Abstract
Background
This study aimed to explore the prognostic role of pan-immune-inflammation value (PIV) and develop a new risk model to guide individualized adjuvant systemic treatment following radiofrequency ablation (RFA) for early-stage hepatocellular carcinoma (HCC).
Materials and methods
Patients with early-stage HCC treated by RFA were randomly divided into training cohort A (n = 65) and testing cohort B (n = 68). Another 265 counterparts were enrolled into external validating cohort C. Various immune-inflammatory biomarkers (IIBs) were screened in cohort A. Prognostic role of PIV was evaluated and validated in cohort B and C, respectively. A nomogram risk model was built in cohort C and validated in pooled cohort D. Clinical benefits of adjuvant anti-angiogenesis therapy plus immune checkpoint inhibitor (AA-ICI) following RFA was assessed in low- and high-risk groups.
Results
The cutoff point of PIV was 120. High PIV was an independent predictor of unfavorable recurrence-free survival (RFS) and overall survival (OS). RFS and OS rates of patients with high PIV were significantly lower than those with low PIV both in cohort B (PRFS=0.016, POS=0.011) and C (PRFS<0.001, POS<0.001). The nomogram model based on PIV, tumor number and BCLC staging performed well in risk stratification in external validating cohort C. Adjuvant AA-ICI treatment showed an added benefit in OS (p = 0.011) for high-risk patients.
Conclusions
PIV is a feasible independent prognostic factor for RFS and OS in early-stage HCC patients who received curative RFA. The proposed PIV-based nomogram risk model could help clinicians identify high-risk patients and tailor adjuvant systemic treatment and disease follow-up scheme.
HIGHLIGHTS
Key findings
High pan-immune-inflammation value (PIV) is an independent indicator of unfavorable recurrence-free survival (RFS) and overall survival (OS) for early-stage hepatocellular carcinoma (HCC) patients who received curative radiofrequency ablation (RFA).
Adjuvant anti-angiogenesis target therapy plus immune checkpoint inhibitor (AA-ICI) treatment showed added benefit in OS for the high-risk patients defined by a nomogram risk model based on PIV, tumor number and BCLC staging.
What is known and what is new?
Inflammation and impaired host immunity are associated with carcinogenesis and progression of HCC. Increasing evidences showed that immune-inflammatory biomarkers (IIBs) had prognostic roles in early-stage HCC patients who received RFA. However, prognostic potential of PIV has not been determined in this setting.
Herein, high PIV was first reported to be an independent risk factor of poor RFS and OS in early-stage HCC patients treated by curative RFA and helped to discriminate patients between low- and high-risk groups. Adjuvant AA-ICI treatment following RFA was beneficial to OS of patients in the high-risk group.
What is the implication, and what should change now?
For early-stage HCC with high-risk factors (high PIV, multiple tumor foci and more advanced BCLC stage), intensive follow-up and adjuvant systemic therapy following curative RFA were warranted.
1. Introduction
Hepatocellular carcinoma (HCC) is the sixth most common cancer and the third leading cause of cancer-related death worldwide [Citation1]. For early-stage HCC, hepatic resection (HR) and liver transplantation (LT) are preferred curative options. However, sometimes LT is not a feasible option because of the shortage of donor organs, while HR is contraindicated for patients with clinically significant portal hypertension, severe cirrhosis and impaired liver function. Ablation through radiofrequency or microwave is recommended as minimally invasive curative alternative if HR and LT are infeasible for early-stage HCC [Citation2].
Inflammation is recognized as a hallmark of cancer. Host immunity and inflammatory status are associated with cancer progression and survival [Citation3,Citation4]. HCC is an inflammation-driven cancer because immunotolerance to chronic infection of hepatitis virus leads to cirrhosis and carcinogenesis [Citation5]. Inflammation has been shown to be correlated with poor differentiation, microvascular invasion (MVI) and micro-metastasis, which increase the probability of insufficient radiofrequency ablation (RFA) and lead to early tumor recurrence [Citation6, Citation7]. Immune-inflammatory biomarkers (IIBs) may play important role in predicting prognosis of HCC undergoing RFA. Up to date, there have been many prognostic indexes constructed to depict systemic immune and/or inflammatory status, e.g., inflammation-immunity-nutrition score (IINS), inflammation burden index (IBI), platelet-lymphocyte ratio (PLR), C-reactive protein/albumin ratio (CAR), neutrophil-lymphocyte ratio (NLR), prognostic nutritional index (PNI), systemic immune-inflammation index (SII), systemic inflammation response index (SIRI), pan-immune-inflammation value (PIV), etc. Increasing evidences show that IIBs are associated with prognosis of HCC treated by RFA, such as PLR [Citation8], NLR [Citation8–12], SIRI [Citation13], PNI [Citation10, Citation14], CAR [Citation11] and SII [Citation15, Citation16]. Low IINS predicted favorable overall survival (OS) and progression-free survival (PFS) for HCC treated with anti-PD-1 therapy [Citation17]. In colorectal cancer (CRC), high IBI was a risk factor for recurrence and shortened survival [Citation18]. High PIV was a strong indicator of poor survival outcomes with better performance than other IIBs in metastatic colorectal cancer (mCRC) [Citation19]. However, prognostic potential of IINS, IBI and PIV has not been determined in early-stage HCC treated by curative RFA yet.
