ABSTRACT
Background
Although spoken discourse is an outcome prioritised by all stakeholders in aphasia rehabilitation, assessment and treatment of discourse are not routine clinical practice. The small evidence base, varied clinical expertise, multiple barriers in the workplace, and challenges for clients in understanding their altered language abilities all contribute to this situation. These factors need serious consideration when developing a new treatment. Involving intended stakeholders as partners in the development process is recommended. This assists with future implementation by ensuring assessment and treatment are practical, feasible, and acceptable to those who will deliver and undertake it.
Aims
This paper reports on the coproduction phase of the Linguistic Underpinnings of Narrative in Aphasia (LUNA) research project and describes the levels of partners’ involvement, the outcomes and impact of coproduction, and the factors that influenced it.
Methods and procedures
Four partners with aphasia and four speech and language therapists (SLTs) worked with academic team members across a 6-month period to create the LUNA assessment and treatment. Separate sessions were held with partners with aphasia (monthly) and SLTs (fortnightly). Coproduction methods included open discussion, the Someone Who Isn’t Me (SWIM) technique (thinking from others’ perspectives), low and high fidelity prototypes, flexible brainstorming, card sort, and active experimentation with assessment and treatment tasks. Verbal and written information was presented, shared and documented during each session in supportive formats, and each session summarised as accessible minutes.
Outcomes and Results
Partners contributed at consultation, cooperation, and co-learning levels during the coproduction phase. Outcomes included joined-up thinking across assessment-goal setting-treatment-desired outcomes; agreed decisions and content for assessment protocol and treatment manual; clarity on personalised, meaningful, and relevant treatment; therapeutic alliance operationalised in treatment manual; and more. Impacts included increased confidence, self-knowledge, pride, validation, peer support, networking, and benefits to SLTs’ services. Coproduction was positively influenced by consistent session structure and conduct, group dynamics, accessible communication methods, active task experimentation, and SWIM technique. Although the process was time and labour intensive, all partners considered this worthwhile.
Conclusions
LUNA has exemplified how an inclusive coproduction process can work well despite the language challenges of aphasia. Authors also believe that coproduction with intended users has resulted in products (assessment protocol, treatment manual) that are more practical, feasible, and acceptable to clinicians and clients than if designed by academics alone. This latter claim now needs testing on a wide scale.
Introduction
The term “discourse” encompasses core, everyday uses of language that are essential for expressing who we are and for engaging with others. Discourse is sometimes referred to in the aphasia literature as “connected speech”, and can be thought of as natural, everyday talk. O’Malley (Citation2019) notes three main perspectives on discourse: as language above the level of the clause or sentence; language in use or in action (how we get things done through language); and language as a way of constructing social identities and social realities.
Given its centrality to human communication, it is unsurprising that language disorders which impact discourse, such as aphasia, have considerable functional and psychosocial consequences, and that the recovery of discourse has been flagged as a priority by all those involved in aphasia rehabilitation (S. Wallace et al., Citation2017a., S.J. Wallace et al., Citation2017b; Worrall et al., Citation2011). Best practice statements emphasise the need for aphasia therapy to impact functional communication in real-world contexts and make reference to discourse treatment as one method for achieving this (Hebert et al., Citation2016; Power et al., Citation2015).
Despite the acknowledged importance of discourse, the inclusion of discourse assessment and treatment in aphasia rehabilitation is far from widespread. Research reporting on clinicians’ general practices in North America and Australia reveals clinicians very rarely assess and treat discourse abilities of people with aphasia and lack knowledge and confidence in discourse approaches (Rose et al., Citation2014; Simmons‐Mackie et al., Citation2005; Verna et al., Citation2009). Specific studies of clinicians’ discourse analysis practices reveal that the majority of clinicians do not routinely analyse clients’ spoken discourse, and the barriers of insufficient time, expertise, training, and resources substantially affect their capacity in this area (Bryant et al., Citation2017; Cruice et al., Citation2020). Reviews of discourse analysis studies show that 536 different linguistic and discourse measures have been used by researchers (Bryant et al., Citation2016; Pritchard et al., Citation2018). Discourse treatment has a small evidence base for varying study designs and levels of evidence, targeting different levels of language production and employing a wide range of therapeutic approaches and outcome measures (Dipper et al., Citation2020). This lack of consensus in discourse assessment and treatment contributes to clinicians’ limited focus on discourse in practice. Furthermore, alternative traditional therapies for people with aphasia typically focus only on word-level or sentence-level targets, and research evaluating these interventions rarely assesses generalisation to discourse level skills (Dipper et al., Citation2020; Webster et al., Citation2015).
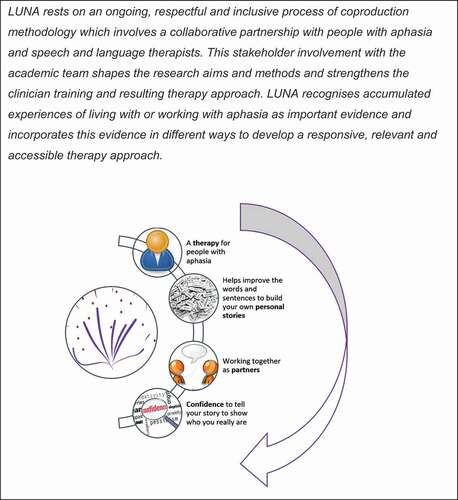
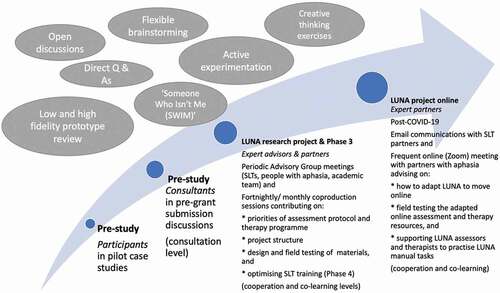
Collectively, these challenges signal not only a need to address discourse treatment, but also highlight that the process of developing this will need to be cognisant of the many barriers that already impact practice and not create further barriers. LUNA is a 3-year developmental proof-of-concept research project (https://blogs.city.ac.uk/luna/) that aims to respond to these dilemmas by developing an intervention which uniquely integrates the analysis and treatment of discourse, and which places a strong emphasis on clinical feasibility and acceptability for clients and clinicians. These factors are crucial for ensuring adherence to and effectiveness of any treatment programme in real-world settings (Bowen et al., Citation2009) and were intentionally foregrounded in this research. LUNA is funded by the UK Stroke Association, and follows the Medical Research Council guidance for the development and evaluation of complex interventions (Craig et al., Citation2008) with five phases: 1) systematic review of the discourse treatment literature; 2) large-scale survey of clinicians’ practices; 3) coproduction of assessment and treatment protocols (the phase reported here); 4) feasibility study of training clinicians in the LUNA analysis protocol; and 5) Randomised feasibility trial of the LUNA treatment, which targets personal storytelling at the word, sentence, and macro-structure level. In order to achieve a deep and authentic understanding of likely future feasibility and acceptability, the academic team embraced patient and public involvement (PPI) from inception. The resultant strong thread of PPI is woven through the project and manifests explicitly in (1) an advisory group comprising people with aphasia, SLTs and researchers who met regularly throughout the project and (2) a dedicated coproduction phase of six months (with these same clinicians and people with aphasia). The latter is the focus of this manuscript. The emphasis on working together in LUNA is clearly reflected in the project Mission Statement ().
