type 1 ∼ 7 and hybrid uterine fibroids; (5) availability of complete clinical data.
Exclusion criteria were as follows: (1) continuous contraception or asexual life after treatment; (2) spouse with infertility or patients with clear infertility etiologies other than uterine fibroids; (3) had other treatment after HIFU or LM; (4) suspected or confirmed malignancy. After the clinical diagnosis was made, two treatment options were offered to the patients. 152 patients chose HIFU treatment (HIFU group) and 194 patients chose LM treatment (LM group). According to the International Federation of Gynecology and Obstetrics (FIGO) [Citation9] classification system of uterine fibroids, fibroids attached to the endometrium by a narrow stalk were classified as type 0; fibroids <50% intramural were classified as type 1; fibroids ≥50% intramural were classified as type 2; fibroids totally extracavitary but abutting the endometrium were classified as type 3; fibroids entirely within the myometrium were classified as type 4; fibroids ≥50% subserosal were classified as type 5; fibroids <50% subserosal were classified as type 6; fibroids attached to the serosa by a stalk were classified as type 7; fibroids that did not relate to the myometrium at all, such as cervical and ligament lesions, were classified as type 8; and fibroids touching both the endometrium and serosa were classified as hybrid fibroids. Based on the relationship between uterine fibroids and the endometrium, fibroids were divided into two groups: the mucosa-associated type (types 1, 2, 3 and hybrid fibroids) and the non-mucosa-associated type (the rest types).
HIFU treatment
Equipment: HIFU treatment was performed using a JC-200 focused ultrasound tumor therapeutic system (Haifu Medical Technology Co., Ltd., Chongqing, China).
Preparation for HIFU treatment: Before the HIFU procedure, all patients were requested to have bowel preparation for 3 days. The patients were asked to ingest a bland diet on day 1, followed by semi-liquid and liquid food without milk on the second and third day, respectively. In addition, the patients were asked to take compound polyethylene glycol electrolyte solution for luminal catharsis. On the morning of HIFU treatment day, the patients were treated with enema to further clean the bowel. One hour before HIFU treatment, skin preparation was made included shaving hair from the umbilicus to the upper margin of the pubic symphysis, degreasing and degassing with 75% ethanol or degassed water. A catheter was inserted before the procedure to control the bladder volume for the duration of treatment.
HIFU ablation
The patients were positioned prone on the HIFU table, with the anterior abdominal wall in contact with degassed water. A degassed water balloon was placed between the abdominal wall and the transducer to help compress and push the bowel away from the acoustic pathway. The HIFU procedure was performed under conscious sedation. The patients were sedated with fentanyl (1 μg/kg) and midazolam (0.02∼0.03 mg/kg) to relieve pain and prevent unnecessary body movement.
HIFU ablation was performed under the guidance of real-time ultrasound. Point scan was selected, and power was set between 350 and 400 watts. The distance from the focal point to the endometrium was at least 1.5 cm, and the distance from the focal point to the subserosal surface of the uterus was 1 cm. During the procedure, therapeutic energy was adjusted based on patient feedback and changes in grayscale on ultrasonographic imaging. This process was repeated until there was an absence of blood supply visualized on contrast-enhanced ultrasound. Contrast-enhanced ultrasound and contrast medium (SonoVue, Bracco, Italy) were used to show the non-perfused volume (NPV) ratio of treated fibroids, which could evaluate the ablation efficacy immediately after HIFU.
LM Treatment
Equipment: LM was performed with standard laparoscopic equipment (Karl Storz & Co., Germany).
Preparation for LM treatment: All the patients underwent careful bowel and skin preparation prior to LM, which included a diet of liquid food for one day prior to surgery, fasting 6 ∼ 8 h before surgery and an enema 2 h before the procedure. The hair shaving range was the same as HIFU treatment, and a urinary catheter was also inserted before the surgery.
LM Procedure: LM was performed under general anesthesia. Patients were placed in the lithotomy position. An arc-shaped incision was made at the upper edge of the umbilicus to create a pneumoperitoneum, and trocars were used to puncture the abdomen and were placed under the laparoscopy to prevent internal organs damage during the whole procedure of treatment. Then 6 ∼ 12 U vasopressin was diluted and injected below the pseudo-capsule of the fibroids over the protruding surface. After the targeted fibroid was removed, the incision was sutured.
