ABSTRACT
Cybersecurity threats in the Health sector are increasing globally due to the rising value of sensitive health information and availability of digitalised personal health records. This systematic review compares international and Australian health system cybersecurity landscapes in relation to the introduction of universal electronic health records. It examines recent trends in healthcare cybersecurity breaches that can disrupt essential services if patient safety and privacy are compromised. Often health systems and health mangers are ill-equipped to mitigate such threats. Recommendations are provided to proactively mature the cybersecurity culture within healthcare organisations, thus increasing their resilience to cyber threat.
Introduction
Healthcare is a ubiquitous need and affects every person in society. The healthcare sector is responsible for collecting and storing highly sensitive and confidential data whilst simultaneously being required to share it amongst medical staff, patients and other organisations. HealthCare Systems (HCS) are compelled to evolve with advances in technology. The transition of healthcare from hospital centred, specialist focused approaches to distributed, patient centred care has been facilitated through health record digitalisationFootnote1 and is widely recognised as both inevitable and essential.Footnote2 Breaches of HCS cybersecurity that expose personal information or data will negatively impact both patients and the healthcare institution, with potentially life-threatening consequences.Footnote3 The cybersecurity risk to healthcare, including ransomware attacks, hacking of personal medical devices and theft of personal medical data, is continuously rising.Footnote4 Stolen health records are worth more than records from any other industry,Footnote5 due to the high value of personal information.Footnote6 Sold on the darkweb, they can fund criminal activity and enable identity theft, blackmail, extortion and even murder.Footnote7 In 2015, the US Office of Personnel Management (OPM) and Anthem Health, which provides healthcare for Federal employees, were both hacked within months of each other, apparently by the same perpetrator.Footnote8 This means the hackers can link personnel records with sensitive health data for federal employees and enable targeted harm to high-value individuals.Footnote9 Despite a global increase in cyberattacks on health entities the healthcare sector has significantly trailed other sectors in the ability to secure its critical data.Footnote10 Cybersecurity in healthcare is identified as an emerging health security challenge, but there is low awareness in the health sector of the risk.Footnote11 A healthcare cybersecurity capability approach is required to address increasing cyberthreats. The recent introduction of a universal electronic medical record My Health Record (MHR) in Australia provides an opportunity to examine healthcare cybersecurity capability.
Health cybersecurity capability is the capacity of the organisation or sector to produce an outcome, such as proactive cyber-awareness and defence.Footnote12 Healthcare institutions have traditionally been focussed on patient care and not cybersecurity and pursued the electronic health record as a holy grail of optimal patient care. Yet healthcare lags behind other sectors in both securing data and developing comprehensive employee cybersecurity training programs.Footnote13 As patient information grows in both volume and value, health managers are required to develop cybersecurity capability across organisations. Cybersecurity capability development includes updating existing information technology but also recognising the need for, and proactively acquiring, new technology, cybersecurity talent and comprehensive organisation training.Footnote14
The paradigm shift to digitalised healthcare requires information technologies to store vast amounts of electronic patient information across diverse operating systems.Footnote15 The integration of new technologies with outdated, legacy or unsupported operating systems compromises interoperability and increases cybersecurity vulnerability.Footnote16 The 2017 global WannaCry ransomware attackFootnote17 provides a stark example of this. Widespread use of obsolete Windows XP softwareFootnote18 in combination with ignored cybersecurity warnings to undertake system upgrades enabled the malware to spread across the National Health Service (NHS) in the UK. WannaCry severely affected NHS” ability to provide patient care for a week between 12–17 May 2017, spread to 200,000 computers in over 100 countries, and is the largest malware cyberattack to date.Footnote19 WannaCry had not specifically targeted the healthcare sector,Footnote20 but was able to spread to 80 out of 236 NHS trusts and 603 primary care organisations across EnglandFootnote21 due to poor cyber-hygiene and a lack of appreciation amongst healthcare executive management of the business risk impact of cyber breaches.Footnote22 Ambulances had to be diverted, diagnostic equipment was infected, pathology and radiology unable to function, patient records were inaccessible and nearly 7000 medical appointments were cancelled.Footnote23
Healthcare has the reputation of ‘low security maturity’,Footnote24 and lacks sophisticated data security tools compared to other industries.Footnote25 This is due to budgetary constraints,Footnote26 lack of cybersecurity training and awareness among health managers, the heterogenous healthcare information infrastructure, and innumerable wireless connected devices.Footnote27 Current healthcare cyber-defence is often reactive and undertaken after malicious attack.Footnote28 The retrospective nature of healthcare cybersecurity,Footnote29 along with sector reliance upon perimeter defence (antivirus, firewalls) for protectionFootnote30 compounds cyber risk. Such measures are unlikely to protect against sophisticated and persistent attacksFootnote31 or mitigate insider threats.Footnote32 Other significant barriers to healthcare cybersecurity are lack of appropriate cybersecurity professionals working in health,Footnote33 constantly emerging and evolving malware threats,Footnote34 and complex network infrastructure.Footnote35
Aims
To compare the international and Australian health system cybersecurity landscape in relation to introduction of the universal MHR in Australia.
To examine recent trends in healthcare cybersecurity breaches in Australia and worldwide.
Methods
A systematic review of the relevant literature and background information regarding global cybersecurity in health systems and digital medical records was conducted using the PRISMA criteria. Ten databases in total were searched: Medline/PubMed; Embase; Emcare; CINAHL; Psycinfo; Web of Science; Scopus; Compendex; IEEE; and Google Scholar Advanced Search to obtain grey literature. The key concepts utilised were e-health records AND cybersecurity. The keywords used in the search are listed below:
Electronic health records/OR medical record, computerised/OR digital health record* OR electronic medical record*
Cyber security/OR data security/OR medical identity theft/OR terrorism/OR Malware/OR Ransomware OR Cyber adj4 (crime OR attack OR security OR threat OR terror)
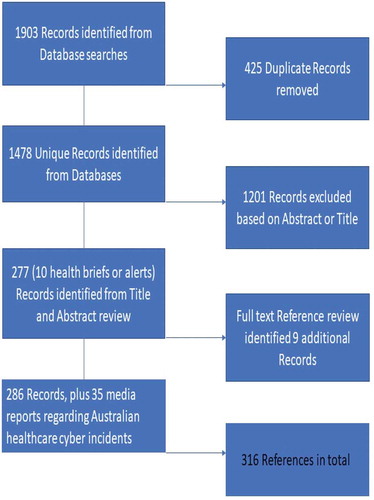
The Google Scholar Advanced Search utilised ‘healthcare AND cybersecurity’ to obtain grey literature such as conference proceeding books, conference papers and thesis dissertations. Due to the emergent nature of electronic health records, the current social and political debate around privacy and security and the recent changes to MHR implementation, the decision was made to include media reports. The Factiva database was utilised to search relevant media articles. Key concepts were health data breach AND MHR. The search process is illustrated below in .
Study eligibility
Articles were considered for inclusion if they were:
English language publications,
Published between 2014–2019 in a peer reviewed or scholarly journal,
Full-text version of the manuscript, conference paper or prospective thesis/paper,
Strategy, Guideline, Report or Policy review documents which provide relevant subject insight or recommendation
Study selection
Studies were selected if they discussed an issue related to cybersecurity in healthcare either in the title or the abstract. Studies were excluded if their content was not specific to cybersecurity within healthcare, or if they were focused solely on presenting a technical algorithmic solution without discussion of the general cybersecurity landscape. Two independent reviewers checked titles and abstracts as collated on a shared EndNote library.
Information synthesis
The findings of the included studies were synthesised narratively into themes which included:
Theme 1 – emerging trends in cybersecurity risk,
Theme 2 – cybersecurity capability countermeasures and mitigation strategies,
Theme 3 – current cybersecurity issues within Australia.
An analysis of Australian healthcare cybersecurity capability is presented in the discussion session.
We also reviewed the accreditation requirements of the two peak bodies in health management in Australia, the Australian College of Health Systems Management Australia and the Royal Australasian College of Medical Educators, for health cybersecurity as a curriculum requirement.
Results
We identified 316 relevant records. Of the 316 records, 100 outlined cyberattacks on HCS. The common cyberattack types identified in the review are defined and categorised in below. Mitigation strategies were presented in 131 of the records. An additional 29 records outlined cyber risk or cyberattack type, but also presented a specific countermeasure to potentially mitigate the threat discussed. A total of 27 records presented findings relevant to the Australian context. A summary of findings is presented in and .
Table 1. HCS cybersecurity attack and threat categories.
Table 2. Summary of findings – Theme 1 Cybersecurity Threat and Risk Landscape.
Table 3. Summary of findings Theme 2 – Cybersecurity Capability, Countermeasures and Mitigation strategies.
Table 4. International regulatory frameworks for data privacy and security.
Ten systematic reviews were identified as part of the search, 5 of which were published since 2018. There were 32 Reports included as relevant to this review. These included official Government responses to data breaches (n = 3), Australian Government publications (n = 9), cybersecurity industry benchmark reports (n = 9), the Royal Australian College of General Practitioners cybersecurity position paper (n = 1), and finally a joint academic and consumer group report. Grey literature was identified and included to address publication bias. A total of 15 Conference Proceeding papers and 4 dissertation thesis papers were identified. The results are summarised in –. shows HCS Cybersecurity Attack and Threat Categories, shows a summary of findings under Theme 1 (Cybersecurity Threat and Risk Landscape), shows a summary of findings under Theme 2 (Cybersecurity Capability, Countermeasures and Mitigation Strategies) and shows the identified international regulatory and legislative frameworks for data privacy and security.
Theme 1 – Emerging trends in cybersecurity risk
Cyber-attacks can occur at any connection of the network and at any endpoint. Interoperability of software, operating platforms, medical device interfaces and information exchange networks is an essential requirement of a digitalised health system and is crucial to cybersecurity risk management.Footnote36 The emergence of medical cyber physical streams, wireless connectivity and the advent of medical applications in healthcare have exponentially increased attack surfaces and vectors.Footnote37 Protecting every entry point to the health system is now impossible.Footnote38
Medical cyber physical systems
This term encapsulates Medical Internet of Things (MIoT) and medical devices, both implantable and wearable. Medical Cyber-Physical Systems (MCPS) are increasingly used in hospitals to provide high-quality healthcare and have emerged as promising platforms for monitoring and controlling multiple aspects of patient health.Footnote39 It is estimated there will be 20 billion connected devices by 2020, and 50 billion by 2028.Footnote40 The intrinsic features of MCPS increase their inherent security risks.Footnote41 These features make MCPS myriad, mobile, heterogenous and increasingly ubiquitous.Footnote42 They are often left unattended (as in implantable devices) to record intimate physiological data and are constrained in size, power and memory function which provides them only basic security capability.Footnote43 MCPS features make them vulnerable to compromiseFootnote44 meaning their connection to and reliance upon the healthcare network significantly increases the cybersecurity risk to the entire healthcare system.Footnote45 MCPS have become considerable potential attack vectorsFootnote46 to enable intrusion by malicious actors, installation of malware and alteration of treatment delivery.Footnote47 Cybersecurity measures such as vulnerability scans or patch management are often not availableFootnote48 or only possible by manufacturers.Footnote49 There exists an international lack of clarity on post-sale ownership, software update and security regulation of MCPS.Footnote50 Manufacturers may be reluctant to provide documentation detailing device cybersecurity vulnerabilitiesFootnote51 or patching and upgrade policiesFootnote52 as this is viewed as proprietary information. The absence of healthcare standardsFootnote53 to promote MCPS interoperabilityFootnote54 increases incompatibilityFootnote55 between different healthcare systems and medical devicesFootnote56 and creates a healthcare vendor market that pushes patient devices to market before cybersecurity issues are addressed.Footnote57 The cybersecurity vulnerability of medical devices and the lack of vendor and regulatory oversight has been recognised as a strategic priority by the Australian Therapeutic Goods Administration.Footnote58
Data confidentiality, privacy and consent
Privacy of confidential patient data and issues concerning the use of personal information was the next sub-theme identified. Risk to personal information can be categorised as cybersecurity threats to healthcare confidentiality, accessibility and integrity.Footnote59 Confidentiality is compromised through loss of personal health records or data, as well loss of consumer confidence.Footnote60 Accessibility to health records, software platforms, operating systems and hardware is affected through denial of service (DoS) malware or ransomware attacks.Footnote61 Integrity of health data is exposed if it is corrupted, deleted or altered; or if wireless communication to essential devices or monitors are compromised.Footnote62
Healthcare is both a vulnerable and attractive target for cyberattack due to its economic sizeFootnote63 and broad attack surface.Footnote64 An increased focus by the health sector on cybersecurity is warranted considering the criticality of the health sector and the type of user information stored within health information systems.Footnote65 Health information and medical data are highly valuable assets to patients, healthcare providers and identity thieves alike.Footnote66 Estimates place health data as between tenFootnote67 and twenty timesFootnote68 more lucrative than credit card or banking details. Credit card or banking details can be changed if stolen. Uniquely identifiable health history or data cannot.Footnote69
Cloud computing
Cloud computing was identified as a cybersecurity risk to data and information both during transfer and storage. The huge volume of health information produced has made centralised storage, encryption, deployment and maintenance of data prohibitive at the individual organisation level.Footnote70 The advent of cloud computing allowed storage, processing and analysis of data to be outsourced to a remote server.Footnote71 Cloud models share the cost of data accessibility and management, as well as sharing the cybersecurity risks – the scalability and efficiency of cloud computing means any potential breach exposes data to a far wider audience.Footnote72 There are two attack vectors possible with cloud storage – attacks to data at rest which modifies or replaces information; and attacks to data in motion occurring during transfer to or from geographically distributed cloud servers. Encryption technology is essential to ensure the security of patient health information and data stored on cloud platforms.Footnote73 A compromised host operating system could enable attackers to access hypervisor processes and services (such as a virtual machine monitor, a computer software, firmware or hardware that creates and runs virtual machines) and, potentially, any client application.