Among common cancers, HCC is currently solitary malignancy without proven adjuvant systemic therapy after potentially curative resection or ablation [Citation20]. There is great heterogeneity in tumor burden of early-stage HCC. The 5-year recurrence rate after RFA was up to 60%, especially in patients with lesion size ≥2 cm, multiple satellite tumor foci, micro-metastasis, etc [Citation9, Citation21]. Therefore, adjuvant systemic treatment following RFA is rational to prevent or reduce tumor recurrence in early-stage HCC with risk factors mentioned above [Citation20, Citation22]. Anti-angiogenesis target therapy combined with immune checkpoint inhibitor (AA-ICI) has been established as standard systemic treatment for advanced HCC [Citation23]. Could IIBs (e.g., PIV, IINS, IBI, etc.) appropriately discriminate early-stage HCC between low- and high-risk groups and guide individualized adjuvant AA-ICI treatment following curative RFA?
This two-center retrospective study aimed to explore the prognostic role of some IIBs in early-stage HCC patients receiving curative RFA as initial or salvage treatment and to develop an IIB-based risk model to individualize adjuvant systemic treatment following RFA.
2. Methods
2.1. Patients and data acquisition
We retrospectively reviewed 398 patients with treatment-naïve or recurrent early-stage HCC in the Fifth Affiliated Hospital (SYSU-Hos5) and Cancer Center (SYSUCC) of Sun Yat-sen University from September 2014 to December 2021. The inclusion criteria were: (a) HCC diagnosed by pathology or noninvasive diagnostic criteria recommended by the European Association for the Study of Liver (EASL) [Citation24]; (b) Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1; (c) absence of extrahepatic metastasis and macrovascular invasion; (d) solitary tumor with diameter ≤ 5 cm, or multiple tumors (≤ 5 nodules) with each diameter ≤2 cm; (e) has curative RFA as initial or salvage curative treatment. The exclusion criteria were: (ⅰ) loss of follow-up; (ⅱ) lack of baseline medical imaging data; (ⅲ) had uncontrollable comorbidities or other malignancies; (ⅳ) had liver transplantation after RFA. Patients from SYSU-Hos5 were assigned to either cohort A (as training set) or cohort B (as Testing set) by a random number table, while patients from SYSUCC were assigned as cohort C (as external validating set). The study flowchart was presented in Supplementary Figure S1. Patients’ demographic and clinicopathological data were recorded: sex, age, etiology, presence of cirrhosis, Child-Pugh class, tumor characteristics (AFP level, size, number, BCLC stage) and previous treatment. Hematological and biochemical tests were performed at least three days before RFA. C-reactive protein (CRP), albumin, white blood cell, neutrophil, lymphocyte, monocyte and platelet counts were obtained. The PNI, IINS, CAR, SII, PLR, NLR, IBI and PIV before RFA were calculated as shown in Supplementary table S1. This study complied with the standards of Helsinki Declaration and was approved by the Research Ethics Committee of SYSU-Hos5 and SYSUCC. Informed consent on treatment was required. Informed consent on enrollment into this study was waived due to its retrospective nature.
2.2. Treatment and follow-up
2.2.1. RFA procedure
Before treatment, dynamic multi-phase contrast-enhanced CT or MR scanning was performed to evaluated tumor characteristics. Candidate lesions to be ablated should be clearly visible on ultrasonography with a safe path. RFA was performed percutaneously in real-time ultrasonic guidance under general anesthesia and intramuscular sedation by using Medsphere system (Medsphere Medical Technology Co., LTD, Shanghai, China). The RFA tip was umbrella-shaped multi-claw electrode with a temperature needle in its center. Cardiovascular and respiratory functions were monitored. Hyperechoic area around the electrode tip was observed under real-time ultrasonic monitoring during RFA procedures. Two to four cycles (5-8 min each) were required during RFA according to tumor size. Overlap ablation was designed to ensure that ablative hyperthermia should cover entire tumor nodule volume plus a 5-10 mm sufficiently safe margin. Supplementary figure S2 illustrated ultrasound-guided RFA for a 63-year-old female with single HCC nodule measured 2.0 cm in liver S8.
2.2.2. Anti-angiogenesis target therapy combined with immune checkpoint inhibitor
Anti-angiogenesis target therapy combined with immune checkpoint inhibitor (AA-ICI) has become standard systemic treatment for advanced HCC [Citation23]. In our study, ninety-three patients had received sequential AA-ICI following RFA per their clinicians’ experience and judgment. The anti-angiogenesis target therapy included apatinib (N = 25), sorafenib (N = 37), lenvatinib (N = 17) and bevacizumab or its biosimilars (N = 14). Immune checkpoint inhibitor therapy included anti-PD-1 monoclonal antibodies (such as sintilimab, camrelizumab, tislelizumab and pembrolizumab) (N = 35) and anti-PD-L1 monoclonal antibodies (such as atezolizumab, durvalumab) (N = 58).