In preparation for LUNA, Dipper and Cruice (Citation2018) carried out a pilot study in a university setting with five individuals with aphasia. Outcomes revealed statistically significant changes at all levels (word, sentence, macro-structure) for participants. However, it was not clear whether the procedures that worked in a university setting would be feasible for, and acceptable to, SLTs working within the National Health Service (NHS) in England. For example, discourse analysis, a focus of LUNA assessment, is time-consuming and infrequently undertaken by clinicians (Cruice et al., Citation2020). It was also important to ensure that the protocol would be maximally acceptable to people with aphasia, because this is essential for clinical effectiveness, adherence, and outcomes in real-world settings (Bowen et al., Citation2009). For example, would people with aphasia readily share personal stories from their lives and accept these being dissected into propositions and parts of speech, worked on, and rebuilt? Acceptability of end users was considered to be critically important. We drew on the minimal aphasia research literature on codesign, coproduction, and participatory action research to derive values, methods, and techniques. These include studies by our own team (e.g., Swinburn et al., Citation2019) as well as other prominent researchers in the field (Herbert et al., Citation2019; Mc Menamin et al., Citation2015; Wilson et al., Citation2015). Overall, coproduction in this field is relatively scarce as highlighted by Isaksen et al. (Citationin press) scoping review of PPI in aphasia research. Other recent literature (e.g., Charalambous et al., Citation2020 for a systematic review of user involvement in quality of life outcome measure development) shows involvement has been mostly consultative in nature.
The term coproduction can be used in various different ways, but here we broadly follow the participatory research definition outlined by Cook et al. (Citation2017) that is: “the maximisation of the participation of those whose life or work is the subject of the research in all stages of the research process” (p. 475).
The emphasis on coproduction in LUNA reflects a growing recognition that it is an important extension of notions of “patient-centredness” in clinical research contexts (Schanberg & Mullins, Citation2019). It recognises that those who experience a health condition can and should be fully engaged in driving the research agenda, including the early development of novel interventions. Recent research has identified a taxonomy of eight approaches to intervention development, in which the Partnership approach resonates clearly with the coproduction ethos of LUNA (O’Cathain et al., Citation2019). In this approach, throughout the development process the people whom the intervention aims to help have at least equal decision-making powers with members of the academic team. illustrates the levels and roles of partner involvement in LUNA and the coproduction methods used. The use of coproduction in LUNA also aims to overcome at least some of the known difficulties in translating research into practice (Graham et al., Citation2006). For example, Bowen et al. (Citation2009) make the point that feasibility research should explore factors that relate to uptake and effectiveness in real-world contexts in addition to focusing on an intervention’s efficacy in highly controlled conditions. These factors include acceptability (for both intervention recipients and providers), demand, implementation (or the degree to which an intervention can be provided in relevant health care settings), and practicality, for example, with respect to resources. Addressing these factors requires the meaningful engagement of practitioners and community members in research. Similar points are made by Kagan and colleagues (Kagan et al., Citation2010) when discussing how to close the gap between research and practice. Reviewing models of Knowledge Transfer Exchange (KTE), they argue for an “iterative process that requires social interaction and stakeholder engagement” (p. 538). Here, intended research beneficiaries are involved in research from the very earliest stages, with coproduction being flagged as the best form of transfer. Coproduction is considered to optimise the impact of research by foregrounding implementation at the outset of all activity between researchers and others (Phipps et al., Citation2016).
This paper describes the coproduction process that underpinned the development of the LUNA assessment and treatment protocol, following the GRIPP2 reporting checklist by Staniszewska et al. (Citation2017) which illustrates how PPI was embedded in the project. See supplementary file for detailed item reporting. This paper outlines the fundamental values of the project, and the aims, content, and techniques of coproduction sessions. It reports the outcomes and impacts of coproduction, and the factors that influenced the process. The discussion focuses on the implications of the coproduction process for the feasibility of the LUNA protocol.
Materials and methods
Design
LUNA was initiated with the intention of involving people with aphasia and SLTs working in this field. The pilot study afforded the opportunity to approach a group of people with aphasia who had participated and invite them personally to collaborate on LUNA. Because feasibility of running the programme in everyday practice also relies on clinician acceptability, we individually invited SLTs known to the lead authors as working in the area of aphasia, from a range of different settings and experience levels. These individuals were seen as partners in the research and not subject to ethics according to the guidance of the Health Research Authority and INVOLVE, the peak body for patient and public involvement in the United Kingdom (Health Research Authority/INVOLVE, Citation2016; see Hersh et al., Citation2021 for an entire manuscript discussing research partners and ethics). Some partners with aphasia had previously been involved in similar roles in training, designing services, and one in research project codesign, and others were new to the process of coproduction. Regarding the writing of this manuscript, core content was first discussed with partners. Academic team members and SLTs drafted various sections. The first draft was circulated in an email to SLTs for consideration, and separately discussed with partners with aphasia during a videoconferencing group call.
Positionality and reflexivity
Whilst the academic team (co-authors MC, LD, MP) aimed to adopt the role of “non-expert” during the sessions (facilitating discussion and gathering all opinions equally), we nevertheless acknowledge that these individuals approached LUNA from a scientific, linguistic, and interventionist position. Academic team members were SLTs (MC, MP) and a clinical linguist (LD) with limited (MP) to extensive (MC, LD) experience in conducting research on topics related to aphasia, and a good level of experience working clinically with people with aphasia (MC). We reflect on this later in the Discussion.
People involved
Four people with aphasia (VD, LS, SM, JB) and four NHS SLTs (SA, NC, SG, RT) worked together with the academic team over a 6-month period. The partners with aphasia had mild or moderate aphasia resulting from stroke on average nine years previously. The individual SLTs were approached to participate based on the breadth and depth of their clinical experience, and the range of clinical insight and expertise they could bring to the process. The group included South-East England-based SLT clinical team leads and managers (average 16 years experience) from settings spanning the continuum of care (e.g., inpatient to community-based services), geographical settings (e.g., rural and urban-based health-provider trusts) and practice settings (e.g., hospitals and private practices). Including this range of experience aimed to represent the views of many potential LUNA end-users (in this case, SLTs) in the design process itself, to help ensure the approaches developed would be responsive and appropriate to their needs (Bowen et al., Citation2009).