Malware
Records under this sub-theme discussed malware generally or applied examples such as the WannaCry attacks in the UK. Malware attack types and threat categorisation is outlined in detail in .
Health application (‘app’) security
The combined ubiquity of use and paucity of security provisions of Health apps are recognised as an increasing cybersecurity risk to the confidentiality of personal data and to the integrity of interconnected HCS infrastructure. Health apps can generate, store, and process huge volumes of identifiable health data.Footnote74 The ubiquity, simplicity, low cost and improved encryption of WhatsApp, makes it attractive for telemedicine servicesFootnote75 in resource constrained settingsFootnote76 and to facilitate professional networks and team communication.Footnote77 Use of WhatsApp is now so commonplace amongst clinicians that urgent guidelines are required to ensure that clinicians do not inadvertently breach patient privacy or confidentiality.Footnote78
Mental health apps are promoted by health services as a discreet, accessible and affordable alternative to face-to-face therapy.Footnote79 However, little research exists examining the safety and security of apps in medical practice, or of the proliferation of apps endorsed for mental health and dementia. A recent Australian study found that over half of government endorsed apps did not have a privacy policy to inform users how personal information would be collected, retained or shared with others.Footnote80 Patient confidentiality and safetyFootnote81 or the security of communications,Footnote82 are often not considered by app developers who are largely unregulated in terms of content, authorship or trustworthiness.Footnote83 The author of a cross-sectional survey investigating the privacy and information security of health apps in wearable devicesFootnote84 identified a lack of awareness among respondents (n = 106) regarding the confidentiality or security of the data collected from their wearable device apps, including what was obtained and how it was transmitted or stored. The author postulates that these results reflect a wider lack of knowledge about potential data security and privacy risks throughout the general population. That these apps have received government endorsement for use in those with dementia and mental illness is of concern. Without adequate security provisions in place, health applications can be vulnerable to both active and passive attacks, resulting in data modification or theft.Footnote85
Insider threat
That cybersecurity mechanisms within health do not appropriately address the issue of insider threat as the ‘entry point’Footnote86 for ransomware was the final sub-theme identified (n = 7). Most data breaches involve some level of insider cooperation, either intentional or not.Footnote87 Not recognising or responding to phishing emails remains a substantial problemFootnote88 with email the most common vector through which healthcare organizations are attacked.Footnote89 Most insider issues are due to ignorance rather than malice, but accidental error is equally damaging, making the lack of health information technology and cyber-hygiene knowledge an important threat. Studies indicate that respondents use weak or insecure passwords and are unaware of data security violation procedure.Footnote90 Malicious intent as it relates to cyber-attacks is poorly understood and requires the integration of human factors into cybersecurity risk assessment to fully understand and characterise its impact upon mitigation strategies.Footnote91 Inadvertent information leakages will remain inevitable due to the innumerable risks associated with collaborative sharing in complex healthcare network systems.Footnote92
Theme 2 – cybersecurity capability, countermeasures and mitigation strategies
The mitigation of risk to and protection of sensitive health information is now a global concern. The concept of a Cybersecurity Centre for Threat Control (based on the US Centers for Disease Control or a Cyber World Health Organisation)Footnote93 is suggested to enable global recognition of the need for international collaboration to combat cybercrime. The incorporation of data breach response into organisational disaster plans, along with proactive partnerships between governments, industry and providers to enhance and develop collective security across healthcare sectors is advocated.Footnote94
Cryptographic architecture or technological solutions
There is strong emphasis, both in the international and Australian records, upon technological solutions and advanced cryptology to promulgate cybersecurity solutions. The greatest number of records identified (n = 63) concerned technological cybersecurity protective architecture, often developed by the authors of the records. It is beyond the scope of this paper to compare and discuss the different cryptographic security available to address data sharing and storage of patient information across network systems, cloud environments or through remote patient monitoring systems.Footnote95 However, two cryptographies will be briefly mentioned due to their broad applicability and potential benefit for health specific challenges. The first, homomorphic encryption (HE) ensures strong security and privacy guarantees whilst enabling analysis on encrypted data and sensitive medical information.Footnote96 Fully homomorphic encryption is versatile but has substantial computational requirements that at present slows processing significantly.Footnote97 HE can also be used in mobile devices to transfer and store medical data without decrypting it, preserving privacy if a node is compromised.Footnote98
The second is Blockchain. Blockchain is a peer-to-peer distributed ledger technology that was initially used in the financial industry.Footnote99 Its characteristics of decentralization, verifiability and immutability enable blockchain to securely store personal medical data.Footnote100 Immutability ensures that any data, once stored in blockchain, cannot be altered or deleted.Footnote101 Applications in health include integration of health information,Footnote102 aggregation of data for research.Footnote103 In blockchain all the data, including the keywords and the patients’ identity are public key encrypted with keyword search. Challenges to blockchain include scalability, security and cost.Footnote104 Whilst blockchain itself is secure, it can be accessed through stolen credentials and root privilege exploits.Footnote105 Blockchain technology will require more research before large-scale production implementations.
Risk assessment and governance
Healthcare data breaches continue to riseFootnote106 with at least one data breach per day in the health industry globally.Footnote107 The average total cost of a healthcare data breach in 2019 was 6 USD.45 million compared to the 2017–18 average of 4 USD.08 million. This is 65% higher than the average total cost of a data breach in any other industry.Footnote108 On average, it takes the healthcare industry longer than any other to identify (mean 236 days) and rectify (93 days) a data breach.Footnote109 The longer a breach goes unnoticed, the greater the estimated cost. The importance of comprehensive cybersecurity risk assessment therefore cannot be underestimated in order to proactively identify vulnerabilities and detect threats or system breaches.Footnote110 This must include detailed assessment and analysis of the cybersecurity risk and vulnerability of all information technology hardware, software, MCPS and vendor or third-party partner cybersecurity agreements.Footnote111 Healthcare cybersecurity risk assessments and strategy frameworks should be standardised across jurisdictions and should include stipulations that demand vendor cybersecurity compliance and accountability.Footnote112 The National eHealth Security and Access Framework v4.0 (NESAF) is the Australian cybersecurity risk assessment framework developed to guide health sector data protection and eHealth security.Footnote113 The applicability, practicality and adoption of NESAF in practice is difficult to determine. The National Institute of Standards and Technology (NIST) Framework, which was developed in the US as a healthcare specific cybersecurity assessment model, could be adopted to the Australian healthcare context,Footnote114 and is used in HCS across the US.
‘Whitehat’ or ‘Ethical’ hackersFootnote115 should also be utilised to regularly test and assess cyber vulnerabilities. ‘Whitehats’ are professional hackers who undertake penetration and infiltration exercises and attempt to breach cybersecurity defences.Footnote116
Regulation and/or legislation
Securing the privacy of collected information and data is a major concern of patientsFootnote117 and the reason why many withhold consent for the use of their data in research.Footnote118 Patient privacy specifically refers to ‘the right of patients to determine when, how, and to what extent their health information is shared with others.’.Footnote119 Regulatory and policy oversight can decrease data and privacy breaches, as indicated by the HIPAA Omnibus Rules 2013Footnote120 which restricted healthcare vendor access to patient information.Footnote121 However comprehensive policy will not guarantee cybersecurity if not reflective of actual healthcare practice, culture or infrastructure limitations, as evinced in the NHS with WannaCry. Nor will it entirely protect against insider agents.Footnote122
A comparison of international privacy and security frameworks and regulations is presented in .
Holistic approach toward proactive cybersecurity culture
There is recognition within the international literature that healthcare cybersecurity is a complex socio-technical challengeFootnote123 requiring a holistic integrated approachFootnote124 to improve staff awareness,Footnote125 competence,Footnote126 and mitigation of threats across the industry. The international records also highlight the importance of developing a proactive cybersecurity culture,Footnote127 in which compliance to protecting information is embedded.Footnote128 Significantly, this theme is not discussed within the Australian records.
There is also recognition that merely enforcing security policies and procedures will not drive cultural change or learning.Footnote129 Healthcare leadership must embrace cybersecurity and develop strong cultures of cyber-vigilanceFootnote130 throughout organisations and amongst all staffFootnote131 to develop a robust, proactive incident response. Building a culture that systematically and continuously analyses the cyber context of an organisation will enable vulnerabilities and threats to be identified.Footnote132
Education and simulated environments
That staff cybersecurity education is the most important strategyFootnote133 against data breaches is not addressed in the identified Australian records. The essential need for comprehensive employee training and educationFootnote134 to enable the identification and assessment of riskFootnote135 is discussed throughout the international records. Cybersecurity simulation modelsFootnote136 indicate that experienced managers make less effective cybersecurity decisions than novices, as they are more likely to seek an optimal decision utilising past experiences. The unpredictable ‘zero-day’ cyber-attacks and ever evolving nature of cyber threats often means optimal reactive decisions are not possible. Rather, the capability to make proactive preventative decisions is key. As employees are often the inadvertent facilitators of security breaches,Footnote137 behavioural skills training and education to raise privacy-protection awareness and change habitual information technology habits into conscious cybersecurity decisions is required.Footnote138 Staff will engage with cybersecurity if interventions are not costly (i.e. time consuming or onerous) and if self-efficacy is enhanced through active involvement in the training.Footnote139 Simulation based trainingFootnote140 to practice and develop cybersecurity capabilities can facilitate this.Footnote141 The magnitude of cybersecurity organisational capability and individual employee skills required to mitigate the risk of vulnerabilities and breaches cannot be underestimated.Footnote142
Capability and cyber maturity
Cybersecurity capability is identified as a strategic asset that every health organization must adopt,Footnote143 along with the concepts of building organisational resilience and the capacity to learn from mistakes.Footnote144 Cybersecurity capability includes the skills, knowledge and competenceFootnote145 of the workforce, organisation, sector and nation to detect, mitigate and protect against threat. The Australian HCS is recognised as having low cybersecurity capability maturity.Footnote146 The lack of an Australian healthcare cybersecurity capability model is recognised as a significant security risk in a country that has adopted an opt-out digitalised health record with MHR.Footnote147
Cyber-hygiene practices
Organisational cyber-hygiene practices are recognised as mandatory safeguards that include email data encryption of patient information, antivirus software, software updates, and at least two-factor authentication patient data stored or shared on cloud platforms.Footnote148 Cyber-hygiene can be practised at employee level, such as in recognition and escalation of suspicious emails, or through enforcement of organisational policy regarding information sharing and protection.Footnote149
Theme 3 – current cybersecurity issues within Australia
“In Australian cybersecurity, there are only two types of healthcare organisations – those that know they’ve been hacked and those that don’t know they’ve been hacked”.Footnote150
The average cost of a data breach in Australia in 2018 was estimated to be 2 USD.5 million.Footnote151 It takes Australia a mean of 200 days (compared to 185 in 2017) to identify a data breach and 81 days to contain the breach incidents.Footnote152 A cross-sector survey of 1894 senior executives and senior IT managers found that almost 70% of data breaches reported in Australia during 2018 were directly attributed to human error.Footnote153 The number of documented data breaches involving the My Health Record (MHR) system in 2017–18 was 42, an increase from 35 the preceding year.Footnote154
At present the Office of the Australian Information Commissioner (OAIC) Notifiable Data Breaches only cover private providers and not public institutions or healthcare systems. This makes it extremely difficult to gauge an accurate picture of the cybersecurity landscape within Australia. An independent cybersecurity report of 4067 cyber incidents, many of which were not included in the quarterly Notifiable Data Breach reports, was undertaken during 2018.Footnote155 The report analysis estimated that there were 445 healthcare cyber incidents in Australia in 2018 which equated to almost 24% of the Australian cyber breach total. Crucially, the report found that the healthcare industry had the lowest cybersecurity capability maturity of any Australian industry to identify and manage risks and to protect against or contain attacks. Specifically, the health sector lacks the capability to anticipate and respond to vulnerabilities and has a very high risk of experiencing a cyber incident within 12 months.Footnote156 In 2018, no community healthcare providers had a dedicated budget for cybersecurity, and only 16% of public hospitals allocate funds specifically to cybersecurity.Footnote157 Over 40% of clinical, specialist non-clinical, and administrative health staff believe they have no responsibility for cybersecurity, and 6.2% of Australian health organisations are unable to undertake operating system updates or patches due to legacy and end of life systems.Footnote158
MHR is the Australian digital health record that supports clinical care and is accessible to authorised health care providers wherever and whenever health services are initiated. The accuracy and relevance of the MHR is a joint responsibility of the individual and health care provider/s.Footnote159 MHR is intended as an integrated eHealth Record ‘to provide a consolidated record of an individual’s health information for consumers to access and as a mechanism for improving care co-ordination between care provider teams’.Footnote160 However, this probably remains an ambitious ideal given the unique challenges and complexities of the Australian federated funding model combined with the ambiguous responsibilities of the commonwealth and states in relation to different aspects of healthcare delivery.Footnote161 As of 28 July 2019, MHR has a 90.1% participation rate across Australia, with 16,400 healthcare providers registered to the system.Footnote162 The legislative framework underpinning the My Health Record system include My Health Records Act 2012,Footnote163 My Health Records Rule 2016 and My Health Records Regulation 2012.