2.2.3. Follow-up
Multi-phase contrast-enhanced CT or MR scanning was performed to evaluate tumor response a month after RFA. Tumor was considered to be completely ablated if contrast enhancement or abnormal wash-out within or around the ablation zone was absent. Patients without viable tumors were followed up every three months with physical examination, routine blood test, liver function test, tumor biomarkers test and abdominal ultrasound. Contrast-enhanced CT or MR scanning was done if tumor recurrence was suspected.
2.3. Statistical analysis
The primary endpoint was overall survival (OS) which was defined as the duration from the starting date of RFA to death or the last follow-up. The secondary endpoint was recurrence-free survival (RFS) which was defined as the duration from the starting date of RFA to the first confirmed tumor recurrence or the last follow-up. Survival curves were determined by the Kaplan-Meier method and compared by the log-rank test. The life table method was used to calculate cumulative survival rates. Univariate and multivariate analysis were both performed using the Cox proportional hazard model to test independent prognostic factors and to calculate hazard ratio (HR) and 95% confidence interval (CI) as well. Quantitative variables were compared by Student t test and Mann-Whitney U test. Categorical variables were compared by the Pearson Chi-square test and Fisher’s exact test. Receiver operator characteristic (ROC) curve and the estimated area under the curve (AUC) were calculated to compare the prognostic ability of IIBs. For an inflammation-based score, a cutoff value on the ROC curve where Youden index was maximum was determined as optimum. A nomogram was developed to identify the proportional effects of independent prognostic factors. Calibration plots with 1000 sets of bootstrap resamples were drawn to estimate the predictive efficacy of the prognostic model. All analyses were two-sided. P value less than 0.05 was considered significant. Statistical analyses were performed by R version 4.3.1 and Statistical Package for Social Science, version 27.0 (SPSS, Chicago, IL, USA).
3. Results
3.1. High PIV was predictive of inferior survival in early-stage HCC treated by curative RFA
To screen which IIBs were predictive of OS, ROC analysis was performed in cohort A (N = 65) and found that PIV was significantly predictive of OS (Supplementary Figure S3). The optimum cutoff of PIV was 120 where maximum Youden index was 0.414. The baseline characteristics of cohort A (N = 65) was presented in Supplementary Table S2. With a median follow-up duration of 33.7 (range, 4.9 ∼ 77.9) months, 54 (83.1%) patients had intrahepatic and/or extrahepatic tumor recurrence, and 26 (40.0%) patients died. The median OS and RFS of cohort A were 58.8 (95% CI, 35.2 ∼ 82.3) months and 9.9 (95% CI, 2.7 ∼ 17.1) months, respectively. The 2-year and 5-year OS rates were 78.8% and 49.4%, respectively. The 2-year and 5-year RFS rates were 29.5% and 11.3%, respectively.
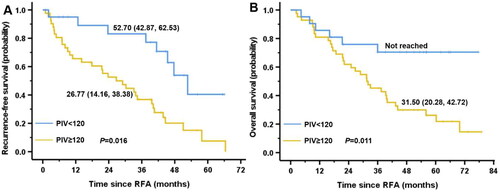
To test the prognostic role of PIV and screen independent prognostic factors, survival analyses were performed in cohort B (N = 68) whose baseline characteristics were Supplementary Table S3. After propensity score matching (PSM) at a ratio of 1:2, there were 21 patients with PIV <120 and 42 patients with PIV ≥120. No imbalanced variables were observed. After a median follow-up of 36.0 (range, 2.3 ∼ 79.0) months, 41 (65.1%) patients had tumor recurrence and 38 (60.3%) patients died. The median OS and RFS of cohort B were 39.4 (95% CI, 27.8 ∼ 50.9) months and 37.5 (95% CI, 27.5 ∼ 47.5) months, respectively. The 2-year and 5-year OS rates were 66.4% and 39.0%. The 2-year and 5-year RFS rates were 62.3% and 19.5%. Patients with low PIV had better OS (5-year OS, 69.3% vs. 26.2%, p = 0.011) and RFS (5-year RFS, 40.5% vs. 10.4%, p = 0.016) than those with high PIV (). As shown in Supplementary Table S4, multivariate analysis with Cox proportional hazard model indicated that high PIV, multiple tumor nodules (Supplementary Figure S4 A and B) and more advanced BCLC stage (Supplementary Figure S4 C and D) were adverse prognostic indicators for OS and RFS.
Figure 1. High PIV was associated with unfavorable recurrence-free survival (RFS) and overall survival (OS) in early-stage hepatocellular carcinoma treated by curative RFA in testing cohort B after propensity score matching. Kaplan-Meier curves for RFS (A) and OS (B) of patients with high or low PIV. PIV: pan-immune-inflammation value; RFA: radiofrequency ablation.