Partners with aphasia drew on their lived experience of aphasia, storytelling with language impairment, and speech therapy; SLT partners drew on their experience of providing aphasia assessment and treatment in a resource-constrained NHS, as well as training and motivating SLTs in changing their everyday clinical practices. The two groups met separately with the same three academic team members (MC, LD, MP) who were present at all sessions. There were roughly equal numbers of academic and non-academic collaborators at each meeting. Sessions were held fortnightly with the SLTs and monthly with people with aphasia. Whilst many coproduction research stakeholders meet together, this separation in LUNA was intentional and had been thoughtfully considered. It was grounded in meaningfulness and respect, reflecting that the groups were frequently contributing to different aspects of the protocol. For example, the SLT partners reviewed and synthesized research findings to select assessment and outcome protocol, whereas the partners with aphasia provided their views about the value of specific treatments and suggested when, where and how they might practice in real-life. Minutes were shared across both coproduction groups to exchange perspectives. Both groups were reimbursed for travel expenses, people with aphasia received an honorarium following INVOLVE guidelines (https://www.invo.org.uk/) and SLTs’ time was reimbursed to the NHS.
Stages of the study and levels of involvement
The aim was to coproduce the LUNA treatment by involving partners at all stages of the study. outline the sessions for partners with aphasia (5 sessions of 6 hFootnote1 each) and SLTs (11 sessions of 4 h eachFootnote2) respectively. For both groups, the main task was to agree the design and the specifics of the LUNA treatment, with SLTs also heavily focused on agreeing the assessment/outcome protocol. Partners also disseminated from this phase, presenting at a national clinical symposium (short oral by SLTs; poster by partner with aphasia and one academic team member). In the following section we outline methods common to both groups, followed by details of the sessions for each of the groups separately.
Table 1. Partners with aphasia session content summary.
Table 2. SLT partners session content summary.
Common coproduction elements
The limited literature on coproduction in aphasia rehabilitation was reviewed and key elements extracted (Mc Menamin et al., Citation2015; Wilson et al., Citation2015) and coproduction values and ethos were established for both groups at the outset. Key points and “ground rules” agreed were that the team would work in partnership, with each person’s contribution being equally considered and valued. That is, members agreed that preference would not be given to academics or professionals or service users, but all comments would be noted and discussed. Minutes from sessions (see further below) are testimony to this. Members were expected to be open-minded and creative while sharing their experiences, perspectives, and opinions, and to listen respectfully to the experiences, perspectives, and opinions of others. In order to facilitate equal weight of opinion across members of the wider team, one member of the academic team assumed the role of chair. This involved facilitating discussion by simplifying language where needed, keeping track of decisions, and representing them visually for the whole group. It was felt to be essential that clear and transparent documentation was implemented throughout sessions. The documentation process involved writing keywords on white boards and supporting communication by documenting using simpler words or constructions, taking and sharing photos of these comments. Accessible minutes for each session were written, circulated by email to SLT partners, and printed in hardcopy for partners with aphasia and SLT partners and reviewed in the subsequent session. Minutes (hardcopy) were also swapped between groups, i.e., minutes from partners with aphasia brought to the next SLT session, and vice versa. This facilitated exchange between the groups. Another key strategy employed was to build in ample time during sessions. This afforded multiple opportunities to actively share different techniques, which included practicing therapy, workshopping personal stories to improve them, and heavily critiquing existing story resources.
Both groups also used a variety of coproduction methods. These included using low and high fidelity prototype materials and working through activities and tasks (active experimentation). Partners were often invited to share reflections. To capture broader perspectives, a technique called “Someone Who Isn’t Me” (SWIM: Wilson et al., Citation2015) was used. This entailed asking each partner to identify an SLT or a person with aphasia whom they knew. Details regarding this person’s abilities, attitudes, and opinions were briefly and physically documented on a sheet of paper so these SWIMs could be referred to and feature in the discussions. At times during sessions, individuals were asked to give their own responses to the issue under consideration and then to report how they thought their SWIM would respond to the same issue. SWIMs have been used successfully in aphasia coproduction research as a starting point to develop personas, i.e., hypothesized archetypal target users (Neate et al., Citation2019).
Coproduction sessions with partners with aphasia
During sessions, information was presented, shared, and documented using aphasia-accessible formats (Stroke Association, Citation2012). Each session began with an introductory period to allow the members to get to know or catch up with each other. After the first meeting, each session reviewed the previous one before introducing the topics and activities for the current session (). The topics and activities included reviewing and refining key concepts, such as discourse and models of discourse. Sessions explored perspectives about important aspects of treatment, such as what makes good speech therapy, and the desirable skills and personal qualities of therapists. Sessions considered how stories were significant in people’s own lives, asking for examples about what kinds of stories they tell and hear, and what makes a good story. The academic team shared the evidence base about treatment, inviting partners with aphasia to actively try and provide feedback on the specific treatment approaches being considered. Following this, partners advised on the best ways to communicate concepts and activities to intended clients and made suggestions about how to design procedural aspects of therapy so that they would be acceptable.
Each session was subsequently summarised in accessible minutes and used as the basis for the review portion of the next session. Minutes included photographs from sessions that aimed to capture the breadth and detail of people’s input. For example, “what constitutes good therapy” included partner quotes “I want them to be flexible to me, there, that day” as well as distilled points (e.g., “good therapy includes choices of goals”). Reviewing and revisiting minutes allowed iterative refinement of the concepts and discussion topics across the sessions.
Coproduction sessions with SLT partners
Beginning with an introduction to the LUNA approach, the coproduction process, and expectations and requirements of the partners, the group then discussed the research evidence about discourse approaches in aphasia (). Here we drew on Boyle (Citation2014) and Pritchard et al. (Citation2018) for approaches to assessment, and Dipper et al. (Citation2020) for approaches to treatment. We also discussed current practice and barriers to using discourse approaches, drawing on SLTs’ own experience as well as LUNA’s survey findings (Cruice et al., Citation2020).
Most sessions were devoted to creating and developing Phase 3 assessment and treatment protocol/manuals, with some limited consideration of Phase 4 SLT training. Using an iterative prototyping method, the group discussed and trialled prototype manuals and published clinical resources and made various modifications. Different sections of the manuals were presented across the weeks corresponding to separate aspects of the LUNA model focusing on word, sentence, and discourse levels. As noted previously, the SWIM technique explored potential responses of an even wider range of clinicians. This approach aimed to maximise future acceptability and uptake by considering the different reactions clinical staff might have if asked to use novel assessments and treatments. It also helped the experienced SLTs to reflect deeply on their own concerns or choices in clinical settings. Other coproduction methods included flexible brainstorming, a visual and tangible approach to idea generation and sharing amongst the group (Mc Menamin et al., Citation2015). This typically entailed putting all generated ideas onto post-it notes, then as a group modifying, confirming, or rejecting the ideas. Flexible brainstorming was often followed by a card-sorting technique to categorise the brainstorming material to clearly convey organisation and salient points. Direct ranking of the cards was used to prioritise ideas. As an example, the group spent 12 hours alone reviewing and debating linguistic analyses for the assessment protocol. Analyses were categorised according to analysis type, then ranked in order of need, usability, and clinical feasibility and acceptability before being mapped and ordered on to a large flow diagram which formed the basis of the assessment protocol.
