Abstract
Purpose
Multiple attempts have been made to manage the pancreatic stump and the pancreatic duct in order to reduce the rate of postoperative pancreatic fistula (POPF) after pancreaticoduodenectomy (PD), however radiofrequency-based technologies could help to achieve this goal. Previous encouraging clinical and experimental results support the use of endoluminal thermal ablation (ETHA) of the main pancreatic duct to reduce pancreatic exocrine secretion and hence POPF. We here describe our initial clinical experience with ETHA of the main pancreatic duct in two cases at high risk of POPF.
Methods
Two cases underwent PD for malignancy with a high risk of POPF (adenocarcinoma, obese patients, surgical difficulties with heavy intraoperative blood loss, soft pancreas or walled-off pancreatitis and a tight small pancreatic main duct). In both cases, ETHA of the main pancreatic duct was conducted intraoperatively just before Blumgart-type pancreatic-jejunal anastomosis using a ClosureFast catheter (Medtronic, Mansfield, MA, USA) normally used for varicose vein treatment (therefore an off-label use).
Results
Although a clear radiological POPF was detected in the second case, the clinical postoperative course in both cases was uneventful. Little pancreatic fluid collected in the abdominal drainage with low levels of amylase enzyme, confirming low exocrine pancreatic function. No other procedure-related complications were detected.
Conclusion
Endoluminal thermal ablation of the main pancreatic duct may be a feasible and safe technique to reduce the adverse effects of POPF after PD.
1. Introduction
Postoperative pancreatic fistula (POPF) remains the most important complication and cause of procedure-related death after pancreaticoduodenectomy (PD) [Citation1,Citation2]. Although several alternatives have been described, the pancreatic remnant is usually sutured to the gastrointestinal tract, which means that the incidence of POPF remains high [Citation1]. Pancreatico-enteric anastomosis therefore still continues to be challenging and suggests that a more effective technique should be developed to avoid this complication. Some risk factors related to POPF include a high body mass index (BMI), long operative time, heavy blood loss as well as pancreatic texture and the diameter of the main pancreatic duct [Citation3]. In a prospective randomized study, POPF was reported in 42% of cases of soft pancreas and main pancreatic duct diameter < 3 mm, with a reoperation rate of 10% [Citation4].
Although many techniques developed to avoid POPF have been described in the literature, such as occlusion of the main pancreatic duct by glue or ligation, the incidence of this complication remains high. Our experience with a porcine experimental model suggests that radiofrequency (RF) energy can be more effective in closing the pancreatic stump than a mechanical stapler [Citation5,Citation6]. We recently reported that endoluminal thermal ablation (ETHA) of the main pancreatic duct in pigs using an RF bipolar catheter can be more effective than glue in occluding the duct, as shown by the degree of atrophy and fewer postoperative pancreatic fistulas [Citation7]. All these findings suggest that an energy-based high-temperature ablative technique could be used to occlude the main pancreatic duct during PD, just before pancreatico-enteric anastomosis, in order to reduce the risk of POPF. We here describe two clinical cases in which ETHA was conducted for this purpose.
2. Methods
2.1. Human subjects
The two reported cases are included in a retrospective review which was approved by the Clinical Research and Ethics Committee of the Hospital del Mar (Barcelona, Spain) and conducted in accordance with principles of the Declaration of Helsinki. The informed consent requirement was not necessary in this case but the removal of any patient identifier was ensured.
2.2. Ablative technique
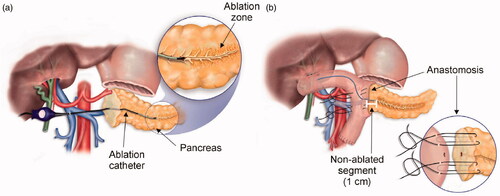
Endolumnal thermal ablation (ETHA) of the main pancreatic duct was performed by the off-label use of the ClosureFast system (Medtronic, Mansfield, MA, USA), originally designed to treat varicose veins [Citation8]. The ClosureFast applicator consists of a 7 F catheter with a coil on its surface which is heated by the passage of RF current through the coil itself [Citation9]. This means that no electrical RF current flows into the tissue and heat is applied only to the tissue surrounding the device, so that the term “radiofrequency ablation” applied to the ClosureFast system may be confusing. In both clinical cases several overlapped 60-s applications were applied to the main pancreatic duct programming a target temperature of 120 °C (see video in supplementary material). The catheter was fully inserted through the pancreatic duct and slowly withdrawn during the double heating cycles (see ), as in treating varicose veins, avoiding ablation over the last proximal centimeter. After completing the ablation zone around the main pancreatic duct, a pancreatico-enteric anastomosis was conducted (see ).