To validate the prognostic role of PIV and build a risk model that divide patients into low- or high-risk group, survival and nomogram analyses were conducted in external validating cohort C (N = 265) enrolled from SYSUCC. Their baseline characteristics were displayed in . There was an imbalance in gender (p = 0.05), HCV infection (p = 0.007) and cirrhosis (p = 0.005) between low and high PIV groups. After PSM at a ratio of 1:1, all variables were balanced. With a median follow-up duration of 20.0 (range, 2.3 ∼ 77.9) months, 155 (72.4%) patients had tumor recurrence and 88 (41.1%) patients died in the PSM cohort C. The median OS and RFS were 39.4 (95% CI, 26.6 ∼ 52.1) months and 13.9 (95% CI, 11.7 ∼ 16.2) months, respectively. The 2-year and 5-year OS rates were 66.8% and 36.4%. The 2-year and 5-year RFS rates were 33.8% and 7.7%. ROC analysis found that PIV was predictive of OS in PSM cohort C (). High PIV was associated with inferior OS (5-year OS, 24.4% vs. 52.6%, p < 0.001) and RFS (5-year RFS, 4.3% vs. 17.2%, p < 0.001) than those with low PIV (). Multivariate analysis () confirmed that high PIV, multiple tumor nodules (Supplementary Figure S5A and B) and more advanced BCLC stage (Supplementary Figure S5C and D) were independent adverse prognostic factors for OS and RFS. Incorporating PIV, tumor number (single vs. multiple) and BCLC stage, a nomogram was constructed for predicting OS () and RFS () in PSM cohort C. The calibration curves of OS nomogram () and RFS nomogram () were well-matched with the idealized 45° lines, indicating sufficient capacity of the nomogram models in predicting actual OS and RFS probabilities. The C-indexes of PIV-based nomogram risk models for predicting OS and RFS probability were 0.752 (95% CI: 0.714-0.788) and 0.726 (95% CI: 0.693-0.749), respectively.
Figure 2. Prognostic role of PIV was validated in external validating cohort C after propensity score matching. The time-dependent receiver operating characteristic curve (A) of PIV cutoff derived from training cohort A to predict the 5-year overall survival (OS), and Kaplan-Meier curves for OS (B) and recurrence-free survival (C) in early-stage hepatocellular carcinoma treated by curative RFA in external validating cohort C. AUC: area under curve; PIV: pan-immune-inflammation value; RFA: radiofrequency ablation.
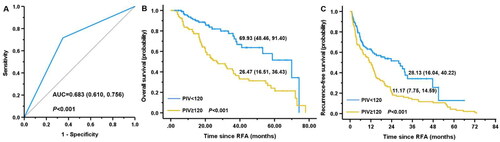
Figure 3. The PIV-based nomogram (A) and calibration curves for predicting the 2-year (B) and 5-year (C) OS in external validating cohort C after propensity score matching. PIV: pan-immune-inflammation value; OS: overall survival; BCLC: Barcelona clinic liver cancer.
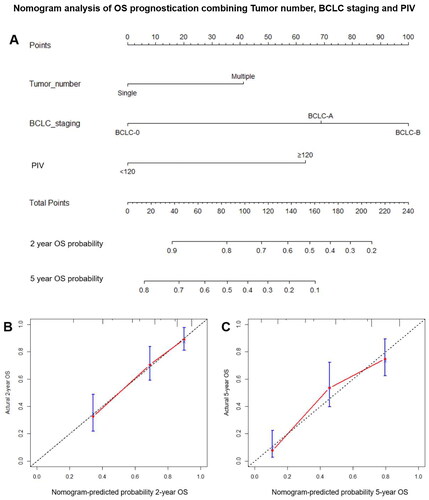
Figure 4. The PIV-based nomogram (A) and calibration curves for predicting the 2-year (B) and 5-year (C) RFS in external validating cohort C after propensity score matching. PIV: pan-immune-inflammation value; RFS: recurrence-free survival; BCLC: Barcelona clinic liver cancer.
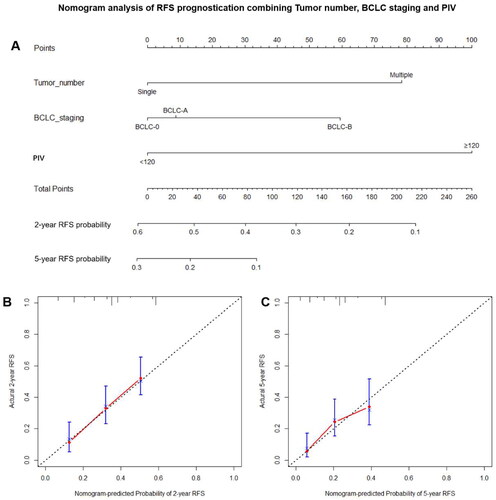
Table 1. Baseline characteristics of patients in the primary and PSM cohorts of external validating cohort C.
Table 2. Univariate and multivariate analysis with the cox proportional hazard model for OS and RFS of early-stage hepatocellular carcinoma treated by radiofrequency ablation in PSM cohort derived from external validating cohort C.