Between sessions, SLTs completed tasks so that trial and usage of developed methods were embedded in the coproduction process. A good example of this process involved trialling and scoring assessment procedures in preparation for the following session to compare outcomes and discuss changes to improve reliability and usability of the assessment protocol. SLTs reflected on what clinicians would accept in terms of time and complexity in the context of a busy clinic. SLTs also utilised feedback from partners with aphasia who critiqued and commented on the solutions that SLTs developed within and between sessions via the exchange of minutes (and verbal recap or explanations from academic team present). All views were important to the decisions made about LUNA processes.
Measuring the impact of coproduction
Overall, a qualitative and reflexive approach was taken to documenting the impact of coproduction in Phase 3. Minutes recorded both discussion points and agreement and were an information source for reflection on writing this manuscript. In the final session, partners with aphasia discussed the impact, benefits and challenges of the process. Facing time pressures in the final session, SLTs individually answered questions via email, and responses were anonymised and returned to the group for further consideration. Academic team members reflected on impact following the end of Phase 3.
Results
Partners attended all sessions, with one SLT and one partner with aphasia each missing one session each due to illness. Partners’ involvement in LUNA can be conceptualised as consultation, cooperation, and co-learning (). Cook et al. (Citation2017) define consultation as “local opinions are asked for but outside researchers conduct the work and decide on a course of action” (p. 478); cooperation as “local people work together with outside researchers to determine priorities, with responsibility remaining with outsiders for directing the process” (p. 478); and co-learning as “local people and outsiders share their knowledge in order to create new understanding and work together to form action plans, with outsiders providing facilitation” (p. 478).
Table 3. Levels of coproduction at each substage of LUNA (phase 3) (following Cook et al., Citation2017).
Outcomes and impacts of PPI on the research: LUNA assessment and treatment
There were numerous positive outcomes of partners’ involvement in this study, and their contributions and the impact of these on the research have been combined in this section (i.e., we have combined the reporting of GRIPP2 items 7a and 7b, Outcomes of PPI and Impact of PPI respectively). With respect to assessment, coproduction resulted in linking goal setting into the assessment process, two companion assessment protocols (resulting further in a new research question), linking outcome measurement indicators to meaningful change from treatment, and a new discourse outcome indicator. First, SLT partners highlighted that patient-centred goal setting was core to their practice and that framing the LUNA assessments in these terms would be important. As such, SLTs felt that LUNA assessments could be integrated where goal-setting discussions indicated the need for support across language levels, a focus on confidence with narrative and discourse-level self-expression. Second, feasibility and acceptability feedback about which discourse outcome indicators (and how many) to include led to a decision to split the assessment protocol into two: i) a core set of indicators for clinical use and ii) an additional set of indicators to inform the treatment trial. This yielded a novel research question exploring the potential association (and possible redundancy) between the two assessment protocols, e.g., #narrative words (clinical protocol) and #Correct Information Units (CIUs; research protocol). Third, there was extensive discussion and debate about indicators at the three different discourse levels (word, sentence, and discourse macrostructure); this discussion highlighted the importance of linking outcome measures to meaningful change for clients, a connection not always evident in the published literature. For example, Dipper et al. (Citation2020) found that outcomes are typically divorced from the treatment provided and certainly not reported in papers in terms of how meaningful they are to clinicians and clients. The relationship between outcome measures and time/resources available was vigorously debated and highlighted how challenging it is for clinicians to work across multiple levels of language. Analyses that yielded limited therapeutic value were not supported. Finally, SLT partners identified overall listener judgment as important at the discourse macro-structure level; this represents a useful outcome measure for future trials (including Phase 5) and accords with UK SLTs’ emphasis on the functional and pragmatic aspects of discourse, i.e., conveying gist and listener awareness (Cruice et al., Citation2020).
With respect to treatment, coproduction confirmed the emphasis on personalised treatment, and resulted in goals that joined up treatment focus with desired outcomes and a clinically applicable treatment and manual. Coproduction also helped realise meaningful and relevant treatment and therapeutic alliance, and informed therapy decision-making when choices were available, e.g., grammar/drill/meaning-focused approaches to sentence level therapy. These are discussed in turn.
First, LUNA treatment became strongly focused on goals. SLT partners were clear that goal setting should be personalised and linked explicitly to treatment and outcome, and much discussion was had that shaped treatment decisions. One SLT partner noted “… having a team of NHS clinicians who were able to support and challenge one another has led to richer discussion and a more balanced viewpoint of what a clinically applicable treatment protocol should look like”. Academic partners noted that sessions with SLTs strongly informed the level of clarity, detail, and specificity that would be needed in a treatment manual for therapists and assistants to deliver the treatment. This emerged consistently during discussions but was explicitly illustrated in SLT SWIM feedback. For example, when commenting on prototype materials, SWIMs reported: “[a] worked example will make me feel safe”; “not confident – didn’t like the flexibility”; “I’m overwhelmed with the number of steps. I’m angry with LUNA for suggesting I have time to do it”; “My SWIM is happy. Likes the tool, likes the rating scales”; and “My SWIM finds it confusing that the model doesn’t match the assessment and therapy”. Academic partners thus realised that intended users would approach LUNA on a continuum of interest, competence and confidence in discourse analysis and treatment, and a treatment manual needs to accommodate this.
Partners with aphasia translated academic team vocabulary regarding the underpinning framework for spoken discourse and the five LUNA goals into accessible vocabulary for future users; for example, the pragmatics, macrostructure planning, propositional and linguistic components (Dipper et al., Citation2021) were turned into much simpler “planning, thinking and organizing words and sentences” and extended to “LUNA will help you by guiding on how to choose the story, select the information, and organize it by putting words in the right order in sentences, and organizing the series of sentences”. Partners with aphasia refined the treatment goals which the academic team had earlier developed: LUNA should make a story 1) richer, 2) more meaningful, 3) more complete, 4) make more sense, and 5) flow more, so that they were expressed in a manner that was clear to them and would be easily understood by others with aphasia; for example, “make it more complete and less boring by using more connecting words and less ‘and/and then’”. These goals were then used as a structure for orientation during sessions in which partners tried out treatment activities; and the joined-up thinking (goals that link treatment focus to desired outcome) features strongly in the resultant treatment manual (Phase 5). For example, in one session partners with aphasia workshopped an SLT partner’s story about a South-East Asian insect delicacy culinary tour by changing the order and removing and adding information to make it more complete and flow more, and make more sense.
Second, partners with aphasia described good treatment as having a choice in their story goals, being able to personalise the work, and having the chance to practice regularly. One specifically highlighted the importance of working 1:1 with the therapist (i.e., high-quality instruction) and not in groups. They emphasised the need to make treatment part of everyday life, providing tools for everyday life, and making activities interesting and fun. Similarly, they noted treatment would only be good if accompanied by a good therapist, someone who was really engaged in therapy and responsive to their client, and who would make clients feel comfortable and support their confidence: “if I tried it [communicating] and it wasn’t good, I go home and hide. If I tried it and people were nice to me, I try again”. Partners with aphasia advised frequently about the best words to use to describe aspects of treatment. For example, semantic feature analysis charts (Boyle, Citation2010) inspired explanations of “spider diagram” for “linking up lost words” and to “learn to find the pathways to words” in order to “stop being boring” and “lessen my frustration”. These were subsequently written into the treatment manual and piloted (Phase 5).