Follow-up observation
Follow-up visits were scheduled at 12 months after HIFU or LM to evaluate symptom improvement via the Uterine Fibroid Symptom (UFS) questionnaire [Citation10]. A 5-point categorical scale (1, not affected; 2, a little affected; 3, somewhat affected; 4, greatly affected; 5, very greatly affected) was used to assess 8 parts (1, heavy bleeding during menstrual period; 2, passage blood clots during menstrual period; 3, fluctuation in the duration of menstrual period; 4, fluctuation in the duration of monthly cycle; 5, feeling of tightness or pressure in pelvic area; 6, frequent daytime urination; 7, frequent nighttime urination; 8, feeling of fatigue) in the UFS questionnaire. The pregnancy outcomes were evaluated in a median follow-up time of 42 months (range: 16 months ∼81 months) after HIFU or LM treatment. The percentage of pregnancies, pregnancy interval, mode of conception, mode of delivery, and complications during the perinatal period were also recorded.
Statistical methods
SPSS 23.0 (SPSS, Inc.) was used for statistical analysis. The skewed distribution data were reported as medians and interquartile range [M (P25, P75)], and the enumeration data were expressed as rate (%). The Wilcoxon-paired rank sum test was used to compare the UFS score before and after HIFU treatment or LM. The Mann-Whitney U test was used for comparison between the two groups of measurement data. The Chi-square test or Fisher exact test was used for enumeration data. A logistic regression analysis and a ROC curve analysis were used to determine the factors affecting pregnancy after HIFU or LM. p < .05 was defined as statistically significant.
Results
Baseline characteristics
This research consisted of 346 patients with uterine fibroids who wished to have a baby, of which 152 patients were in the HIFU group and 194 patients were in the LM group. In the HIFU group, the median age of patients was 35 years (range: 24 ∼ 44). In the LM group, the median age of patients was 34.5 years (range: 22 ∼ 40). There were no statistically significant differences between the HIFU group and the LM group before treatment in terms of age, body mass index (BMI), infertility history, hemoglobin level, size, number and type of uterine fibroids ().
Table 1. Baseline characteristics of patients with uterine fibroids treated with HIFU or LM.
Evaluation of HIFU treatment and LM
In the HIFU group, after a single session of HIFU treatment, the median NPV ratio of uterine fibroids was 84.87% (range: 38.74%∼100%). Among the 152 patients, 130 of them had a NPV ratio higher than 70%. And the median hospital stay after HIFU ablation was 2 days (range: 1 ∼ 3). No severe complications occurred. In the LM group, the median hospital stay after the surgery was 4 days (range: 3 ∼ 6). No severe complications were observed. In addition, compared with LM group, the HIFU group showed a significantly shorter hospital stay after the treatment (p = .000).
Follow-up observation
In HIFU group, 38 patients performed significant fibroid symptoms, while 66 patients performed significant fibroid symptoms in LM group. Follow-up data showed after 12 months, a significant decrease in UFS score before and after treatment in patients with symptoms in both the two groups (p < .05) (see supplementary material, ).
Table 2. Comparison of UFS score before and after treatment in patients with symptoms.
Reproductive outcomes after HIFU treatment or LM
During a median follow-up time of 42 months (range: 16 ∼ 81), of the 152 patients treated with HIFU, 113 (74.34%, 113/152) patients became pregnant, of which 62 (54.87%, 62/113) patients delivered healthy babies, 20 (17.7%, 20/113) patients had spontaneous miscarriages and 22 (19.5%, 22/113) patients had abortions, 2 (1.77%, 2/113) patients had ectopic pregnancies, 7 (6.19%, 7/113) patients were still pregnant. Of the patients who delivered babies successfully, 50 (80.65%, 50/62) of them were delivered by cesarean section due to uterine scars in 18 cases, placenta previa in 1 case, oligohydramnios in 3 cases, fetal distress in 2 cases, breech presentation in 2 cases, cephalopelvic disproportion in 1 case, twin pregnancy in 1 case, failure of labor induction in 2 cases, macrosomia in 3 cases, elderly primipara in 1 case, and social factors in 16 cases. Of the 194 patients treated with LM, 146 (75.26%, 146/194) patients were pregnant, of which 101 (69.18%, 101/146) patients delivered healthy babies, 20 (13.7%, 20/146) patients had miscarriages, 13 (8.9%, 13/146) patients had induced abortions, 3 (2.05%, 3/146) patients had ectopic pregnancies, and 9 (6.16%, 9/146) patients were still pregnant. Of the patients who had successfully delivered babies, 83 (82.18%, 83/101) of them delivered by cesarean section due to uterine scars in 33 cases, placenta previa in 2 cases, oligohydramnios in 3 cases, fetal distress in 4 cases, breech presentation in 3 cases, cephalopelvic disproportion in 1 case, twin pregnancy in 2 cases, induced labor failure in 1 case, macrosomia in 3 cases, elderly primipara in 3 cases, gestational hypertension in 1 case, and social factors in 27 cases. No uterine ruptures were observed during pregnancy and delivery in any cases.