3.2. The PIV-based risk model helps to tailor adjuvant AA-ICI treatment following curative RFA
Cohort A, B, and C were pooled together to form cohort D. Patients were divided into low- or high-risk group. Low PIV was scored as 0 while high PIV as 1; solitary tumor was scored as 0 while multiple tumor nodules as 1; BCLC-0 stage was scored as 0, BCLC-A stage as 1 and BCLC-B stage as 2. The sum of scores from PIV, tumor number and BCLC stage were calculated for every patient. The grouping criteria were as follow: (ⅰ) total score ≤1, low-risk; (ⅱ) total score ≥2, high-risk. Finally, 186 (46.7%) patients and 212 (53.3%) patients were in low-risk and high-risk groups, respectively (supplementary table S5). Imbalance existed in HCV infection, cirrhosis, tumor size and Child-Pugh class between low- and high-risk groups. After PSM at a ratio of 1:1, the imbalance was eliminated. In PSM cohort, after median follow-up duration of 20.2 (2.3 ∼ 79.0) months, 191 (69.2%) patients had tumor recurrence and 117 (42.4%) patients died. The median OS and RFS were 37.5 (95% CI, 31.6 ∼ 43.3) months and 14.1 (95% CI, 10.9 ∼ 17.4) months, respectively. The 2-year and 5-year OS rates were 66.3% and 39.9%. The 2-year and 5-year RFS rates were 35.2% and 11.4%. As shown in Supplementary Figure S6, the PIV-based risk model performed well in discriminating prognosis of all patients. The OS (5-year OS, 58.6% vs. 22.1%, p < 0.001) and RFS (5-year RFS, 18.4% vs. 3.8%, p < 0.001) of low-risk group were significantly better than those of high-risk group.
To explore the ability of the PIV-based risk model in guiding adjuvant systemic treatment following curative RFA, patients who had received AA-ICI following RFA were analyzed. Their characteristics were displayed in . Adjuvant AA-ICI following RFA improved RFS both in low- and high-risk groups and exhibited added benefit to OS of high-risk group. In low-risk group, no OS improvement was observed when adjuvant AA-ICI was given following RFA (). Multivariate analysis confirmed that adjuvant AA-ICI following RFA significantly favored both RFS and OS in high-risk group (Supplementary Table S6). These results indicated that early-stage HCC patients in high-risk group needed adjuvant AA-ICI treatment following curative RFA to improve OS.
Figure 5. Adjuvant AA-ICI treatment following curative RFA exhibited more benefit in early-stage hepatocellular carcinoma patients in high-risk group in the pooled cohort D. Kaplan-Meier curves for RFS (A) and OS (B) of patients in low-risk group with adjuvant AA-ICI treatment or not. Kaplan-Meier curves for RFS (C) and OS (D) of patients in high-risk group with adjuvant AA-ICI treatment or not. RFA: radiofrequency ablation; RFS: recurrence-free survival; OS: overall survival; AA-ICI: anti-angiogenesis target therapy plus immune checkpoint inhibitor.
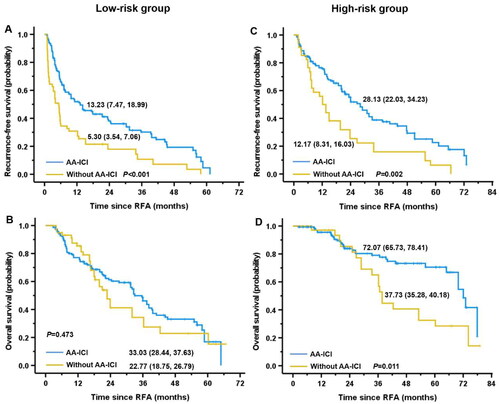
Table 3. Baseline characteristics of early-stage hepatocellular carcinoma patients with or without adjuvant AA-ICI treatment following curative RFA between low- and high-risk groups.
4. Discussion
In this study, we found that high PIV could predict inferior OS and RFS in early-stage HCC treated by curative RFA. A risk model consisting of PIV, tumor number and BCLC staging performed well in discriminating early-stage HCC between low- and high-risk groups. Adjuvant AA-ICI treatment following curative RFA could improve OS in high-risk group. Although various IIBs had been reported to be predictive of recurrence and survival after RFA [Citation8–16], the role of PIV in prognosticating outcomes of early-stage HCC treated by curative RFA remained unknown. Literatures on IIBs-based risk models established to guide individualized adjuvant treatment following RFA are rare. To the best of our knowledge, this is the first study to identify the correlationship between PIV and survivals and to introduce a PIV-based risk model to guide individualized adjuvant systemic treatment following curative RFA.