The Australian Digital Health Agency (ADHA) is the System Operator of MHR. Healthcare organisations and providers are required to report potential or confirmed data ‘breaches’ involving MHR to the System Operator (the ADHA). MHR data breaches must also be reported to the OAIC, except where the healthcare provider organisation is a state or territory authority.Footnote164 The Digital Health Cyber Security Centre (DHCSC) provides operational security support for the MHR on behalf of the ADHA. During a national healthcare sector cyber crisis, the DHCSC is responsible for coordinating responses across the health sector in liaison with other Government organisations such as the Australian Cyber Security Centre and CERT (Computer Emergency Response Team) Australia.Footnote165 In other words, the ADHA coordinates the cybersecurity response for major for cybersecurity breaches potentially caused by its own system vulnerabilities.
There is a paucity of research within Australia to measure or gauge Government, public-private sector or users’ cybersecurity capacity to adopt or engage with an electronic health system such as MHR,Footnote166 or to measure public understanding or perceptions of the potential use of their data in research.Footnote167 A 2016 studyFootnote168 of the Personally Controlled Electronic Health Record (PCEHR) which essentially incarnated into MHR in July 2018, identified a multitude of security weaknesses. PCEHR consisted of a distributed network of interconnected systems with multiple interfaces required to enable a variety of providers, services and applications have access. The potential security weaknesses included system misconfiguration and implementation flaws, inconsistent authorisation policies and authorisation errors, and insecure transfer of privileges between healthcare providers in the PCEHR system.
An analysis of the timeline of Australian electronic health record development and an examination of the failed ‘HealthConnect’ project which preceded it (and which subsequently has been removed from Department of Health websites)Footnote169 concludes that enduring tensions exist between those seeking to enhance the widespread availability of individual health information reform, and those who view it as a threat to privacy. There appears to be an inability to seek compromise or learn from divergent viewpoints and values. This has been particularly evident since the transition of MHR to an opt out systemFootnote170 which commenced on 16 July 2018 and was extended to 31 January 2019.
An important note of interest and consideration in the Australian cybersecurity context is that the healthcare industry is not included as critical infrastructure in the Australian Security of Critical Infrastructure Act 2018. In contrast, healthcare is recognised as critical infrastructure internationally.Footnote171 The cybersecurity challenges created by digital health transformation requires universal cross-sectoral governance and coordination that emphasises ‘healthcare as Critical National Infrastructure’.Footnote172 This concept must be identified and protected. Creating cybersecurity silos in which healthcare is separate from other critical infrastructure could potentially weaken healthcare cybersecurity defence and capability.
Health security breaches in Australia
The following section draws on current open access media reports to ascertain the extent of health related ‘breaches’ or ‘incidents’ occurring within Australia. It is not intended to be exhaustive, but rather indicative of public awareness around the issues of cybersecurity as it relates to health generally and MHR specifically. As this is an emerging topic there are limited scholarly studies published.
Medicare has been plagued with security and privacy issues. Medicare details have been found available for sale on the dark web,Footnote173 though any ‘breach’ of MHR was denied by ADHA: ‘there has not been a cyber security breach of our systems as such, but rather it is more likely to have been a traditional criminal activity’ (involving a likely insider).Footnote174 In 2016 the Australian government published a deidentified data set comprising the health details of 10% of the Australian population with information collected since 1984.Footnote175 A week later a group of University of Melbourne academics privately informed the government that it had been able to re-identify the entire data set. The government immediately withdrew the data set from the website, however access logs indicated the data set had been downloaded 1,500 times but could not indicate who had accessed it.
The Australian Bureau of Statistics (ABS) was ‘attacked’ by Macquarie University academics to illustrate weaknesses in the TableBuilder tool used by ABS to enable low dataset counts to be retrieved. TableBuilder creates tables, graphs and maps of Australian census data. As the tool could be manipulated through unlimited query counts to include cell counts of 1, it was theoretically possible to re-identify individuals from census data.Footnote176 The ABS were made aware of the vulnerability and have consequently changed the ToolBuilder interface.
HealthEngine was the government endorsed health appointment and scheduling app recommended by the ADHA. HealthEngine was exposed for editing negative reviews of GP practices, revealing the identifying details of 75 users via a website flaw and sharing hundreds of patient’s data to personal injury legal firms.Footnote177 HealthEngine provided access to MHR information such as Medicare records, test results, scans and prescriptions, for their app users to view on mobile phones.Footnote178
The difficulty of estimating the extent of cybersecurity breaches at state level is also raised. The state of NSW does not currently have a mandatory notifiable data breach reporting requirement, with the NSW Privacy Commissioner recommending a voluntary reporting scheme only.Footnote179 As the National Data Breach scheme covers only federal government agencies and private sector organisations regulated by the Australian Privacy Principles, it virtually impossible to determine at a national level how many data breaches have occurred in the patient record systems of state-based health services.Footnote180
In a politically interesting and provocative act, the Victorian Auditor General hacked into his own health databases to expose sensitive patient information.Footnote181 ‘Patient data in Victoria’s public health system could be easily hacked in a system riddled with weaknesses. The sector is highly vulnerable to cyber-attacks but staff awareness of data security is low, with issues around physical security, password management and other access controls’.Footnote182 The official Auditor General report of Victorian security vulnerabilities states: ‘There are key weaknesses in health services’ physical and logical security covering password management and other user access controls. Staff awareness of data security is low, which increases the likelihood of success of social engineering techniques such as phishing or tailgating into corporate areas where ICT infrastructure and servers may be located’.Footnote183 Also in Victoria, Cabrini Hospital based Melbourne Heart Group was unable to access approximately 15,000 files in February 2019 due to a server ransomware attack which corrupted and encrypted data. The ransom was reportedly paid: ‘The My Health Record database will be an enormously tempting target for cybercriminals, not just now but for years, if not decades, to come.’Footnote184
These cybersecurity breaches whether notifiable or not, highlight the need for expertly trained cybersecurity professionals within the healthcare system. At present however, across NSW and Australia, there is a significant shortfall in sufficiently skilled and experienced cybersecurity experts required to develop products and services to meet ever evolving cybersecurity threats.Footnote185 A new Certificate IV in cyber security was accredited nationally and is being implemented in NSW. One of the key aspects of the NSW Cybersecurity Strategy is the alignment of streamlined cybersecurity training with industry. The report does not specifically mention the healthcare sector as an area of need.
The idea of informed consent is contentious within MHR, in that implied consent is taken to have been granted if there has been no active opt-out of the MHR system. Several authors question the notion of ongoing consent inherent within systems such as MHR.Footnote186 ‘The MHR Act does not specify the types of applicants that may access MHR system data for secondary use’.Footnote187 Ongoing consent for secondary use of health information and data through MHR is condoned by the ADHA. Section 66(2) of the FrameworkFootnote188 specifically enables ‘secondary use of identified MHR data, noting that the System Operator (ADHA) is authorised to collect, use and disclose an individual’s health care information (i.e. identifiable information) with the consent of the individual’.Footnote189 How and when this consent is obtained, and by whom is not elucidated. The concept of ongoing consent as a breach of trust was raised when the Department of Human Services (DHS) acted on behalf of a third-party research organisation to access Medicare prescription data and contact (via letter) 50, 000 Australians who had been prescribed Lithium.Footnote190 DHS claims that researchers had no access to private patient information disregards the point that an open access letter did contain private and potentially damaging information, as well as avoiding the issue that consent to share private prescription data had not been sought from any of the people contacted. How was consent obtained for secondary use in this case?
Health management training in Australia
Health management courses in Australia (such as Masters in Health Management) are a prerequisite for health manager jobs, yet these do not usually cover cybersecurity in their curricula. We did not identify any Masters level degree in health or hospital management which teaches cybersecurity. The Australasian College of Health Service Management (ACHSM) Guideline for Universities (2017) lists the five core competencies required of health service managers including the requisite knowledge, skills and behaviours expected of graduates. Cybersecurity (risk awareness, assessment, mitigation or management) is not listed. Nor is it mentioned by RACMA, the other peak body for health management.
Discussion
The healthcare sector is a complex system of interconnected organisations, providers, staff and patients, of which MHR is an important component. As highlighted throughout, human factors play a crucial role in cybersecurity with employees often the weakest link in organizational cybersecurity.Footnote191 However, lack of mandatory reporting of breaches, lack of health management training in cybersecurity, lack of investment in cybersecurity infrastructure in health systems and use of old, legacy computing systems by hospitals, leaves Australia vulnerable to cyberattacks. The potential advantages of a centralised and accessible patient health record are clear, but the cybersecurity issues inherent in collating, transferring and storing electronic patient records and health information must be comprehensively addressed. The Privacy Act 1988 protects the personal information of Australians in federal agencies or private organisations but does not cover state and territory public hospitals or health services. The OAIC Notifiable Data Breach Scheme (NDBS) has the legislative power under the Privacy Act IIIC to enforce penalties for data breaches. As of February 2018, no fines have been issued despite 967 reported breaches that have affected tens of thousands of Australians. This is in stark contrast to HIPAA in the US which accredits health care organisations to enforce cybersecurity and data protection compliance, and which issues penalties of between 50,000 USD to 1.5 USD million US for noncompliance. HIPAA was amended in 2005 to protect the electronic protected health information stored, collected or transferred by any healthcare provider. Even with the protections of HIPAA, the US has suffered ransomware attacks on hospitals and other health data breaches. Without any such protection, Australia would be even more vulnerable, and should consider adopting a data protection scheme and framework that includes a critical analysis of the capability of multiple health providers and organisations with disparate operating systems to ensure health data security, confidentiality and integrity. Mandatory reporting of breaches should also be adopted. Cybersecurity capability must integrate all aspects of information security measures to protect health information from malicious access or breach.Footnote192 Currently this provision does not exist within Australia. Health budgets should include resources to upgrade computer systems and hire cybersecurity personnel.
Data breaches adversely affect patient and community faith in healthcare to protect privacy and can lead to health information being withheld from healthcare providers due to confidentiality concerns.Footnote193 Non-disclosure of information could lead to inaccurate or delayed diagnoses and compromised patient safety. However, it is essential that allaying security and privacy concerns and protecting provider reputation not become motivation to withhold cybersecurity breach reporting. Mandatory reporting and open discussion of cybersecurity incidents and breaches can facilitate real world learning and become the basis for education and training programmes. Cybersecurity capability is the capacity to manage previously unknown and seen situations and is best developed through multiple experiences of dealing with new situations.Footnote194
There are significant concerns regarding the ethics and consent in MHR. The rights of the patient regarding information collected about them, especially when considering ‘ongoing consent’ for secondary research sharing and use are paramount.Footnote195 It could be argued that the least influential and most vulnerable people are being co-opted into MHR by an opt-out system, without their informed consent, further cementing health inequity and disparity. The Government has not fully addressed access and consent issues relating to many vulnerable communities including adolescents, abuse victims, sex workers, people with HIV and those with mental illnesses.Footnote196 MHR raises the concept of a social licence not only for the open disclosure of potential cybersecurity risks, but also regarding the secondary use of health record data for research.Footnote197 Consumers are entitled to control how their data are used, but this must be balanced to ensure that informed consent can be obtained to enable high quality primary and public health research.