Finally, partners with aphasia trialled a wide range of treatment activities during sessions, based on the different therapies from the systematic review (Dipper et al., Citation2020). These experiential exercises provided useful immediate learning and insights, and the explicit feedback from partners with aphasia informed what therapies and activities LUNA should eventually incorporate. Comments indicated which treatment activities were acceptable (“I understand this”; “I can hear what I’m doing”; “we did a little bit, step by step … that helped”) or not (“I didn’t get anywhere … very complex”; “it hurt my brain … it’s so frustrating; “why did we both with that? It didn’t make a story”).
In addition to Phase 5 assessment and treatment protocol outcomes, academic partners noted outcomes/benefits more broadly across the project. SLT partners fed back on Phase 4 prototype training slides, improving the acceptability through explanations and use of examples, and advising about how much could realistically be achieved in one day. Discussions with SLT partners on the LUNA evidence synthesis highlighted that published reviews have limited value for informing clinicians about the treatments undertaken. This influenced the academic team’s Phase 1 dissemination resulting in some considerable treatment detail being tabulated in Dipper et al. (Citation2020) and knowledge exchange resources developed for clinicians (see https://cityaccess.org/). Finally, both partners with aphasia and SLT partners were engaged in dissemination from Phase 3 as noted earlier in this paper, presenting at a national clinical symposium.
Impact of coproduction
Research partners’ reflections (captured in the minutes from discussions within sessions and on email following study completion; see Methods) illustrated the impact of coproduction on themselves personally and professionally. Partners with aphasia reported benefits which included learning about the evidence base for treatments: “The research … no one ever tells you … it was good to hear”, and increased confidence and self-knowledge: “It’s helped me to be more forward [confident/taking opportunities] because of what we’re doing here.” One person’s comments reflected the value she placed on meeting other people with aphasia and learning from them. There was obvious communicative benefit to her of coming together and being exposed to how other people with aphasia talked, and she was inspired by it.
SLT partners described the experience as interesting, fun, and clinically relevant; collaborative, building something creative and meaningful; and feeling validated, and gaining valuable insights. They reported many individual benefits pertaining to professional development, peer learning, and support. They highlighted gains in knowledge and skills, both in the assessment and treatment of discourse and in research processes and appraisal, some of which directly influenced practice:
“The first time in a while that I’ve looked at one short language sample in such depth and with such discussion. Great reminder of the value of doing this to gain a better understanding of someone’s communication, and worth the time and effort cost. This has resulted in a direct change to my own practice and advice given to local SLTs”.
They also identified advantages to working in a team with colleagues from different clinical services, and the academic team in terms of networking, learning from others, and reflecting on one’s own skills. At the service level, partners recounted the opportunities to share learning outcomes with colleagues and explore new therapy ideas with service users. They highlighted specific service developments relating to their involvement in the research, such as: encouraging colleagues to attend the training days, reflecting as a team on discourse assessment and therapy approaches, and advocating and supporting delivery of discourse level intervention.
Contextual and process factors
In terms of contextual and process factors that enabled or hindered coproduction, partners with aphasia noted session structure, group dynamics, and accessible methods as enablers. Partners saw the structure of the sessions as helpful: “I like the way that you present it for us … it’s regular, it’s got a pattern”. Group dynamics were positive: “If someone wasn’t so nice maybe I wouldn’t have said so much”, “I feel comfortable, I can say what I want, it doesn’t matter if we make a mistake, we feel comfortable and you’ve done that”, and “Three or four people different aphasia … very different things [language strengths and difficulties] for different people … different aphasia talents”. People also felt that the methods used to document the sessions were good: “[Pointing to academic team] you’re very clever … at getting stuff down [pointing at flipcharts, minutes] … helps me remember”. One person acknowledged that the sessions were challenging, but still produced feelings of satisfaction: “Like here … am completely exhausted when we leave. It’s much more talking, I have to take a day before to rest, and a day after. I’m drained afterwards – I need to nap, but I love it”. Finally, when asked what worked and what didn’t work about the process, people with aphasia were mainly positive: “Safe space”, “Been heard and know that it will help people” and only had a few negative comments: “Some has not been fantastic” and “It is a little bit sad that we are here because we have aphasia … if we were okay, we wouldn’t be here”.
SLT partners noted SWIM method, exchange of information with partners with aphasia, and session conduct. The SWIM approach was mentioned as a helpful, although sometimes challenging, methodology. SWIM was found to encourage empathy from the perspectives of others, and challenge inherent assumptions, in order to give new insights. In particular, SLT SWIMs gave valuable contributions specifically the “reflections and thoughts of a time and resource poor clinician with multiple demands” (benefit reflected by one SLT SWIM at the end of project). Academic partners noted that SWIMs were usually more revealing with SLTs, however at a specific point they helped illuminate different views in partners of aphasia. For example, during experimentation with sentence therapy activities, two SWIMs preferred a meaning-focused approach to sentence treatment activities; one preferred a rule-based approach, “because he likes boring things and is good at rules”; and one preferred a drill focused approach “because it’s straightforward”.
SLTs additionally commented on the benefits of the feedback from partners with aphasia and the opportunity to discuss similarities and differences between the outcomes of the two concurrent series of sessions. Testing activities (at home or in the workplace) during and between sessions were beneficial in providing accurate feedback.
In terms of practicalities, SLTs valued the regularity and timing of the sessions and having clear aims and objectives. There was general praise for the leadership of the academic team and having nominated personnel to chair and minute the sessions. The role of the chair was to facilitate discussion by simplifying language where needed, keeping track of decisions, and representing them visually for the whole group. This role was viewed as key to the process of maintaining equal value across all members. Overall, feedback on the process was overwhelmingly positive, and there were minimal suggestions for improvement, although the labour- and time-intensive process of coproduction was acknowledged.
Finally, academic partners noted that time, familiarity, and documentation were important. Having ample time for partners to meet properly, discuss tasks and experiences, experiment with activities was key to developing rapport and a safe space to share and express their opinions. Time was often needed for explaining and recapping; one partner with aphasia said: “[you] give me time to … get ideas out. [if the session was] quick quick quick … I just don’t say anything”. With respect to familiarity, keeping to a similar format or structure to the sessions was helpful, inducing predictability so that people could relax and know what to expect. Finally, accessible agendas and minutes, and communication support during sessions was key to enabling partners with aphasia to contribute.
Discussion
The investment in a rigorous coproduction process aimed to operationalise the LUNA Mission Statement, to align with the team’s commitment to person-centred practice, and to optimise LUNA as a novel intervention that would be genuinely feasible and acceptable to stakeholders. Considering the difficulties reported by SLTs in incorporating discourse level work into their clinical practice (Cruice et al., Citation2020), the academic team felt that it was important that the LUNA discourse analysis protocol and the LUNA treatment manual would be carefully tailored for intended users – SLTs working in mainstream service provision and clients with post-stroke aphasia most likely in outpatient/community settings.