3. Results
3.1. Case 1
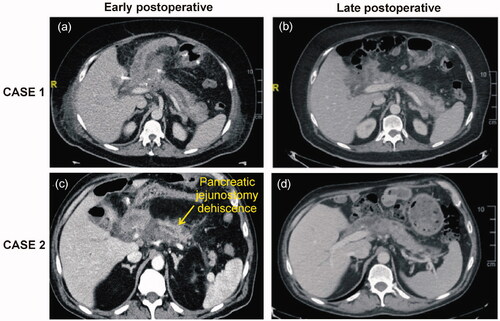
A 56-year-old man with a BMI of 30.2 was admitted to our center (Hospital del Mar-IMIM, Barcelona, Spain) with painless jaundice in February 2020. Computerized tomography (CT) showed a 2.7 cm mass in the pancreatic head, considered as resectable. Abdominal magnetic resonance (MR) revealed a main pancreatic duct <2 mm in diameter. A biliary stent was endoscopically placed to reduce jaundice and PD was indicated. During surgery, an important peripancreatic and liver hilum edema component was observed mainly due to the cancer itself and the biliary stent associated with very soft pancreas texture. As the association of a long intervention (almost 5 h), soft pancreas and confirmation of the main pancreatic diameter <2 mm suggested a very high likelihood of developing POPF, we decided to perform ETHA of the main pancreatic duct prior to Blumgart-type pancreatico-jejunal anastomosis with abdominal drainage. The postoperative period was uneventful, with slightly elevated amylase levels (40 IU/L) in the drainage fluid on the 3rd postoperative day, with a mean drainage output of 20 cc per day and a normal CT scan (). Drainage was removed on the 10th postoperative day and the patient was discharged 2 days later. Histopathological examination revealed a pT3N1 moderately differentiated adenocarcinoma with all margins being negative. One month after surgery, fecal elastase was 64 m μg/gr, demonstrating exocrine pancreatic insufficiency due to ETHA. To date, the patient has had no further symptoms related to exocrine pancreatic insufficiency such as steatorrhea or the need for substitute pancreatic enzymes.
3.2. Case 2
A 58-year-old man with a BMI of 31.2 was admitted to our center with epigastric pain, oral intolerance and weight loss. CT showed a 3.6 cm mass in the uncinate process of the pancreas infiltrating the duodenum and a main pancreatic duct < 2 mm in diameter. The tumor was assessed as resectable and the patient was scheduled for PD. Dissection of the pancreas was challenging, mainly due to a desmoplastic reaction of the liver hilum and upper border of the pancreatic head and deep extension of the tumor to the mesopancreas. After sectioning the pancreatic neck, an extremely soft fragile pancreas remnant and a pancreatic duct <2 mm were observed. Considering the very high risk of POPF, we performed ETHA of the main pancreatic duct prior to Blumgart-type pancreatic-jejunal anastomosis. Amylase determination in the abdominal drainage on the 3rd postoperative day was 193 IU/L with drainage output of 15 cc/day. A CT scan was thereafter performed, observing complete dehiscence of the pancreatic-jejunal anastomosis (). Despite the dehiscence, the postoperative course was uneventful with the progressive reduction of drainage output. Histopathological examination showed a mixed neuroendocrine-adenocarcinoma pT3N1 tumor with free margins. At 1 month after surgery, fecal elastase was <15 μg/gr.
4. Discussion
POPF is still a relevant complication after pancreatic resection and can lead to severe secondary complications such as intra-abdominal abscess, hemorrhage, lengthy hospital stays and impaired patient quality of life [Citation2]. Several attempts have been made in the past to reduce POPF, including ligation, section and injecting glue into the pancreatic duct [Citation10]. However, none of these techniques have been shown to be more effective than pancreatic-enteric anastomosis to manage the pancreatic stump after PD [Citation2]. In fact, similar complication rates were found with no differences in exocrine insufficiency rates in a recent randomized controlled PD trial comparing glue occlusion versus pancreaticojejunostomy. Other sealing methods, such mechanical staples or conventional ligatures have provided similar results [Citation6,Citation11].