As shown in , the pregnancy interval in the HIFU group was significantly shorter than that in the LM group (p < .05). However, no significant difference was observed in pregnancy rate, assisted pregnancy rate, pregnancy outcome, cesarean section delivery rate, rate of perinatal complications, preterm birth rate and postpartum hemorrhage rate between the two groups (p > .05).
Table 3. Comparison of pregnancy outcomes between groups.
Logistic regression analysis of factors influencing reproductive outcomes after HIFU or LM treatment
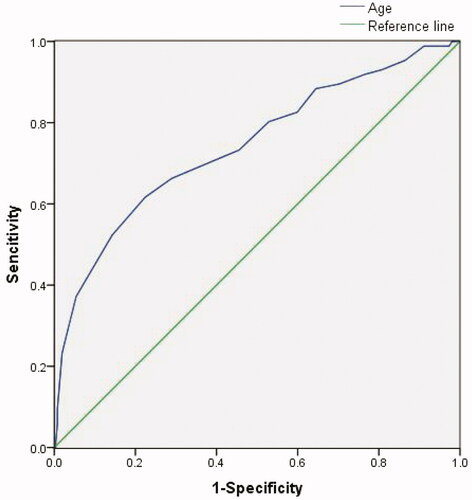
In this study, a total of 259 patients conceived after HIFU or LM, while 87 patients did not conceive. Univariate logistic regression analysis showed that hemoglobin level, pretreatment UFS score, post-treatment UFS score, uterine position, the size of fibroids, and therapeutic modality were not significantly associated with pregnancy rate. However, significant differences between the pregnant group and non-pregnant group were observed in age, BMI, infertility history, uterine size, the number and type of fibroids (). Furthermore, multiple logistic regression analysis showed that advanced maternal age and infertile patients with mucosa-associated fibroids or multiple uterine fibroids were associated with less improvement in reproductive outcomes (). Finally, we investigated the correlation between age and pregnancy rate using the ROC curve (). The results showed that the largest Youden Index was 36.5 for age. It indicated that pregnancy rate was significantly lower in patients older than 36.5 years old ().
Table 4. Univariate factors influencing reproductive outcomes after treatment.
Table 5. Multiple logistic regression analysis of factors influencing reproductive outcomes after treatment.
A hierarchical comparison of HIFU treatment and LM in pregnancy rate
Age, infertility history, the number and type of fibroids may have effects on pregnancy rate. So we performed a hierarchical comparison to investigate if any significant differences existed between the patients treated with HIFU and LM. As shown in , no significant differences in pregnancy rates were observed between the HIFU and the LM group for age, infertility history, number and type of uterine fibroids ().
Table 6. A hierarchical comparison of HIFU treatment and LM in pregnancy rate.
Discussion
Uterine fibroids are a benign type of ovarian steroid hormone dependent tumors, which pose worldwide health risks for women of childbearing age. Fibroids can affect quality of life and even lead to infertility and miscarriage in some cases [Citation11]. The goal of treatment for uterine fibroids is not only to achieve symptom relief, but also to improve pregnancy outcomes. There are many treatments for uterine fibroids, and the choice depends on many factors, such as age, fertility intention, symptoms and the location, size and number of uterine fibroids [Citation12]. Although hysterectomy is considered the most effective approach to treat uterine fibroids, it is not suitable for patients who have the desire to give birth [Citation7].
