Abstract
Background
Heatstrokes are a serious threat to human health, particularly the cardiovascular system. Understanding the clinical features and risk factors related to death in patients with myocardial injury (MI) complicated by heat stroke is crucial.
Method
This study included the baseline data of all patients with severe heatstroke between October 2008 and May 2019.
Results
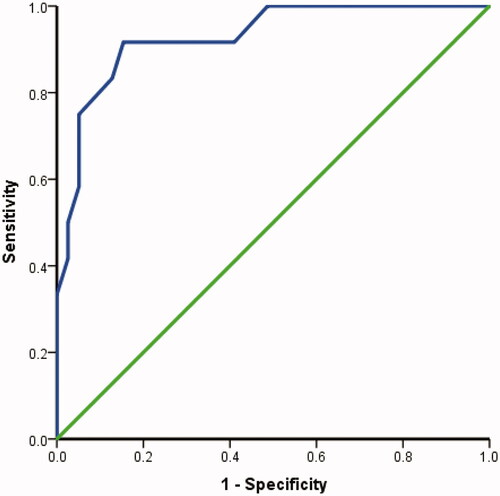
Of the 162 patients enrolled, 75 (46.3%) were in the MI group and 87 (53.7%) were in the non-MI group. A significant difference was noted in 90-day survival between the two groups even after correction for Age, Acute Physiology, and Chronic Health Evaluation II (APACHE II) scores, Sequential Organ Failure Assessment (SOFA) scores, Glasgow Coma Score (GCS), and activated partial thromboplastin time (before correction (p < .001; after correction, p = .023). Survival analysis showed that the 90-day survival time of patients with MI was shorter than that of patients without MI (p < .001). The area under the receiver operating characteristic (ROC) curve for predicting mortality based on the SOFA score was 92.8% (95% CI 0.847–1.000, p < .001), the optimal cutoff value was 7.5, the sensitivity was 91.7%, and the specificity was 94.6%.
Conclusion
Patients with heatstroke having MI had more severe clinical conditions, 90-day mortality was significantly increased, and the survival time was shortened. A high SOFA score is an independent risk factor for death in patients with heatstroke having MI, with an optimal cutoff value of 7.5, sensitivity of 91.7%, and specificity of 94.6%.
Introduction
Heatstroke is a serious threat to human health, with multiple organ dysfunction syndrome and a mortality rate of 20–70% [Citation1,Citation2]. The cardiovascular system is a vital target organ of heat injury [Citation3,Citation4], and the incidence of myocardial injury (MI) is as high as 43.4–65.2% [Citation5]. The regulation of the cardiovascular system plays a key role in the pathogenesis of heatstroke. Factors involved in multiple-organ dysfunction syndrome include abnormal temperature regulation, blood pressure, and perfusion function [Citation6]. At present, reports on the clinical characteristics and prognosis of heatstroke complicated with MI are limited. In this study, we retrospectively collected the clinical and prognostic data of heatstroke patients admitted to the intensive care unit of a third-class hospital in China over 10 years. However, the related risk factors for death in patients with concurrent MI were analyzed to provide a reference for timely and effective clinical treatment.
Methods
Study design and participants
This single-center retrospective cohort study included all patients with severe heatstroke admitted to the ICU of the General Hospital of Southern Theater Command of PLA between October 2008 and May 2019. This study was approved by the Ethics Committee of the General Hospital of the Southern Theater Command (Number: Hospital Ethics [2020]-9), and the need to obtain informed consent was waived.
The inclusion criteria were as follows: (1) age ≥ 18 years; (2) met the diagnostic criteria for severe heatstroke described below; (3) had complete data regarding the clinical manifestations of cardiac markers; (4) the diagnostic criteria for severe heat stroke were as follows: classic or exertional heat stroke with a history of exposure to hot and humid weather or strenuous activity, concurrent hyperthermia (central temperature above 40 °C), and neurological dysfunction, including delirium, cognitive disorders, and disturbed consciousness. The exclusion criteria were existing irreversible underlying diseases affecting mortality, pregnancy, or breastfeeding.