Outcomes and impacts: a critical perspective
Although further intervention refinement and definitive testing are still needed, the team has prioritised developing a new assessment, treatment, and outcome measure package that can be implemented in real contexts, even with the reported barriers to lack of time and resources for SLTs. We believe the coproduction within LUNA has helped to make this possible. Approaches to intervention development now explicitly acknowledge user engagement in a coproduction partnership approach (O’Cathain et al., Citation2019). Similarly, Yardley et al. (Citation2015) argue for a “person-based approach” in intervention development and argue for mixed methods research (interviews, focus groups, observation, questionnaire studies) to systematically investigate the beliefs, attitudes, needs, and situations of those who will be using the intervention. This degree of systematic inquiry into users’ views (recipients and providers) was not possible in LUNA, although the survey of SLTs’ practices (Cruice et al., Citation2020) is one such example. Further consideration of this approach in intervention development in aphasia rehabilitation is warranted.
SLTs’ feedback consistently emphasised key issues: time pressure, lack of access to resources, the level of clarity and detail needed for busy clinicians, and the centrality of client goals in guiding assessment and intervention. These points have strengthened the links between client goals, treatment, and outcome measures. This transparency of links between goals, assessment, treatment, and outcome (Hersh et al., Citation2012) is an important element in working collaboratively with clients with aphasia. LUNA therefore rests on a model of coproduction but also promotes ongoing collaboration by deliberately building it into all stages of the intervention. A person with aphasia does not receive therapy with LUNA but co-creates it through their choices and cultivation of a story that gives them confidence and a way to express themselves and their identity.
The SWIM method brought many more hypothetical SLT perspectives into the room, which helped crystallise how to make LUNA acceptable to a wider range of SLTs than those physically present. Ultimately, the delivery of LUNA will rely on individual practitioners and SLT teams making the choice to respond to the acknowledged importance of discourse and so do something different in their practice. In designing the LUNA materials, the desire is to support as many SLTs as possible and not to alienate them. As a result of the coproduction process, we feel that we have addressed a range of SLT perspectives and thereby maximised acceptability. Although the SWIM method has been used successfully with people with aphasia (e.g., Wilson et al., Citation2015) it did not work as well for partners with aphasia as for the SLT partners. The SWIM technique is known to work better for people whose language is more mildly or moderately (rather than severely) impaired (Wilson et al., Citation2015); however, this does not account for the comparatively reduced success here. It was instead due to resources. It took cognitive and linguistic efforts to create an additional persona, and then to express views and opinions on their behalf, making it difficult to combine SWIM reflections and LUNA activity practice in a single session. In other research projects, whole workshops have been dedicated to SWIM and persona generation, leading to successful and effective application (Neate et al., Citation2019).
Coproducing LUNA with partners with aphasia helped to capture what was important to them. They shaped the content of LUNA by suggesting words to explain it to future users in a meaningful way, and by providing ideas about practicing stories and more complex language in their everyday lives. Experimentation with actual activities resulted in the richest insights from partners with aphasia, whereas more explicit requests for comment were sometimes less effective. Active engagement with activities led to detailed feedback about what makes for good therapy. Partners were also vocal about the important qualities that a therapist should demonstrate during therapy, which is known to influence how someone engages in their rehabilitation (Lawton et al., Citation2018). As noted in the Methods, partners with aphasia had been involved as research participants in early pilot work towards LUNA, and undoubtedly their experience influenced their engagement in this current process. Indeed, one individual repeatedly said: “I learnt more from you in 10 weeks than 8.5 years at college”, and her genuine appreciation was a strong current during sessions. However, we acknowledge that this (earlier involvement as participant) is atypical for usual coproduction. This process helped to ensure that LUNA treatment makes sense to those who will receive it, is practical for patients, and motivates people with aphasia to be fully engaged in their aphasia rehabilitation to optimise potential outcomes. Furthermore, partners with aphasia reported several benefits from being involved: pride in their achievements, greater confidence, less boredom, and new friendships. Having a safe space for discussion helped people to share their opinions, to feel that they were heard, and to be proud to be able to help others. These benefits largely align with those identified by Brett et al. (Citation2012) regarding empowerment and feeling valued, listened to, and more positive about one’s experiences.
Brett et al. (Citation2012) highlight that good user involvement needs to be well-planned, and takes time, and this was reflected in the six-month timeframe given to the coproduction phase. It is important to acknowledge our funders and their review panel for recognising the value of this. The commitment of partners in terms of time and effort was also crucial. This commitment went beyond turning up on the day and contributing; for SLT partners there was additional “invisible” time spent reflecting on the ideas in their own time and in their own clinical settings; and for partners with aphasia there was often preparation before and recuperation after each session.
Critical reflection: definition, process, and methods
The process of coproduction is not always effective and can be impeded by power imbalances, lack of commitment to the process by the different parties, inadequate methods for gathering experiences, lack of follow-through and poor implementation of suggestions (Dimopoulos-Bick et al., Citation2018). In the case of LUNA, these challenges were met by approaching both groups as partners, by capturing feedback effectively, and by integrating suggestions in a transparent manner. A systematic review of PPI in health and social care research highlights that involving stakeholders as partners in the team, and threading involvement throughout the research (rather than sporadically) leads to positive outcomes (Brett et al., Citation2012). It was possible to achieve this on LUNA with the three academic team members, four people with aphasia, and four SLTs working together, forming strong relationships and building trust. Spending time with partners was core to the success of LUNA’s coproduction and indeed an extraordinary time commitment was devoted. This was deemed essential though when working with partners with altered language abilities after stroke, and in working jointly with SLTs through the minutiae of decision-making. Academic members were positively biased in this regard, as SLTs and clinical linguists themselves accustomed to this time expenditure. Our assumptions that this would lead to strong relationships, respect and trust were seen through (for more researcher reflections, see Mc Menamin et al., Citationin press). We acknowledge however that not all academic teams may be able to devote this time, and indeed not all funders support this. Furthermore, the coproduction sessions with partners with aphasia – essentially day workshops – reflected a level of contribution that might not be universally acceptable to others with aphasia. Indeed, limiting session times has often been the practice and important in equalising and supporting participation for some collaborators with aphasia. Caution is needed here, and researchers need to adjust the process and activities to accommodate the needs of individuals taking part in research initiatives. Howe et al. (Citation2017) noted that relational aspects of PPI – developing relationships and team building – are core to the success of PPI in research. It is beyond the scope of this paper to reflect fully on all aspects of our coproduction philosophy; however, Howe et al. (Citation2017) provide an extensive list of ingredients that facilitate good PPI which are worthy of further consideration in aphasia rehabilitation research. Overall, our coproduction process in LUNA met the definition raised earlier (Cook et al., Citation2017) in that partners were involved in a genuine sense at nearly all stages of the project design. However, our approach did not extend to partners collecting or analysing data, which would not have been feasible given the other aims of the funded trial. In future studies, academic teams might look to designing interventions which even more fully involve people with aphasia at these levels.