LM is the most classical treatment for patients with uterine fibroids who wish to conceive. The newly developed HIFU treatment is a noninvasive technique. The fibroids can be precisely ablated by HIFU under the guidance of real-time ultrasound without damaging the normal uterine smooth muscle. After HIFU treatment, the treated fibroid is absorbed by the tissue nearby, and the uterine structure and uterine cavity gradually return to normal. Over the last few years, several studies [Citation2,Citation8] have shown the safety and efficacy of HIFU treatment for patients with uterine fibroids who intend to conceive; however, few studies have compared the pregnancy rate and pregnancy outcomes between patients with uterine fibroids treated with HIFU and LM.
In our study, the median NPV ratio of uterine fibroids was 84.87%, and the 12-month follow-up showed that the UFS score significantly decreased in patients with symptoms. Unfortunately, many patients in our department did not have MRI or ultrasonography imagings to evaluate the volume changes of the treated fibroids, so we could not show the volume reduction of the fibroids one year after HIFU treatment. Previous studies [Citation13] have demonstrated that the NPV ratio of fibroids is closely related to long-term symptom relief. Zou et al. [Citation2] presented an 83.5% NPV ratio average; at 6 months after treatment, the rate of volume reduction of the fibroids exceeded 50% in 84% patients. Therefore, symptom relief is sustained if the NPV ratio reached over 80%.
Our results showed that the pregnancy rate after HIFU or LM was 74.3% (113/152) or 75.3% (146/194), respectively. There was no significant difference in pregnancy rate between HIFU and LM groups (p > .05). Furthermore, the multivariate logistic regression analysis showed that age, infertility history, the number and type of uterine fibroids affected the pregnancy rate. We further grouped the patients by two age ranges (≤36 or >36), by having or not having infertility history, by single or multiple fibroids, and by Mucosa-associated or Non-mucosa-associated fibroids; the results did not show any significant difference between the two groups (p > .05). Therefore, the previous study [Citation12] showed that the efficacy of HIFU treatment was equivalent to that of LM, and our study suggested that the pregnancy outcomes of patients treated with HIFU were also equivalent to the patients treated with LM. Uterine fibroids may cause miscarriages; Klatsky [Citation14] and Radhika [Citation15] reported the miscarriage rate in patients with uterine fibroids was 20%∼46.7%. In our study, the miscarriage rate was 17.7% (20/113) in the group of patients treated with HIFU, and it was 13.7% (20/146) in the group of patients treated with LM (). Our results demonstrated that both HIFU and LM improved the pregnancy outcomes of patients with uterine fibroids.
The cesarean section rate was 80.6% (50/62) in the HIFU treatment group and the cesarean 82.2% (83/101) in the LM treatment group. While both appear high, no significant difference was observed in cesarean delivery rate between the two groups. Among the patients who had cesarean section, 18 (36.0%, 18/50) patients treated with HIFU and 33 (39.8%, 33/83) patients treated with LM were patients with uterus scars. That is to say, these patients had histories of cesarean delivery, which may impact their choice of delivery. In our study, all of them chose cesarean delivery due to the fear of uterine rupture. In HIFU group, 16 (32.0%, 16/50) patients chose cesarean delivery due to the lack of evidence of vaginal delivery successfully after HIFU treatment and patients preferred cesarean delivery because they believed it would be safer than vaginal delivery. However, recent data has been updating as the number of successful vaginal delivery cases after HIFU increases [Citation2]. In addition, no uterine ruptures were observed after HIFU or LM in this study. Lower preterm birth rate and postpartum hemorrhage rate also suggest the efficacy and safety in pregnancy and delivery after both treatments.
The advantages of HIFU treatment for uterine fibroids included fewer complications, shorter hospital stays, lower postoperative pain, and faster recovery in comparison with surgical treatment, thus greatly improving the quality of life of patients [Citation16]. Our results revealed that the pregnancy interval after HIFU was significantly shorter than that after LM (10 months VS. 13 months). Although LM could effectively reduce the rate of miscarriage and improve the live-birth rate, it could injure the normal uterine muscle and demands a longer recovery time before pregnancy [Citation17]. One of the advantages of HIFU treatment is the ability to maximally maintain uterine wall integrity.
However, this study is limited because it is a retrospective observational study. Although HIFU had a shorter pregnancy interval than LM, and the other main demographic characteristics showed no differences in the two groups, some other unexpected factors may have existed and affected the results. Moreover, many patients in our department did not have MRI or ultrasonography imagings to evaluate the volume changes of the treated fibroids, so we could not show the efficacy by volume reduction of the fibroids after HIFU treatment. Finally, the choice of delivery was affected by patients with uterine scars and social factors, which led to a higher cesarean section rate. In the future, prospective, randomized, and multi-center studies with a large number of patients and full follow-up data including MRI are needed.