It is impossible to completely mitigate cyber threats: ‘Today it has become a question of “when”, and “at what level”’Footnote198 systems such as MHR will be breached. This does not invalidate the need for comprehensive, integrated and accessible electronic health records such as MHR. Instead it indicates the need for open disclosure of and proactive dialogue about cyber-attacks, innovate and holistic strategies and policies to reduce cyber threat, and cyber education and training for all health staff in order to develop cybersecurity awareness and capability. A healthcare culture that shares risk and threat informationFootnote199 is as essential as infrastructure management such as replacing legacy software and hardware, patching and updates and undertaking comprehensive risk assessments of connected devices.Footnote200
The overall cybersecurity maturity of healthcare organisations should be assessed to ensure a secure healthcare environment of interconnected systems.Footnote201 The multiple health providers, organisations and agencies combining information into a comprehensive electronic health record provide innumerable potential attack interfaces. Cybersecurity threats are emerging from new vectors. Healthcare is also vulnerable from rapidly evolving technologies including wireless sensor networked medical devices, healthcare applications, and implantable medical devices. ‘Enhancing the security and privacy in MCPS remains a serious challenge demanding careful considerations and joint efforts by the industry, the health systems, and the research community’.Footnote202
Limitations
There are three main limitations to this systematic review. The first is that the cybersecurity landscape is evolving at such an exponential rate, that new information is emerging regularly. The second is that as this is such an emerging field, the number of scholarly research articles published on this topic is sparse. Third, the scope of this review was broad and some themes were not able to be considered in detail.
Conclusion
This review investigates the body of literature on global cyberattacks against the healthcare sector, in order to categorise the cyber threats to health, and present mitigating countermeasures or protective strategies in relation to a universal electronic health record in Australia. Cyberattacks against healthcare are rising due to the lucrative patient data available in digitalised health systems, and because healthcare has poor cybersecurity defences and awareness. Australia lacks some of the protections that other countries such as the US has, such as the HIPAA law and mandatory reporting of breaches. Outdated health computing systems and lack of investment by the hospital sector in cybersecurity is an additional problem. Health management training lacks cybersecurity content, and until this is addressed, the health system will remain vulnerable. If healthcare mangers are not taught essential cybersecurity skills, it is unlikely they will lead change in the development of healthcare cybersecurity capability and resilience in the workplace. There is no way to completely mitigate the risk of a cybersecurity incident or breach within the healthcare system, globally or within Australia. However, building a proactive healthcare culture of cybersecurity maturity can help to reduce cybersecurity risk.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Notes on contributors
K. L. Offner
K. L. Offner is a clinical nurse educator, currently studying a Master of Public Health and Health Management.
E. Sitnikova
Dr, E. Sitnikova, PhD, BE (Hon), CSSLP, SFHEA is is an award-winning academic and researcher at UNSW Canberra and Adjunct Professor at University of Alabama in Huntsville. She is a global leader in cutting-edge research in Critical Infrastructure protection, focusing on intrusion detection for Supervisory Control and Data Acquisition (SCADA) systems cyber security, cyber-physical systems and Industrial Internet of Things (IIoT). Given the increasing number of cyber-attacks globally, Elena’s research explores systems resilience and the use of artificial intelligence in the analytics of abnormal data that may affect critical systems. Her contribution in the field is demonstrated through the recent Spitfire Memorial Defence Fellowship Award. She is one of the first Australians to be certified in CSSLP - Certified Secure Software Lifecycle Professional
K. Joiner
Dr, K. Joiner is Group Captain (Ret’d), PhD, MMgmt, MSc, BEng(Aero), CPEng, CPPD, MAIPM, MIEAust and Senior Lecturer Test, Evaluation & Aircraft Systems. He is an Educationally Focussed Academic at The UNSW Canberra Cyber at the Australian Defence Force Academy (ADFA)
C. R. MacIntyre
Professor C. R. MacIntyre MBBS (Hons 1), M App Epid, PhD, FRACP, FAFPHM is Professor of Global Biosecurity and NHMRC Principal Research Fellow at the Kirby Institute, UNSW Australia, and an adjunct professor at Arizona State University. She is a specialist physician with a masters and PhD in epidemiology. She leads a research program in control and prevention of infectious diseases, spanning epidemiology, risk analysis, vaccinology, bioterrorism, mathematical modelling, public health and clinical trials. She is best known for research in the detailed understanding of the transmission dynamics and prevention of infectious diseases, particularly respiratory pathogens such as influenza, tuberculosis, bioterrorism agents and vaccine-preventable infections. She has led the largest body of research internationally on face masks and respirators in health care workers. She won many career awards including the Sir Henry Wellcome Medal and Prize, from the Association of Military Surgeons of the United States for her work on a risk-priority scoring system for category A bioterrorism agents; and the highest national award in infectious diseases, the Frank Fenner Award for Research in Infectious Diseases. She has also won the CAPHIA Research Team Prize, The Public Health Association of Australia National Immunisation Achievement Award, the Peter Baume Public Health Impact Prize and a Harkness Fellowship. She has over 370 peer reviewed publications and sits on several expert committees and editorial boards including Vaccine, BMJ Open, Global Biosecurity and Epidemiology & Infection. She is currently on the Global Accreditation Board for TEPHINET, the network of global field epidemiology programs. She also has an interest in the ethics of medicine, and specifically in dual-use research of concern and has been on the World Organisation for Animal Health (OIE) committee for developing Guidelines For Responsible Conduct in Veterinary Research Identifying, Assessing and Managing Dual Use Research.
Notes
1. Abd-alrazaqa et al., “Factors that affect the use of electronic personal health records among patients: A systematic review.”
2. Zeb et al., U-prove based security framework for mobile device authentication in eHealth networks.
3. Abouzakhar and Angelopoulou. Internet of Things Security: A Review of Risks and Threats to Healthcare Sector.
4. Global Digital Health Partnership, Securing Digital Health 2018.
5. BDO USA Healthcare, Brace for the Breach – Cyberthreat Insights 2019.
6. Institute for Critical Infrastructure Technology (ICIT). Industry Brief: Hacking Healthcare.
7. MacIntyre et al., “Converging and emerging threats to health security.”
8. Ibid.
9. IT News, “Hack linked to attack on US insurer Anthem”.
10. Forcepoint Whitepaper. Life Support: Eliminating Data Breaches in the Healthcare Sector.
11. Gordon, Fairhall and Landman, “Threats to Information Security – Public Health Implications.”
12. Jalali & Kaiser, “Cybersecurity in Hospitals: A Systematic, Organizational Perspective.”
13. Argaw et al., “The state of research on cyberattacks against hospitals and available best practice recommendations: a scoping review.”
14. See note 12 above.
15. Sittig & Singh. “A Socio-technical Approach to Preventing, Mitigating, and Recovering from Ransomware Attacks.”; Small et al., “Patient Perceptions About Data Sharing & Privacy: Insights from Action.”
16. Kruse et al., “Cybersecurity in healthcare: A systematic review of modern threats and trends.”
17. National Audit Office Report, Investigation: WannaCry Cyber Attack and the NHS.
18. Wirth A., “Cyberinsights. Hardly Ever a Dull Moment: The Ongoing Cyberthreats of 2017.”
19. See note 17 above.
20. Walker-Roberts et al., A Systematic Review of the Availability and Efficacy of Countermeasures to Internal Threats in Healthcare Critical Infrastructure.
21. O”Sullivan
22. Schwartz et al., “The evolving state of medical device cybersecurity.”
23. See note 17 above.
24. Pratt, “How cyberattacks can impact physicians.”; Connory, 2019 Annual Report. State of cyber security.
25. See note 20 above.
26. Farringer, “Cybersecurity Report Identifies Unique Challenges to Tackling Cybersecurity in Health Care.”; Sedlack, Understanding Cyber Security Perceptions Related to Information Risk in a Healthcare Setting.
27. Boddy et al., A Study into Data Analysis and Visualisation to increase the CyberResilience of Healthcare Infrastructures.
28. Akinsanya, Papadaki & Sun. Current Cybersecurity Maturity Models: How Effective in Healthcare Cloud?.
29. See note 27 above.
30. Sittig & Singh. “A Socio-technical Approach to Preventing, Mitigating, and Recovering from Ransomware Attacks.”
31. Reagin & Gentry. “Enterprise Cybersecurity: Building a Successful Defense Program.”
32. Safavi et al., Cyber Vulnerabilities on Smart Healthcare, Review and Solutions.
33. Carlton, Development of a Cybersecurity Skills Index: A Scenarios-Based Hands on Measure of Non-IT Professionals Cybersecurity Skills 2016.; NSW Dept of Industry. NSW-cyber-security-industry-development-strategy 2018.
34. Chen et al., “Blockchain-Based Medical Records Secure Storage and Medical Service Framework.”
35. Wilson & Khansa. “Migrating to electronic health record systems: A comparative study between the United States and the United Kingdom.”
36. Zaidan et al., “A Security Framework for Nationwide Health Information Exchange based on Telehealth Strategy.”
37. Nippon Telegraph and Telephone (NTT) Security. Global Threat Intelligence Report 2019.
38. Dogaru & Dumitrache, Cyber Security in Healthcare Networks. Conference Proceedings of the 6th IEEE International Conference on E-Health and Bioengineering – EHB 2017.
39. Chaudhry et al., POStCODE Middleware for Post-market Surveillance of Medical Devices for Cyber Security in Medical and Healthcare Sector in Australia.
40. See note 5 above.
41. Zhou et al., “The Effect of IoT New Features on Security and Privacy: New Threats, Existing Solutions, and Challenges Yet to Be Solved.”
42. Raber, McCarthy & Yeh. “Health Insurance and Mobile Health Devices: Opportunities and Concerns. JAMA.”
43. Almohri et al., On Threat Modeling and Mitigation of Medical Cyber-Physical Systems.
44. See note 27 above.
45. Zheng et al., From WannaCry to WannaDie: Security trade-offs and design for implantable medical devices.
46. Camara, Peris-Lopez & Tapiador, “Security and privacy issues in implantable medical devices: A comprehensive survey.”
47. Stern, “A life cycle approach to medical device cybersecurity.”
48. Rubenfire, “The nightmare scenario: dialing devices to deadly.”
49. See note 22 above.
50. See note 39 above.
51. See note 47 above.
52. Smigielski, “Hardening Infusion Pump Communication Software for Medical Device Cybersecurity.”
53. See note 39 above.
54. O”Dowd, “NHS patient data security is to be tightened after cyberattack.”
55. Jayaratne et al., “A data integration platform for patient-centered e-healthcare and clinical decision support.”
56. See note 35 above.
57. See note 43 above.
58. Holdsworth, Glisson & Choo. “Medical device vulnerability mitigation effort gap analysis taxonomy.”
59. Siddique et al., A survey of big data security solutions in healthcare.
60. Shenoy & Appel, “Safeguarding Confidentiality in Electronic Health Records.”
61. Wirth, “Cyberinsights. The Times They Are a-Changin”: Part One.”
62. Baranchuk et al., “Cybersecurity for Cardiac Implantable Electronic Devices: What Should You Know?”.
63. Blanke & McGrady. “When it comes to securing patient health information from breaches, your best medicine is a dose of prevention: A cybersecurity risk assessment checklist.”
64. Coventry & Branley. “Cybersecurity in healthcare: A narrative review of trends, threats and ways forward.”
65. Martin et al., “Cybersecurity and healthcare: How safe are we?”.
66. See note 16 above.
67. Beeksow, “Reducing Security Risk using data loss prevention technology.”
68. Kruse, Smith & Vanderlinden and A. Nealand. Security Techniques for the Electronic Health Records.
69. See note 11 above.
70. Lee, Moon & Park. CloudRPS: a cloud analysis based enhanced ransomware prevention system.; Abrar et al., “Risk Analysis of Cloud Sourcing in Healthcare and Public Health Industry.”
71. Sahi, Lai & Li. “Security and privacy preserving approaches in the eHealth clouds with disaster recovery plan.”
72. Sajid & Abbas. “Data Privacy in Cloud-assisted Healthcare Systems: State of the Art and Future Challenges.”
73. See note 71 above.
74. Rosenfeld, Torous & Vahia. “Data Security and Privacy in Apps for Dementia: An Analysis of Existing Privacy Policies.”
75. Kamel Boulos, Giustini & Wheeler. “Instagram and WhatsApp in Health and Healthcare: An Overview.”
76. Scott, “WhatsApp in Clinical Practice: A Literature Review.”
77. Chan & Leung. “Use of Social Network Sites for Communication Among Health Professionals: Systematic Review.”
78. Morris, Scott & Mars. “Security and Other Ethical Concerns of Instant Messaging in Healthcare.”
79. Parker et al., “How private is your mental health app data? An empirical study of mental health app privacy policies and practices.”
80. Ibid.
81. Huckvale et al., “Unaddressed privacy risks in accredited health and wellness apps: a cross-sectional systematic assessment.”; Mense et al., “Analyzing Privacy Risks of mHealth Applications.”
82. Thamilarasu & Lakin. “A Security Framework for Mobile Health Applications. Proceedings −5th International Conference on Future Internet of Things and Cloud Workshops (FiCloudW)”.
83. Grundy et al., Finding Peace of Mind: Navigating the Marketplace of Mental Health Apps, Australian Communications Consumer Action Network, Sydney.