Research procedures
The baseline data of the patients were collected, including inflammatory and organ function parameters on admission, and the Acute Physiology and Chronic Health Evaluation II (APACHE II) scores, Sequential Organ Failure Assessment (SOFA) scores, and Glasgow Coma Score (GCS) were also collected. We divided all patients into MI and non-MI groups according to whether they had MI. The main result was the 90-day mortality. Survival curve analysis was also performed. The MI group was further divided into survivor and nonsurvivor subgroups, and the characteristics of the subgroups were compared to investigate risk factors for mortality.
Definitions
Diagnostic criteria for MI: plasma cardiac troponin I (CTN I) > 0.1 ng/mL was considered as MI [Citation7].
Statistical analysis
Categorical data are expressed as numbers and percentages, and intergroup comparisons were performed using the Mann–Whitney U test, χ2 test, or Fisher’s exact test. Continuous variables are expressed as medians and interquartile ranges. Continuous data with a Gaussian distribution were compared using Student’s t test or one-way ANOVA, and those with a non-Gaussian distribution were compared using the Wilcoxon rank-sum test. The patient endpoint event was death within 90 days of onset. Survival curves were drawn using the Kaplan–Meier method. Significant indicators were identified using single-factor analysis, and those with p < .1, were included in the multifactor Cox regression model. The forward selection was used to gradually eliminate them. The impact of each indicator on prognosis was analyzed, and prognostic risk factors were identified. ROC curves were used to predict the prognosis of patients with severe heat stroke complicated with MI to evaluate the significance of the effects of independent risk factors on clinical prognosis. Statistical analyses were performed using SPSS Windows v11.0 (SPSS, Chicago, IL, USA), and a two-tailed p < .05 was considered statistically significant.
Results
Demographics and baseline characteristics
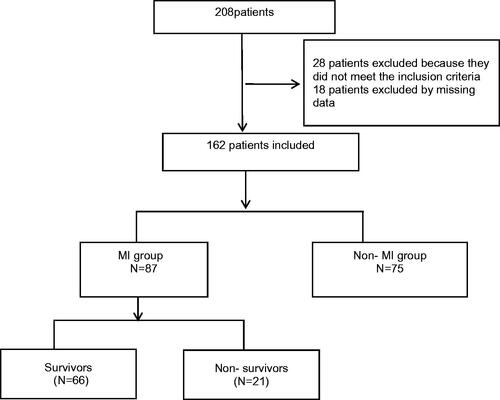
Data from 208 patients were analyzed. After screening, 28 patients were excluded because they did not meet the inclusion criteria, 18 patients were excluded due to missing data, and 162 patients were finally included (). All 162 patients were male, with a median age of 21.0 years (IQR 19.0–27.0), APACHE II scores of 12.0 (IQR 8.0–17.0), SOFA scores of 4.0 (IQR 2.0–6.5), and GCS score of 12.0 (IQR 6.5–14.0). A total of 75 patients (46.3%) did not have MI, and 87 patients (53.7%) had MI.
Comparison of groups
Compared with those patients without MI, patients with MI had higher APACHE II scores [median 16.0 (IQR 13.0–22.0) vs. 8.0 (IQR 7.0–11.0)] and SOFA scores [median 6.0 (IQR 3.0–9.0) vs. 2.0 (IQR 2.0–4.0)], and lower GCS [median 8.0 (IQR 5.0–12.0) vs. 13.5 (IQR 12.0–14.0)]. The MI group had severe organ damage, including damage to the liver, kidneys, and coagulation system (all p < .05, ).
Table 1. Baseline characteristics of clinical and laboratory findings in MI group and Non-MI group.
Main outcomes
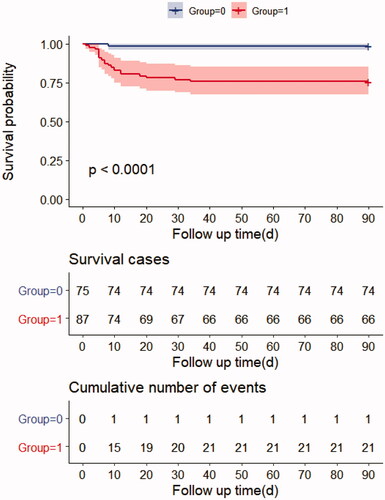
The 90-day mortality rate in the MI group was 24% (21/87) and in the non-MI group was 1.3% (1/75), and the difference was significant even after correction for age, APACHE II score, SOFA score, GCS, and activated partial thromboplastin time (before correction p < .001; after correction p = .023) (). Survival analysis showed that the 90-day survival time of patients with MI was shorter than that of patients without MI (p < .001) ().