Conclusion
Based on the results of patients with uterine fibroids treated with HIFU or LM, it appears that both HIFU and LM are safe and effective in treating patients with uterine fibroids who wish to conceive. Both HIFU and LM have improved the pregnancy outcomes of patients with uterine fibroids. Compared with LM, HIFU treatment has the advantages of no blood loss, no new scar, and shorter pregnancy interval. HIFU is a promising alternative treatment for patients with uterine fibroids who wish to have a baby.
Supplemental Material
Download MS Excel (12.7 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Lethaby A, Vollenhoven B. Fibroids (uterine myomatosis, leiomyomas). BMJ Clin Evid. 2015;2015:0814.
- Zou M, Chen L, Wu C, et al. Pregnancy outcomes in patients with uterine fibroids treated with ultrasound-guided high-intensity focused ultrasound. BJOG: Int J Obstet Gy. 2017;124:30–35.
- Lebovitz O, Orvieto R, James KE, et al. Predictors of reproductive outcomes following myomectomy for intramural fibroids. Reprod Biomed Online. 2019;39(3):484–491.
- King R, Overton C. Management of fibroids should be tailored to the patient. Practitioner. 2011;255:19–23, 2-3.
- Donnez J, Dolmans MM. Uterine fibroid management: from the present to the future. Hum Reprod Update. 2016;22(6):665–686.
- Koo YJ, Lee JK, Lee YK, et al. Pregnancy outcomes and risk factors for uterine rupture after laparoscopic myomectomy: a single-center experience and literature review. J Minim Invasive Gynecol. 2015;22(6):1022–1028.
- Huang Y, Deng J, Wei X, et al. A comparison of reproductive outcomes of patients with adenomyosis and infertility treated with high-intensity focused ultrasound and laparoscopic excision. Int J Hyperthermia. 2020;37(1):301–307.
- Qin J, Chen JY, Zhao WP, et al. Outcome of unintended pregnancy after ultrasound-guided high-intensity focused ultrasound ablation of uterine fibroids. Int J Gynaecol Obstet. 2012;117(3):273–277.
- Malcolm GM, Hilary OD, Michael SB, et al. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynecol Obstet. 2011;113:3–13.
- Spies JB, Coyne K, Guaou NG, et al. The UFS-QOL, a new disease-specific symptom and health-related quality of life questionnaire for leiomyomata. Obstet Gynecol. 2002;99(2):290–300.
- Huang X, Yu D, Zou M, et al. The effect of exercise on high-intensity focused ultrasound treatment efficacy in uterine fibroids and adenomyosis: a retrospective study. BJOG: Int J Obstet Gy. 2017;124:46–52.
- Liu Y, Ran W, Shen Y, et al. High-intensity focused ultrasound and laparoscopic myomectomy in the treatment of uterine fibroids: a comparative study. BJOG: Int J Obstet Gy. 2017;124:36–39.
- Verpalen IM, Anneveldt KJ, Nijholt IM, et al. Magnetic resonance-high intensity focused ultrasound (MR-HIFU) therapy of symptomatic uterine fibroids with unrestrictive treatment protocols: a systematic review and meta-analysis. Eur J Radiol. 2019;120:UNSP:108700.
- Klatsky PC, Tran ND, Caughey AB, et al. Fibroids and reproductive outcomes: a systematic literature review from conception to delivery. Am J Obstet Gynecol. 2008;198(4):357–366.
- Radhika BH, Naik K, Shreelatha S, et al. Case series: pregnancy outcome in patients with uterine fibroids. J Clin Diagn Res. 2015;9(10):QR01–QR04.
- Zhang C, Jacobson H, Ngobese ZE, et al. Efficacy and safety of ultrasound-guided high intensity focused ultrasound ablation of symptomatic uterine fibroids in Black women: a preliminary study. BJOG: Int J Obstet Gy. 2017;124:12–17.
- Campo S, Campo V, Gambadauro P. Reproductive outcome before and after laparoscopic or abdominal myomectomy for subserous or intramural myomas. Eur J Obstet Gynecol Reprod Biol. 2003;110(2):215–219.