84. Cilliers, “Wearable devices in healthcare: Privacy and information security issues.”
85. Al-Muhtadi et al., “Cybersecurity and privacy issues for socially integrated mobile healthcare applications operating in a multi-cloud environment.”
86. Spence et al., “Ransomware in Healthcare Facilities: A Harbinger of the future?”.
87. Yasnoff, Breach Risk Magnitude: A Quantitative Measure of Database Security.
88. Gordon et al., “Evaluation of a mandatory phishing training program for high-risk employees at a US healthcare system.”
89. Klas-CHIME, Whitepaper: How Aligned Are Provider Organizations with the Health Industry Cybersecurity Practices (HICP) Guidelines?.
90. Fernandez-Aleman
91. King et al., “Characterizing and Measuring Maliciousness for Cybersecurity Risk Assessment.”
92. See note 88 above.
93. Smith, “Malware and Disease: Lessons from Cyber Intelligence for Public Health Surveillance.”
94. Magnus, Public Report of the Committee of Inquiry (COI) into the Cyber Attack on SingHealth 10 January 2019.
95. Coventry & Branley. “Cybersecurity in healthcare: A narrative review of trends, threats and ways forward.”; Wang, Gao & Zhang. Searchable and revocable multi-data owner attribute-based encryption scheme with hidden policy in cloud storage.; Zhang, Xue & Liu. “Searchable Encryption for Healthcare Clouds: A Survey.”; Gardiyawasam Pussewalage & Oleshchuk. “Privacy preserving mechanisms for enforcing security and privacy requirements in E-health solutions.”
96. Raisaro et al., “Are privacy-enhancing technologies for genomic data ready for the clinic? A survey of medical experts of the Swiss HIV Cohort Study.”
97. Saleem et al., Survey on cybersecurity issues in wireless mesh networks based eHealthcare.
98. Wang & Zhang. Data Division Scheme Based on Homomorphic Encryption in WSNs for Health Care Wireless sensor networks.
99. Dubovitskaya et al., Secure and Trustable Electronic Medical Records Sharing using Blockchain.
100. Akinsanya, Papadaki & Sun. Current Cybersecurity Maturity Models: How Effective in Healthcare Cloud?; Carlton, Development of a Cybersecurity Skills Index: A Scenarios-Based Hands on Measure of Non-IT Professionals Cybersecurity Skills 2016.
101. Esposito et al., “Blockchain: A Panacea for Healthcare Cloud-Based Data Security and Privacy?”.
102. Park et al., “Is Blockchain Technology Suitable for Managing Personal Health Records? Mixed-Methods Study to Test Feasibility.”
103. See note 99 above.
104. Alonso et al., “Proposing New Blockchain Challenges in eHealth.”; Angraal, Krumholz & Schulz. “Blockchain Technology: Applications in Health Care.”
105. Firdaus et al., “Root Exploit Detection and Features Optimization: Mobile Device and Blockchain Based Medical Data Management.”
106. See note 35 above.
107. See note 10 above.
108. Ponemon Institute, Cost of a Data Breach Report 2019.
109. Verizon, 2019 Data Breach Investigations Report.
110. Connory, 2019 Annual Report. State of cyber security.; Ponemon Institute. Cost of a Data Breach Report 2019.
111. Holdsworth, Glisson & Choo. “Medical device vulnerability mitigation effort gap analysis taxonomy.”; Upendra et al., “Operationalizing Medical Device Cybersecurity at a Tertiary Care Medical Center.”
112. Terry, “HIPAA BREACH. Secure data & prevent fines.”
113. Australian Digital Health Agency, National health security and access framework – NESAF.
114. Akinsanya et al., Current Cybersecurity Maturity Models: How Effective in Healthcare Cloud? Online Proceedings of the 5th Collaborative European Research Conference.
115. Taylor, “An SOS on Cybersecurity: To protect patient data, hospitals beef up risk management programs. Hello, chief security officers and “white hat hackers”.
116. Perakslis & Califf. “Employ Cybersecurity Techniques Against the Threat of Medical Misinformation.”
117. Papoutsi et al., “Patient and public views about the security and privacy of Electronic Health Records (EHRs) in the UK: results from a mixed methods study.”
118. Carter, “Considerations for Genomic Data Privacy and Security when Working in the Cloud.”
119. Andriole, “Security of electronic medical information and patient privacy: what you need to know.”
120. HIPAA Omnibus Rule 2013 Summary.
121. Yaraghi & Gopal, “The Role of HIPAA Omnibus Rules in Reducing the Frequency of Medical Data Breaches: Insights from an Empirical Study.”
122. See note 20 above.
123. See note 30 above.
124. Natsiavas et al., “Comprehensive user requirements engineering methodology for secure and interoperable health data exchange.”
125. Pullin, “Cybersecurity: Positive Changes Through Processes and Team Culture.”
126. Rajamäki et al. Cybersecurity education and training in hospitals: Proactive resilience educational framework (Prosilience EF).
127. Coventry & Branley. “Cybersecurity in healthcare: A narrative review of trends, threats and ways forward.”; Verizon, 2019 Data Breach Investigations Report.; Nippon Telegraph and Telephone (NTT) Security. Global Threat Intelligence Report 2019.
128. Raths, “What to Do If a Breach Happens to You.”
129. Ropp & Quammen. “Protecting health data in a troubling time. Understand who and what you’re up against.”
130. Dameff et al., “Clinical Cybersecurity Training Through Novel High-Fidelity Simulations.”
131. See note 5 above.
132. Wickham, M. H. Exploring Data Breaches and Means to Mitigate Future Occurrences in Healthcare Institutions: A Content Analysis.
133. See note 16 above.
134. Gordon, Fairhall and Landman, “Threats to Information Security – Public Health Implications.”; Dameff et al., “Clinical Cybersecurity Training Through Novel High-Fidelity Simulations.”
135. Sedlack, Understanding Cyber Security Perceptions Related to Information Risk in a Healthcare Setting.
136. See note 12 above.
137. See note 11 above.
138. Zafar, Cybersecurity: Role of behavioral training in healthcare.; Sher et al., “Compliance with Electronic Medical Records Privacy Policy: An Empirical Investigation of Hospital Information Technology Staff.”
139. Blythe & Coventry. “Costly but effective: Comparing the factors that influence employee anti-malware behaviours.”
140. Gaynor, Omer & Turner. “Teaching EHRs security with simulation for non-technical healthcare managers.”
141. Zafar, Cybersecurity: Role of behavioral training in healthcare.
142. Carlton, Development of a Cybersecurity Skills Index: A Scenarios-Based Hands on Measure of Non-IT Professionals Cybersecurity Skills 2016.
143. See note 31 above.
144. See note 30 above.
145. Carlton, Development of a Cybersecurity Skills Index: A Scenarios-Based Hands on Measure of Non-IT Professionals Cybersecurity Skills 2016.
146. Connory, 2019 Annual Report. State of cyber security.
147. Burke et al., Cybersecurity Indexes for eHealth.
148. Pratt, “How cyberattacks can impact physicians.”
149. McSweeney, Motivating cybersecurity compliance in critical infrastructure industries: A grounded theory study.
150. Pinskier, Royal Australian College of General Practitioners.
151. Ponemon Institute. Cost of a Data Breach Report 2019.
152. Ibid.
153. See note 146 above.
154. Australian Digital Health Agency (ADHA). Annual Report 2017–18.
155. See note 146 above.
156. Ibid.
157. Health Informatics Society Australia, Healthcare-Cybersecurity-Report_June-2018.
158. Ibid.
159. Department of Health, Framework to guide the secondary use of My Health Record system data.
160. See note 154 above.
161. Garetty et al., “National electronic health record systems as wicked projects the Australian experience.”
162. My Health Record Statistics (28 July 2019).
163. My Health Records Act 2012.
164. Office of the Australian Information Commissioner, My Health Record Privacy.
165. Global Digital Health Partnership, Securing Digital Health 2018.; ADHA. About the DH Cyber Security Centre, ADHA.
166. See note 147 above.
167. Canaway et al., “Gathering data for decisions: best practice use of primary care electronic records for research.”
168. Zhou, Varadharajan & Gopinath. “A Secure Role-Based Cloud Storage System for Encrypted Patient-Centric Health Records.”
169. See note 161 above.
170. Australian Government. 14 November 2018. My Health Records (National Application) Amendment (Extension of Opt-out Period No. 2) Rules 2018.
171. Ogunlana, Countering expansion and organization of terrorism in cyberspace.; Shah, Protecting Australian critical national infrastructure in an era of IT and OT convergence.; Walker-Roberts et al., A Systematic Review of the Availability and Efficacy of Countermeasures to Internal Threats in Healthcare Critical Infrastructure.; Boddy et al., A Study into Data Analysis and Visualisation to increase the CyberResilience of Healthcare Infrastructures.; Rajamäki et al. Cybersecurity education and training in hospitals: Proactive resilience educational framework (Prosilience EF).
172. Global Digital Health Partnership, Securing Digital Health 2018.
173. Farrell, “Medicare Machine – patient details of any Australian for sale on Darknet”.
174. Minion, “Leaked ADHA document gives inside look at My Health Record challenges”.
175. Phillips, Dove & Knoppers. “Criminal Prohibition of Wrongful Re-Identification: Legal Solution or Minefield for Big-Data?”.
176. Asghar & Dali. Averaging Attacks on Bounded Perturbation Algorithms.
177. See note 174 above.
178. ABC News (24 July 2018).
179. Information and Privacy Commission NSW.
180. Information and Privacy Commission NSW, Voluntary Breach Notification.
181. ABC News (30 May 2019).
182. The Victorian Auditor General.
183. Ibid.
184. ABC News (22 February 2019); Houston & Colangelo. “Crime syndicate hacks 15,000 medical files at Cabrini Hospital demands ransom”.
185. NSW Dept of Industry.
186. Garetty et al., “National electronic health record systems as wicked projects the Australian experience.”; Mendelson, “The European Union General Data Protection Regulation (Eu 2016/679) and the Australian My Health Record Scheme – A Comparative Study of Consent to Data Processing Provisions.”; Rumbold & Pierscionek. “The Effect of the General Data Protection Regulation on Medical Research.”; Rocher et al., “Estimating the success of re-identifications in incomplete datasets using generative models.”
187. See note 159 above.
188. Ibid.
189. Ibid.
190. Arnold & Bonython. “No, its not OK for the government to use your prescription details to recruit you for a study”.
191. See note 12 above.
192. See note 119 above.
193. Khan & Latiful Hoque. “Digital Health Data: A Comprehensive Review of Privacy and Security Risks and Some Recommendations.”
194. Baillie, Bowden & Meyer. “Threshold capabilities: threshold concepts and knowledge capability linked through variation theory.”
195. Stahl et al., “Critical theory as an approach to the ethics of information security.”
196. Woodruff, “Fixing My Health Record will take more than Hunt”s promises”.
197. See note 159 above.
198. See note 12 above.
199. See note 13 above.
200. Nippon Telegraph and Telephone (NTT) Security, Global Threat Intelligence Report 2019.
201. See note 28 above.
202. See note 43 above.
Bibliography
- ABC News. (February 22, 2019). Accessed July 26, 2019. https://www.abc.net.au/news/2019-02-22/melbourne-heart-hack-cyber-criminals-my-health-record-risks/10834482/
- ABC News. (July 24, 2018) https://www.abc.net.au/news/2018-07-24/digital-health-agency-changes-my-health-record-app-contracts/10026644/
- ABC News. (May 30, 2019) https://www.abc.net.au/news/2019-05-30/victorian-hospitals-vulnerable-attack-auditor-general-hack-finds/11162352
- Abd-alrazaqa, A., B. M. Bewicka, T. Farraghera, and P. Gardner. “Factors that Affect the Use of Electronic Personal Health Records among Patients: A Systematic Review.” International Journal of Medical Informatics 126 (2019): 164–175. doi:10.1016/j.ijmedinf.2019.03.014.
- Abouzakhar, N. S., A. Jones, and O. Angelopoulou. “Internet of Things Security: A Review of Risks and Threats to Healthcare Sector. Joint 10th IEEE International Conference on Internet of Things, iThings 2017, 13th IEEE International Conference on Green Computing and Communications, GreenCom 2017.” 10th IEEE International Conference on Cyber, Physical and Social Computing, CPSCom 2017 and the 3rd IEEE International Conference on Smart Data, Smart Data. June 21, 2017 - June 23, 2017, Exeter UK.
- Abrar, H., S. J. Hussain, J. Chaudhry, K. Saleem, M. A. Orgun, J. Al-Muhtadi, and C. Valli. “Risk Analysis of Cloud Sourcing in Healthcare and Public Health Industry.” IEEE Access 6 (2018): 9140–9150.