Table 2. Outcomes of non-MI group and MI group.
Subgroup analysis
In the subgroup analysis of the MI group, there were 66 survivors (75.9%) and 21 nonsurvivors (24.1%). Compared with survivors, nonsurvivors had higher APACHE II scores (median 14.0 [IQR 12.0–18.0] vs. 22.5 [IQR 18.5–24.8]), higher SOFA scores (median 4.0 [IQR 3.0–6.0] vs 12.5 [IQR 9.3–15.0]), and lower GCS scores (median 9.0 [IQR 6.0–12.0] vs 4.0 [IQR 3.0–7.0]). In addition, the liver and blood coagulation systems were more serious in the nonsurvivors (p < .05, ).
Table 3. Baseline characteristics of survivors and non-survivors in patients with MI.
Risk factor analysis
The multivariate Cox risk regression model showed that the SOFA score was an independent risk factor for the survival of patients with MI (). The area under the ROC curve for the prediction of mortality based on SOFA scores was 92.8% (95% CI 0.847–1.000, p < .001), the optimal cutoff value was 7.5, the sensitivity was 91.7%, and the specificity was 94.6% ().
Table 4. Risk factors for death in MI patients with severe heat stroke.
Discussion
The results of this retrospective cohort study revealed that patients with severe heat stroke complicated by MI had more severe clinical conditions, significantly increased 90-day mortality, and shortened survival. Multivariate Cox regression analysis revealed that an increased SOFA score was an independent risk factor for death in patients with heatstroke complicated by MI. The cutoff value for the SOFA score predicted by the ROC curve was 7.5, with a sensitivity of 91.7% and a specificity of 94.6%.
Severe heatstroke can lead to multiple organ dysfunctions, of which the heart is considered one of the most vulnerable. During a heatstroke, the central vascular system is involved in whole-body heat dissipation response and organ perfusion. The body increases myocardial contractility, accelerates heart rate, and increases cardiac output to increase perspiration and heat dissipation [Citation8–10]. In heatstroke, cardiac function is affected by the thermoregulatory center and nervous system. The degree of myocardial damage is related to temperature, duration, and disease of heatstroke. CTNI is an important biomarker for the early evaluation of myocardial cell injury after heat stroke, with high sensitivity and specificity [Citation11], and we used this indicator to assess whether heatstroke patients were associated with MI. The proportion of heart dysfunction caused by heatstrokes can be as high as 43.4% to 65.2% [Citation5]; in our study, 53.7% of heatstroke patients had complicated MI. Heat shock can directly lead to degeneration and necrosis of cardiomyocytes, weakened antioxidant capacity of heart tissues, and elevated levels of cardiac proinflammatory factors, leading to myocardial ischemia, arrhythmias, circulatory disorders, heart failure, multiorgan dysfunction, and other life-threatening conditions [Citation12,Citation13]. Our study also found that compared with the non-MI group, the MI group had more severe clinical diseases, including liver damage, kidney damage, abnormal blood coagulation system, and inflammation; in the 90-day survival analysis, the mortality in the MI group increased significantly (13%).
Multivariate Cox regression analysis indicated that the SOFA score was an independent risk factor for death in patients with severe heat stroke combined with MI. The SOFA score is a measure of multiple organ dysfunction; the higher the score, the more severe the patient [Citation14]. The SOFA score can better reflect and predict the disease severity and prognosis of critically ill patients and is widely used in the clinical practice [Citation15]. In this study, the SOFA score of patients with heatstroke combined with MI was higher in the nonsurvivor group than in the survivor group, indicating that the disease severity was consistent with the fatality rate. The cutoff value for the ROC curve prediction SOFA score was 7.5, with a sensitivity of 91.7% and specificity of 94.6%, suggesting that a SOFA score >7.5 increases the risk of death in patients. Thus, early clinical assessment of the overall condition is crucial in patients with heatstroke and diagnostic prognosis for early cardiac protection. Clinically, for patients with heatstroke, timely SOFA scoring on admission to determine the cutoff point can assess the prognosis of their condition as soon as possible and timely targeted symptomatic and organ protection treatment.