Our group investigated the efficacy of ETHA in managing the pancreatic stump and occluding the main pancreatic duct in pigs, achieving exocrine pancreatic atrophy [Citation7]. ETHA has also been shown to be clinically effective for vessel occlusion, as in the treatment of varicose veins. In this setting, this study reports what we believe to be the first cases of ETHA of the pancreatic duct after PD in humans. ETHA effectiveness seems to be based on the shrinkage of the vessel wall and more specifically on achieving the denaturation of collagen and other proteins by a controlled rise of temperature using a technique that has achieved complete occlusion of 98.4% of the vessels [Citation12,Citation13]. Given the morphological similarity in the structure of the vessels and the pancreatic duct, we considered that an efficient ETHA could achieve complete obstruction of the pancreatic duct and eliminate the exocrine function, thus avoiding POPF in the absence of functional exocrine secretion.
As in our previous success with ETHA in animal models for distal pancreatectomy, the effectiveness of this procedure was shown by the complete occlusion of the major pancreatic duct observed in all the animals during necropsy when compared with glue occlusion [Citation7,Citation14]. Our previous study with animal models had also shown that ETHA was a safe technique, as none of the animals suffered pancreatitis or endocrine insufficiency [Citation7].
The two patients subjected to ETHA were obese, presented surgical difficulties and had a very soft pancreas texture with a small main pancreatic duct, all of which are recognized high-risk POPF factors, and pathological examination of the specimen revealed a fatty infiltration of the pancreatic parenchyma. As the probability of these patients’ developing POPF could be as high as 50% [Citation2,Citation15] we decided to perform ETHA in these 2 cases while preserving the last 1 cm of the main pancreatic duct to perform pancreato-enteric anastomosis.
The technical success of the procedure was clear in the early postoperative CT scan performed at 7 days from the surgery, which detected a hypodensity line along the main pancreatic duct related to ETHA (). At 1 and 6 months after the procedure CT images showed only a slight atrophy of the pancreatic parenchyma (). In both cases, a clinical follow-up of 8 and 9 months was carried out, respectively. Safety is paramount when introducing new indications of a technique. As in our previous experimental studies [Citation7], neither of the present two cases showed technique-complications during the follow-up, such as pancreatitis or pancreatic endocrine insufficiency. We also performed pancreatico-enteric anastomosis with a duct-mucosa suture while maintaining the vitality of the last centimeter of the pancreatic duct.
Interestingly, the second case showed a radiological image of pancreatic fistula. clearly shows dehiscence between the jejunum and the pancreatic margin. In this patient, a clinically relevant POPF was expected with a high amylase level in the drainage fluid. However, on the contrary, the amylase drainage level was only slightly elevated (193 IU/L) and the POPF evolved without complications, while a scarce amount of pancreatic fluid collected in the drainage, with a mean of almost 15 cc/day, thus confirming the effectiveness of ETHA. On the late postoperative CT image (6 months), we found that this dehiscence was almost completely resolved ().
We have therefore shown that ETHA significantly reduces the exocrine function of the pancreas. Using fecal elastase levels at 30 postoperative days as a marker of exocrine function both patients had low levels (< 200 μg/g), which we associate with the POPF’s low clinical relevance. Six months after surgery, the patients have had no further symptoms related to exocrine pancreatic insufficiency such as steatorrhea or the need for substitute pancreatic enzymes, in spite of the fact that clinically diagnosed pancreatic insufficiency is observed in approximately 25 − 50% of those following a PD [Citation14].