- ACHSM university course accreditation guidelines. 2017. https://www.achsm.org.au/Portals/15/documents/education/university-accreditation/ACHSM-university-accreditation-guidelines.pdf
- ADHA. “About the DH Cyber Security Centre, ADHA.” https://www.digitalhealth.gov.au/about-the-agency/digital-health-cyber-security-centre/about
- Ahanger, T. A., and A. Aljumah. “Internet of Things: A Comprehensive Study of Security Issues and Defense Mechanisms.” IEEE Access 7 (2019): 11020–11028. doi:10.1109/ACCESS.2018.2876939.
- Akinsanya, O., M. Papadaki, and L. Sun. “Current Cybersecurity Maturity Models: How Effective in Healthcare Cloud?” Online Proceedings of the 5th Collaborative European Research Conference (CERC) March 29-30, 2019. http://ceur-ws.org/Vol-2348/
- Almohri, H., L. Cheng, D. Yao, and H. Alemzadeh. “On Threat Modeling and Mitigation of Medical Cyber-Physical Systems.” 2017 IEEE/ACM International Conference on Connected Health: Applications, Systems and Engineering Technologies (CHASE). DOI 10.1109/CHASE.2017.84
- Al-Muhtadi, J., B. Shahzad, K. Saleem, W. Jameel, and M. A. Orgun. “Cybersecurity and Privacy Issues for Socially Integrated Mobile Healthcare Applications Operating in a Multi-cloud Environment.” Health Informatics Journal 25, no. 2 (2019): 315–329. doi:10.1177/1460458217706184.
- Alonso, S. G., J. Arambarri, M. Lopez-Coronado, and I. de la Torre Diez. “Proposing New Blockchain Challenges in eHealth.” Journal of Medical Systems 43, no. 64 (2019). doi:10.1007/s10916-019-1195-7.
- Andriole, K. P. “Security of Electronic Medical Information and Patient Privacy: What You Need to Know.” Journal American College of Radiology 11, no. 12 (2014): 1212–1216. doi:10.1016/j.jacr.2014.09.011.
- Angraal, S., H. M. Krumholz, and W. L. Schulz. “Blockchain Technology: Applications in Health Care.” Circulatory & Cardiovasc Qual Outcomes 10 (2017): e003800. doi:10.1161/CIRCOUTCOMES.117.003800.
- Argaw, S. T., N. E. Bempong, B. Eshaya-Chauvin, and A. Flahault. The State of Research on Cyberattacks against Hospitals and Available Best Practice Recommendations: A Scoping Review. BMC Medical Informatics and Decision Making 19, 10 (2019). https://doi.org/10.1186/s12911-018-0724-5.
- Arnold, B. B., and W. Bonython. 2019. “No, It’s Not OK for the Government to Use Your Prescription Details to Recruit You for a Study”. The Conversation, July 31
- Asghar, H. J., and K. Dali. Averaging Attacks on Bounded Perturbation Algorithms. Australia: Macquarie University, 2019. February.
- Australian Cyber Security Centre (ACSC). 2018. “Joint Report on Publicly Available Hacking Tools. Australian Government Signals Directorate.” https://www.cyber.gov.au/sites/default/files/2019-03/u5-joint-product-acsc-release-final.pdf
- Australian Digital Health Agency. “National Health Security and Access Framework – NESAF V.4.” Australian Government. Accessed August 18, 2019. https://www.digitalhealth.gov.au/implementation-resources/ehealth-foundations/EP-1544-2014.
- Australian Digital Health Agency (ADHA). “Annual Report 2017–18.” Australian Government.
- Australian Government. 2018. “My Health Records (National Application) Amendment (Extension of Opt-out Period No. 2) Rules 2018.” Federal Register of Legislation, November 14.
- Australian Privacy Act. 1988. https://www.legislation.gov.au/Details/C2019C00241
- Baillie, C., J. A. Bowden, and J. H. Meyer. “Threshold Capabilities: Threshold Concepts and Knowledge Capability Linked through Variation Theory.” Higher Education 65, no. 2 (2012): 227–246. doi:10.1007/s10734-012-9540-5.
- Baranchuk, A., M. M. Refaat, K. K. Patton, M. K. Chung, K. Krishnan, V. Kutyifa, G. Upadhyay, J. D. Fisher, and D. R. Lakkireddy. “Cybersecurity for Cardiac Implantable Electronic Devices: What Should You Know?” Journal of the American College of Cardiology (JACC) 71, no. 11 (2018): 1284–1288. doi:10.1016/j.jacc.2018.01.023.
- BDO USA Healthcare. 2019. “Brace for the Breach - Cyberthreat Insights.” https://www.bdo.com/getattachment/630056fa-52ef-48e8-a25c-8e9fcff168a6/attachment.aspx?HC_Cyber-Threats_Insight_2-19_WEB.pdf
- Beeksow, J. 2015. “Reducing Security Risk Using Data Loss Prevention Technology.” Healthcare Financial Management, November, p.108–111.
- Blanke, S. J., and E. McGrady. “When It Comes to Securing Patient Health Information from Breaches, Your Best Medicine Is A Dose of Prevention: A Cybersecurity Risk Assessment Checklist.” Journal of Healthcare Risk Management 36, no. 1 (2016): 14–24. doi:10.1002/jhrm.21230.
- Blythe, J. M., and L. Coventry. “Costly but Effective: Comparing the Factors that Influence Employee Anti-malware Behaviours.” Computers in Human Behavior 87 (2018): 87–97. doi:10.1016/j.chb.2018.05.023.
- Boddy, A., W. Hurst, M. Mackay, and A. El Rhalibi. “A Study into Data Analysis and Visualisation to Increase the CyberResilience of Healthcare Infrastructures.” Online Proceedings of the Institute of Managers and Leaders (IML) Conference ‘International Conference on Internet of Things and Machine Learning’ October 17-18, 2017. http://iml-conference.org
- Boddy, A., W. Hurst, M. Mackay, A. El Rhalibi, T. R. Baker, and C. A. C. Montañez. “An Investigation into Healthcare-data Patterns.” Future Internet 11, no. 2 (2019): p1–23. doi:10.3390/fi11020030.
- Burke, W., T. Oseni, A. Jolfaei, and I. Gondal. “Cybersecurity Indexes for eHealth.” Proceedings - Australasian Computer Science Week Multiconference, ACSW January 29-31, 2019: 2019. doi:10.1145/3290688.3290721.
- Camara, C., P. Peris-Lopez, and J. E. Tapiador. “Security and Privacy Issues in Implantable Medical Devices: A Comprehensive Survey.” Journal of Biomedical Informatics 55 (2015): 272–289. doi:10.1016/j.jbi.2015.04.007.
- Canaway, R., D. I. R. Boyle, J. E. Manski‐Nankervis, J. Bell, J. S. Hocking, K. Clarke, M. Clark, J. Gunn, and J. Emery. “Gathering Data for Decisions: Best Practice Use of Primary Care Electronic Records for Research.” Medical Journal of Australia 210 (2019): S12–S16. doi:10.5694/mja2.50026.
- Carlton, M. 2016. Development of A Cybersecurity Skills Index: A Scenarios-Based Hands on Measure of Non-IT Professionals Cybersecurity Skills. Doctoral dissertation. Nova Southeastern University. NSU Works, College of Engineering and Computing. (979). https://nsuworks.nova.edu/gscis_etd/979
- Carter, A. B. “Considerations for Genomic Data Privacy and Security When Working in the Cloud.” The Journal of Molecular Diagnostics 21, no. 4 (2019): 542–552. doi:10.1016/j.jmoldx.2018.07.009.
- Chan, W. S. Y., and A. Y. M. Leung. “Use of Social Network Sites for Communication among Health Professionals: Systematic Review.” Journal Medical Internet Research 20, no. 3 (2018): e117. doi:10.2196/jmir.8382.
- Chaudhry, J., M. Crowley, P. Roberts, C. Valli, and J. Haass. “POStCODE Middleware for Post-market Surveillance of Medical Devices for Cyber Security in Medical and Healthcare Sector in Australia.” Conference: 2018 12th International Symposium on Medical Information and Communication Technology (ISMICT). Sydney, NSW, Australia.
- Chen, Y., S. Ding, Z. Xu, H. Zheng, and S. Yang. “Blockchain-Based Medical Records Secure Storage and Medical Service Framework.” Journal Medical Systems 43, no. 5 (2019). doi:10.1007/s10916-018-1121-4.
- Cilliers, L. “Wearable Devices in Healthcare: Privacy and Information Security Issues.” Health Information Management Journal ( Online Access 2019): 1–7. https://doi.org/10.1177/1833358319851684.
- Connory, M. 2019 “Annual Report.” State of Cyber Security. Security in Depth. https://securityindepth.com.au/
- Coventry, L., and D. Branley. “Cybersecurity in Healthcare: A Narrative Review of Trends, Threats and Ways Forward.” Maturitas 113 (2018): 48–52. doi:10.1016/j.maturitas.2018.04.008.
- Dameff, C. J., J. A. Selzer, J. Fisher, J. P. Killeen, and J. L. Tully. “Clinical Cybersecurity Training Through Novel High-Fidelity Simulations.” Journal of Emergency Medicine 56, no.2 ( 0736-4679 2019): 233–238. doi:10.1016/j.jemermed.2018.10.029.
- Department of Health. Framework to guide the secondary use of My Health Record system data. 2018. “Australian Government.” May. https://www1.health.gov.au/internet/main/publishing.nsf/Content/F98C37D22E65A79BCA2582820006F1CF/$File/MHR_2nd_Use_Framework_2018_ACC_AW3.pdf
- Department of Industry. “NSW Cyber Security Industry Development Strategy 2018.” NSW Government.
- Dogaru, D. I., and I. Dumitrache. “Cyber Security in Healthcare Networks.” Conference Proceedings of the 6th IEEE International Conference on E-Health and Bioengineering - EHB 2017, June 22-24. 978-1-5386-0358-1/17/
- Dubovitskaya, A., Z. Xu, S. Ryu, M. Schumacher, and F. Wang. “Secure and Trustable Electronic Medical Records Sharing Using Blockchain.” Proceedings - Annual Symposium proceedings. AMIA Symposium. 2017, p.650–659. New York, United States.
- Esposito, C., A. De Santis, G. Tortora, H. Chang, and -K.-K. R. Choo. “Blockchain: A Panacea for Healthcare Cloud-Based Data Security and Privacy?” IEEE Cloud Computing 5, Jan/Feb (2018): 31–37. doi:10.1109/MCC.2018.011791712.
- Farrell, P. 2017. “Medicare Machine – Patient Details of Any Australian for Sale on Darknet”. The Guardian, July 04. https://www.theguardian.com/australia-news/2017/jul/04/the-medicare-machine-patient-details-of-any-australian-for-sale-on-darknet/
- Farringer, D. “Cybersecurity Report Identifies Unique Challenges to Tackling Cybersecurity in Health Care.” J. Health & Life Sci. L 11, no. 1 (2017): 117.
- Fernandez-Aleman, J. L., A. Sanchez-Henarejos, A. Toval, A. B. Sanchez-Garcia, I. Hernandez-Hernandez, and L. Fernandez-Luque. Analysis of health professional security behaviors in a real clinical setting: An empirical study. International Journal of Medical Informatics. 84 (2015): 454–467.
- Firdaus, A., N. B. Anuar, M. F. A. Razak, I. A. B. Hashem, S. Bachok, and A. K. Sangaiah. “Root Exploit Detection and Features Optimization: Mobile Device and Blockchain Based Medical Data Management.” Journal of Medical Systems 42 (2018): 112. doi:10.1007/s10916-018-0966-x.
- Flaumenhaft, Y., and O. Ben-Assuli. “Personal Health Records, Global Policy and Regulation Review.” Health Policy 122, no. 8 (2018): 815–826. doi:10.1016/j.healthpol.2018.05.002.
- Food and Drug Administration (FDA). https://www.fda.gov/medical-devices
- Forcepoint Whitepaper. 2018. “Life Support: Eliminating Data Breaches in the Healthcare Sector.” https://www.forcepoint.com//whitepapers/
- Gardiyawasam Pussewalage, H. S., and V. A. Oleshchuk. “Privacy Preserving Mechanisms for Enforcing Security and Privacy Requirements in E-health Solutions.” International Journal of Information Management 36 (2016): 1161–1173. doi:10.1016/j.ijinfomgt.2016.07.006.
- Garetty, K., I. McLoughlin, A. Dalley, R. Wilson, and P. Yue. “National Electronic Health Record Systems as Wicked Projects the Australian Experience.” Information Polity 21 (2016): 367–381. doi:10.3233/IP-160389.
- Gaynor, M., G. Omer, and J. S. Turner. “Teaching EHRs Security with Simulation for Non-technical Healthcare Managers.” Journal of Healthcare Protection Management 32, no. 1 (2016): 84–97.
- General Data Protection Rule. 2018. https://gdpr-info.eu/
- Global Digital Health Partnership. 2018. “Securing Digital Health.” https://www.gdhp.org/media-hub/news_feed/gdhp-reports
- Gordon, W. J., A. Fairhall, and A. Landman. “Threats to Information Security — Public Health Implications.” The New England Journal of Medicine 377, no. 8 (2017): 707–709. doi:10.1056/NEJMp1707212.