Conclusion
Coproduction in LUNA has been integral to the research project, core to the philosophy, the working relationships, the product and the planned implementation. LUNA exemplifies how coproduction at consultation, co-operation and co-learning levels can work well despite the language challenges of aphasia, and contribute to a feasible, acceptable novel intervention to assist with discourse-level rehabilitation.
APH-SI_20-179-File008.docx
Download MS Word (21.2 KB)Acknowledgments
This research is funded by The Stroke Association, grant number TSA2017/01. We would like to thank Dr Kate Swinburn for comments on the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
Notes
1. This included morning and afternoon refreshment breaks and lunch break
2. This included a morning tea break and a working lunch
References
- Bowen, D. J., Kreuter, M., Spring, B., Cofia-Woerpel, L., Linnan, L., Weiner, D., Bakken, S., Kaplan, C. P., Squiers, L., Fabrizio, C., & Fernandez, M. (2009). How we design feasibility studies. American Journal of Preventive Medicine, 36(5), 452–457. https://doi.org/10.1016/j.amepre.2009.02.002
- Boyle, M. (2010). Semantic feature analysis treatment for aphasic word retrieval impairments: What’s in a name? Topics in Stroke Rehabilitation, 17(6), 411–422. https://doi.org/10.1310/tsr1706-411
- Boyle, M. (2014). Test-retest stability of word retrieval in aphasic discourse. Journal of Speech, Language, and Hearing Research, 57(3), 966–978. https://doi.org/10.1044/2014_JSLHR-L-13-0171
- Brett, J., Staniszewska, S., Mockford, C., Herron-Marx, S., Hughes, J., Tysall, C., & Suleman, R. (2012). Mapping the impact of patient and public involvement on health and social care research: A systematic review. Health Expectations, 17(5), 637–650. https://doi.org/10.1111/j.1369-7625.2012.00795.x
- Bryant, L., Ferguson, A., & Spencer, E. (2016). Linguistic analysis of discourse in aphasia: A review of the literature. Clinical Linguistics & Phonetics, 30(7), 489–518. https://doi.org/10.3109/02699206.2016.1145740
- Bryant, L., Spencer, E., & Ferguson, A. (2017). Clinical use of linguistic discourse analysis for the assessment of language in aphasia. Aphasiology, 31(10), 1105–1126. https://doi.org/10.1080/02687038.2016.1239013
- Charalambous, M., Kambanaros, M., & Annoni, J.-M. (2020). Are people with aphasia (PWA) involved in the creation of quality of life and aphasia impact-related questionnaires? A scoping review. Brain Sciences, 10(10), 688. https://doi.org/10.3390/brainsci10100688
- Cook, T., Boote, J., Buckley, N., Vougioukalou, S., & Wright, M. (2017). Accessing participatory research impact and legacy: Developing the evidence base for participatory approaches in health research. Educational Action Research, 25(4), 472–488. https://doi.org/10.1080/09650792.2017.1326964
- Craig, P., Dieppe, P., Macintyre, S., Michie, S., Nazareth, I., & Petticrew, M. (2008). Developing and evaluation complex interventions: the new Medical Research Council guidance. BMJ, 337, a1655 https://doi.org/10.1136/bmj.a1655
- Cruice, M., Botting, N., Marshall, J., Marshall, J., Hersh, D., Pritchard, M., & Dipper, L. (2020). UK speech and language therapists’ views and reported practices of discourse analysis in aphasia rehabilitation. International Journal of Language and Communication Disorders, 55(3), 417–442. Advance online publication. https://doi.org/10.1111/1460-6984.12528
- Dimopoulos-Bick, T., Dawda, P., Maher, L., Verma, R., & Palmer, V. (2018). Experience-Based Co-Design: Tackling common challenges. Journal of Health Design, 3(1), 86–93. https://doi.org/10.21853/JHD.2018.46
- Dipper, L., & Cruice, M. (2018). Personal storytelling in aphasia: A single case study of LUNA therapy [abstract]. Aphasiology, 32(suppl.1), 60–61. https://doi.org/10.1080/02687038.2018.1487919
- Dipper, L., Marshall, J., Boyle, M., Botting, N., Hersh, D., Pritchard, M., & Cruice, M. (2020). Treatment for improving discourse in aphasia: A systematic review and synthesis of the evidence base. Aphasiology, 1–43. https://doi.org/10.1080/02687038.2020.1765305
- Dipper, L., Marshall, J., Boyle, M., Hersh, D., Hersh, D., & Cruice, M. (2021). Creating a theoretical framework to underpin discourse assessment and intervention in aphasia. Brain Sciences, 11(2), 183. https://doi.org/10.3390/brainsci11020183
- Graham, I. D., Logan, J., Harrison, M. B., Straus, S. E., Tetroe, J., Caswell, W., & Robinson, N. (2006). Lost in knowledge translation: Time for a map? The Journal of Continuing Education in the Health Professions, 26(1), 13–24. https://doi.org/10.1002/chp.47
- Health Research Authority/INVOLVE. (2016). Public involvement in research and research ethics committee review. https://www.invo.org.uk/wp-content/uploads/2016/05/HRA-INVOLVE-updated-statement-2016.pdf
- Herbert, D., Patrice Lindsay, M., McIntyre, A., Kirton, A., Rumney, P., Bagg, S., Bayley, M., Dowlatshahi, D., Dukelow, S., Garnhum, M., Glasser, E., Halabi, M.-L., Kang, E., MacKay-Lyons, M., Martino, R., Rochette, A., Rowe, S., Salbach, N., Semenko, B., & Teasell, R. (2016). Canadian stroke best practice recommendations: Stroke rehabilitation practice guidelines, update 2015. International Journal of Stroke, 11(4), 459–484. https://doi.org/10.1177/1747493016643553
- Herbert, R., Gregory, E., & Haw, C. (2019). Collaborative design of accessible information with people with aphasia. Aphasiology, 33(12), 1504–1530. https://doi.org/10.1080/02687038.2018.1546822
- Hersh, D., Israel, M., & Shiggins, C. (2021). The ethics of patient and public involvement across the research process: Towards partnership with people with aphasia. Aphasiology, 1–27. https://doi.org/10.1080/02687038.2021.1896870
- Hersh, D., Worrall, L., Howe, T., Sherratt, S., & Davidson, B. (2012). SMARTER goal setting in aphasia rehabilitation. Aphasiology, 26/2(2), 220–233. https://doi.org/10.1080/02687038.2011.640392
- Howe, A., Mathie, E., Munday, D., Cowe, M., Goodmanm, C., Keenan, J., Kendall, S., Poland, F., Staniszewska, S., & Wilson, P. (2017). Learning to work together – lessons from a reflective analysis of a research project on public involvement. Research Involvement and Engagement, 3(1), 1–22. https://doi.org/10.1186/s40900-016-0051-x
- Isaksen, J., Shiggins, C., Olsen, A. M., Coath, C., & Mc Menamin, R. (in press). Involvement of people with aphasia in research: A scoping review. Aphasiology.