In addition, many other studies have explored the subject of myocardial infarction [Citation10]. Our study differs from them. First, the two papers looked at the complications of heatstroke differently. The main research of one article [Citation10] was acute myocardial infarction among hospitalizations for heat stroke, whereas our paper focused on exertional heatstroke complicated with MI. Second, in our study, we retrospectively collected the clinical and prognostic data of heatstroke patients admitted to the ICU of a third-class hospital in China over 10 years. We divided the patients into MI and non-MI groups. We followed up with the two groups of patients and analyzed the outcomes at 90 days. In addition, the MI group was further divided into survivor and nonsurvivor subgroups, and the characteristics of the subgroups were compared with investigating risk factors for mortality, and the optimal cutoff value was also analyzed.
This study has certain limitations. This was a single-center retrospective cohort study with a relatively small number of patients. All the patients were male, which failed to fully reflect the overall population and may have reduced the reliability of the statistical analysis. Future studies should include a larger sample size with both sexes.
Conclusions
Heatstrokes with MI had more severe clinical conditions, the 90-day mortality was significantly increased, and the survival time was shortened. A high SOFA score was an independent risk factor for death in heatstrokes with MI, with an optimal cutoff value of 7.5, with a sensitivity of 91.7% and a specificity of 94.6%.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Lei S. Review and enlightenment on the prevention and treatment of heatstroke. PLA Med J. 2011;36(09):883–885.
- Epstein Y, Yanovich R. Heatstroke. N Engl J Med. 2019;380(25):2449–2459.
- Lou Y, Lin H, Wang H, et al. [Research progress in the heatstroke-induced myocardial injury]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2019;31(10):1304–1306.
- Ko WC, Lin CH, Lee JJ, et al. Therapeutic hypothermia protects against heat stroke-induced arterial hypotension via promoting left ventricular performance in rats. Int J Med Sci. 2020;17(4):525–535.
- Leon LR, Bouchama A. Heat stroke. Compr Physiol. 2015;5(2):611–647.
- Low DA, Keller DM, Wingo JE, et al. Sympathetic nerve activity and whole body heat stress in humans. J Appl Physiol. 2011;111(5):1329–1334.
- Jacob JA. New sepsis diagnostic guidelines shift focus to organ dysfunction. Jama. 2016;315(8):739–740.
- Pease S, Bouadma L, Kermarrec N, et al. Early organ dysfunction course, cooling time and outcome in classic heatstroke. Intensive Care Med. 2009;35(8):1454–1458.
- Hifumi T, Kondo Y, Shimizu K, et al. Heat stroke. J Intensive Care. 2018;6(1):30.
- Bathini T, Thongprayoon C, Chewcharat A, et al. Acute myocardial infarction among hospitalizations for heat stroke in the United States. J Clin Med. 2020;9(5):1357.
- Hausfater P, Doumenc B, Chopin S, et al. Elevation of cardiac troponin I during non-exertional heat-related illnesses in the context of a heatwave. Crit Care. 2010;14(3):R99.
- Xingxing H, Zhifeng L, Lei S. Research progress on the mechanism of heart injury in heatstroke. Chin Elec J Crit Care Med. 2018;4(4):363–367.
- Bouchama A, Ollivier V, Roberts G, et al. Experimental heatstroke in baboon: analysis of the systemic inflammatory response. Shock. 2005;24(4):332–335.
- Lambden S, Laterre PF, Levy MM, et al. The SOFA score-development, utility and challenges of accurate assessment in clinical trials. Crit Care. 2019;23(1):374.
- Ferreira FL, Bota DP, Bross A, et al. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286(14):1754–1758.