ETHA can be potentially delivered intraoperatively as described in this report or preoperatively through an endoscopic approach. In this case, the catheter could be introduced (as per endoscopic retrograde cholangiopancreatography, ERCP) through the papilla and gently advanced into the Wirsung duct, as has been described in treating endoluminal pancreatic tumors [Citation15]. This technique could become relevant in high risk POPF with a small main pancreatic duct and a soft/friable pancreatic parenchyma, as in the 2 previously described cases. However, the technique should be further improved, since none of the existing catheters were specifically developed for the main pancreatic duct. Should ETHA be widely adopted for this procedure, in the future different catheter sizes should be available to better fit the main pancreatic duct. However, these results are insufficient to draw firm conclusions, although these promising data merit being confirmed in future controlled studies which we plan to carry out.
5. Conclusions
This study has shown that ETHA of the main pancreatic duct could be an alternative technique to reduce the adverse effects of POPF after PD. These results need to be confirmed by longer series and randomized trials.
Disclosure statement
The authors have no conflict of interests to disclose. The present study was not sponsored/promoted by external parties.
Additional information
Funding
References
- Kleeff J, Diener MK, Z'graggen K, et al. Distal pancreatectomy: risk factors for surgical failure in 302 consecutive cases. Ann Surg. 2007;245(4):573–582.
- Mauriello C, Polistena A, Gambardella C, et al. Pancreatic stump closure after pancreatoduodenectomy in elderly patients: a retrospective clinical study. Aging Clin Exp Res. 2017;29(S1):35–40.
- Bassi C, Dervenis C, Butturini G, et al.; International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138(1):8–13.
- Kamarajah SK, Bundred JR, Lin A, et al. PARANOIA Study Group. Systematic review and meta-analysis of factors associated with post-operative pancreatic fistula following pancreatoduodenectomy. ANZ J Surg. 2020. Epub ahead of print.
- Dorcaratto D, Burdío F, Fondevila D, et al. Radiofrequency is a secure and effective method for pancreatic transection in laparoscopic distal pancreatectomy: results of a randomized, controlled trial in an experimental model. Surg Endosc. 2013;27(10):3710–3719.
- Burdío F, Dorcaratto D, Hernandez L, et al. Radiofrequency-induced heating versus mechanical stapler for pancreatic stump closure: in vivo comparative study. Int J Hyperthermia. 2016;32(3):272–280.
- Andaluz A, Ewertowska E, Moll X, et al. Endoluminal radiofrequency ablation of the main pancreatic duct is a secure and effective method to produce pancreatic atrophy and to achieve stump closure. Sci Rep. 2019;9(1):5928.
- Almeida JI, Kaufman J, Göckeritz O, et al. Radiofrequency endovenous ClosureFAST versus laser ablation for the treatment of great saphenous reflux: a multicenter, single-blinded, randomized study (RECOVERY study). J Vasc Interv Radiol. 2009;20(6):752–759.
- Bauzá Moreno H, Dotta M, Katsini R, et al. Endovascular radiofrequency ablation. Effect on the vein diameter using the ClosureFast(®) catheter. Cir Esp. 2016;94(6):353–357.
- Mazzaferro V, Virdis M, Sposito C, et al. Permanent pancreatic duct occlusion with neoprene-based glue injection after pancreatoduodenectomy at high risk of pancreatic fistula: a prospective clinical study. Ann Surg. 2019;270(5):791–798.
- Diener MK, Seiler CM, Rossion I, et al. Efficacy of stapler versus hand-sewn closure after distal pancreatectomy (DISPACT): a randomised, controlled multicentre trial. Lancet. 2011;377(9776):1514–1522.
- Braithwaite B, Hnatek L, Zierau U, et al. Radiofrequency-induced thermal therapy: results of a European multicentre study of resistive ablation of incompetent truncal varicose veins. Phlebology. 2013;28(1):38–46.
- Lane T, Bootun R, Dharmarajah B, et al. A multi-centre randomised controlled trial comparing radiofrequency and mechanical occlusion chemically assisted ablation of varicose veins - Final results of the Venefit versus Clarivein for varicose veins trial. Phlebology. 2017;32(2):89–98.
- Alfieri S, Quero G, Rosa F, et al. Indications and results of pancreatic stump duct occlusion after duodenopancreatectomy. Updates Surg. 2016;68(3):287–293.
- Vanella G, Capurso G, Arcidiacono PG. Endosonography-guided radiofrequency ablation in pancreatic diseases: time to fill the gap between evidence and enthusiasm. J Clin Gastroenterol. 2020;54(7):591–601.