- Kagan, A., Simmons-Mackie, N., Gibson, J. B., Conklin, J., & Elman, R. J. (2010). Closing the evidence, research, and practice loop: Examples of knowledge transfer and exchange from the field of aphasia. Aphasiology, 24(4), 535–548. https://doi.org/10.1080/02687030902935959
- Lawton, M., Haddock, G., Conroy, P., Serrant, L., & Sage, K. (2018). People with aphasia’s perception of the therapeutic alliance in aphasia rehabilitation post stroke: A thematic analysis. Aphasiology, 32(12), 1397–1417. https://doi.org/10.1080/02687038.2018.1441365
- Mc Menamin, R., Griffin, M., Gryzbowska, B., & Pound, C. (in press). Working together: Experiences of people with aphasia as co-researchers in participatory health research studies. Aphasiology. doi: 10.1080/02687038.2021.1923948
- Mc Menamin, R., Tierney, E., & MacFarlane, A. (2015). Who decides what criteria are important to consider in exploring the outcomes of conversation approaches? A participatory health research study. Aphasiology, 29(8), 914–938. https://doi.org/10.1080/02687038.2015.1006564
- Neate, T., Bourazeri, K., Roper, A., Stumpf, S., & Wilson, S. (2019). Co-created personas: Engaging and empowering users with diverse needs within the design process. CHI 2019 Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems (pp. 650). New York, USA.
- O’Cathain, A., Croot, L., Sworn, K., Duncan, E., Rousseau, N., Turner, K., Yardley, L., & Hoddinott, P. (2019). Taxonomy of approaches to development interventions to improve health: A systematic methods overview. Pilot and Feasibility Studies, 5(41), 1–27. https://doi.org/10.1186/s40814-019-0425-6
- O’Malley, M.-P. (2019). Discourse. In J. S. Damico & M. J. Ball (Eds.), Encyclopaedia of human communication sciences and disorders,606–608. SAGE. https://doi.org/10.4135/9781483380810.n201
- Phipps, D., Cummings, J., Pepler, D., Craig, W., & Cardinal, S. (2016). The co-produced pathway to impact describes knowledge mobilization processes. Journal of Community Engagement and Scholarship, 91(1), 31–40. https://digitalcommons.northgeorgia.edu/jces/vol9/iss1/5/
- Power, E., Thomas, E., Worrall, L., Rose, M., Togher, L., Nickels, L., Hersh, D., Godecke, E., O’Halloran, R., Lamont, S., O’Conner, C., & Clark, K. (2015). The development and validation of Australian aphasia rehabilitation Best Practice Statements using the RAND/UCLA appropriateness method. BMJOpen, 5, e007641. https://doi.org/10.1136/bmjopen-2015-007641
- Pritchard, M., Hilari, K., Cocks, N., & Dipper, L. (2017). Reviewing the quality of discourse information measures in aphasia. International Journal of Language and Communication Disorders, 52(6), 689–732. https://doi.org/10.1111/1460-6984.12318
- Pritchard, M., Hilari, K., Cocks, N., & Dipper, L. (2018). Psychometric properties of discourse measures in aphasia: Acceptability, reliability, and validity. International Journal of Language & Communication Disorders, 53(6), 1078–1093. https://doi.org/10.1111/1460-6984.12420
- Rose, M., Ferguson, A., Power, E., Togher, L., & Worrall, L. (2014). Aphasia rehabilitation in Australia: Current practices, challenges and future directions. International Journal of Speech-Language Pathology, 16(2), 169–180. https://doi.org/10.3109/17549507.2013.794474
- Schanberg, L. E., & Mullins, C. D. (2019). If patients are the true north, patient-centeredness should guide research. Nature Reviews. Rheumatology, 15(1), 5–6. https://doi.org/10.1038/s41584-018-0129-y
- Simmons‐Mackie, N., Threats, T., & Kagan, A. (2005). Outcome assessment in aphasia: A survey. Journal of Communication Disorders, 38(1), 1–27. https://doi.org/10.1016/j.jcomdis.2004.03.007
- Staniszewska, S., Brett, J., Simera, I., Seers, K., Mockford, C., Goodlad, S., Altman, D., Moher, D., Barber, R., Denegri, S., Entwhistle, A., Littlejohns, P., Morriss, C., Suleman, R., Thomas, V., & Tysall, C. (2017). GRIPP2 reporting checklists: Tools to improve reporting of patient and public involvement in research. BMJ, 358, j3453. https://doi.org/10.1136/bmj.j3453
- Stroke Association (2012). Accessible information guidelines. making information accessible for people with aphasia. https://www.stroke.org.uk/shop/product/accessible-information-guidelines.
- Swinburn, K., Best, W., Cruice, M., Smith, L., Pearce Willis, E., Ledingham, K., Sweeney, J., & McVicker, S. (2019). A concise patient reported outcome measure for people with aphasia: The aphasia impact questionnaire 21. Aphasiology, 33(9), 1035–1060. https://doi.org/10.1080/02687038.2018.1517406
- Verna, A., Davidson, B., & Rose, T. (2009). Speech‐language pathology services for people with aphasia: A survey of current practice in Australia. International Journal of Speech-Language Pathology, 11(3), 191–205. https://doi.org/10.1080/17549500902726059
- Wallace, S., Worrall, L., Rose, T., Le Dorze, G., Cruice, M., Isaksen, J., Kong, A., Simmons Mackie, N., Scarinci, N., & Gauvreau, C. (2017a). Which outcomes are most important to people with aphasia and their families? An international nominal group technique study framed within the ICF. Disability and Rehabilitation, 39(14), 1364–1379. https://doi.org/10.1080/09638288.2016.1194899
- Wallace, S. J., Worrall, L., Rose, T., & Le Dorze, G. (2017b). Which treatment outcomes are most important to aphasia clinicians and managers? An international e-Delphi consensus study. Aphasiology, 31(6), 643–673. https://doi.org/10.1080/02687038.2016.1186265
- Webster, J., Whitworth, A., & Morris, J. (2015). Is it time to stop “fishing”? A review of generalisation following aphasia intervention. Aphasiology, 29(11), 1240–1264. https://doi.org/10.1080/02687038.2015.1027169
- Wilson, S., Roper, A., Marshall, J., Galliers, J. R., Devane, N., Booth, T., & Woolf, C. (2015). Codesign for people with aphasia through tangible design languages. CoDesign, 11(1), 21–34. https://doi.org/10.1080/15710882.2014.997744
- Worrall, L., Sherratt, S., Rogers, P., Howe, T., Hersh, D., Ferguson, A., & Davidson, B. (2011). What people with aphasia want: Their goals according to the ICF. Aphasiology, 25(3), 309–322. https://doi.org/10.1080/02687038.2010.508530
- Yardley, L., Ainsworth, B., Arden-Close, E., & Muller, I. (2015). The person-based approach to enhancing the acceptability and feasibility of interventions. Pilot and Feasibility Studies, 1(37). https://doi.org/10.1186/s40814-015-0033-z