The important role of immunity and inflammation in carcinogenesis and cancer progression has been increasingly emphasized in plenty of studies [Citation3–5]. In China, HCC mostly arises from underlying chronic liver inflammation, fibrosis and cirrhosis, and progresses because of malignantly transformed liver cells evading immune recognition and clearance [Citation7]. The association between immunity or inflammation and prognosis has aroused particular interest of clinicians in the past decades. Several IIBs such as PLR, NLR, SIRI, PNI, CAR, and SII have emerged to predict the prognosis of early-stage HCC treated by RFA and been proven to be associated with recurrence and overall survival [Citation8–16]. Herein, our two-center study found that high PIV was an independent risk factor for tumor recurrence and shortened survival in early-stage HCC treated by curative RFA. Recent studies indicated that neutrophil could be part of tumor-promoting inflammation by driving angiogenesis, extracellular matrix remodeling, metastasis and immunosuppression [Citation25]; platelet could stimulate circulating tumor cells (CTCs) anoikis resistance, epithelial-to-mesenchymal transition (EMT), angiogenesis, extravasation and eventually metastasis [Citation26]; monocyte could exert pro-tumor functions via promoting angiogenesis, remodeling extracellular matrix and differentiation toward type 2 tumor-associated macrophages (M2-TAMs) [Citation27]; lymphocyte could suppress cancer proliferation by inducing apoptosis and inhibiting tumor migration and invasion [Citation4]. As an integrative IIB based on peripheral neutrophil, platelet, monocyte and lymphocyte counts, high PIV usually means thrombocythemia, neutrophilia, monocytosis and lymphopenia, suggesting excessive inflammation and impaired anti-tumor immunity. PIV had been demonstrated to be a useful prognostic biomarker in various cancers, e.g., mCRC [Citation19, Citation28], breast cancer [Citation29], small-cell lung cancer [Citation30], and metastatic renal cell carcinoma [Citation31], etc. Furthermore, high PIV was an indicator of inferior therapeutic efficacy of immunotherapy in metastatic renal cell carcinoma and melanoma [Citation31, Citation32], and advanced non-small cell lung cancer [Citation33].
The 5-year recurrence rates of early-stage HCC treated by RFA were as high as 60 ∼ 70% [Citation21]. Great heterogeneity existed in early-stage HCC in terms of tumor size, number and location which were responsible for incomplete RFA, leading to more aggressive phenotype changes, e.g., invasion, metastasis, and immune escape [Citation34]. Our former research indicated that insufficient RFA resulted in PD-L1 overexpression in HCC cells and T cell exhaustion, which was conducive to growth and progression of residual tumor [Citation35]. Thus, it was rational to prescribe adjuvant systemic treatment to patients with high-risk factors. Adjuvant sorafenib after RFA was reported to be superior to RFA alone in improving survival outcomes in patients with recurrent HCC within Milan criteria [Citation36]; however, STORM trial did not show benefit of adjuvant sorafenib in HCC patients after resection or ablation [Citation37]. Atezolizumab (a PD-L1 monoclonal antibody) plus bevacizumab (a VEGF monoclonal antibody) has won sorafenib by a landslide in terms of survival improvement for advanced unresectable HCC [Citation38]. On-going IMbrave 050 trial aims to compare atezolizumab plus bevacizumab versus active surveillance for early-stage HCC patients at high-risk of recurrence following curative ablation or resection [Citation20]. In practice, adjuvant anti-angiogenesis target therapy (e.g., sorafenib, lenvatinib, bevacizumab) plus ICI immunotherapy was given to certain patients according to their clinical physicians’ knowledge, experience and judgment. However, criteria to select appropriate candidates for adjuvant systemic treatment following curative RFA are unavailable until now. Our study found that the PIV-based risk model incorporating tumor number, PIV and BCLC staging effectively divided early-stage HCC treated by curative RFA into low- and high-risk groups; adjuvant AA-ICI treatment prolonged RFS both in low- and high-risk groups but only improved OS in high-risk group. Maybe early-stage HCC patients with high PIV, multiple tumor foci and advanced BCLC stage benefited more from adjuvant AA-ICI treatment following curative RFA.
There were several limitations in this study. Firstly, our study was retrospectively designed. Secondly, up to 80% of HCC patients in our study resulted from hepatitis B virus infection, whereas in Japan, the United States and Europe, hepatitis C virus, alcohol abuse and nonalcoholic fatty liver disease were the predominant etiologies. Thirdly, counts of neutrophil, lymphocyte, monocyte and platelet are also affected by infection, ischemia, metabolic syndrome, diabetes mellitus and renal or hepatic dysfunction which might be confounding factors when assessing the role of IIBs-based scores in HCC prognostication. Finally, only RFA was evaluated here. Whether the PIV-based risk model is applicable to early-stage HCC treated by microwave ablation (MWA) was unknown.
In conclusion, PIV is a feasible independent prognostic factor for RFS and OS in early-stage HCC patients who received curative RFA. The proposed PIV-based nomogram risk model could help clinicians to individualize adjuvant systemic treatment and follow-up scheme.
Authors’ contributions
Xuexia Liang designed this research. Xuexia Liang, Juyuan Bu, Yanhui Jiang, Shuqin Zhu, Qing Ye and Yun Deng collected and analyzed the data. Xuexia Liang drafted the manuscript. Wuzhu Lu provided imaging resources and contributed substantially to the review & editing of this manuscript. Qiaodan Liu made substantial contribution to the design of the work and revised the manuscript. All authors read and approved the final manuscript.