- Gordon, W. J., A. Wright, R. J. Glynn, J. Kadakia, C. Mazzone, E. Leinbach, and A. Landman. “Evaluation of a Mandatory Phishing Training Program for High-risk Employees at a US Healthcare System.” Journal of the American Medical Informatics Association 26, no. 6 (2019): 547–552. doi:10.1093/jamia/ocz005.
- Grundy, Q., L. Parker, M. Raven, D. Gillies, B. Mintzes, J. Jureidini, and L. Bero. Finding Peace of Mind: Navigating the Marketplace of Mental Health Apps. Sydney: Australian Communications Consumer Action Network, 2017.
- “Health Informatics Society Australia.” Healthcare-Cybersecurity-Report, June-2018.
- HIPAA Omnibus Rule. 2013. “Summary.” http://www.hipaasurvivalguide.com/hipaa-omnibus-rule.php
- HIPAA Privacy Rule 1996.
- Holdsworth, J., W. B. Glisson, and K. K. Choo. “Medical Device Vulnerability Mitigation Effort Gap Analysis Taxonomy.” Smart Health 12 (2017): 82–98. doi:10.1016/j.smhl.2017.12.001.
- Houston, C., and A. Colangelo. 2019. “Crime Syndicate Hacks 15,000 Medical Files at Cabrini Hospital Demands Ransom”. The Age, February 22. Accessed July 30, 2019. https://www.theage.com.au/national/victoria/crime-syndicate-hacks-15-000-medical-files-at-cabrini-hospital-demands-ransom-20190220-p50z3c.html
- Huckvale, K., J. T. Prieto, M. Tilney, P.-J. Benghozi, and J. Car. “Unaddressed Privacy Risks in Accredited Health and Wellness Apps: A Cross-sectional Systematic Assessment.” BMC Medicine (2015) 13:214. doi:10.1186/s12916-015-0444-y.
- Information and Privacy Commission NSW. https://www.ipc.nsw.gov.au/data-breach-guidance
- Information and Privacy Commission NSW. Accessed July 27, 2019. https://www.ipc.nsw.gov.au/privacy/voluntary-data-breach-notification/
- Institute for Critical Infrastructure Technology (ICIT). 2016. Industry Brief: Hacking Healthcare. https://icitech.org/wp-content/uploads/2016/01/ICIT-Brief-Hacking-Healthcare-IT-in-2016.pdf
- IT News. 2015. “Hack linked to attack on US insurer Anthem.” June 22. https://www.itnews.com.au/news/opm-hack-linked-to-attack-on-us-insurer-anthem-405514
- Jalali, M. S., and J. P. Kaiser. “Cybersecurity in Hospitals: A Systematic, Organizational Perspective.” J Med Internet Res 20, no. 5, May (2018): e10059. doi:10.2196/10059.
- Jalali, M. S., M. Siegel, and S. Madnick. “Decision-making and Biases in Cybersecurity Capability Development: Evidence from a Simulation Game Experiment.” Journal of Strategic Information Systems 28 (2019): 66–82. doi:10.1016/j.jsis.2018.09.003.
- Jayaratne, M., D. Nallaperuma, D. De Silva, D. Alahakoon, B. Devitt, K. E. Webster, and N. Chilamkurti. “A Data Integration Platform for Patient-centered E-healthcare and Clinical Decision Support.” Future Generation Computer Systems 92 (2019): 996–1008. doi:10.1016/j.future.2018.07.061.
- Kamel Boulos, M., D. Giustini, and S. Wheeler. “Instagram and WhatsApp in Health and Healthcare: An Overview.” Future Internet 8, no. 37 (2016): 37. doi:10.3390/fi8030037.
- Khan, S. I., and A. S. L. Hoque. “Digital Health Data: A Comprehensive Review of Privacy and Security Risks and Some Recommendations.” Computer Science Journal of Moldova 24, no. 71 (2016): 2.
- King, Z. M., D. S. Henshel, L. Flora, M. G. Cains, B. Hoffman, Blaine, and C. Sample. “Characterizing and Measuring Maliciousness for Cybersecurity Risk Assessment.” Frontiers in Psychology 9, no. 39 (2018): p1–19.
- Klas-CHIME. 2019. “Whitepaper: How Aligned are Provider Organizations with the Health Industry Cybersecurity Practices (HICP) Guidelines?” KLAS Research and College of Healthcare Information Management Executives (CHIME). www.klasresearch.com/reports
- Kruse, C. S., B. Frederick, T. Jacobson, and D. K. Monticone. “Cybersecurity in Healthcare: A Systematic Review of Modern Threats and Trends.” Technology and Health Care 25 (2017): 1–10. doi:10.3233/THC-161263.
- Kruse, C. S., B. Smith, H. Vanderlinden, and A. Nealand. “Security Techniques for the Electronic Health Records.” J Med Syst 41 (2017): 127. doi:10.1007/s10916-017-0778-4.
- Lee, J. K., S. Y. Moon, and J. H. Park. “CloudRPS: A Cloud Analysis Based Enhanced Ransomware Prevention System.” The Journal of Supercomputing 73, no. 7 (2016): 3065–3084. doi:10.1007/s11227-016-1825-5.
- MacIntyre, C. R., T. E. Engells, M. Scotch, D. J. Heslop, A. B. Gumel, G. Poste, X. Chen, et al. “Converging and Emerging Threats to Health Security.” Environment and System Decisions 38, no. 2 (2018): 198–207. doi:10.1007/s10669-017-9667-0.
- Magnus, R. 2019. “Public Report of the Committee of Inquiry (COI) into the Cyber Attack on SingHealth.” January 10. https://www.mci.gov.sg/coireport
- Martin, G., P. Martin, C. Hankin, A. Darzi, and J. Kinross. “Cybersecurity and Healthcare: How Safe are We?” BMJ (Online) 358 (2017): j3179. doi:10.1136/bmj.3179.
- McSweeney, K. “Motivating Cybersecurity Compliance in Critical Infrastructure Industries: A Grounded Theory Study.” Dissertation Abstracts International Section A: Humanities and Social Sciences, 79. Dissertation Thesis. Capella University, January 2018
- Mendelson, D. “The European Union General Data Protection Regulation (Eu 2016/679) and the Australian My Health Record Scheme – A Comparative Study of Consent to Data Processing Provisions.” Journal of Law and Medicine 26 (2018): 23–38.
- Mense, A., A. Steger, M. Sulek, D. Jukic-Sunaric, and A. Meszaros. “Analyzing Privacy Risks of mHealth Applications.” Studies in Health Technology & Informatics 221 (2016): 41–45.
- Minion, L. “MHR Security Concerns Persist - ADHA Issues Amended Contracts for Third Party Apps”. Healthcare IT News. Accessed July 26 2019. https://www.healthcareit.com.au/article/my-health-record-security-concerns-persist-adha-issues-amended-contracts-third-party-apps
- Minion, L. 2018. “Leaked ADHA Document Gives inside Look at My Health Record Challenges”. Healthcare IT News, August. https://www.healthcareit.com.au/article/exclusive-leaked-adha-document-gives-inside-look-my-health-record-challenges
- Morris, C., R. E. Scott, and M. Mars. “Security and Other Ethical Concerns of Instant Messaging in Healthcare.” Studies in Health Technology & Informatics 254 (2018): 77–85. doi:10.3233/978-1-61499-914-0-77.
- My Health Record Statistics. 2019, July 28. Accessed August 12, 2019. www.myhealthrecord.gov.au
- My Health Records Act 2012, No. 63. https://www.legislation.gov.au/Details/C2017C00313
- National Audit Office Report. Investigation: WannaCry Cyber Attack and the NHS. https://www.nao.org.uk/wp-content/uploads/2017/10/Investigation-WannaCry-cyber-attack-and-the-NHS.pdf (2017).
- National Institute of Standards and Technology (NIST) Framework. https://www.nist.gov/cyberframework
- Natsiavas, P., J. Rasmussen, M. Voss-Knude, K. Votis, L. Coppolino, P. Campegiani, I. Cano, et al. “Comprehensive User Requirements Engineering Methodology for Secure and Interoperable Health Data Exchange.” BMC Medical Informatics & Decision Making 18, no. 85 (2018). doi:10.1186/s12911-018-0664-0.
- Nippon Telegraph and Telephone (NTT) Security. 2019. “Global Threat Intelligence Report.” https://www.nttsecurity.com/landing-pages/2019-gtir
- NSW Dept of Industry. 2018. “NSW-cyber-security-industry-development-strategy.”
- O’Dowd, and A. O’Dowd. “NHS Patient Data Security Is to Be Tightened after Cyberattack.” BMJ 358 (2017): j3412. doi:10.1136/bmj.j3412.
- O’Sullivan, D. M., E. O’Sullivan, M. O’Connor, D. Lyons, and J. McManus. “WhatsApp Doc?” BMJ Innovations 3 (2017): 238–239. doi:10.1136/bmjinnov-2017-000239.
- Office of the Australian Information Commissioner. My Health Record Privacy. (July 19, 2019). https://www.oaic.gov.au/privacy/other-legislation/my-health-record/
- Ogunlana, S. O. “Countering Expansion and Organization of Terrorism in Cyberspace.” Dissertation Abstracts International: Section B: The Sciences and Engineering 80 (2019): 3-B(E).
- Papoutsi, C., J. E. Reed, C. Marston, R. Lewis, A. Majeed, and D. Bell. “Patient and Public Views about the Security and Privacy of Electronic Health Records (Ehrs) in the UK: Results from a Mixed Methods Study.” BMC Medical Informatics & Decision Making 15, no. 86 (2015). doi:10.1186/s12911-015-0202-2.
- Park, Y. R., E. Lee, W. Na, S. Park, Y. Lee, and J.-H. Lee. “Is Blockchain Technology Suitable for Managing Personal Health Records? Mixed-Methods Study to Test Feasibility.” Journal Med Internet Research 21, no. 2 (2019): e12533. doi:10.2196/12533.
- Parker, L., V. Halter, T. Karliychuk, and Q. Grundy. “How Private Is Your Mental Health App Data? an Empirical Study of Mental Health App Privacy Policies and Practices.” International Journal of Law & Psychiatry 64 (2019): 198–204. doi:10.1016/j.ijlp.2019.04.002.
- Perakslis, E., and R. M. Califf. “Employ Cybersecurity Techniques against the Threat of Medical Misinformation.” JAMA. 322: 207. Published online June 14, 2019. https://jamanetwork.com/
- Phillips, M., E. S. Dove, and B. M. Knoppers. “Criminal Prohibition of Wrongful Re-Identification: Legal Solution or Minefield for Big-Data?” Bioethical Inquiry 14 (2017): 527–539. doi:10.1007/s11673-017-9806-9.
- PHIPA http://www.health.gov.on.ca/english/providers/project/priv_legislation/phipa_pipeda_qa.html
- Pinskier, N. “Royal Australian College of General Practitioners; Cited by Whigham, N.” https://www.news.com.au/technology/online/hacking/health-sector-tops-the-list-as-australians-hit-by-300-data-breaches-since-february/news-story/5e95c47694418ad072bf34d872e22124
- PIPEDA http://www.health.gov.on.ca/english/providers/project/priv_legislation/phipa_pipeda_qa.html
- Ponemon Institute. Cost of a Data Breach Report. 2019. IBM Security. https://www.ibm.com/security/data-breach/2019
- Pratt, M. “How Cyberattacks Can Impact Physicians.” Medical Economics 93, no. 12 (June, 2016): 43–47.
- Privacy Amendment (Notifiable Data Breaches) Act 2017, No. 12. https://www.legislation.gov.au/Details/C2017A00012
- Pullin, D. W. “Cybersecurity: Positive Changes through Processes and Team Culture.” Frontiers of Health Services Management 35, no. 1 (2018): 3–12. doi:10.1097/HAP.0000000000000038.
- Raber, I., C. P. McCarthy, and R. W. Yeh. “Health Insurance and Mobile Health Devices: Opportunities and Concerns.” Journal of the American Medical Association 321, no. 18 (2019): 1767–1768. doi:10.1001/jama.2019.3353.
- Raisaro, J. L., P. J. McLaren, J. Fellay, M. Cavassini, C. Klersy, and J.-P. Hubaux. “Are Privacy-enhancing Technologies for Genomic Data Ready for the Clinic? A Survey of Medical Experts of the Swiss HIV Cohort Study.” Journal of Biomedical Informatics 79 (2018): 1–6. doi:10.1016/j.jbi.2017.12.013.
- Rajamäki, J., J. Nevmerzhitskaya, and C. Virág. “Cybersecurity Education and Training in Hospitals: Proactive Resilience Educational Framework (Prosilience EF).” Proceedings - IEEE Global Engineering Education Conference (EDUCON), 17-20 April 2018, p.2042–2046. doi:10.1109/EDUCON.2018.8363488
- Raths, D. “What to Do if a Breach Happens to You.” Behavioral Healthcare V0l.36, no. 2 (2016): 45–46.
- Reagin, M. J., and M. V. Gentry. “Enterprise Cybersecurity: Building a Successful Defense Program.” American College of Healthcare Executives Journal 35, no. 1 (2018): 13–22.
- Rocher, L., . L., J. M. Hendrickx, and Y. de Montjoye. “Estimating the Success of Re-identifications in Incomplete Datasets Using Generative Models.” Nature Communications 10, no. 1 (2019). doi:10.1038/s41467-019-10933-3.
- Ropp, R., and B. Quammen. “Protecting Health Data in a Troubling Time. Understand Who and What You’re up Against.” Health Management Technology 36, no. 7 (2015): 14–15.
- Rosenfeld, L., J. Torous, and I. V. Vahia. “Data Security and Privacy in Apps for Dementia: An Analysis of Existing Privacy Policies.” American Journal Geriatric Psychiatry 25, no. 8 (2017): 873–877. doi:10.1016/j.jagp.2017.04.009.
- Rubenfire, A. “The Nightmare Scenario: Dialing Devices to Deadly.” Modern Healthcare 47 (2017): 4.
- Rumbold, J. M. M., and B. Pierscionek. “The Effect of the General Data Protection Regulation on Medical Research.” Journal of Medical Internet Research 19, no. 2 (2017): e47. doi:10.2196/jmir.7108.
- Safavi, S., A. M. Meer, E. K. J. Melanie, and Z. Shakur. “Cyber Vulnerabilities on Smart Healthcare, Review and Solutions.” Online Proceedings Cyber Resilience Conference (CRC). 2018 November 15- 18. doi:10.1109/CR.2018.8626826
- Sahi, A., D. Lai, and Y. Li. “Security and Privacy Preserving Approaches in the eHealth Clouds with Disaster Recovery Plan.” Computers in Biology and Medicine 78 (2016): 1–8. doi:10.1016/j.compbiomed.2016.09.003.
- Sajid, A., and H. Abbas. “Data Privacy in Cloud-assisted Healthcare Systems: State of the Art and Future Challenges.” Journal of Medical Systems 40, no. 155 (2016). doi:10.1007/s10916-016-0509-2.
- Saleem, K., K. Zeb, A. Derhab, H. Abbas, J. Al-Muhtadi, M. A. Orgun, and Gawanmeh. “Survey on Cybersecurity Issues in Wireless Mesh Networks Based eHealthcare.” Proceedings - 18th IEEE International Conference on e-Health Networking, Applications and Services, Healthcom, September 14-16, 2016. DOI: 10.1109/HealthCom.2016.7749423
- Schwartz, S., A. Ross, S. Carmody, P. Chase, S. C. Coley, J. Connolly, C. Petrozzino, and M. Zuk. “The Evolving State of Medical Device Cybersecurity.” Biomedical Instrumentation and Technology 52, no. 2 (2018): 103–110. doi:10.2345/0899-8205-52.2.103.
- Scott, R. E. “WhatsApp in Clinical Practice: A Literature Review.” Studies in Health Technology and Informatics 231 (2016): p 82–90. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emexa&AN=621263287.
- Sedlack, D. J. “Understanding Cyber Security Perceptions Related to Information Risk in a Healthcare Setting.” Conference Proceedings: Cyber Security Strategy in Healthcare. Twenty-second Americas Conference on Information Systems, San Diego, California, USA, 2016.
- Shah, R. “Protecting Australian Critical National Infrastructure in an Era of IT and OT Convergence.” Policy Brief Report No. 18/2019.
- Shenoy, A., and J. M. Appel. “Safeguarding Confidentiality in Electronic Health Records.” Cambridge Quarterly of Healthcare Ethics 26, no. 2 (2017): 337–341. doi:10.1017/S0963180116000931.
- Sher, M. L., P. C. Talley, C.-W. Yang, and K.-M. Kuo. “Compliance with Electronic Medical Records Privacy Policy: An Empirical Investigation of Hospital Information Technology Staff.” INQUIRY: The Journal of Health Care Organization, Provision, and Financing 54 (2017): 1–12.
- Siddique, M., M. A. Mirza, M. Ahmad, J. Chaudhry, and R. Islam. “A Survey of Big Data Security Solutions in Healthcare.” 14th International EAI Conference on Security and Privacy in Communication Networks, (SecureComm) August 8-10, 2018. Lecture Notes of the Institute for Computer Sciences, Social-Informatics and Telecommunications Engineering, LNICST, 255, p.391–406. Doi: 10.1007/978-3-030-01704-0_21
- Sittig, D. F., and H. Singh. “A Socio-technical Approach to Preventing, Mitigating, and Recovering from Ransomware Attacks.” Appl Clin Inform 7 (2016): 624–632. doi:10.4338/ACI-2016-04-SOA-0064.
- Small, S., D. Peddie, C. Ackerley, C. M. Hohl, and E. Balka. “Patient Perceptions about Data Sharing & Privacy: Insights from Action.” In Context Sensitive Health Informatics: Redesigning Healthcare Work, C. Nøhr, C.E. Kuziemsky, Z.S.-Y. Wong edited by. 2017, p.109–116. IOS Press: Amsterdam, Netherlands.
- Smigielski, R. “Hardening Infusion Pump Communication Software for Medical Device Cybersecurity.” Biomedical Instrumentation & Technology (2017): 46–50. https://search.proquest.com/docview/1967813395?accountid=12763.
- Smith, F. L. “Malware and Disease: Lessons from Cyber Intelligence for Public Health Surveillance.” Health Security 14, no. 5 (2016): 305–314. doi:10.1089/hs.2015.0077.
- Spence, N., N. Niharika Bhardwaj, D. P. Paul III, and A. Coustasse. “Ransomware in Healthcare Facilities: A Harbinger of the Future?” Perspectives in Health Information Management, Summer (2018): 1–22.
- Stahl, B. C., N. F. Doherty, M. Shaw, and H. Janicke. “Critical Theory as an Approach to the Ethics of Information Security.” Science and Engineering Ethics 20, no. 3 (2014): 675–699. doi:10.1007/s11948-013-9496-6.
- Stern, G. “A Life Cycle Approach to Medical Device Cybersecurity.” Biomedical Instrumentation and Technology 52, no. 6 (2018): 464–466. doi:10.2345/0899-8205-52.6.464.
- Taylor, M. “An SOS on Cybersecurity: To Protect Patient Data, Hospitals Beef up Risk Management Programs. Hello, Chief Security Officers and ‘White Hat Hackers’.” Hospitals & Health Networks 89, no. 2 (2015): 36–38.
- Terry, K. “HIPAA BREACH. Secure Data & Prevent Fines.” Medical Economics 92, no. 14 (2015): 26–32.
- Thakkar, V., and K. Gordon. “Privacy and Policy Implications for Big Data and Health Information Technology for Patients: A Historical and Legal Analysis.” Studies in Health Technology & Informatics 257 (2019): 413–417. doi:10.3233/978-1-61499-951-5-413.
- Thamilarasu, G., and C. Lakin. “A Security Framework for Mobile Health Applications. Proceedings −5th International Conference on Future Internet of Things and Cloud Workshops (FiCloudW)”. 2017, p.221–226. DOI 10.1109/W-FiCloud.2017.35
- UK Data Protection Act 2018 ico.org.uk. 2018-07-20
- Upendra, P., P. Prasad, G. Jones, and H. Fortune. “Operationalizing Medical Device Cybersecurity at a Tertiary Care Medical Center.” Biomedical Instrumentation & Technology 49, no. 4 (2019): 251–258. doi:10.2345/0899-8205-49.4.251.
- “Verizon 2019 Data Breach Investigations Report.” Verizon Enterprise Solutions. https://enterprise.verizon.com/resources/reports/dbir/
- The Victorian Auditor General, Andrew Greaves. https://www.theguardian.com/australia-news/2019/may/29/victorias-patient-data-vulnerable-to-cyber-attacks-says-audit/.
- Victorian Auditor General’s Office. 2019. “Independent Assurance Report to Parliament 2018–19.” May 23.
- Walker-Roberts, S., M. Hammoudeh, and A. Dehghantanha. “A Systematic Review of the Availability and Efficacy of Countermeasures to Internal Threats in Healthcare Critical Infrastructure, 2018.” IEEE Access. doi:10.1109/ACCESS.2018.2817560i.
- Wang, S., R. Gao, and Y. Zhang. “Searchable and Revocable Multi-data Owner Attribute-based Encryption Scheme with Hidden Policy in Cloud Storage.” PLoS ONE [Electronic Resource] 13, no.11 ( pone 2018): 0206126. doi:10.1371/journal.
- Wang, X., and Z. Zhang. “Data Division Scheme Based on Homomorphic Encryption in WSNs for Health Care Wireless Sensor Networks.” Journal of Medical Systems 39, no. 12 (2015): 1–7. doi:10.1007/s10916-015-0340-1.
- Wickham, M. H. “Exploring Data Breaches and Means to Mitigate Future Occurrences in Healthcare Institutions: A Content Analysis.” Dissertation Northcentral University, San Diego, School of Business and Technology Management, April 2019.
- Wilson, K., and L. Khansa. “Migrating to Electronic Health Record Systems: A Comparative Study between the United States and the United Kingdom.” Health Policy 122, no. 11 (2018): 1232–1239. doi:10.1016/j.healthpol.2018.08.013.
- Wirth, A. “Cyberinsights. Hardly Ever a Dull Moment: The Ongoing Cyberthreats of 2017.” Biomedical Instrumentation & Technology 51, no. 5 (2017): 431–443. doi:10.2345/0899-8205-51.5.431.
- Wirth, A. “Cyberinsights. The Times They are a-Changin’: Part One.” Biomedical Instrumentation & Technology 52, no. 2 (2018): 148–152.
- Woodruff, T. 2018. “Fixing My Health Record Will Take More than Hunt’s Promises”. Crikey INQ, August 02. https://www.crikey.com.au/2018/08/02/fixing-my-health-record-will-take-more-than-hunts-promises/
- Wright, A., S. Aaron, and D. W. Bates. “The Big Phish: Cyberattacks Against U.S. Healthcare Systems.” Journal of General Internal Medicine 31, no. 10 (2016): 1115–1118. doi:10.1007/s11606-016-3741-z.
- Yaraghi, N. I., and R. A. Gopal. “The Role of HIPAA Omnibus Rules in Reducing the Frequency of Medical Data Breaches: Insights from an Empirical Study.” Milbank Quarterly 96 (2018): 144–166. doi:10.1111/1468-0009.12314.
- Yasnoff, W. A. “Breach Risk Magnitude: A Quantitative Measure of Database Security.” AMIA 2016 Annual Symposium Proceedings/AMIA Symposium, 2017, (2016): p. 1258–1263.
- Zafar, H. “Cybersecurity: Role of Behavioral Training in Healthcare.” Proceedings - 22nd Americas Conference on Information Systems: Surfing the IT Innovation Wave, AMCIS 2016, August 11-14. San Diego, California, USA.
- Zaidan, B. B., A. Haiqi, A. A. Zaidan, M. Abdulnabi, M. L. Kiah, and H. Muzamel. “A Security Framework for Nationwide Health Information Exchange Based on Telehealth Strategy.” Journal of Medical Systems 39 (2015): 5. doi:10.1007/s10916-015-0235-1.
- Zeb, K., K. Saleem, J. Al Muhtadi, and C. Theummeler. “U-prove Based Security Framework for Mobile Device Authentication in eHealth Networks.” 2016 IEEE 18th International Conference on e-Health Networking, Applications and Services (Healthcom). DOI: 10.1109/HealthCom.2016.7749518
- Zhang, R., R. Xue, and L. Liu. “Searchable Encryption for Healthcare Clouds: A Survey.” IEEE Transactions on Services Computing 11, no. 6 (2018): 978–996. doi:10.1109/TSC.2017.2762296.
- Zheng, G., G. Zhang, W. Yang, C. Valli, R. Shankaran, and M. A. OrguA. “From WannaCry to WannaDie: Security Trade-offs and Design for Implantable Medical Devices.” Proceedings - 17th International Symposium on Communications and Information Technologies (ISCIT), September 25-27, 2017. DOI: 10.1109/ISCIT.2017.8261228
- Zhou, L., V. Varadharajan, and K. Gopinath. “A Secure Role-Based Cloud Storage System for Encrypted Patient-Centric Health Records.” Computer Society Journal 59, no. 11 (2016): 1159–1611.
- Zhou, W., Y. Jia, A. Peng, Y. Zhang, and P. Liu. “The Effect of IoT New Features on Security and Privacy: New Threats, Existing Solutions, and Challenges yet to Be Solved.” IEEE Internet of Things Journal 6, no. 2 (2019): 1606–1616. doi:10.1109/JIOT.2018.2847733.