Supplemental Material
Download MS Word (2.6 MB)Acknowledgement
We thanked Miss Yanna Ma for her selfless help in checking and revising the writing language.
Disclosure statement
No potential conflict of interest was reported by all authors.
Data availability statement
Data can not be shared publicly because the data from this study contain potentially sensitive private information. Data would be available from the corresponding authors upon reasonable request or on the research data deposit (RDD) platform of Sun Yat-sen University after the manuscript was published.
Additional information
Funding
References
- Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660.
- Reig M, Forner A, Rimola J, et al. BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol. 2022;76(3):681–693.
- Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation . Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013.
- Diakos CI, Charles KA, Mcmillan DC, et al. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493-503–e503. doi: 10.1016/S1470-2045(14)70263-3.
- Kubes P, Jenne C. Immune responses in the liver . Annu Rev Immunol. 2018;36(1):247–277. doi: 10.1146/annurev-immunol-051116-052415.
- Zheng J, Seier K, Gonen M, et al. Utility of serum inflammatory markers for predicting microvascular invasion and survival for patients with hepatocellular carcinoma . Ann Surg Oncol. 2017;24(12):3706–3714. doi: 10.1245/s10434-017-6060-7.
- Cabillic F, Corlu A. Regulation of transdifferentiation and retrodifferentiation by inflammatory cytokines in hepatocellular carcinoma. Gastroenterology. 2016;151(4):607–615. doi: 10.1053/j.gastro.2016.06.052.
- Chen Y, Yang Y, Zhang XY, et al. Nomogram based on neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio to predict recurrence in patients with hepatocellular carcinoma after radiofrequency ablation. Cardiovasc Intervent Radiol. 2021;44(10):1551–1560. doi: 10.1007/s00270-021-02872-8.
- Canale M, Ulivi P, Foschi FG, et al. Clinical and circulating biomarkers of survival and recurrence after radiofrequency ablation in patients with hepatocellular carcinoma . Crit Rev Oncol Hematol. 2018;129:44–53.
- Chu MO, Shen CH, Chang TS, et al. Pretreatment inflammation-based markers predict survival outcomes in patients with early stage hepatocellular carcinoma after radiofrequency ablation . Sci Rep. 2018;8(1):16611. doi: 10.1038/s41598-018-34543-z.
- Shen Y, Wang H, Li W, et al. Prognostic significance of the CRP/alb and neutrophil to lymphocyte ratios in hepatocellular carcinoma patients undergoing TACE and RFA. J Clin Lab Anal. 2019;33(9):e22999.
- Hayashi M, Abe K, Fujita M, et al. Combination of psoas muscle mass index and neutrophil-to-lymphocyte ratio as a noninvasive prognostic marker in hepatocellular carcinoma patients undergoing radiofrequency ablation . Eur J Gastroenterol Hepatol. 2023;35(5):568–574. doi: 10.1097/MEG.0000000000002532.
- Xin Y, Zhang X, Li Y, et al. A systemic inflammation response index (SIRI)-based nomogram for predicting the recurrence of early stage hepatocellular carcinoma after radiofrequency ablation . Cardiovasc Intervent Radiol. 2022;45(1):43–53. doi: 10.1007/s00270-021-02965-4.
- Pan J, Chen S, Tian G, et al. Preoperative albumin-bilirubin grade with prognostic nutritional index predicts the outcome of patients with early-stage hepatocellular carcinoma after percutaneous radiofrequency ablation . Front Med . 2020;7:584871. doi: 10.3389/fmed.2020.584871.
- Yang Q, Yu XL, Wang Y, et al. Predictive effects of a combined indicator in patients with hepatocellular carcinoma after thermal ablation . J Cancer Res Ther. 2020;16(5):1038–1050. doi: 10.4103/jcrt.JCRT_1080_19.
- Xin Y, Yang Y, Liu N, et al. Prognostic significance of systemic immune-inflammation index-based nomogram for early stage hepatocellular carcinoma after radiofrequency ablation. J Gastrointest Oncol. 2021;12(2):735–750. doi: 10.21037/jgo-20-342.
- Zhang Z, Liang Y, Zhong D, et al. Prognostic value of inflammation-immunity-nutrition score in patients with hepatocellular carcinoma treated with anti-PD-1 therapy . J Clin Lab Anal. 2022;36(5):e24336. doi: 10.1002/jcla.24336.
- Xie H, Ruan G, Wei L, et al. Comprehensive comparative analysis of prognostic value of serum systemic inflammation biomarkers for colorectal cancer: results from a large multicenter collaboration [J]. Front Immunol. 2022;13:1092498. doi: 10.3389/fimmu.2022.1092498.
- Fucà G, Guarini V, Antoniotti C, et al. The pan-immune-inflammation value is a new prognostic biomarker in metastatic colorectal cancer: results from a pooled-analysis of the valentino and TRIBE first-line trials. Br J Cancer. 2020;123(3):403–409. doi: 10.1038/s41416-020-0894-7.
- Hack SP, Spahn J, Chen M, et al. IMbrave 050: a phase III trial of atezolizumab plus bevacizumab in high-risk hepatocellular carcinoma after curative resection or ablation. Future Oncol. 2020;16(15):975–989. doi: 10.2217/fon-2020-0162.
- Huang J, Yan L, Cheng Z, et al. A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the milan criteria . Ann Surg. 2010;252(6):903–912. doi: 10.1097/SLA.0b013e3181efc656.
- EUROPEAN ASSOCIATION FOR THE STUDY OF THE LIVER. ELECTRONIC ADDRESS E E E, EUROPEAN ASSOCIATION FOR THE STUDY OF THE L. EASL clinical practice guidelines: management of hepatocellular carcinoma . J Hepatol. 2018;69(1):182–236.
- Llovet JM, Castet F, Heikenwalder M, et al. Immunotherapies for hepatocellular carcinoma . Nat Rev Clin Oncol. 2022;19(3):151–172. doi: 10.1038/s41571-021-00573-2.
- EUROPEAN ASSOCIATION FOR STUDY OF L, EUROPEAN ORGANISATION FOR R, TREATMENT OF C. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma . Eur J Cancer. 2012;48(5):599–641.
- Jaillon S, Ponzetta A, DI Mitri D, et al. Neutrophil diversity and plasticity in tumour progression and therapy . Nat Rev Cancer. 2020;20(9):485–503. doi: 10.1038/s41568-020-0281-y.
- Liu Y, Zhang Y, Ding Y, et al. Platelet-mediated tumor metastasis mechanism and the role of cell adhesion molecules . Crit Rev Oncol Hematol. 2021;167:103502. doi: 10.1016/j.critrevonc.2021.103502.
- Olingy CE, Dinh HQ, Hedrick CC. Monocyte heterogeneity and functions in cancer . J Leukoc Biol. 2019;106(2):309–322. doi: 10.1002/JLB.4RI0818-311R.
- Corti F, Lonardi S, Intini R, et al. The pan-immune-inflammation value in microsatellite instability-high metastatic colorectal cancer patients treated with immune checkpoint inhibitors . Eur J Cancer. 2021;150:155–167.
- Şahin AB, Cubukcu E, Ocak B, et al. Low pan-immune-inflammation-value predicts better chemotherapy response and survival in breast cancer patients treated with neoadjuvant chemotherapy. Sci Rep. 2021;11(1):14662. doi: 10.1038/s41598-021-94184-7.
- Kucuk A, Topkan E, Ozkan EE, et al. A high pan-immune-inflammation value before chemoradiotherapy indicates poor outcomes in patients with small-cell lung cancer. Int J Immunopathol Pharmacol. 2023;37:3946320231187759. doi: 10.1177/03946320231187759.
- Yekedüz E, Tural D, Ertürk İ, et al. The relationship between pan-immune-inflammation value and survival outcomes in patients with metastatic renal cell carcinoma treated with nivolumab in the second line and beyond: a Turkish oncology group kidney cancer consortium (TKCC) study. J Cancer Res Clin Oncol. 2022;148(12):3537–3546. doi: 10.1007/s00432-022-04055-5.
- Fucà G, Beninato T, Bini M, et al. The pan-immune-inflammation value in patients with metastatic melanoma receiving first-line therapy. [Target Oncol. 2021;16(4):529–536. J doi: 10.1007/s11523-021-00819-0.
- Chen Y, Gong L, Gu P, et al. Pan-immune-inflammation and its dynamics: predictors of survival and immune-related adverse events in patients with advanced NSCLC receiving immunotherapy . BMC Cancer. 2023;23(1):944. doi: 10.1186/s12885-023-11366-4.
- Wang K, Wang C, Jiang H, et al. Combination of ablation and immunotherapy for hepatocellular carcinoma: where we are and where to go . Front Immunol. 2021;12:792781. doi: 10.3389/fimmu.2021.792781.
- Liang X, Liu Q, Zhu S, et al. GSDME has prognostic and immunotherapeutic significance in residual hepatocellular carcinoma after insufficient radiofrequency ablation. J Transl Oncol. 2023;39:101796. doi: 10.1016/j.tranon.2023.101796.
- Zhou Q, Wang X, Li R, et al. Sorafenib as adjuvant therapy following radiofrequency ablation for recurrent hepatocellular carcinoma within milan criteria: a multicenter analysis. J Gastroenterol. 2022;57(9):684–694. doi: 10.1007/s00535-022-01895-3.
- Bruix J, Takayama T, Mazzaferro V, et al. Adjuvant sorafenib for hepatocellular carcinoma after resection or ablation (STORM): a phase 3, randomised, double-blind, placebo-controlled trial . Lancet Oncol. 2015;16(13):1344–1354. doi: 10.1016/S1470-2045(15)00198-9.
- Finn RS, Qin S, Ikeda M, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382(20):1894–1905. doi: 10.1056/NEJMoa1915745.
